Neurofibromatosis 1 is a tumor predisposition genetic syndrome with autosomal dominant inheritance and virtually 100% penetrance by the age of 5 years. NF1 results from a loss-of-function mutation in the NF1 gene, resulting in decreased levels of neurofibromin in the cell. Neurofibromin is a negative regulator of various intracellular signaling pathways involved in the cellular proliferation. Although the loss of heterozygosity in the NF1 gene may predispose NF1 patients to certain malignancies, additional genetic alterations are a prerequisite for their development. The precise nature of these additional genetic alterations is not well defined, and genetic testing of all malignancies in NF1 patients becomes an essential component of future research in this subset of patients. In addition to germline NF1 mutations, alteration of the somatic NF1 gene is associated with sporadic malignancies such as adenocarcinoma of the colon, myelodysplastic syndrome, and anaplastic astrocytoma. The lack of well-defined screening tests for early detection and the nonspecific clinical presentation contribute to a poorer outcome in malignancies associated with NF1. Small study group size, mixed patient population, and a lack of uniformity in reporting research results make comparison of treatment outcome for this group difficult. An International Consensus Meeting to address and recommend best practices for screening, diagnosis, management, and follow-up of malignancies associated with NF1 is needed.
Keywords: NF1, Neurofibromatosis, Malignancy, Cancer
Learning Objectives
After completing this course, the reader will be able to:
Describe phenotypic and clinical features associated with neurofibromatosis 1.
Identify malignant tumors associated with neurofibromatosis 1.
This article is available for continuing medical education credit at CME.TheOncologist.com
Abstract
Introduction.
Neurofibromatosis 1 is a tumor predisposition genetic syndrome with autosomal dominant inheritance and virtually 100% penetrance by the age of 5 years. NF1 results from a loss-of-function mutation in the NF1 gene, resulting in decreased levels of neurofibromin in the cell. Neurofibromin is a negative regulator of various intracellular signaling pathways involved in the cellular proliferation. Although the loss of heterozygosity in the NF1 gene may predispose NF1 patients to certain malignancies, additional genetic alterations are a prerequisite for their development. The precise nature of these additional genetic alterations is not well defined, and genetic testing of all malignancies in NF1 patients becomes an essential component of future research in this subset of patients. In addition to germline NF1 mutations, alteration of the somatic NF1 gene is associated with sporadic malignancies such as adenocarcinoma of the colon, myelodysplastic syndrome, and anaplastic astrocytoma.
Materials and Methods.
A comprehensive English and non-English language search for all articles pertinent to malignancies associated with NF1 was conducted using PubMed, a search engine provided by the U.S. National Library of Medicine and the National Institutes of Health. Key words searched included the following: “malignancies associated with NF1”, “tumors associated with NF1”, and “NF1 and malignancies”. A comprehensive analysis in terms age and mode of presentation, investigation and therapeutic modalities, and outcome of the published data was performed and compared with similar information on the sporadic cases.
Results.
Malignancies in NF1 patients typically occur at an earlier age and, with an exception of optic pathway gliomas, certain types of malignancies carry a poor prognosis compared with their sporadic counterparts. Malignancies are the leading cause of death in NF1 patients, resulting in a 10- to 15-year decreased life expectancy compared with the general population.
Conclusions.
The lack of well-defined screening tests for early detection and the nonspecific clinical presentation contributes to a poorer outcome in malignancies associated with NF1. Small study group size, mixed patient population, and a lack of uniformity in reporting research results make comparison of treatment outcome for this group difficult. An International Consensus Meeting to address and recommend best practices for screening, diagnosis, management, and follow-up of malignancies associated with NF1 is needed.
Introduction
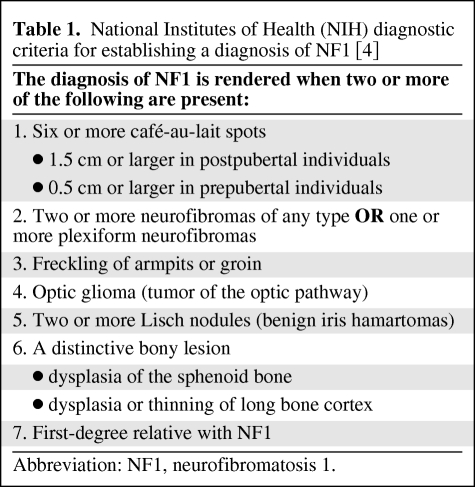
Neurofibromatosis 1 (NF1) is one of the most common genetic syndromes affecting all racial and ethnic groups, with a prevalence of 1 in 2000 to 1 in 5000 persons [1]. NF1 has an autosomal dominant inheritance with 100% penetrance and variable degrees of expression [2]. The phenotype of uniquely affected individuals may vary, but the cardinal manifestations of NF1 are multiple café au lait spots, cutaneous neurofibromas, and Lisch nodules of the iris [3]. The clinical diagnosis of NF1 is based on criteria established by the National Institutes of Health Consensus Development Conference in 1987 (Table 1). The diagnosis of NF1 is confirmed when at least 2 of the 7 criteria are identified [4]. Note that most clinical manifestations cited are not exclusive to NF1; however, axillary freckling and Lisch nodules can be considered pathognomonic of NF1 [5, 6]. Although NF1 typically runs a benign clinical course, unique malignancies associated with NF1 are the most common cause of death in this group and reduce average life expectancy by 10–15 years [7].
Table 1.
National Institutes of Health (NIH) diagnostic criteria for establishing a diagnosis of NF1 [4]
Abbreviation: NF1, neurofibromatosis 1.
Genetics
Neurofibromatosis 1 results from a loss-of-function mutation in the NF1 gene localized to chromosome band 17q11.2, and comprised of 60 exons and 350 kb of genomic DNA [8]. More than 500 different NF1 mutations have been identified, of which most are unique to a particular kindred [9]. The protein product of NF1, neurofibromin, is known to activate ras GTPase, which promotes the hydrolysis of active ras-GTP to inactive ras-GDP [10–14]. Reduction (in haploinsufficient cells) or complete loss (in cells that have also lost function of the normal NF1 allele) of neurofibromin leads to activation of ras signal transduction pathway, which regulates a cascade of downstream signaling pathways, including mitogen-activated protein kinase (MAPK), phosphatidylinositol 3-kinase (PI3K), protein kinase B (PKB), and mammalian target of rapamycin (mTOR) kinase. Activation of these pathways results in a variety of cellular effects that generally stimulate cellular proliferation and survival [15].
Neurofibromatosis 1 and Malignancy
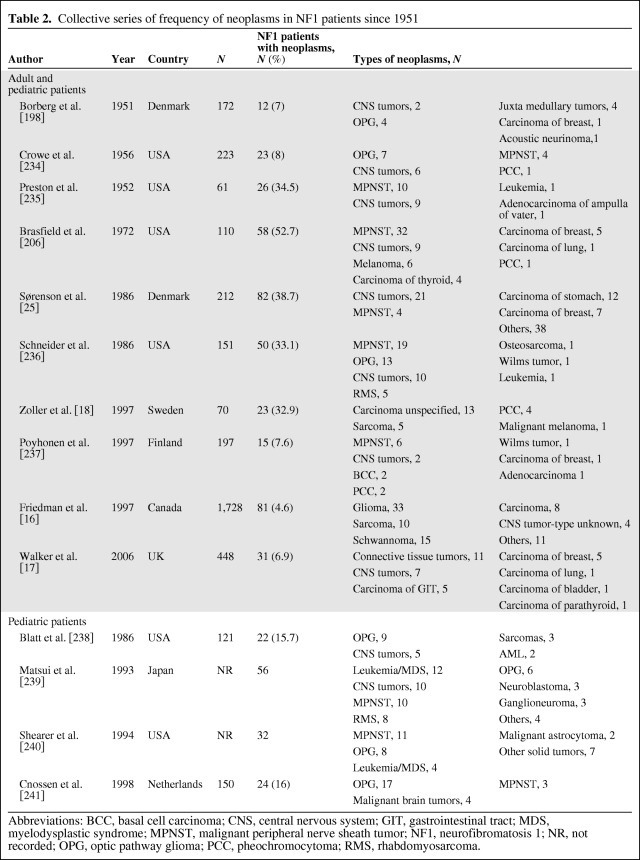
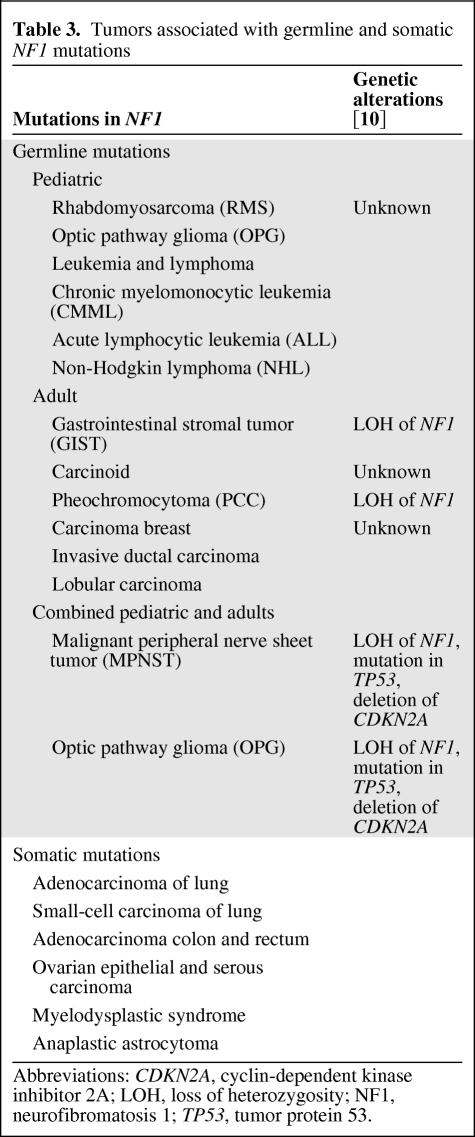
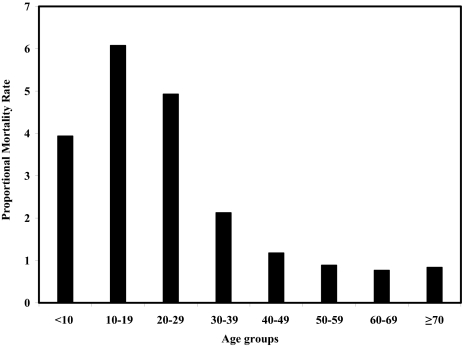
Patients with NF1 harbor an increased risk for developing both benign and malignant tumors. Overall, NF1 patients have 2.7-fold increased cancer risk with a cumulative risk of 20% in affected patients >50 years of age [16]. The incidence of malignancy varies between 4% and 52% in NF1 patients (Table 2) [17, 18]. Malignant peripheral nerve sheath tumors are the most common malignant tumors observed in NF1 patients [1, 19, 20]. Other malignant tumors strongly associated with NF1 patients include rhabdomyosarcoma, gastrointestinal stromal tumors, neuroectodermal tumors, pheochromocytomas, and breast carcinoma (Table 3) [20]. In addition to germline NF1 mutations, somatic alteration of the NF1 gene is also associated with sporadic malignancies such as small cell carcinoma of lung, adenocarcinoma of the colon and rectum, ovarian epithelial and serous carcinomas, myelodysplastic syndrome, and anaplastic astrocytoma (Table 3). Cancer is the most common cause of death in individuals affected with NF1 and results in a 10- to 15-year decreased life expectancy [7]. The proportional mortality due to malignancy in NF1 patients <40 years is more than twofold and for patients >40 years it is between 0.77 and 1.18 (Fig. 1) [7]. The proportional mortality for different age groups of NF1 patients is mainly dependent on variations in incidence of malignancies in those age groups. Overall malignant neoplasms occurred more frequently in NF1 patients <39 years of age compared with patients >40 years of age [7].
Table 2.
Collective series of frequency of neoplasms in NF1 patients since 1951
Abbreviations: BCC, basal cell carcinoma; CNS, central nervous system; GIT, gastrointestinal tract; MDS, myelodysplastic syndrome; MPNST, malignant peripheral nerve sheath tumor; NF1, neurofibromatosis 1; NR, not recorded; OPG, optic pathway glioma; PCC, pheochromocytoma; RMS, rhabdomyosarcoma.
Table 3.
Tumors associated with germline and somatic NF1 mutations
Abbreviations: CDKN2A, cyclin-dependent kinase inhibitor 2A; LOH, loss of heterozygosity; NF1, neurofibromatosis 1; TP53, tumor protein 53.
Figure 1.
Proportional mortality rate (PMR) was calculated for malignancy-related deaths in NF1 patients. There were 3,770 cases of presumed NF1 among 32,722,122 deaths in the United States between 1983 and 1997. Overall PMR for malignancy in NF1 patients was 1.21 (95% confidence interval [CI] 1.14–1.28). From the graph it can be seen that the PMR due to malignancy in NF1 patients aged under 40 years is >2 and for patients older than 40 years it is between 0.77 and 1.18. PMR is highest (6.07; 95% CI 4.88–7.45) for persons who died at 10–19 years of age, followed by (4.93; 95% CI 4.14–5.82) for those who died at 20–29 years of age [7].
Individuals with NF1 are heterozygous for an NF1 mutation, in the sense they have one normal and one mutated copy of the NF1 gene. Mutation in the normal copy of the NF1 gene (loss of heterozygosity, LOH) is a prerequisite for the development of malignancies in NF1 patients [21]. In addition to LOH, development of specific tumors typically requires additional genetic alterations (Table 3). In addition, the association between certain neoplasms and Neurofibromatosis 1 is based on observed increased prevalence in NF1 patients compared with the general population, but specific reasons explaining these associations are not clear. Furthermore, the reported prevalence of different neoplasms in the NF1 patients varies across different age groups and continents (Table 2). As discussed above, loss of heterozygosity in the NF1 gene certainly increases the risk of developing a neoplasm in NF1 patients but these mutations are also observed in some of the sporadic tumors. Hence it becomes difficult to ascertain a true relation between these tumor types with Neurofibromatosis 1, unless an additional mutation(s) specific for NF1 patients is identified.
