This phase III trial compared the efficacy and safety of bevacizumab alone with that of bevacizumab and capecitabine plus oxaliplatin (XELOX) as maintenance treatment following induction chemotherapy with XELOX plus bevacizumab in the first-line treatment of patients with metastatic colorectal cancer. Noninferiority could not be confirmed, but the median progression-free survival detriment was >3 weeks.
Keywords: Capecitabine, Oxaliplatin, 5-FU, Bevacizumab, Metastatic colorectal cancer
Abstract
Purpose.
The aim of this phase III trial was to compare the efficacy and safety of bevacizumab alone with those of bevacizumab and capecitabine plus oxaliplatin (XELOX) as maintenance treatment following induction chemotherapy with XELOX plus bevacizumab in the first-line treatment of patients with metastatic colorectal cancer (mCRC).
Patients and Methods.
Patients were randomly assigned to receive six cycles of bevacizumab, capecitabine, and oxaliplatin every 3 weeks followed by XELOX plus bevacizumab or bevacizumab alone until progression. The primary endpoint was the progression-free survival (PFS) interval; secondary endpoints were the overall survival (OS) time, objective response rate (RR), time to response, duration of response, and safety.
Results.
The intent-to-treat population comprised 480 patients (XELOX plus bevacizumab, n = 239; bevacizumab, n = 241); there were no significant differences in baseline characteristics. The median follow-up was 29.0 months (range, 0–53.2 months). There were no statistically significant differences in the median PFS or OS times or in the RR between the two arms. The most common grade 3 or 4 toxicities in the XELOX plus bevacizumab versus bevacizumab arms were diarrhea, hand–foot syndrome, and neuropathy.
Conclusion.
Although the noninferiority of bevacizumab versus XELOX plus bevacizumab cannot be confirmed, we can reliably exclude a median PFS detriment >3 weeks. This study suggests that maintenance therapy with single-agent bevacizumab may be an appropriate option following induction XELOX plus bevacizumab in mCRC patients.
Introduction
Capecitabine in combination with oxaliplatin (the CapeOX or XELOX regimens) is considered one of the standard chemotherapy regimens in the treatment of metastatic colorectal cancer (mCRC), having efficacy similar to that of regimens based on continuous infusions of 5-fluorouracil (5-FU) combined with oxaliplatin, as evaluated in several phase III studies [1–5] and in a recent meta-analysis [6].
Bevacizumab is a humanized monoclonal antibody that inhibits vascular endothelial growth factor [7, 8] and has been shown to result in longer progression-free survival (PFS) and overall survival (OS) times when combined with chemotherapy for the treatment of patients with mCRC in the first- and second-line settings [4, 9–13]. These findings have also been replicated in two large observational studies in the U.S. (Bevacizumab Regimens: Investigation of Treatment Effects and Safety) and Europe (Bevacizumab Expanded Access Trial) [14–17].
In the NO16966 study, the addition of bevacizumab to chemotherapy resulted in a longer PFS interval but not OS time, although the durations of treatment were similar in the two groups of patients even though the protocol allowed for continued bevacizumab until disease progression [10]. This led the authors to speculate that continuation of treatment with bevacizumab until progression might be necessary to maximize its efficacy. However, none of the studies performed to date have evaluated the role of bevacizumab as maintenance treatment after induction chemotherapy.
Several recent studies have suggested different strategies to limit the toxicity of chemotherapy, specifically focusing on oxaliplatin using intermittent schedules, a “stop-and-go” approach, and even chemotherapy holidays [18–22]. The present study, Maintenance treatment in advanced colorectal cancer (MACRO) by the Spanish Cooperative Group for the Treatment of Digestive Tumors (TTD), was designed to assess the feasibility and effectiveness of maintenance treatment with single-agent bevacizumab after induction chemotherapy plus bevacizumab as an alternative to maintenance chemotherapy plus bevacizumab in patients with mCRC.