Malignant Tumors Associated with NF1
Malignant Peripheral Nerve Sheath Tumors
Malignant peripheral nerve sheath tumors (MPNSTs; neurofibrosarcoma, neurogenic sarcoma, malignant neurolemmoma, malignant schwannoma, and anaplastic neurofibroma) are neurogenic sarcomas which can arise from any peripheral nerve cell (or cell showing nerve sheath differentiation), with the exception of tumors originating within the perineurium or the peripheral nerve vasculature [22]. MPNSTs can arise in any part of the body but are most common in the proximal portions of the upper and lower extremities and the trunk [23–25]. MPNSTs account for 3%–10% of all soft tissue sarcomas with 15% to 70% occurring in NF1 patients [26]. The incidence of MPNSTs in NF1 patients is 2%–29% compared with 0.001% in the general population [23, 27, 28]. The cumulative risk of developing MPNSTs in NF1 patients during their lifetime is 8%–13% and it remains the leading cause of death in this group [1]. MPNSTs in NF1 patients commonly arise from pre-existing plexiform neurofibromas and subcutaneous/spinal nerve root neurofibromas, but never within cutaneous neurofibroma [29]. The risk of developing MPNSTs is increased 3-fold in the presence of subcutaneous neurofibromas and 20-fold in the presence of internal plexiform neurofibromatosis [30]. From 10% to 50% of MPNSTs result from malignant transformation of plexiform neurofibromas [31, 32].
Pathologically, MPNSTs are spindle cell tumors that arise from Schwann cells. Mature Schwann cells stain positive on immunohistochemical stains for S-100 marker, but this staining may be absent in 50% of MPNSTs because of dedifferentiation [26]. In addition to LOH in NF1, mutations in TP53 and deletions of the CDKN2A genes are seen in the tumor cells of subgroups of patients with MPNSTs. NF1 microdeletions lead to twofold increased risk for developing MPNSTs [33]. Malignant triton tumors, MPNST with rhabdomyoblastic differentiation or other divergent differentiation, are rarely seen in NF1 patients [34]. MPNSTs often metastasize widely by a hematogenous route, heralding a poor prognosis [23, 29], and the most common sites of metastasis are the lung and bone [24, 35].
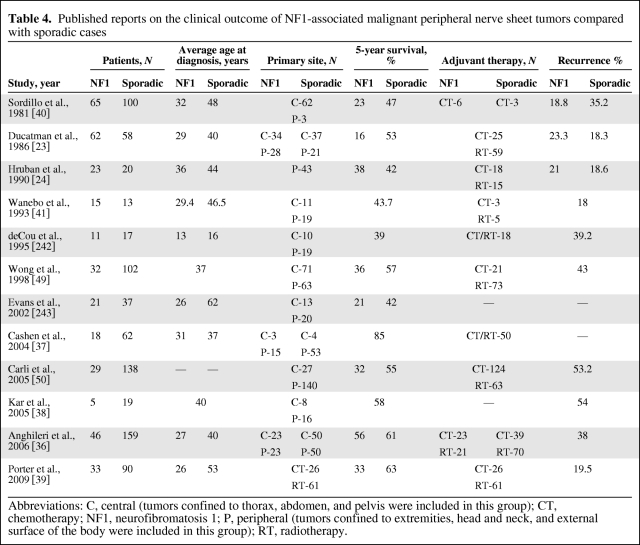
MPNSTs are found primarily in adults (in the third to sixth decade of life) and occurrence in childhood and adolescence is uncommon. The mean age of patients with NF1-associated MPNST is approximately a decade younger than that in sporadic cases (Table 4). The male/female ratio varies from 0.7:1 to 2.7:1 in different studies [23, 36–41]. The initial complaint is typically an enlarging mass or pain in the involved site [23, 24, 36, 42, 43]. Persistent pain that disturbs sleep, rapid increase in size, change in texture from soft to hard, and new or unexplained neurologic deficits should suggest malignant transformation of a pre-existing neurofibroma [29]. MPNSTs are difficult to diagnose as the clinical and radiologic features are shared by benign neurofibromas and plexiform neurofibromas. Accurate diagnosis can be made only by a combination of histopathologic and immunohistochemical evaluation [23]. Magnetic resonance (MR) imaging of MPNSTs typically shows a nonspecific heterogeneous mass with ill-defined margins with greater uptake of gallium-67 citrate compared with benign lesions [44]. Ferner et al. have shown that fluorine-18 labeled fluorodeoxyglucose-positron emission tomography (FDG-PET) has a sensitivity and specificity of 89% and 95% for the diagnosis of MPNSTs in NF1 patients. The mean SUV was 5.7 for MPNSTs compared with 1.5 for plexiform neurofibromas. No malignant tumors had an SUV <2.5 [45]. Those authors recommend that symptomatic neurofibromas with an SUV >3.5 should be excised and lesions with SUVmax between 2.5 and 3.5 should be followed with FDG-PET-CT every 3 months [45].
Table 4.
Published reports on the clinical outcome of NF1-associated malignant peripheral nerve sheet tumors compared with sporadic cases
Abbreviations: C, central (tumors confined to thorax, abdomen, and pelvis were included in this group); CT, chemotherapy; NF1, neurofibromatosis 1; P, peripheral (tumors confined to extremities, head and neck, and external surface of the body were included in this group); RT, radiotherapy.
The treatment and management principles of MPNSTs are similar to other soft tissue sarcomas [46]. Complete resection with negative resection margins (R0) is the treatment of choice. Resectability is dependent on anatomical location and ranges from 20% in paraspinal MPNST to 95% in tumors of the extremity [23, 24, 41, 47–49]. In a review of 134 patients (32 patients with NF1), Wong et al. reported a 5-year survival of 57% for patients in whom R0 resection was achieved compared with 22% for patients with a positive resection margins (R1). An international consensus statement on the management of MPNSTs in NF1 recommends adjuvant radiation therapy (RT) for all intermediate- to high-grade tumors and for all low-grade tumors with positive resection margins [49]. Chemotherapy (CT) is reserved for metastatic or unresectable tumors [29, 50]. In general, MPNSTs in NF1 have a poorer prognosis compared with sporadic cases [23, 27, 51–53]. The overall 5-year survival of patients with NF1-associated MPNSTs is in the range of 16%–38% compared with 42%–57% for sporadic cases (Table 4). MPNSTs are highly aggressive and achieving local control can be difficult [50] as they have the highest local recurrence rate of all sarcomas [54]. Local recurrence has been reported in 18.8%–21% of NF1 patients with MPNSTs (Table 4). Tumor size >5 cm, high tumor grade, central location of the tumors, and adjuvant radiation therapy are factors associated with poor prognosis on multivariate analysis [36].
Gastrointestinal Stromal Tumor
Gastrointestinal stromal tumors (GISTs) are the most common nonepithelial tumors of the gastrointestinal tract, accounting for 1%–3% of all gastrointestinal malignancies [55]. GISTs can arise from any part of the gastrointestinal tract; however, the most commonly affected site in NF1 patients is the small intestine compared with the stomach in the general population [56, 57]. Patients with NF1 are at 45-fold increased risk of developing GISTs compared with normal controls. The incidence of GIST in NF1 patients is 3.9%–25% compared with 10–13 per 100,000 in the general population [57, 58]. Most notably, the prevalence of NF1 in patients with GIST is up to 6% [57].
Pathologically, GISTs are mesenchymal tumors that arise from the interstitial cell of Cajal [59–61]. LOH of the NF1 gene, and mutation in the proto-oncogene c-kit which lead to increased expression of KIT and platelet-derived growth factor receptor-alpha (PGDFRA), are thought to be pivotal to GIST development. GISTs in NF1 patients have wild-type KIT receptors (type III tyrosine kinase receptor) that signal through the MAP kinase pathway [62] compared with PI3K-AKT cascade used by sporadic GISTs [63, 64]. The later finding points toward different pathogenesis and differential response to imatinib for GISTs associated with NF1. GISTs are classified into three histologic subtypes: (a) spindle cell type (70%), (b) epithelioid type (20%), and (c) mixed spindle cell and epithelioid cell type [65]. Spindle cell variety is more common in NF1-associated GISTs (80%) [56]. On immunohistochemical staining, 95% are positive for CD117, 70% for CD34, and 40% for smooth muscle actin [56]. GISTs spread by the hematogeneous route, with the most common sites of metastases being the liver, lung, peritoneum, and lymph nodes [66].
NF1 patients with GISTs tend to present at a younger age (median age 50 years) than sporadic cases (median age 55 to 65 years) [67]. The male:female ratio varies from 0.9:1 to 1:1.4 in different studies [55, 56, 58, 68]. GISTs are generally asymptomatic and only 5% present with symptoms [58]. The most common symptoms are nonspecific abdominal pain, bleeding, perforation, and rarely gastrointestinal obstruction (due to intraluminal growth, intussusception, and volvulus) [68–70]. Symptomatic patients tend to have high and intermediate risk tumors as well as distant metastasis at presentation [66]. There are no radiologic signs specific for GISTs, although on computed tomography they may appear as an inhomogeneous mass caused by areas of necrosis and hemorrhage with peripheral contrast enhancement of the viable tumor [71].
Information on therapeutic options in NF1 with GISTs is limited; published reports on management of sporadic GISTs suggest surgical resection as the treatment of choice for GISTs and biological therapy (imatinib) is recommended for patients with unresectable or metastatic disease, or in the adjuvant setting for high-risk GISTs [65]. Of note, as discussed below, imatinib is not considered standard for NF1 patients. In general, the surgical treatment of GIST involves a wedge resection of the involved gastric area or a segmental resection of the small intestinal tumors. More extensive resections may be required for tumors involving the esophagus, duodenum, or rectum [65]. Mussi et al. reported on a cohort of 28 NF1 patients with GISTs. Five patients (17.9%) in this group had metastasis at the time of diagnosis [66]. All patients underwent resection as initial treatment, two of whom had only debulking surgery in view of peritoneal metastasis. Four patients were treated with imatinib adjuvantly for high GISTs following R0 resection. The 5-year disease-specific survival and event-free survival were 54.3% and 46.9%, respectively. Response to imatinib was poor in this group. Three of the four patients exhibited progressive disease and only one achieved a temporary stabilization of disease. All four patients died of disease within 2 years of beginning therapy. Poor response of NF1-associated GISTs to imatinib therapy has been similarly documented by others [72, 73].
Rhabdomyosarcoma
Rhabdomyosarcoma (RMS) is a non-neurogenic sarcoma that accounts for almost 5% of all childhood cancers [74–76]. The prevalence of RMS in NF1-affected children is 1.4%–6%, which is 20-fold increased risk compared with non-NF1 children [77–81]. The urogenital system is the most common anatomic site involved [81].
Pathologically, RMS comprises small round blue cell tumors that arise from neural crest cells [82]. In addition to a LOH in NF1, mutations in TP53 and a t (2; 13) translocation corresponding to a PAX3-FKHR gene fusion and t (1; 13) translocation corresponding to a PAX7-FKHR gene fusion are recognized in the pathogenesis of RMS [83, 84].
RMS occurs most commonly in the pediatric NF1 patients with a male/female ratio of 1.5:1 [81]. RMS most commonly presents as a palpable mass or with symptoms reflecting the presence of a mass. There are no radiologic features specific for RMS and histopathology of the biopsied or resected specimen provides confirmative diagnosis.
The management of RMS has varied over the years and a detailed discussion of treatment is beyond the scope of this review. Two large study groups have recommended a conservative approach with surgery performed if the tumor can be resected without significant effect on cosmesis and function. Adjuvant chemotherapy and radiation may have a role in select patient groups [74, 85].
Carcinoid Tumor
Carcinoid tumors are neuroendocrine tumors arising from mucosal or submucosal endocrine cells, primarily within the gastrointestinal tract or lungs, but may also involve the mediastinum, thymus, bronchus, pancreas, liver, kidneys, testicles, ovaries, and prostate [86]. Carcinoids occur in 1% of NF1 patients, and involve the periampullary region almost exclusively [87, 88] with a prevalence of 27.5% compared with 2–3 per 100,000 in the general population [89–91]. Somatostatinoma is the most commonly reported subtype in NF1 patients, a majority of which (40%) are localized in the periampullary region [92, 93]. In NF1 patients carcinoids may be associated with adenocarcinomas [94], gastrointestinal stromal tumors [95, 96], and pheochromocytomas [97, 98]. This discussion will be limited to the diagnosis and management of periampullary carcinoids in NF1 patients.
Pathologically, carcinoids are enterochromafin and argentafin positive tumors derived from stem cells and orthotopic neuroendocrine cells of the epithelium of the respective organs [99]. A variety of genetic alterations are associated with carcinoids, most notably 18q and 11q chromosomal losses [86]. In particular, somatostatinomas are positive for neuron-specific enolase, chromogranin A, and synaptophysin on immunohistochemical staining [100].
NF1 patients with carcinoids typically are 21–70 years of age compared with 40–70 years of age in sporadic cases [91, 96]. NF1-associated carcinoids are more common in females (1:1.5) [96] and African Americans (87.5%) [87, 101, 102]. Periampullary carcinoids generally present with jaundice (65%) and nonspecific abdominal pain (31%) [103]. Less common clinical presentations include melena, iron deficiency anemia, gastrointestinal obstruction, cholangitis, and pancreatitis [86, 104, 105]. The occurrence of the somatostatinoma syndrome (diabetes, diarrhea, and gallstones) is extremely rare [106, 107]. Although clinical diagnosis is based on symptoms, biochemical confirmation is necessary [86]. Biochemical markers such as 5-hydroxy indolacetic acid (5-IHAA) and chromogranin A have high specificity and predictive value for diagnosing carcinoids [108]. Upper gastrointestinal endoscopy along with ERCP is helpful in the evaluation of biliary obstruction and determining the extent of common bile duct involvement. Biopsy of a suspicious lesion and sphincterotomy and stenting can be performed at the same time [90]. Endoscopic ultrasonography has a high sensitivity in localizing gastric or duodenal carcinoids and can detect lesions as small as 2–3 mm [109, 110]. CT scan and magnetic resonance (MR) imaging provide an important means for initial localization and detection of metastasis. Unfortunately, accurate preoperative diagnosis by endoscopic biopsy is achieved in only 15% of ampullary NETs [90]. The hallmark features of carcinoids on CT and MR imaging are the presence of radiating strands of fibrosis and spiculation, especially in the presence of a mass lesion [111]. Octreotide scan (Octreoscan) detects somatostatin receptor 2 (SSTR 2) and SSTR 5 positive carcinoids. The median tumor detection rate and sensitivity for Octreoscan are 89% and 84%, respectively, compared with 80% for CT and MR imaging [112]. In the evaluation of carcinoids FDG-PET-CT has been used in sporadic instances, but its clinical significance remains uncertain [113, 114].