Patients and Methods
Study Design
This study was a multicenter, randomized, open-label, phase III trial designed to evaluate the efficacy and safety of six cycles of XELOX plus bevacizumab followed by maintenance with XELOX plus bevacizumab versus single-agent bevacizumab in mCRC patients. Local ethics committee approval was obtained before enrollment of any patient into the study, which was performed in accordance with the Declaration of Helsinki and its subsequent amendments as well as the Good Clinical Practice Guidelines. Signed informed consent was obtained from all patients before study entry.
Patient Population
Outpatients aged ≥18 years with histologically confirmed mCRC, an Eastern Cooperative Oncology Group performance status score ≤2, and a life expectancy >3 months were enrolled. All patients had to have at least one measurable lesion according to the Response Evaluation Criteria In Solid Tumors (RECIST) [23]. Adjuvant chemotherapy (a fluoropyrimidine with or without leucovorin), if administered, had to have been completed >6 months prior to study entry.
Patients had to have adequate hematologic (hemoglobin >9 g/dL, neutrophil count >1.5 × 109/L, and platelet count >100 × 109/L), hepatic (serum bilirubin <1.5 × the upper normal limit [UNL], glutamic oxaloacetic transaminase and glutamic pyruvic transaminase <2.5 × UNL in the absence of hepatic metastases or <5 × UNL in the presence of hepatic metastases, and alkaline phosphatase ≤2.5 × UNL or ≤5 × UNL in cases of hepatic metastases or ≤10 × UNL in cases of bone metastases), and renal (creatinine clearance ≥30 mL/minute or serum creatinine <2 mg/dL) functions. Pregnant or breast-feeding women were excluded. Other exclusion criteria were: clinically significant cardiac disease or myocardial infarction within the last 6 months, lack of physical integrity of the upper gastrointestinal tract, peripheral neuropathy, a history of malignancy other than cured basal cell carcinoma or in situ cervical carcinoma, and central nervous system metastases.
Treatment Plan
Patients were randomized 1:1 to one of two treatment arms. Initially, both groups received six cycles of XELOX (oxaliplatin, 130 mg/m2 on day 1, and capecitabine, 1,000 mg/m2 twice daily on days 1–14 every 3 weeks) plus bevacizumab (7.5 mg/kg) on day 1 of the 3-weekly cycle. Patients then received maintenance therapy consisting of either bevacizumab (7.5 mg/kg) once every 3 weeks (hereafter, the single-agent bevacizumab group) or XELOX plus bevacizumab (7.5 mg/kg) every 3 weeks until disease progression, severe toxicity, or withdrawal of consent (hereafter, XELOX plus bevacizumab group). The dose of capecitabine was reduced to 750 mg/m2 twice daily in patients with a creatinine clearance of 30–50 mL/minute.
During the initial treatment period (and maintenance period for patients in the XELOX plus bevacizumab group), capecitabine and bevacizumab could be continued at the physician's discretion in the event of discontinuation of oxaliplatin. Patients could continue receiving XELOX if bevacizumab was discontinued or capecitabine alone if oxaliplatin and bevacizumab were discontinued. Patients were removed from the study if capecitabine and bevacizumab were discontinued. During the maintenance phase in the single-agent bevacizumab group, patients were withdrawn from the study if bevacizumab was discontinued for >3 weeks. Patients were also removed from the study if their tumor became operable and they underwent resection.
Assessments
A medical history, physical examination, routine blood analysis (hematology and biochemistry), and pregnancy test for women of child-bearing age were performed within 1 week, and carcinoembryonic antigen measurement and electrocardiogram were performed within 4 weeks of entry. Imaging studies (including chest x-ray, computed tomography scans, and other examinations as indicated) were performed within 4 weeks of study entry and were repeated every 9 weeks during treatment.
The RECIST [23] were used to define all responses after patients received at least 9 weeks of therapy as follows: complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD). Disease control was defined as the sum of patients achieving a CR, PR, or SD. Confirmation of all responses was required after 4 weeks. Response was assessed by investigators only (i.e., there was no independent response evaluation committee).