The treatment of periampullary carcinoids is surgical resection whenever possible [95]. In carcinoids associated with NF1, pancreaticoduodenectomy was required in 60% of patients with a median survival of 14.5 months (range 4 to 60 months). The outcome of periampullary carcinoids in NF1 patients is less clear; so far, only 2 of the 32 published cases have reported a death in their patients during follow-up [95].
Pheochromocytoma
Pheochromocytoma (PCC) is a catecholamine-secreting tumor of the adrenal medulla or other sites within the sympathetic nervous system. NF1-associated PCC are solitary and unilateral in the majority of patients (84%), but may be bilateral (9.6%) or extraadrenal (6.1%) [115]. The incidence of PCC in NF1 patients is 0.1%–5.7% compared with 2–8 per 100,000 in the general population [115, 116]. Notably, the incidence of PCC increases up to 20%–50% in NF1 patients with hypertension [115]. PCC in NF1 patients is usually benign, and malignant PCC accounts for only 11.5% of reported cases [115]. In rare cases, composite tumors of pheochromocytoma and ganglioneuroblastoma or ganglioneuroma may occur in NF1 patients [117].
The mean age of presentation for NF1-associated PCC is 42 years compared with 47 years for sporadic cases with a male/female ratio of 1:1.4 [115, 118]. Symptoms related to PCC like headache, palpitations, diaphoresis, anxiety, and hypertension are seen in 61% of patients with NF1-associated PCC [115]. Diagnosis of PCC requires both biochemical confirmation and tumor localization using imaging modalities [119]. Plasma-free metanephrine level is the screening test of choice for PCC [120, 121]. Plasma metanephrine level of <61 ng/L excludes PCC, whereas values >236 ng/L confirm the diagnosis of PCC and values between 6 and 236 ng/L require additional testing [122]. In the evaluation of PCC, plasma-free metanephrines, plasma total metanephrines, and urinary fractionated metanephrines have equal sensitivity and specificity [123]. Most cases of PCC show high attenuation values (>10 Hounsfield units) on CT scan, with hyperintensity on T2 MRI and gadolinium contrast enhancement on T1 MRI [124]. The sensitivity and specificity of CT and MR imaging in localizing PCC range from 88% to 100% and from 96% to 100%, respectively [124–126]. 131I-metaiodobenzylguanidine (MIBG) scintigraphy is shown to have a higher specificity but lower sensitivity compared with MR imaging [127]. 18F-labeled dihydroxyphenylalanine (18F-DOPA) PET scan is a newer diagnostic technique with sensitivity similar to that of MR imaging and specificity of 100% in localizing PCC [127].
Surgery is curative for benign PCC with a 5-year survival of 95% [128]. Chemotherapy may be indicated for patients with metastatic pheochromocytoma, but its efficacy is not supported by large randomized controlled trials [129]. Malignant PCC has an unpredictable outcome; approximately half of these patients exhibit a rapid downhill course with death due to disease within 4–5 years [130]. However, the remaining patients have an indolent course with an occasional patient surviving >20 years even in the absence of cytotoxic therapy [130]. Chemotherapy with cyclophosphamide, vincristine, and dacarbazine (CVD) is associated with an overall 5-year survival of ∼50% with a complete response rate of 11% and a partial response rate of 44% in the setting of metastases [130]. Radiopharmaceutical therapy with 131I-MIBG results in a 75% to 90% symptomatic response with tumor response rates in the range of 30% to 47% [131]. The role of additional therapeutic modalities such as radiation therapy, cryoablation, radiofrequency ablation, and transcatheter arterial embolization is investigational [128].
Optic Pathway Gliomas
Optic pathway gliomas (OPGs) are the most common intracranial tumors in patients with NF1 [132]. Although these tumors may arise anywhere along the optic pathway, the most common site in NF1 patients is the anterior optic pathway compared with the posterior optic pathways in sporadic cases [133–135]. Optic pathway tumors account for nearly 2%–5% of all brain tumors in the pediatric population with 70% of these occurring in patients with NF1 [132]. The prevalence of OPGs in NF1 patients varies widely from 1.55% reported in a population-based study [136] to 58% seen in some referral centers [137–142]. The incidence of OPGs in NF1 patients is probably between 1.5% and 7.5% [132]. NF1-associated OPGs that typically demonstrate indolent clinical behavior [143–147] generally manifest early in childhood and rarely grow or cause symptoms after the first decade of life [148–151].
Pathologically, OPGs are low-grade pilocytic astrocytomas with low growth potential possibly arising from small clusters of proliferating immature progenitors. NF1 inactivation in the progenitor cells is thought to play a major role in the development of these tumors [152–154]. OPGs are positive for astroglial progenitor cell markers (brain lipid-binding protein and nestin) along with glial fibrillary acidic protein (GFAP) on immunohistochemical stains [152–154].
NF1 patients <6 years of age are at the greatest risk for developing OPGs; however, presentation in adulthood has been reported [132, 148]. The male/female ratio varies from 1.6:1 to 2:1 [133, 139]. The majority (50%–75%) of patients are asymptomatic at the time of diagnosis [134, 139]. Nearly 8%–52% of OPGs show either clinical or radiologic progression after their initial diagnosis [155]. The progression usually occurs within 2 years of initial diagnosis [155]. On the other hand, progression of tumor has been noted to occur as late as 5 years after initial diagnosis [156]. Grill et al. observed 20 (18.8%) patients with clinically silent optic pathway glioma, of which 12 (11.8%) patients developed progressive disease within 16.5 months, warranting treatment [146]. Clinical presentation depends on the location and extent of the tumor with intraorbital tumors presenting with proptosis, and optic chiasm and hypothalamic tumors presenting with vision loss and precocious puberty [134, 139, 157–160]. The most common clinical signs in NF1 patients are decreased visual acuity, decreased visual fields, and proptosis [161, 162]. In view of the indolent and unpredictable course of OPGs, it is difficult to recommend specific investigational schema or management strategy applicable to all patients [155]. The majority of OPGs display a stable course, but some may undergo rapid progression or spontaneous or biopsy-related regression with or without clinical improvement [143, 149, 163, 164]. Although a few authors have proposed diagnostic and management algorithms for OPGs, their clinical utility is not fully established [20, 150]. Annual systematic ophthalmologic examination until age 6, and at longer intervals thereafter, is indicated in all children diagnosed with NF1 [132]. Routine screening with radiologic imaging is not indicated as incidentally discovered OPGs rarely require treatment [165]. Visual-evoked potential (VEP) is recommended as a good screening tool by some authors and has a sensitivity and specificity of 76% and 86% for diagnosing OPGs, although its use is discouraged by “Consensus Statement from the NF1 Optic Pathway Glioma task Force (1997)” [166, 167]. Flicker VEP (F-VEP) and Sweep VEP are two modifications of the standard VEP, which may offer increased information about the neurophysiologic status of patients with OPGs. Agreement between F-VEP and MRI changes is approximately 78.9% (p <.001) [166]. Falsini et al. have recommended that F-VEP be used for both screening and in follow-up of all patients with OPGs [166].
Symptomatic lesions that cause visual impairment, hypothalamic dysfunction, and hydrocephalus should be treated [168]. Treatment options for patients younger than 7 years include either surgery or chemotherapy with radiotherapy reserved for patients >10 years. Treatment recommendations for patients between 7 and 10 years old are controversial [156]. The selection of appropriate management strategy for each individual patient should be based on tumor location, histology, and evolution, and also patient age [140]. Surgery offers a definitive cure for most intraorbital and anterior optic pathway tumors, whereas resection of the posterior optic pathway tumors is associated with high rates of recurrence and/or progression [140]. Noncurative debulking surgery is undertaken to preserve visual function in rapidly growing tumors, to obtain quick relief of raised intracranial pressure (ICP) and in cases where adjuvant therapies are ineffective [169]. Marsupialization of cystic tumor into the ventricular system or CSF shunting may also be performed when tumors are associated with high ICP [169]. Deliganis et al. reported on 16 patients with NF1-associated OPGs: 5 patients were managed conservatively, 1 patient was treated with surgery alone, and 10 patients were treated with radiation therapy with or without surgery. The 5-, 10-, and 15-year survival rates were 93%, 81%, and 81%, respectively [170]. In a similar study, Thiagalingam et al. reported on 17 patients with NF1-associated OPGs. Five patients were treated with surgery, 7 patients with radiation therapy, 2 patients with chemotherapy, and 3 patients with combined therapy. Post-treatment, 53.7% of patients had mild or no visual impairment, 14.8% had moderate impairment, and 31.5% had severe impairment in their worse eye. The majority of patients expressed only mild or no impairment in the better eye (83.3%) [162]. At present, chemotherapy has replaced radiation therapy as a first-line treatment for evolving or slow-growing OPGs [169]. Carboplatin and vincristine are the most commonly used chemotherapeutic agents, with overall response rates between 25% and 73% [132, 155, 156, 169]. Additional chemotherapeutic agents have been used for the treatment of OPGs, including temozolomide, procarbazine, vincristine, 6-thioguanine, and chloroethylcyclohexylnitrosourea (CCNU; lomustine). However, the use of alkylating agents and multidrug regimens in children with NF1 runs the theoretical risk for the development of secondary malignancies [169, 171, 172]. Between 31% and 42.8% of tumors fail to respond to chemotherapy, with treatment failure more common among the posterior OPGs [173, 174]. Radiation therapy is mainly indicated for progressive or recurrent OPGs in patients >10 years of age [169]. The long-term adverse effects of radiation therapy include learning disabilities, growth retardation, radiation-induced neoplasms, optic neuropathy, precocious puberty, and delayed vascular occlusion [146, 175–177]. These effects are particularly common in infants and young (<7 years) children, hence, the caveat to restrict radiation to patients older than 10 years [169]. OPGs are extremely radiation-sensitive and tumor control is achievable in 80%–90% of patients [146] and a 3-year progression-free survival is achievable in 70%–100% of patients [169].
Brainstem Gliomas
Brainstem gliomas are the second most common intracranial tumors in patients with NF1 [148]. Brainstem gliomas account for nearly 15%–20% of all brain tumors in the pediatric population and the incidence varies from 4% to 20% in NF1 patients [178, 179]. The medulla oblongata (68%) is the most common site in NF1 patients compared with the pons in sporadic cases (80%) [180, 181]. NF1-associated brainstem gliomas typically demonstrate an indolent clinical behavior compared with sporadic cases [181, 182].
Diffusely infiltrating astrocytomas (21%) are the most common brainstem astrocytomas in NF1 patients, followed by low-grade astrocytomas of indeterminate type (17%) and pilocytic astrocytomas (12%) [183]. Neurofibromin, a protein product of NF1 gene, inhibits proliferation of astrocytes directly and through negative regulation of p21-ras protein. Hence, loss of heterozygosity of the NF1 gene results in increased proliferation of astrocytes [184].
The mean age at the diagnosis of brainstem gliomas in NF1 patients is 7.8–8.4 years (<1 month to 17 years); however, presentation in adulthood has been reported [180, 185, 186]. The male/female ratio varies from 2.1:1 to 3.3:1 [180, 185]. The majority (52.3%–76.4%) of patients are symptomatic at presentation, with headache being the most common symptom (36%–53%) [180, 185, 187]. Neurologic signs depend on the lesion location; however, gross motor abnormality, cranial neuropathies, and dysarthria are most common [180, 185].
Similar to OPGs, the majority of brainstem gliomas display a stable course, but some may undergo rapid progression or spontaneous regression. Although clinical progression occurs in only 14.3%–17.6% of NF1 patients with brainstem gliomas, radiologic progression is observed in 35.3%–42.9% [180, 185]. Pollack et al. have recommend a baseline neuroimaging study in all NF1 patients before the age of 5 years with a repeat study after 2–3 years if the child is too young for detailed evaluation [187]. Note that it is probably not cost-effective to perform neuroimaging in all NF1 patients, as only 9.1% of patients will harbor occult intracranial lesions that require further surgery [187]. Once a brainstem mass is identified, a neurologic examination every 3 months with biannual neuroimaging for the first year to rule out tumor progression or hydrocephalus is indicated. Subsequent neurologic examination and neuroimaging should be performed annually [185].
Gliomas that exhibit rapid growth, become symptomatic, or demonstrate contrast enhancement on neuroimaging should be treated [179, 182]. Treatment of NF1-associated brainstem glioma and sporadic brainstem glioma is no different. Accessible lesions, such as dorsally exophytic brainstem tumors, cervicomedullary junction lesions, and superficial tegmental lesions are treated with surgical resection. Tumors deemed unresectable, or in the event of tumor recurrence, may be treated with whole brain or stereotactic radiotherapy. Chemotherapy has modest efficacy for unresectable low-grade gliomas and may be preferable as initial treatment for patients younger than 5 years. A variety of regimens have been utilized (e.g., vincristine-actinomycin D, carboplatinum-vincristine, and 6-thioguanine-procarbazine-dibromodulcitol-CCNU-vincristine) with tumor response rates of 20%–80% and response or stabilization rates of 75%–100% [187].
Molloy et al. reported on 17 NF1 patients with brainstem gliomas: 10 (58.8%) patients were managed conservatively, 7 (41.2%) required placement of a ventriculoperitoneal shunt, and 2 (11.8%) underwent partial resection of a medulary tumor. Only three NF1 patients (17%) received chemotherapy and/or radiation. This group experienced an 11.8% mortality (N = 2) and a 5.8% (N = 1) tumor progression rate at a mean follow-up of 63 months [185]. In a separate study of 21 NF1 patients with brainstem glioma, 12 (57%) NF1 patients had symptomatic lesions, of which 5 (23.8%) required a ventriculoperitoneal shunt and 7 (33.3%) were managed expectantly. There were no mortalities in this group at a follow-up of 3.7 years [187].
Although brainstem gliomas associated with NF1 are known to have better outcomes compared with sporadic brainstem gliomas, 5- and 10-year mortality rates as high as 30% and 37%, respectively, have been reported [183]. Age <10 years, asymptomatic tumors, diffusely infiltrating astrocytomas, focally enhancing tumors, and a tectal location are indicators of good prognosis [148, 183, 187].
Leukemia
Children with NF1 have a 500-fold increased risk of developing myeloid malignancies compared with the general population [188]. In a population-based study, Stiller et al. reported a 200-fold increased risk of chronic myelomonocytic leukemia (CMML)/juvenile chronic myelogenous leukemia (JCML) in children, a 5-fold increased risk for non-Hodgkin lymphoma (NHL), and a 10-fold increased risk for acute lymphocytic leukemia (ALL) across all the NF1-affected age groups [189]. Bader et al. reported reversal of the ratio between ALL and nonlymphocytic leukemia from 4:1 in the general population to 9:20 in patients with NF1 [190]. Rare subtypes like chronic myelogenous leukemia (CML) and acute myelomonocytic (AMML) are also commonly seen in NF1 patients [190].
In at least half of affected NF1 patients, LOH of the NF1 gene is detected, resulting in uncontrolled activation of the ras signal transduction pathway [188, 191]. NF1 is a tumor suppressor gene whose product negatively regulates ras signal transduction. Ras signaling pathway activation by point mutation in the RAS gene is a common event in acute myeloid malignancies and may account for the increased leukemia in NF1 patients [192–197].
The average age of NF1 children at the time of diagnosis was 32 months for JCML, 86 months for ALL, and 79 months for NHL, with a male/female ratio of 1.6:1 [189]. The median survival was 5 months for NF1-associated JCML, 52 months for ALL, and 13.5 months for NHL. Notably, the prognosis of NF1-associated leukemia and NF1-associated NHL does not differ from that of sporadic cases [189].
Carcinoma Breast
Breast carcinoma among NF1 patients was reported by Borberg et al. in 1951 [198]; since then, several additional cases have been reported, mostly from Japan. There is a paucity of information on this topic in the English language; Murayama et al. have reported on 34 NF1 patients with 38 breast cancers [199]. Sørensen et al. reported 57 non-neurologic malignancies in a cohort of 212 patients with NF1 [25]. In this later cohort, breast cancer was the second most common malignancy (7 out of 57, 12.3%) after gastric cancer (12 out of 57, 21.1%) [25]. In a population-based study, Sharif et al. reported a standardized incidence ratio (SIR) of 3.5 (95% CI 1.9–5.9) for carcinoma breast among NF1 patients [200].
NF1-associated breast cancer occurs more commonly in a younger age group compared with the general population. Nakamura et al. reported that 18.5% of NF1-associated breast cancer occurred in patients <30 years old, which is more than twice the number of patients with breast cancer of a similar age group in the general population [201]. A similar increased incidence in younger patients was observed by Sharif et al. with a calculated standardized incidence ratio (SIR) of 4.9 (95% CI 2.4–8.8) for patients <50 years of age [200]. So far, only a single case of male breast cancer in an NF1 patient has been reported [202]. In view of earlier age of onset and the clinical difficulty in differentiating a breast lump from a cutaneous or subcutaneous neurofibroma, it is recommended that all NF1 patients begin early screening and follow-up in specialized centers.
The locus for BRCA1 on chromosome 17 is at a distance of only 20 cM from the NF1 locus. This finding may account for the increased incidence of breast carcinoma in NF1 patients [203]. Ceccaroni et al. were the first to demonstrate BRCA1 mutations in a case of NF1-associated breast cancer [203]. Guran et al. have demonstrated LOH for NF1 in a case of NF1-associated breast cancer, but failed to identify a BRCA mutation [204]. In the United Kingdom, the most commonly reported histologic subtypes of NF1-associated breast cancer are invasive ductal carcinoma (77.8%), lobular carcinoma (16.7%), and ductal carcinoma in situ (5.6%) [200], whereas in Japan the most commonly reported histologic subtypes are invasive ductal carcinoma (84.2%), mucinous carcinoma (7.9%), lobular (2.6%), squamous cell carcinoma (2.6%), and ductal carcinoma in situ (2.6%) [201].
The treatment of breast cancer in NF1 patients does not differ from sporadic forms and it is beyond the scope of this review to discuss treatment further. In view of the rarity of this entity and paucity of data in the English literature, it is difficult to comment on the outcome of NF1-associated breast cancer. Stagé et al. have reported a recurrence-free survival of 14 years following mastectomy for a patient with NF1-associated grade II intraductal breast cancer [205]. On the other hand, Brasfield et al. reported on five female NF1 patients with breast cancer and all five died from breast cancer within 5 years of the diagnosis [206].
Additional NF1-Associated Malignancies
Several other malignancies such as adenocarcinoma of the esophagus [207], stomach [208], colon [209, 210], small intestine [211–216], pancreas [216, 217], gall bladder [218], and bile ducts [219], as well as melanoma [220, 221], Wilm's tumor [222, 223], neuroblastoma [101, 224], and thyroid carcinoma [206] have been reported in patients with NF1. It is difficult to ascertain which of these are random occurrences or may represent true associations with NF1. However, the increased prevalence of these tumors in the general population compared with NF1 patients suggests an incidental finding. Having said that, adenocarcinoma of the small intestine in patients with NF1 may be an exception given the large number of reported cases among NF1 patients [214]. The majority of small intestinal adenocarcinoma occurring in patients with NF1 are periampullary in location and this was discussed previously [212, 214]. Williams et al. have suggested that any association between adenocarcinoma of the small intestine and NF1 is tenuous at best given the established association between carcinoids and NF1 and the difficulty in distinguishing between adenocarcinoma and carcinoids histopathologically [225].
Somatic NF1 Mutations
Mutations involving the NF1 gene in somatic cells have been demonstrated in a variety of solid tumors. However, none of the mutation types are specific for a group of tumors or a particular tumor type. Although mutations in the somatic NF1 gene locus have been found, the cause and effect relationship has not been established; rather, there is a suggestion of an interplay of this mutation with other genetic and environmental factors that may lead to an increased risk of tumor development. Table 3 summarizes the common somatic NF1 tumors reported. In a pilot project to characterize cancer genomes, Ding et al. conducted mutation analysis in 188 primary lung adenocarcinomas [226]. Among the 26 significantly mutated genes associated with adenocarcinoma of the lung, 16 mutations involved the NF1 gene in 13 tumors. There were 4 nonsense mutations, 5 splice-site mutations, and 1 frame shift mutation in the NF1 coding region [226]. Reports on the type of mutation involving NF1 in colorectal adenocarcinoma vary widely; LOH involving NF1 gene may occur in 14%–57% of colorectal carcinomas [227, 228]. Alhiquist et al. have reported a gain in parts of or even complete duplication of the NF1 gene in 17% of colorectal carcinomas [229]. Similarly, Cacev et al. has also reported significant increase in the expression of NF1 mRNA in colorectal tumors compared with normal tissue [230]. In a separate study, Furukawa et al. analyzed 37 patients with primary lung cancer and identified NF1 mutations in three patients, all of which had small cell lung carcinoma. All three mutations identified were located in the GTPase-activating protein (GAP)-related domain (GRD) close to the mutational hot spot within exon 24 [231]. Li et al. have reported three cases of adenocarcinoma of the colon, myelodysplastic syndrome, and anaplastic astrocytoma, which also had NF1 mutations involving the GRD domain [232]. Finally, Sangha et al. reported reduced to absent NF1 in 5 out of 18 ovarian epithelial cancer cell lines and 9 out of 41 primary ovarian serous carcinomas [233].
Conclusions
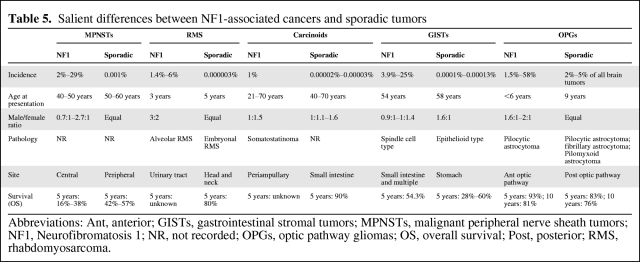
Neurofibromatosis 1 is a tumor predisposition genetic syndrome with autosomal dominant inheritance and virtually 100% penetrance by the age of 5 years. NF1 results from a loss-of-function mutation in the NF1 gene resulting in decreased levels of neurofibromin in the cell. Neurofibromin is a negative regulator of various intracellular signaling pathways involved in the proliferation of cell. Although a loss-of-function mutation in the NF1 gene, especially LOH, may predispose NF1 patients to certain malignancies, additional genetic alterations are a prerequisite for malignant transformation. The precise nature of these additional genetic alterations is not well defined, which mandates genetic testing of all malignancies detected in NF1 patients. In addition to the germ line NF1 mutations, alteration of the somatic NF1 gene has also been associated with sporadic malignancies such as adenocarcinoma of the colon, myelodysplastic syndrome, and anaplastic astrocytoma. Malignancies in NF1 patients typically occur at an earlier age and, with an exception of OPGs, carry a poor prognosis compared with the general population (Table 5). Cancer is the leading cause of death among NF1 patients, resulting in a 10- to 15-year decreased life expectancy compared with the general population. The lack of well-defined screening tests for early detection and the nonspecific clinical presentation contribute to the poor outcome in NF1-associated malignancies. Small study group size, mixed patient population, and a lack of uniformity in reporting research results make comparison of treatment outcome for this group difficult. An International Consensus Meeting to address and recommend best practices for the screening, diagnosis, management, and follow-up of malignancies associated with NF1 is needed.
Table 5.
Salient differences between NF1-associated cancers and sporadic tumors
Abbreviations: Ant, anterior; GISTs, gastrointestinal stromal tumors; MPNSTs, malignant peripheral nerve sheath tumors; NF1, Neurofibromatosis 1; NR, not recorded; OPGs, optic pathway gliomas; OS, overall survival; Post, posterior; RMS, rhabdomyosarcoma.
Footnotes
- (C/A)
- Consulting/advisory relationship
- (RF)
- Research funding
- (E)
- Employment
- (H)
- Honoraria received
- (OI)
- Ownership interests
- (IP)
- Intellectual property rights/inventor/patent holder
- (SAB)
- Scientific advisory board
Author Contributions
Conception/Design: Ronald Chamberlain
Provision of study material or patients: Sachin Patil
Collection and/or assembly of data: Sachin Patil
Data analysis and interpretation: Sachin Patil
Manuscript writing: Sachin Patil
Final approval of manuscript: Ronald Chamberlain
References
- 1.Rasmussen SA, Friedman JM. NF1 gene and neurofibromatosis 1. Am J Epidemiol. 2000;151:33–40. doi: 10.1093/oxfordjournals.aje.a010118. [DOI] [PubMed] [Google Scholar]
- 2.Riccardi VM, Lewis RA. Penetrance of von Recklinghausen neurofibromatosis: a distinction between predecessors and descendants. Am J Hum Genet. 1988;42:284–289. [PMC free article] [PubMed] [Google Scholar]
- 3.Riccardi VM. Baltimore: John Hopkins University Press; 1992. Neurofibromatosis: phenotype, natural history, and pathogenesis. [Google Scholar]
- 4.Neurofibromatosis. [Accessed March 15, 2010];NIH Consens Statement Online. 1987 6:1–19. [Google Scholar]
- 5.Crowe FW. Axillary freckling as a diagnostic aid in Neurofibromatosis. Ann Intern Med. 1964;61:1142–1143. doi: 10.7326/0003-4819-61-6-1142. [DOI] [PubMed] [Google Scholar]
- 6.Korf BR. Clinical features and pathobiology of neurofibromatosis 1. J Child Neurol. 2002;17:573–577. doi: 10.1177/088307380201700806. [DOI] [PubMed] [Google Scholar]
- 7.Rasmussen SA, Yang Q, Friedman JM. Mortality in neurofibromatosis 1: an analysis using U.S. death certificates. Am J Hum Genet. 2001;68:1110–1118. doi: 10.1086/320121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010;12:1–11. doi: 10.1097/GIM.0b013e3181bf15e3. [DOI] [PubMed] [Google Scholar]
- 9.Ars E, Kruyer H, Morell M, et al. Recurrent mutations in the NF1 gene are common among neurofibromatosis type 1 patients. J Med Genet. 2003;40:e82. doi: 10.1136/jmg.40.6.e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brems H, Beert E, de Ravel T, et al. Mechanisms in the pathogenesis of malignant tumours in neurofibromatosis type 1. Lancet Oncol. 2009;10:508–515. doi: 10.1016/S1470-2045(09)70033-6. [DOI] [PubMed] [Google Scholar]
- 11.Dilworth JT, Kraniak JM, Wojtkowiak JW, et al. Molecular targets for emerging anti-tumor therapies for neurofibromatosis type 1. Biochem Pharmacol. 2006;72:1485–1492. doi: 10.1016/j.bcp.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Gottfried ON, Viskochil DH, Fults DW, et al. Molecular, genetic, and cellular pathogenesis of neurofibromas and surgical implications. Neurosurgery. 2006;58:1–16. doi: 10.1227/01.neu.0000190651.45384.8b. [DOI] [PubMed] [Google Scholar]
- 13.Ismat FA, Xu J, Lu MM, et al. The neurofibromin GAP-related domain rescues endothelial but not neural crest development in Nf1 mice. J Clin Invest. 2006;116:2378–2384. doi: 10.1172/JCI28341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trovó-Marqui AB, Tajara EH. Neurofibromin: a general outlook. Clin Genet. 2006;70:1–13. doi: 10.1111/j.1399-0004.2006.00639.x. [DOI] [PubMed] [Google Scholar]
- 15.Denayer E, de Ravel T, Legius E. Clinical and molecular aspects of RAS related disorders. J Med Genet. 2008;45:695–703. doi: 10.1136/jmg.2007.055772. [DOI] [PubMed] [Google Scholar]
- 16.Friedman JM, Birch PH. Type 1 neurofibromatosis: a descriptive analysis of the disorder in 1,728 patients. Am J Med Genet. 1997;70:138–143. doi: 10.1002/(sici)1096-8628(19970516)70:2<138::aid-ajmg7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Walker L, Thompson D, Easton D, et al. A prospective study of neurofibromatosis type 1 cancer incidence in the UK. Br J Cancer. 2006;95:233–238. doi: 10.1038/sj.bjc.6603227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zöller ME, Rembeck B, Oden A, et al. Malignant and benign tumors in patients with neurofibromatosis type 1 in a defined Swedish population. Cancer. 1997;79:2125–2131. [PubMed] [Google Scholar]
- 19.Carroll SL, Ratner N. How does the Schwann cell lineage form tumors in NF1? Glia. 2008;56:1590–1605. doi: 10.1002/glia.20776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yohay K. Neurofibromatosis type 1 and associated malignancies. Curr Neurol Neurosci Rep. 2009;9:247–253. doi: 10.1007/s11910-009-0036-3. [DOI] [PubMed] [Google Scholar]
- 21.Ruggieri M, Packer RJ. Why do benign astrocytomas become malignant in NF1? Neurology. 2001;56:827–829. doi: 10.1212/wnl.56.7.827. [DOI] [PubMed] [Google Scholar]
- 22.Woodruff JM, Kourea HP, Louis DN, et al. Malignant peripheral nerve sheath tumour (MPNST) In: Kleihues P, Cavenee WK, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Nervous System. Lyon, France: IARC Press; 2000. pp. 172–174. [Google Scholar]
- 23.Ducatman BS, Scheithauer BW, Piepgras DG, et al. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986;57:2006–2021. doi: 10.1002/1097-0142(19860515)57:10<2006::aid-cncr2820571022>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 24.Hruban RH, Shiu MH, Senie RT, et al. Malignant peripheral nerve sheath tumors of the buttock and lower extremity. A study of 43 cases. Cancer. 1990;66:1253–1265. doi: 10.1002/1097-0142(19900915)66:6<1253::aid-cncr2820660627>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 25.Sørensen SA, Mulvihill JJ, Nielsen A. Long-term follow-up of von Recklinghausen neurofibromatosis. Survival and malignant neoplasms. N Engl J Med. 1986;314:1010–1015. doi: 10.1056/NEJM198604173141603. [DOI] [PubMed] [Google Scholar]
- 26.Bhattacharyya AK, Perrin R, Guha A. Peripheral nerve tumors: management strategies and molecular insights. J Neurooncol. 2004;69:335–349. doi: 10.1023/b:neon.0000041891.39474.cb. [DOI] [PubMed] [Google Scholar]
- 27.Das Gupta TK, Brasfield RD. Solitary malignant schwannoma. Ann Surg. 1970;171:419–428. doi: 10.1097/00000658-197003000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riccardi VM, Powell PP. Neurofibrosarcoma as a complication of von Recklinghausen neurofibromatosis. Neurofibromatosis. 1989;2:152–165. [PubMed] [Google Scholar]
- 29.Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res. 2002;62:1573–1577. [PubMed] [Google Scholar]
- 30.Tucker T, Wolkenstein P, Revuz J, et al. Association between benign and malignant peripheral nerve sheath tumors in NF1. Neurology. 2005;65:205–211. doi: 10.1212/01.wnl.0000168830.79997.13. [DOI] [PubMed] [Google Scholar]
- 31.Mrugala MM, Batchelor TT, Plotkin SR. Peripheral and cranial nerve sheath tumors. Curr Opin Neurol. 2005;18:604–610. doi: 10.1097/01.wco.0000179507.51647.02. [DOI] [PubMed] [Google Scholar]
- 32.Upadhyaya M, Han S, Consoli C, et al. Characterization of the somatic mutational spectrum of the neurofibromatosis type 1 (NF1) gene in neurofibromatosis patients with benign and malignant tumors. Hum Mutat. 2004;23:134–146. doi: 10.1002/humu.10305. [DOI] [PubMed] [Google Scholar]
- 33.De Raedt T, Brems H, Wolkenstein P, et al. Elevated risk for MPNST in NF1 microdeletion patients. Am J Hum Genet. 2003;72:1288–1292. doi: 10.1086/374821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singer S, Corson JM, Demetri GD, et al. Prognostic factors predictive of survival for truncal and retroperitoneal soft-tissue sarcoma. Ann Surg. 1995;221:185–195. doi: 10.1097/00000658-199502000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiss SW, Goldblum JR. Soft Tissue Tumors. 4th ed. St. Louis: Mosby; 2001. Malignant tumors of the peripheral nerves; pp. 1209–1265. [Google Scholar]
- 36.Anghileri M, Miceli R, Fiore M, et al. Malignant peripheral nerve sheath tumors: prognostic factors and survival in a series of patients treated at a single institution. Cancer. 2006;107:1065–1074. doi: 10.1002/cncr.22098. [DOI] [PubMed] [Google Scholar]
- 37.Cashen DV, Parisien RC, Raskin K, et al. Survival data for patients with malignant schwannoma. Clin Orthop Relat Res. 2004;(426):69–73. doi: 10.1097/01.blo.0000131256.82455.c5. [DOI] [PubMed] [Google Scholar]
- 38.Kar M, Deo SV, Shukla NK, et al. Malignant peripheral nerve sheath tumors (MPNST)–clinicopathological study and treatment outcome of twenty-four cases. World J Surg Oncol. 2006;4:55. doi: 10.1186/1477-7819-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Porter DE, Prasad V, Foster L, et al. Survival in malignant peripheral nerve sheath tumours: a comparison between sporadic and neurofibromatosis type 1-associated tumours. Sarcoma. 2009;2009 doi: 10.1155/2009/756395. 756395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sordillo PP, Helson L, Hajdu SI, et al. Malignant schwannoma–clinical characteristics, survival, and response to therapy. Cancer. 1981;47:2503–2509. doi: 10.1002/1097-0142(19810515)47:10<2503::aid-cncr2820471033>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 41.Wanebo JE, Malik JM, VandenBerg SR, et al. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 28 cases. Cancer. 1993;71:1247–1253. doi: 10.1002/1097-0142(19930215)71:4<1247::aid-cncr2820710413>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 42.D'Agostino AN, Soule EH, Miller RH. Sarcomas of the peripheral nerves and somatic soft tissues associated with multiple neurofibromatosis (Von Recklinghausen's Disease) Cancer. 1963;16:1015–1027. doi: 10.1002/1097-0142(196308)16:8<1015::aid-cncr2820160808>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 43.King AA, Debaun MR, Riccardi VM, et al. Malignant peripheral nerve sheath tumors in neurofibromatosis 1. Am J Med Genet. 2000;93:388–392. [PubMed] [Google Scholar]
- 44.Murphey MD, Smith WS, Smith SE, et al. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999;19:1253–1280. doi: 10.1148/radiographics.19.5.g99se101253. [DOI] [PubMed] [Google Scholar]
- 45.Ferner RE, Golding JF, Smith M, et al. [18F]2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG PET) as a diagnostic tool for neurofibromatosis 1 (NF1) associated malignant peripheral nerve sheath tumours (MPNSTs): a long-term clinical study. Ann Oncol. 2008;19:390–394. doi: 10.1093/annonc/mdm450. [DOI] [PubMed] [Google Scholar]
- 46.Nambisan RN, Rao U, Moore R, et al. Malignant soft tissue tumors of nerve sheath origin. J Surg Oncol. 1984;25:268–272. doi: 10.1002/jso.2930250410. [DOI] [PubMed] [Google Scholar]
- 47.Kourea HP, Bilsky MH, Leung DH, et al. Subdiaphragmatic and intrathoracic paraspinal malignant peripheral nerve sheath tumors: a clinicopathologic study of 25 patients and 26 tumors. Cancer. 1998;82:2191–2203. doi: 10.1002/(sici)1097-0142(19980601)82:11<2191::aid-cncr14>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 48.Vege DS, Chinoy RF, Ganesh B, et al. Malignant peripheral nerve sheath tumors of the head and neck: a clinicopathological study. J Surg Oncol. 1994;55:100–103. doi: 10.1002/jso.2930550208. [DOI] [PubMed] [Google Scholar]
- 49.Wong WW, Hirose T, Scheithauer BW, et al. Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J Radiat Oncol Biol Phys. 1998;42:351–360. doi: 10.1016/s0360-3016(98)00223-5. [DOI] [PubMed] [Google Scholar]
- 50.Carli M, Ferrari A, Mattke A, et al. Pediatric malignant peripheral nerve sheath tumor: the Italian and German soft tissue sarcoma cooperative group. J Clin Oncol. 2005;23:8422–8430. doi: 10.1200/JCO.2005.01.4886. [DOI] [PubMed] [Google Scholar]
- 51.Doorn PF, Molenaar WM, Buter J, et al. Malignant peripheral nerve sheath tumors in patients with and without neurofibromatosis. Eur J Surg Oncol. 1995;21:78–82. doi: 10.1016/s0748-7983(05)80073-3. [DOI] [PubMed] [Google Scholar]
- 52.Ghosh BC, Ghosh L, Huvos AG, et al. Malignant schwannoma. A clinicopathologic study. Cancer. 1973;31:184–190. doi: 10.1002/1097-0142(197301)31:1<184::aid-cncr2820310126>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 53.Loree TR, North JH, Jr, Werness BA, et al. Malignant peripheral nerve sheath tumors of the head and neck: analysis of prognostic factors. Otolaryngol Head Neck Surg. 2000;122:667–672. doi: 10.1016/S0194-5998(00)70193-8. [DOI] [PubMed] [Google Scholar]
- 54.Collin C, Godbold J, Hajdu S, et al. Localized extremity soft tissue sarcoma: an analysis of factors affecting survival. J Clin Oncol. 1987;5:601–612. doi: 10.1200/JCO.1987.5.4.601. [DOI] [PubMed] [Google Scholar]
- 55.Nishida T, Hirota S. Biological and clinical review of stromal tumors in the gastrointestinal tract. Histol Histopathol. 2000;15:1293–1301. doi: 10.14670/HH-15.1293. [DOI] [PubMed] [Google Scholar]
- 56.Andersson J, Sihto H, Meis-Kindblom JM, et al. NF1-associated gastrointestinal stromal tumors have unique clinical, phenotypic, and genotypic characteristics. Am J Surg Pathol. 2005;29:1170–1176. doi: 10.1097/01.pas.0000159775.77912.15. [DOI] [PubMed] [Google Scholar]
- 57.Barahona-Garrido J, Aguirre-Gutierrez R, Gutierrez-Manjarrez JI, et al. Association of GIST and somatostatinoma in a patient with type-1 neurofibromatosis: is there a common pathway? Am J Gastroenterol. 2009;104:797–799. doi: 10.1038/ajg.2008.133. [DOI] [PubMed] [Google Scholar]
- 58.Joo M, Lee HK, Kim H, et al. Multiple small intestinal stromal tumors associated with neurofibromatosis-1. Yonsei Med J. 2004;45:564–567. doi: 10.3349/ymj.2004.45.3.564. [DOI] [PubMed] [Google Scholar]
- 59.Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 60.Kindblom LG, Remotti HE, Aldenborg F, et al. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259–1269. [PMC free article] [PubMed] [Google Scholar]
- 61.Sakurai S, Fukasawa T, Chong JM, et al. C-kit gene abnormalities in gastrointestinal stromal tumors (tumors of interstitial cells of Cajal. Jpn J Cancer Res. 1999;90:1321–1328. doi: 10.1111/j.1349-7006.1999.tb00715.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chian R, Young S, Danilkovitch-Miagkova A, et al. Phosphatidylinositol 3 kinase contributes to the transformation of hematopoietic cells by the D816V c-Kit mutant. Blood. 2001;98:1365–1373. doi: 10.1182/blood.v98.5.1365. [DOI] [PubMed] [Google Scholar]
- 63.Corless CL, McGreevey L, Haley A, et al. KIT mutations are common in incidental gastrointestinal stromal tumors one centimeter or less in size. Am J Pathol. 2002;160:1567–1572. doi: 10.1016/S0002-9440(10)61103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin Oncol. 2004;22:3813–3825. doi: 10.1200/JCO.2004.05.140. [DOI] [PubMed] [Google Scholar]
- 65.Blay JY, Bonvalot S, Casali P, et al. Consensus meeting for the management of gastrointestinal stromal tumors. Report of the GIST Consensus Conference of 20–21 March 2004, under the auspices of ESMO. Ann Oncol. 2005;16:566–578. doi: 10.1093/annonc/mdi127. [DOI] [PubMed] [Google Scholar]
- 66.Mussi C, Schildhaus HU, Gronchi A, et al. Therapeutic consequences from molecular biology for gastrointestinal stromal tumor patients affected by neurofibromatosis type 1. Clin Cancer Res. 2008;14:4550–4555. doi: 10.1158/1078-0432.CCR-08-0086. [DOI] [PubMed] [Google Scholar]
- 67.Basile U, Cavallaro G, Polistena A, et al. Gastrointestinal and retroperitoneal manifestations of type 1 neurofibromatosis. J Gastrointest Surg. 2010;14:186–194. doi: 10.1007/s11605-009-0940-5. [DOI] [PubMed] [Google Scholar]
- 68.Giuly JA, Picand R, Giuly D, et al. Von Recklinghausen disease and gastrointestinal stromal tumors. Am J Surg. 2003;185:86–87. doi: 10.1016/s0002-9610(02)01111-x. [DOI] [PubMed] [Google Scholar]
- 69.Marín-Gómez LM, Vega-Ruiz V, Garcia-Urena MA, et al. [Diagnosis and satisfactory surgical treatment of a jejunal stromal tumor] Rev Gastroenterol Mex. 2008;73:33–35. [PubMed] [Google Scholar]
- 70.Rizzo S, Bonomo S, Moser A, et al. [Bilateral pheochromocytoma associated with duodeno-jejunal GIST in patient with von Recklinghausen disease: report of a clinical case] Chir Ital. 2001;53:243–246. [PubMed] [Google Scholar]
- 71.Da Ronch T, Modesto A, Bazzocchi M. Gastrointestinal stromal tumour: spiral computed tomography features and pathologic correlation. Radiol Med. 2006;111:661–673. doi: 10.1007/s11547-006-0064-x. [DOI] [PubMed] [Google Scholar]
- 72.Kalender ME, Sevinc A, Tutar E, et al. Effect of sunitinib on metastatic gastrointestinal stromal tumor in patients with neurofibromatosis type 1: a case report. World J Gastroenterol. 2007;13:2629–2632. doi: 10.3748/wjg.v13.i18.2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee JL, Kim JY, Ryu MH, et al. Response to imatinib in KIT- and PDGFRA-wild type gastrointestinal stromal associated with neurofibromatosis type 1. Dig Dis Sci. 2006;51:1043–1046. doi: 10.1007/s10620-006-8003-1. [DOI] [PubMed] [Google Scholar]
- 74.Crist WM, Anderson JR, Meza JL, et al. Intergroup rhabdomyosarcoma study-IV: results for patients with nonmetastatic disease. J Clin Oncol. 2001;19:3091–3102. doi: 10.1200/JCO.2001.19.12.3091. [DOI] [PubMed] [Google Scholar]
- 75.Wexler LH, Meyer WH, Helman LJ. Rhabdomyosarcoma and the undifferentiated sarcomas. In: Pizzo PA, Poplack DG, editors. Principles and Practice of Pediatric Oncology. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 971–1002. [Google Scholar]
- 76.Young JL, Jr, Ries LG, Silverberg E, et al. Cancer incidence, survival, and mortality for children younger than age 15 years. Cancer. 1986;58(2 Suppl):598–602. doi: 10.1002/1097-0142(19860715)58:2+<598::aid-cncr2820581332>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 77.Hadjistilianou T, Mastrangelo D, Gragnoli A, et al. Letter to the editor: neurofibromatosis type 1 (NF 1) associated with embryonal rhabdomyosarcoma of the orbit. Med Pediatr Oncol. 2002;38:449. doi: 10.1002/mpo.1362. [DOI] [PubMed] [Google Scholar]
- 78.Lampe AK, Seymour G, Thompson PW, et al. Familial neurofibromatosis microdeletion syndrome complicated by rhabdomyosarcoma. Arch Dis Child. 2002;87:444–445. doi: 10.1136/adc.87.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nascimento AF. Rhabdomyosarcomas in adults: classification and differential diagnosis. Diagn Histopathol. 2008;14:538–545. [Google Scholar]
- 80.Reich S, Overberg-Schmidt US, Leenen A, et al. Neurofibromatosis 1 associated with embryonal rhabdomyosarcoma of the urinary bladder. Pediatr Hematol Oncol. 1999;16:263–266. doi: 10.1080/088800199277335. [DOI] [PubMed] [Google Scholar]
- 81.Sung L, Anderson JR, Arndt C, et al. Neurofibromatosis in children with Rhabdomyosarcoma: a report from the Intergroup Rhabdomyosarcoma study IV. J Pediatr. 2004;144:666–668. doi: 10.1016/j.jpeds.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 82.Vogel KS, Klesse LJ, Velasco-Miguel S, et al. Mouse tumor model for neurofibromatosis type 1. Science. 1999;286:2176–2179. doi: 10.1126/science.286.5447.2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ferrari A, Bisogno G, Macaluso A, et al. Soft-tissue sarcomas in children and adolescents with neurofibromatosis type 1. Cancer. 2007;109:1406–1412. doi: 10.1002/cncr.22533. [DOI] [PubMed] [Google Scholar]
- 84.Sørensen PH, Lynch JC, Qualman SJ, et al. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: a report from the children's oncology group. J Clin Oncol. 2002;20:2672–2679. doi: 10.1200/JCO.2002.03.137. [DOI] [PubMed] [Google Scholar]
- 85.Stevens MC, Rey A, Bouvet N, et al. Treatment of nonmetastatic rhabdomyosarcoma in childhood and adolescence: third study of the International Society of Paediatric Oncology–SIOP Malignant Mesenchymal Tumor 89. J Clin Oncol. 2005;23:2618–2628. doi: 10.1200/JCO.2005.08.130. [DOI] [PubMed] [Google Scholar]
- 86.Modlin IM, Kidd M, Latich I, et al. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128:1717–1751. doi: 10.1053/j.gastro.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 87.Burke AP, Sobin LH, Shekitka KM, et al. Somatostatin-producing duodenal carcinoids in patients with von Recklinghausen's neurofibromatosis. A predilection for black patients. Cancer. 1990;65:1591–1595. doi: 10.1002/1097-0142(19900401)65:7<1591::aid-cncr2820650723>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 88.Levy AD, Taylor LD, Abbott RM, et al. Duodenal carcinoids: imaging features with clinical-pathologic comparison. Radiology. 2005;237:967–972. doi: 10.1148/radiol.2373041863. [DOI] [PubMed] [Google Scholar]
- 89.Dayal Y, Tallberg KA, Nunnemacher G, et al. Duodenal carcinoids in patients with and without neurofibromatosis. A comparative study. Am J Surg Pathol. 1986;10:348–357. doi: 10.1097/00000478-198605000-00007. [DOI] [PubMed] [Google Scholar]
- 90.De Palma GD, Masone S, Siciliano S, et al. Endocrine carcinoma of the major papilla: report of two cases and review of the literature. Surg Oncol. 2010;19:235–242. doi: 10.1016/j.suronc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 91.Robertson RG, Geiger WJ, Davis NB. Carcinoid tumors. Am Fam Physician. 2006;74:429–434. [PubMed] [Google Scholar]
- 92.Hatzitheoklitos E, Buchler MW, Friess H, et al. Carcinoid of the ampulla of Vater. Clinical characteristics and morphologic features. Cancer. 1994;73:1580–1588. doi: 10.1002/1097-0142(19940315)73:6<1580::aid-cncr2820730608>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 93.Makhlouf HR, Burke AP, Sobin LH. Carcinoid tumors of the ampulla of Vater: a comparison with duodenal carcinoid tumors. Cancer. 1999;85:1241–1249. doi: 10.1002/(sici)1097-0142(19990315)85:6<1241::aid-cncr5>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 94.Deschamps L, Dokmak S, Guedj N, et al. Mixed endocrine somatostatinoma of the ampulla of vater associated with a neurofibromatosis type 1: a case report and review of the literature. JOP. 2010;11:64–68. [PubMed] [Google Scholar]
- 95.Bettini R, Falconi M, Crippa S, et al. Ampullary somatostatinomas and jejunal gastrointestinal stromal tumor in a patient with Von Recklinghausen's disease. World J Gastroenterol. 2007;13:2761–2763. doi: 10.3748/wjg.v13.i19.2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Usui M, Matsuda S, Suzuki H, et al. Somatostatinoma of the papilla of Vater with multiple gastrointestinal stromal tumors in a patient with von Recklinghausen's disease. J Gastroenterol. 2002;37:947–953. doi: 10.1007/s005350200159. [DOI] [PubMed] [Google Scholar]
- 97.Griffiths DF, Williams GT, Williams ED. Duodenal carcinoid tumours, phaeochromocytoma and neurofibromatosis: islet cell tumour, phaeochromocytoma and the von Hippel-Lindau complex: two distinctive neuroendocrine syndromes. Q J Med. 1987;64:769–782. [PubMed] [Google Scholar]
- 98.Kainuma O, Ito Y, Taniguchi T, et al. Ampullary somatostatinoma in a patient with von Recklinghausen's disease. J Gastroenterol. 1996;31:460–464. doi: 10.1007/BF02355041. [DOI] [PubMed] [Google Scholar]
- 99.Brunaud L, Clark OH. Neuroendocrine Tumors of the Gastrointestinal System (Carcinoid Tumors) In: Clark OH, editor. Endocrine tumors. Atlanta: American Cancer Society; 2002. p. 223. [Google Scholar]
- 100.Levy AD, Sobin LH. From the archives of the AFIP: Gastrointestinal carcinoids: imaging features with clinicopathologic comparison. Radiographics. 2007;27:237–257. doi: 10.1148/rg.271065169. [DOI] [PubMed] [Google Scholar]
- 101.Hope DG, Mulvihill JJ. Malignancy in neurofibromatosis. Adv Neurol. 1981;29:33–56. [PubMed] [Google Scholar]
- 102.Weichert RF, III, Roth LM, Krementz ET, et al. Carcinoid-islet cell tumors of the duodenum. Report of twenty-one cases. Am J Surg. 1971;121:195–205. doi: 10.1016/0002-9610(71)90098-5. [DOI] [PubMed] [Google Scholar]
- 103.Hartel M, Wente MN, Sido B, et al. Carcinoid of the ampulla of Vater. J Gastroenterol Hepatol. 2005;20:676–681. doi: 10.1111/j.1440-1746.2005.03744.x. [DOI] [PubMed] [Google Scholar]
- 104.Cappelli C, Agosti B, Braga M, et al. Von Recklinghausen's neurofibromatosis associated with duodenal somatostatinoma. A case report and review of the literature. Minerva Endocrinol. 2004;29:19–24. [PubMed] [Google Scholar]
- 105.Ghassemi KA, Ou H, Roth BE. Multiple rectal carcinoids in a patient with neurofibromatosis. Gastrointest Endosc. 2010;71:216–218. doi: 10.1016/j.gie.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 106.Clements WM, Martin SP, Stemmerman G, et al. Ampullary carcinoid tumors: rationale for an aggressive surgical approach. J Gastrointest Surg. 2003;7:773–776. doi: 10.1016/s1091-255x(03)00114-8. [DOI] [PubMed] [Google Scholar]
- 107.Green BT, Rockey DC. Duodenal somatostatinoma presenting with complete somatostatinoma syndrome. J Clin Gastroenterol. 2001;33:415–417. doi: 10.1097/00004836-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 108.Eriksson B, Oberg K. Peptide hormones as tumor markers in neuroendocrine gastrointestinal tumors. Acta Oncol. 1991;30:477–483. doi: 10.3109/02841869109092404. [DOI] [PubMed] [Google Scholar]
- 109.Rösch T, Lightdale CJ, Botet JF, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. 1992;326:1721–1726. doi: 10.1056/NEJM199206253262601. [DOI] [PubMed] [Google Scholar]
- 110.Zimmer T, Ziegler K, Liehr RM, et al. Endosonography of neuroendocrine tumors of the stomach, duodenum, and pancreas. Ann N Y Acad Sci. 1994;733:425–436. doi: 10.1111/j.1749-6632.1994.tb17292.x. [DOI] [PubMed] [Google Scholar]
- 111.Pantongrag-Brown L, Buetow PC, Carr NJ, et al. Calcification and fibrosis in mesenteric carcinoid tumor: CT findings and pathologic correlation. AJR Am J Roentgenol. 1995;164:387–391. doi: 10.2214/ajr.164.2.7839976. [DOI] [PubMed] [Google Scholar]
- 112.Modlin IM, Tang LH. Approaches to the diagnosis of gut neuroendocrine tumors: the last word (today) Gastroenterology. 1997;112:583–590. doi: 10.1053/gast.1997.v112.pm9024313. [DOI] [PubMed] [Google Scholar]
- 113.Juergens KU, Weckesser M, Bettendorf O, et al. Duodenal somatostatinoma and gastrointestinal stromal tumor associated with neurofibromatosis type 1: diagnosis with PET/CT. AJR Am J Roentgenol. 2006;187:W233–W234. doi: 10.2214/AJR.05.1328. [DOI] [PubMed] [Google Scholar]
- 114.Takai A, Setoyama T, Miyamoto S. Pancreatic somatostatinoma with von Recklinghausen's disease. Clin Gastroenterol Hepatol. 2009;7:A28. doi: 10.1016/j.cgh.2008.08.036. [DOI] [PubMed] [Google Scholar]
- 115.Walther MM, Herring J, Enquist E, et al. von Recklinghausen's disease and pheochromocytomas. J Urol. 1999;162:1582–1586. [PubMed] [Google Scholar]
- 116.Guerrero MA, Schreinemakers JM, Vriens MR, et al. Clinical spectrum of pheochromocytoma. J Am Coll Surg. 2009;209:727–732. doi: 10.1016/j.jamcollsurg.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 117.Chetty R, Duhig JD. Bilateral pheochromocytoma-ganglioneuroma of the adrenal in type 1 neurofibromatosis. Am J Surg Pathol. 1993;17:837–841. doi: 10.1097/00000478-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 118.Zografos GN, Vasiliadis GK, Zagouri F, et al. Pheochromocytoma associated with neurofibromatosis type 1: concepts and current trends. World J Surg Oncol. 2010;8:14. doi: 10.1186/1477-7819-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Nguyen-Martin MA, Hammer GD. Pheochromocytoma: an update on risk groups, diagnosis, and management. Hosp Physician. 2006;2:17–24. [Google Scholar]
- 120.Ilias I, Pacak K. Current approaches and recommended algorithm for the diagnostic localization of pheochromocytoma. J Clin Endocrinol Metab. 2004;89:479–491. doi: 10.1210/jc.2003-031091. [DOI] [PubMed] [Google Scholar]
- 121.Lenders JW, Pacak K, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287:1427–1434. doi: 10.1001/jama.287.11.1427. [DOI] [PubMed] [Google Scholar]
- 122.Pacak K, Linehan WM, Eisenhofer G, et al. Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med. 2001;134:315–329. doi: 10.7326/0003-4819-134-4-200102200-00016. [DOI] [PubMed] [Google Scholar]
- 123.Grouzmann E, Drouard-Troalen L, Baudin E, et al. Diagnostic accuracy of free and total metanephrines in plasma and fractionated metanephrines in urine of patients with pheochromocytoma. Eur J Endocrinol. 2010;162:951–960. doi: 10.1530/EJE-09-0996. [DOI] [PubMed] [Google Scholar]
- 124.Berglund AS, Hulthen UL, Manhem P, et al. Metaiodobenzylguanidine (MIBG) scintigraphy and computed tomography (CT) in clinical practice. Primary and secondary evaluation for localization of phaeochromocytomas. J Intern Med. 2001;249:247–251. doi: 10.1046/j.1365-2796.2001.00792.x. [DOI] [PubMed] [Google Scholar]
- 125.Pacak K, Eisenhofer G, Carrasquillo JA, et al. Diagnostic localization of pheochromocytoma: the coming of age of positron emission tomography. Ann N Y Acad Sci. 2002;970:170–176. doi: 10.1111/j.1749-6632.2002.tb04423.x. [DOI] [PubMed] [Google Scholar]
- 126.Witteles RM, Kaplan EL, Roizen MF. Sensitivity of diagnostic and localization tests for pheochromocytoma in clinical practice. Arch Intern Med. 2000;160:2521–2524. doi: 10.1001/archinte.160.16.2521. [DOI] [PubMed] [Google Scholar]
- 127.Lumachi F, Tregnaghi A, Zucchetta P, et al. Sensitivity and positive predictive value of CT, MRI and 123I-MIBG scintigraphy in localizing pheochromocytomas: a prospective study. Nucl Med Commun. 2006;27:583–587. doi: 10.1097/00006231-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 128.Manger WM, Eisenhofer G. Pheochromocytoma: diagnosis and management update. Curr Hypertens Rep. 2004;6:477–484. doi: 10.1007/s11906-004-0044-2. [DOI] [PubMed] [Google Scholar]
- 129.Gonias S, Goldsby R, Matthay KK, et al. Phase II study of high-dose [131I]metaiodobenzylguanidine therapy for patients with metastatic pheochromocytoma and paraganglioma. J Clin Oncol. 2009;27:4162–4168. doi: 10.1200/JCO.2008.21.3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Huang H, Abraham J, Hung E, et al. Treatment of malignant pheochromocytoma/paraganglioma with cyclophosphamide, vincristine, and dacarbazine: recommendation from a 22-year follow-up of 18 patients. Cancer. 2008;113:2020–2028. doi: 10.1002/cncr.23812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Grünwald F, Ezziddin S. 131I-metaiodobenzylguanidine therapy of neuroblastoma and other neuroendocrine tumors. Semin Nucl Med. 2010;40:153–163. doi: 10.1053/j.semnuclmed.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 132.Listernick R, Louis DN, Packer RJ, et al. Optic pathway gliomas in children with neurofibromatosis 1: consensus statement from the NF1 Optic Pathway Glioma Task Force. Ann Neurol. 1997;41:143–149. doi: 10.1002/ana.410410204. [DOI] [PubMed] [Google Scholar]
- 133.Hayostek CJ, Shaw EG, Scheithauer B, et al. Astrocytomas of the cerebellum. A comparative clinicopathologic study of pilocytic and diffuse astrocytomas. Cancer. 1993;72:856–869. doi: 10.1002/1097-0142(19930801)72:3<856::aid-cncr2820720335>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 134.Hoyt WF, Baghdassarian SA. Optic glioma of childhood. Natural history and rationale for conservative management. Br J Ophthalmol. 1969;53:793–798. doi: 10.1136/bjo.53.12.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rodriguez HA, Berthrong M. Multiple primary intracranial tumors in von Recklinghausen's neurofibromatosis. Arch Neurol. 1966;14:467–475. doi: 10.1001/archneur.1966.00470110011002. [DOI] [PubMed] [Google Scholar]
- 136.Burger PC, Scheithauer BE. Silver Spring, MD: American Registry of Pathology; 1994. Atlas of Tumor Pathology: Tumors of the Central Nervous System. [Google Scholar]
- 137.Blazo MA, Lewis RA, Chintagumpala MM, et al. Outcomes of systematic screening for optic pathway tumors in children with Neurofibromatosis Type 1. Am J Med Genet A. 2004;127A:224–229. doi: 10.1002/ajmg.a.20650. [DOI] [PubMed] [Google Scholar]
- 138.Lewis RA, Gerson LP, Axelson KA, et al. von Recklinghausen neurofibromatosis. II. Incidence of optic gliomata. Ophthalmology. 1984;91:929–935. doi: 10.1016/s0161-6420(84)34217-8. [DOI] [PubMed] [Google Scholar]
- 139.Listernick R, Charrow J, Greenwald M, et al. Natural history of optic pathway tumors in children with neurofibromatosis type 1: a longitudinal study. J Pediatr. 1994;125:63–66. doi: 10.1016/s0022-3476(94)70122-9. [DOI] [PubMed] [Google Scholar]
- 140.Nicolin G, Parkin P, Mabbott D, et al. Natural history and outcome of optic pathway gliomas in children. Pediatr Blood Cancer. 2009;53:1231–1237. doi: 10.1002/pbc.22198. [DOI] [PubMed] [Google Scholar]
- 141.Singhal S, Birch JM, Kerr B, et al. Neurofibromatosis type 1 and sporadic optic gliomas. Arch Dis Child. 2002;87:65–70. doi: 10.1136/adc.87.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Szudek J, Birch P, Riccardi VM, et al. Associations of clinical features in neurofibromatosis 1 (NF1) Genet Epidemiol. 2000;19:429–439. doi: 10.1002/1098-2272(200012)19:4<429::AID-GEPI13>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 143.Astrup J. Natural history and clinical management of optic pathway glioma. Br J Neurosurg. 2003;17:327–335. doi: 10.1080/02688690310001601216. [DOI] [PubMed] [Google Scholar]
- 144.Chateil JF, Soussotte C, Pedespan JM, et al. MRI and clinical differences between optic pathway tumours in children with and without neurofibromatosis. Br J Radiol. 2001;74:24–31. doi: 10.1259/bjr.74.877.740024. [DOI] [PubMed] [Google Scholar]
- 145.Fouladi M, Wallace D, Langston JW, et al. Survival and functional outcome of children with hypothalamic/chiasmatic tumors. Cancer. 2003;97:1084–1092. doi: 10.1002/cncr.11119. [DOI] [PubMed] [Google Scholar]
- 146.Grill J, Laithier V, Rodriguez D, et al. When do children with optic pathway tumours need treatment? An oncological perspective in 106 patients treated in a single centre. Eur J Pediatr. 2000;159:692–696. doi: 10.1007/s004310000531. [DOI] [PubMed] [Google Scholar]
- 147.Tow SL, Chandela S, Miller NR, et al. Long-term outcome in children with gliomas of the anterior visual pathway. Pediatr Neurol. 2003;28:262–270. doi: 10.1016/s0887-8994(02)00628-8. [DOI] [PubMed] [Google Scholar]
- 148.Guillamo JS, Creange A, Kalifa C, et al. Prognostic factors of CNS tumours in Neurofibromatosis 1 (NF1): a retrospective study of 104 patients. Brain. 2003;126(Pt 1):152–160. doi: 10.1093/brain/awg016. [DOI] [PubMed] [Google Scholar]
- 149.Kornreich L, Blaser S, Schwarz M, et al. Optic pathway glioma: correlation of imaging findings with the presence of neurofibromatosis. AJNR Am J Neuroradiol. 2001;22:1963–1969. [PMC free article] [PubMed] [Google Scholar]
- 150.Listernick R, Ferner RE, Piersall L, et al. Late-onset optic pathway tumors in children with neurofibromatosis 1. Neurology. 2004;63:1944–1946. doi: 10.1212/01.wnl.0000144341.16830.01. [DOI] [PubMed] [Google Scholar]
- 151.Liu GT, Brodsky MC, Phillips PC, et al. Optic radiation involvement in optic pathway gliomas in neurofibromatosis. Am J Ophthalmol. 2004;137:407–414. doi: 10.1016/j.ajo.2003.09.055. [DOI] [PubMed] [Google Scholar]
- 152.Bachoo RM, Maher EA, Ligon KL, et al. Epidermal growth factor receptor and Ink4a/Arf: convergent mechanisms governing terminal differentiation and transformation along the neural stem cell to astrocyte axis. Cancer Cell. 2002;1:269–277. doi: 10.1016/s1535-6108(02)00046-6. [DOI] [PubMed] [Google Scholar]
- 153.Dai C, Holland EC. Astrocyte differentiation states and glioma formation. Cancer J. 2003;9:72–81. doi: 10.1097/00130404-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 154.Uhrbom L, Dai C, Celestino JC, et al. Ink4a-Arf loss cooperates with KRas activation in astrocytes and neural progenitors to generate glioblastomas of various morphologies depending on activated Akt. Cancer Res. 2002;62:5551–5558. [PubMed] [Google Scholar]
- 155.Sylvester CL, Drohan LA, Sergott RC. Optic-nerve gliomas, chiasmal gliomas and neurofibromatosis type 1. Curr Opin Ophthalmol. 2006;17:7–11. doi: 10.1097/01.icu.0000193070.32369.37. [DOI] [PubMed] [Google Scholar]
- 156.Farmer JP, Khan S, Khan A, et al. Neurofibromatosis type 1 and the pediatric neurosurgeon: a 20-year institutional review. Pediatr Neurosurg. 2002;37:122–136. doi: 10.1159/000064398. [DOI] [PubMed] [Google Scholar]
- 157.Alvord EC, Jr., Lofton S. Gliomas of the optic nerve or chiasm. Outcome by patients' age, tumor site, and treatment. J Neurosurg. 1988;68:85–98. doi: 10.3171/jns.1988.68.1.0085. [DOI] [PubMed] [Google Scholar]
- 158.Balcer LJ, Liu GT, Heller G, et al. Visual loss in children with neurofibromatosis type 1 and optic pathway gliomas: relation to tumor location by magnetic resonance imaging. Am J Ophthalmol. 2001;131:442–445. doi: 10.1016/s0002-9394(00)00852-7. [DOI] [PubMed] [Google Scholar]
- 159.Czyzyk E, Jozwiak S, Roszkowski M, et al. Optic pathway gliomas in children with and without neurofibromatosis 1. J Child Neurol. 2003;18:471–478. doi: 10.1177/08830738030180070401. [DOI] [PubMed] [Google Scholar]
- 160.Habiby R, Silverman B, Listernick R, et al. Precocious puberty in children with neurofibromatosis type 1. J Pediatr. 1995;126:364–367. doi: 10.1016/s0022-3476(95)70449-3. [DOI] [PubMed] [Google Scholar]
- 161.Gayre GS, Scott IU, Feuer W, et al. Long-term visual outcome in patients with anterior visual pathway gliomas. J Neuroophthalmol. 2001;21:1–7. doi: 10.1097/00041327-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 162.Thiagalingam S, Flaherty M, Billson F, et al. Neurofibromatosis type 1 and optic pathway gliomas: follow-up of 54 patients. Ophthalmology. 2004;111:568–577. doi: 10.1016/j.ophtha.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 163.Parsa CF, Hoyt CS, Lesser RL, et al. Spontaneous regression of optic gliomas: thirteen cases documented by serial neuroimaging. Arch Ophthalmol. 2001;119:516–529. doi: 10.1001/archopht.119.4.516. [DOI] [PubMed] [Google Scholar]
- 164.Shuper A, Horev G, Kornreich L, et al. Visual pathway glioma: an erratic tumour with therapeutic dilemmas. Arch Dis Child. 1997;76:259–263. doi: 10.1136/adc.76.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.King A, Listernick R, Charrow J, et al. Optic pathway gliomas in neurofibromatosis type 1: the effect of presenting symptoms on outcome. Am J Med Genet A. 2003;122A:95–99. doi: 10.1002/ajmg.a.20211. [DOI] [PubMed] [Google Scholar]
- 166.Falsini B, Ziccardi L, Lazzareschi I, et al. Longitudinal assessment of childhood optic gliomas: relationship between flicker visual evoked potentials and magnetic resonance imaging findings. J Neurooncol. 2008;88:87–96. doi: 10.1007/s11060-008-9537-1. [DOI] [PubMed] [Google Scholar]
- 167.Wolsey DH, Larson SA, Creel D, et al. Can screening for optic nerve gliomas in patients with neurofibromatosis type I be performed with visual-evoked potential testing? J AAPOS. 2006;10:307–311. doi: 10.1016/j.jaapos.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 168.Stern J, DiGiacinto GV, Housepian EM. Neurofibromatosis and optic glioma: clinical and morphological correlations. Neurosurgery. 1979;4:524–528. doi: 10.1227/00006123-197906000-00006. [DOI] [PubMed] [Google Scholar]
- 169.Massimi L, Tufo T, Di RC. Management of optic-hypothalamic gliomas in children: still a challenging problem. Expert Rev Anticancer Ther. 2007;7:1591–1610. doi: 10.1586/14737140.7.11.1591. [DOI] [PubMed] [Google Scholar]
- 170.Deliganis AV, Geyer JR, Berger MS. Prognostic significance of type 1 neurofibromatosis (von Recklinghausen Disease) in childhood optic glioma. Neurosurgery. 1996;38:1114–1118. doi: 10.1097/00006123-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 171.Binning MJ, Liu JK, Kestle JR, et al. Optic pathway gliomas: a review. Neurosurg Focus. 2007;23:E2. doi: 10.3171/FOC-07/11/E2. [DOI] [PubMed] [Google Scholar]
- 172.Listernick R, Ferner RE, Liu GT, et al. Optic pathway gliomas in neurofibromatosis-1: controversies and recommendations. Ann Neurol. 2007;61:189–198. doi: 10.1002/ana.21107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kaufman LM, Doroftei O. Optic glioma warranting treatment in children. Eye (Lond) 2006;20:1149–1164. doi: 10.1038/sj.eye.6702379. [DOI] [PubMed] [Google Scholar]
- 174.Khafaga Y, Hassounah M, Kandil A, et al. Optic gliomas: a retrospective analysis of 50 cases. Int J Radiat Oncol Biol Phys. 2003;56:807–812. doi: 10.1016/s0360-3016(02)04512-1. [DOI] [PubMed] [Google Scholar]
- 175.Bajenaru ML, Hernandez MR, Perry A, et al. Optic nerve glioma in mice requires astrocyte Nf1 gene inactivation and Nf1 brain heterozygosity. Cancer Res. 2003;63:8573–8577. [PubMed] [Google Scholar]
- 176.Cummings TJ, Provenzale JM, Hunter SB, et al. Gliomas of the optic nerve: histological, immunohistochemical (MIB-1 and p53), and MRI analysis. Acta Neuropathol. 2000;99:563–570. doi: 10.1007/s004010051161. [DOI] [PubMed] [Google Scholar]
- 177.Kortmann RD, Timmermann B, Taylor RE, et al. Current and future strategies in radiotherapy of childhood low-grade glioma of the brain. Part II: Treatment-related late toxicity. Strahlenther Onkol. 2003;179:585–597. doi: 10.1007/s00066-003-8104-0. [DOI] [PubMed] [Google Scholar]
- 178.Raffel C, McComb JG, Bodner S, et al. Benign brain stem lesions in pediatric patients with neurofibromatosis: case reports. Neurosurgery. 1989;25:959–964. doi: 10.1097/00006123-198912000-00018. [DOI] [PubMed] [Google Scholar]
- 179.Ullrich NJ, Raja AI, Irons MB, et al. Brainstem lesions in neurofibromatosis type 1. Neurosurgery. 2007;61:762–766. doi: 10.1227/01.NEU.0000298904.63635.2D. [DOI] [PubMed] [Google Scholar]
- 180.Bilaniuk LT, Molloy PT, Zimmerman RA, et al. Neurofibromatosis type 1: brain stem tumours. Neuroradiology. 1997;39:642–653. doi: 10.1007/s002340050484. [DOI] [PubMed] [Google Scholar]
- 181.Ueoka DI, Nogueira J, Campos JC, et al. Brainstem gliomas–retrospective analysis of 86 patients. J Neurol Sci. 2009;281:20–23. doi: 10.1016/j.jns.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 182.Hottinger AF, Khakoo Y. Neuro-oncology of Neurofibromatosis Type 1. Curr Treat Options Neurol. 2009;11:306–314. doi: 10.1007/s11940-009-0034-4. [DOI] [PubMed] [Google Scholar]
- 183.Rodriguez FJ, Perry A, Gutmann DH, et al. Gliomas in neurofibromatosis type 1: a clinicopathologic study of 100 patients. J Neuropathol Exp Neurol. 2008;67:240–249. doi: 10.1097/NEN.0b013e318165eb75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Listernick R, Charrow J, Gutmann DH. Intracranial gliomas in neurofibromatosis type 1. Am J Med Genet. 1999;89:38–44. doi: 10.1002/(sici)1096-8628(19990326)89:1<38::aid-ajmg8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 185.Molloy PT, Bilaniuk LT, Vaughan SN, et al. Brainstem tumors in patients with neurofibromatosis type 1: a distinct clinical entity. Neurology. 1995;45:1897–1902. doi: 10.1212/wnl.45.10.1897. [DOI] [PubMed] [Google Scholar]
- 186.Norfray JF, Darling C, Byrd S, et al. Short TE proton MRS and neurofibromatosis type 1 intracranial lesions. J Comput Assist Tomogr. 1999;23:994–1003. doi: 10.1097/00004728-199911000-00033. [DOI] [PubMed] [Google Scholar]
- 187.Pollack IF, Shultz B, Mulvihill JJ. The management of brainstem gliomas in patients with neurofibromatosis 1. Neurology. 1996;46:1652–1660. doi: 10.1212/wnl.46.6.1652. [DOI] [PubMed] [Google Scholar]
- 188.Shannon KM, O'Connell P, Martin GA, et al. Loss of the normal NF1 allele from the bone marrow of children with type 1 neurofibromatosis and malignant myeloid disorders. N Engl J Med. 1994;330:597–601. doi: 10.1056/NEJM199403033300903. [DOI] [PubMed] [Google Scholar]
- 189.Stiller CA, Chessells JM, Fitchett M. Neurofibromatosis and childhood leukaemia/lymphoma: a population-based UKCCSG study. Br J Cancer. 1994;70:969–972. doi: 10.1038/bjc.1994.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Bader JL, Miller RW. Neurofibromatosis and childhood leukemia. J Pediatr. 1978;92:925–929. doi: 10.1016/s0022-3476(78)80362-x. [DOI] [PubMed] [Google Scholar]
- 191.Garicochea B, Giorgi R, Odone VF, et al. Mutational analysis of N-RAS and GAP-related domain of the neurofibromatosis type 1 gene in chronic myelogenous leukemia. Leuk Res. 1998;22:1003–1007. doi: 10.1016/s0145-2126(98)00076-9. [DOI] [PubMed] [Google Scholar]
- 192.Bartram CR, Ludwig WD, Hiddemann W, et al. Acute myeloid leukemia: analysis of ras gene mutations and clonality defined by polymorphic X-linked loci. Leukemia. 1989;3:247–256. [PubMed] [Google Scholar]
- 193.Bos JL, Verlaan-de VM, van der Eb AJ, et al. Mutations in N-ras predominate in acute myeloid leukemia. Blood. 1987;69:1237–1241. [PubMed] [Google Scholar]
- 194.Farr CJ, Saiki RK, Erlich HA, et al. Analysis of RAS gene mutations in acute myeloid leukemia by polymerase chain reaction and oligonucleotide probes. Proc Natl Acad Sci U S A. 1988;85:1629–1633. doi: 10.1073/pnas.85.5.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hirai H, Kobayashi Y, Mano H, et al. A point mutation at codon 13 of the N-ras oncogene in myelodysplastic syndrome. Nature. 1987;327:430–432. doi: 10.1038/327430a0. [DOI] [PubMed] [Google Scholar]
- 196.Senn HP, Tran-Thang C, Wodnar-Filipowicz A, et al. Mutation analysis of the N-ras proto-oncogene in active and remission phase of human acute leukemias. Int J Cancer. 1988;41:59–64. doi: 10.1002/ijc.2910410112. [DOI] [PubMed] [Google Scholar]
- 197.Toksoz D, Farr CJ, Marshall CJ. ras gene activation in a minor proportion of the blast population in acute myeloid leukemia. Oncogene. 1987;1:409–413. [PubMed] [Google Scholar]
- 198.Borberg A. Clinical and genetic investigations into tuberous sclerosis and Recklinghausen's neurofibromatosis; contribution to elucidation of interrelationship and eugenics of the syndromes. Acta Psychiatr Neurol Scand Suppl. 1951;71:1–239. [PubMed] [Google Scholar]
- 199.Murayama Y, Yamamoto Y, Shimojima N, et al. Ti breast cancer associated with Von Recklinghausen's neurofibromatosis. Breast Cancer. 1999;6:227–230. doi: 10.1007/BF02967173. [DOI] [PubMed] [Google Scholar]
- 200.Sharif S, Moran A, Huson SM, et al. Women with neurofibromatosis 1 are at a moderately increased risk of developing breast cancer and should be considered for early screening. J Med Genet. 2007;44:481–484. doi: 10.1136/jmg.2007.049346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Nakamura M, Tangoku A, Kusanagi H, et al. Breast cancer associated with Recklinghausen's disease: report of a case. Nippon Geka Hokan. 1998;67:3–9. [PubMed] [Google Scholar]
- 202.Wilson CH, Griffith CD, Shrimankar J, et al. Gynaecomastia, neurofibromatosis and breast cancer. Breast. 2004;13:77–79. doi: 10.1016/j.breast.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 203.Ceccaroni M, Genuardi M, Legge F, et al. BRCA1-related malignancies in a family presenting with von Recklinghausen's disease. Gynecol Oncol. 2002;86:375–378. doi: 10.1006/gyno.2002.6757. [DOI] [PubMed] [Google Scholar]
- 204.Güran S, Safali M. A case of neurofibromatosis and breast cancer: loss of heterozygosity of NF1 in breast cancer. Cancer Genet Cytogenet. 2005;156:86–88. doi: 10.1016/j.cancergencyto.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 205.Satgé D, Sasco AJ, Goldgar D, et al. A 23-year-old woman with Down syndrome, type 1 neurofibromatosis, and breast carcinoma. Am J Med Genet A. 2004;125A:94–96. doi: 10.1002/ajmg.a.20429. [DOI] [PubMed] [Google Scholar]
- 206.Brasfield RD, Das Gupta TK. Von Recklinghausen's disease: a clinicopathological study. Ann Surg. 1972;175:86–104. doi: 10.1097/00000658-197201000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Desigan G, Dunn GD, Halter S. Adenocarcinoma of the esophagus associated with neurofibromatosis. J Tenn Med Assoc. 1985;78:138–140. [PubMed] [Google Scholar]
- 208.Basu S, Majumdar J, Mitra R, et al. Primary adenocarcinoma of the stomach associated with peripheral neurofibromatosis: report of a case. Surg Today. 1997;27:57–59. doi: 10.1007/BF01366940. [DOI] [PubMed] [Google Scholar]
- 209.Jenkins DH, Gill W. A case of carcinoma of the colon in association with neurofibromatosis. Br J Surg. 1972;59:322–323. doi: 10.1002/bjs.1800590417. [DOI] [PubMed] [Google Scholar]
- 210.Shousha S, Smith PA. Colonic ganglioneuroma. Report of a case in a patient with neurofibromatosis, multiple colonic adenomas and adenocarcinoma. Virchows Arch A Pathol Anat Histol. 1981;392:105–109. doi: 10.1007/BF00430553. [DOI] [PubMed] [Google Scholar]
- 211.Colarian J, Pietruk T, LaFave L, et al. Adenocarcinoma of the ampulla of vater associated with neurofibromatosis. J Clin Gastroenterol. 1990;12:118–119. [PubMed] [Google Scholar]
- 212.Costi R, Caruana P, Sarli L, et al. Ampullary adenocarcinoma in neurofibromatosis type 1. Case report and literature review. Mod Pathol. 2001;14:1169–1174. doi: 10.1038/modpathol.3880454. [DOI] [PubMed] [Google Scholar]
- 213.Jones TJ, Marshall TL. Neurofibromatosis and small bowel adenocarcinoma: an unrecognised association. Gut. 1987;28:1173–1176. doi: 10.1136/gut.28.9.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Joo YE, Kim HS, Choi SK, et al. Primary duodenal adenocarcinoma associated with neurofibromatosis type 1. J Gastroenterol. 2002;37:215–219. doi: 10.1007/s005350200024. [DOI] [PubMed] [Google Scholar]
- 215.Kingston RD. Neurofibromatosis and small bowel adenocarcinoma–an unrecognised association. Gut. 1988;29:134. doi: 10.1136/gut.29.1.134-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Niv Y, Abu-Avid S, Oren M. Adenocarcinoma of pancreas and duodenum associated with cutaneous neurofibromatosis. Am J Med. 1987;82:384–385. doi: 10.1016/0002-9343(87)90096-9. [DOI] [PubMed] [Google Scholar]
- 217.Keller RT, Logan GM., Jr Adenocarcinoma of the pancreas associated with neurofibromatosis. Cancer. 1977;39:1264–1266. doi: 10.1002/1097-0142(197703)39:3<1264::aid-cncr2820390337>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 218.Ching CK, Greer AJ. Metachronous biliary tract cancers in a patient with von Recklinghausen's disease. Am J Gastroenterol. 1993;88:1124–1125. [PubMed] [Google Scholar]
- 219.Sprengers DP, Knockaert DC, Van SW, et al. Primary bile duct cancer and von Recklinghausen disease. Ann Intern Med. 1987;106:772. doi: 10.7326/0003-4819-106-5-772_2. [DOI] [PubMed] [Google Scholar]
- 220.Guillot B, Dalac S, Delaunay M, et al. Cutaneous malignant melanoma and neurofibromatosis type 1. Melanoma Res. 2004;14:159–163. doi: 10.1097/00008390-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 221.To KW, Rabinowitz SM, Friedman AH, et al. Neurofibromatosis and neural crest neoplasms: primary acquired melanosis and malignant melanoma of the conjunctiva. Surv Ophthalmol. 1989;33:373–379. doi: 10.1016/0039-6257(89)90014-3. [DOI] [PubMed] [Google Scholar]
- 222.Obringer AC, Zackai EH, Meadows AT. The Neurofibromatosis Clinic of the Children's Hospital of Philadelphia. Neurofibromatosis. 1988;1:179–181. [PubMed] [Google Scholar]
- 223.Stay EJ, Vawter G. The relationship between nephroblastoma and neurofibromatosis (Von Recklinghausen's disease) Cancer. 1977;39:2550–2555. doi: 10.1002/1097-0142(197706)39:6<2550::aid-cncr2820390636>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 224.Kushner BH, Hajdu SI, Helson L. Synchronous neuroblastoma and von Recklinghausen's disease: a review of the literature. J Clin Oncol. 1985;3:117–120. doi: 10.1200/JCO.1985.3.1.117. [DOI] [PubMed] [Google Scholar]
- 225.Williams GT, Griffiths DF, Williams ED. Small intestinal adenocarcinoma, duodenal carcinoid tumour, and von Recklinghausen's neurofibromatosis. Gut. 1988;29:553. doi: 10.1136/gut.29.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ding L, Getz G, Wheeler DA, et al. Somatic mutations affect key pathways in lung adenocarcinoma. Nature. 2008;455:1069–1075. doi: 10.1038/nature07423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Cawkwell L, Lewis FA, Quirke P. Frequency of allele loss of DCC, p53, RBI, WT1, NF1, NM23 and APC/MCC in colorectal cancer assayed by fluorescent multiplex polymerase chain reaction. Br J Cancer. 1994;70:813–818. doi: 10.1038/bjc.1994.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Leggett B, Young J, Buttenshaw R, et al. Colorectal carcinomas show frequent allelic loss on the long arm of chromosome 17 with evidence for a specific target region. Br J Cancer. 1995;71:1070–1073. doi: 10.1038/bjc.1995.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ahlquist T, Bottillo I, Danielsen SA, et al. RAS signaling in colorectal carcinomas through alteration of RAS, RAF, NF1, and/or RASSF1A. Neoplasia. 2008;10:680–686. doi: 10.1593/neo.08312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Cacev T, Radosevic S, Spaventi R, et al. NF1 gene loss of heterozygosity and expression analysis in sporadic colon cancer. Gut. 2005;54:1129–1135. doi: 10.1136/gut.2004.053348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Furukawa K, Yanai N, Fujita M, et al. Novel mutations of neurofibromatosis type 1 gene in small cell lung cancers. Surg Today. 2003;33:323–327. doi: 10.1007/s005950300074. [DOI] [PubMed] [Google Scholar]
- 232.Li Y, Bollag G, Clark R, et al. Somatic mutations in the neurofibromatosis 1 gene in human tumors. Cell. 1992;69:275–281. doi: 10.1016/0092-8674(92)90408-5. [DOI] [PubMed] [Google Scholar]
- 233.Sangha N, Wu R, Kuick R, et al. Neurofibromin 1 (NF1) defects are common in human ovarian serous carcinomas and co-occur with TP53 mutations. Neoplasia. 2008;10:1362–1372. doi: 10.1593/neo.08784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Crowe FW, Schull WJ, Neel JV. Springfield: Charles C Thomas; 1956. A clinical, pathological, and genetic study of multiple neurofibromatosis. [Google Scholar]
- 235.Preston FW, Walsh WS, Clarke TH. Cutaneous neurofibromatosis (Von Recklinghausen's disease); clinical manifestation and incidence of sarcoma in sixty-one male patients. AMA Arch Surg. 1952;64:813–827. [PubMed] [Google Scholar]
- 236.Schneider M, Obringer AC, Zackai E, et al. Childhood neurofibromatosis: risk factors for malignant disease. Cancer Genet Cytogenet. 1986;21:347–354. doi: 10.1016/0165-4608(86)90216-5. [DOI] [PubMed] [Google Scholar]
- 237.Poyhonen M, Niemela S, Herva R. Risk of malignancy and death in neurofibromatosis. Arch Pathol Lab Med. 1997;121:139–143. [PubMed] [Google Scholar]
- 238.Blatt J, Jaffe R, Deutsch M, et al. Neurofibromatosis and childhood tumors. Cancer. 1986;57:1225–1229. doi: 10.1002/1097-0142(19860315)57:6<1225::aid-cncr2820570627>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 239.Matsui I, Tanimura M, Kobayashi N, et al. Neurofibromatosis type 1 and childhood cancer. Cancer. 1993;72:2746–2754. doi: 10.1002/1097-0142(19931101)72:9<2746::aid-cncr2820720936>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 240.Shearer P, Parham D, Kovnar E, et al. Neurofibromatosis type I and malignancy: review of 32 pediatric cases treated at a single institution. Med Pediatr Oncol. 1994;22:78–83. doi: 10.1002/mpo.2950220203. [DOI] [PubMed] [Google Scholar]
- 241.Cnossen MH, de Goede-Bolder A, van den Broek KM, et al. A prospective 10 year follow up study of patients with neurofibromatosis type 1. Arch Dis Child. 1998;78:408–412. doi: 10.1136/adc.78.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.deCou JM, Rao BN, Parham DM, et al. Malignant peripheral nerve sheath tumors: the St. Jude Children's Research Hospital experience. Ann Surg Oncol. 1995;2:524–529. doi: 10.1007/BF02307086. [DOI] [PubMed] [Google Scholar]
- 243.Evans DG, Baser ME, McGaughran J, et al. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39:311–314. doi: 10.1136/jmg.39.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]