Toxicity was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (version 3.0). In addition, the incidence of the following specific adverse events (irrespective of their possible relationship to bevacizumab treatment) was assessed: gastrointestinal perforation, wound-healing complications, bleeding/hemorrhage, hypertension, proteinuria, and thromboembolism (venous and arterial).
Statistical Analysis
The primary endpoint was the PFS interval, defined as the time from the start of treatment to progression or death. Secondary endpoints included the OS time, defined as the time from treatment initiation to death; objective tumor response; time to response (TTR), defined as the time from initiation of treatment until objective CR or PR; response duration; and safety.
Assuming an estimated PFS duration of 10 months in both treatment groups and a prespecified noninferiority limit for the hazard ratio (HR) of 1.32 (corresponding to a hypothetical inferiority of 7.6 months with single-agent bevacizumab maintenance therapy) to be excluded, it was estimated that a total of 470 patients (235 in each arm) needed to be randomized to achieve 80% statistical power with a one-sided α error of 0.025. Noninferiority was concluded if the upper limit of the 95% confidence interval (CI) of the HR was ≤1.32. Results were described for the intent-to-treat population (all randomized patients) and the safety population (all patients who received at least one dose of medication).
Survival curves were estimated using the Kaplan–Meier method and compared using the log-rank test. A Cox regression model, including treatment group as a variable, was performed to estimate HRs for the survival analysis.
Results
Patients and Treatment
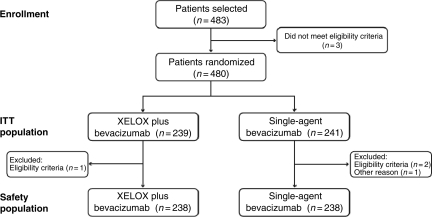
Between July 2006 and September 2008, 480 patients were entered into the study; 239 were randomized to maintenance XELOX plus bevacizumab after induction XELOX plus bevacizumab and 241 were randomized to single-agent bevacizumab after induction XELOX plus bevacizumab (Fig. 1). Three patients in the single-agent bevacizumab group and one patient in the XELOX plus bevacizumab group were not included in the safety population: the patient in the XELOX plus bevacizumab group was excluded because he did not fulfill the eligibility criteria, whereas two patients in the single-agent bevacizumab group were excluded because they did not fulfill the eligibility criteria and one was included outside the recruitment period. The safety population therefore consisted of 238 patients in each arm. Baseline demographic and clinical characteristics were well balanced between treatment arms (Table 1).
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow chart.
Abbreviations: ITT, intent to treat; XELOX, capecitabine plus oxaliplatin.
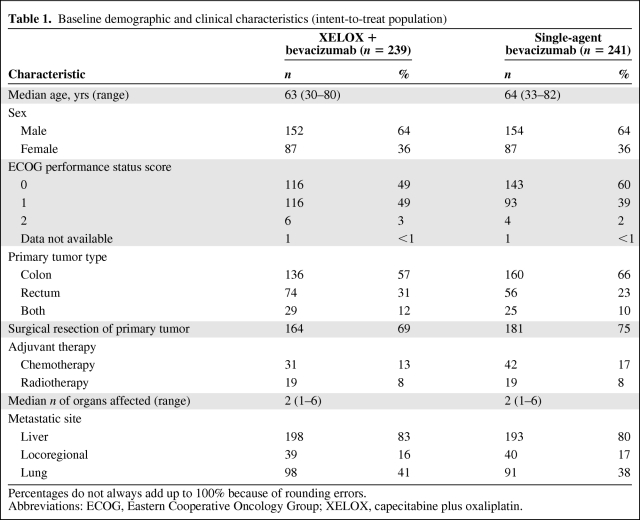
Table 1.
Baseline demographic and clinical characteristics (intent-to-treat population)
Percentages do not always add up to 100% because of rounding errors.
Abbreviations: ECOG, Eastern Cooperative Oncology Group; XELOX, capecitabine plus oxaliplatin.
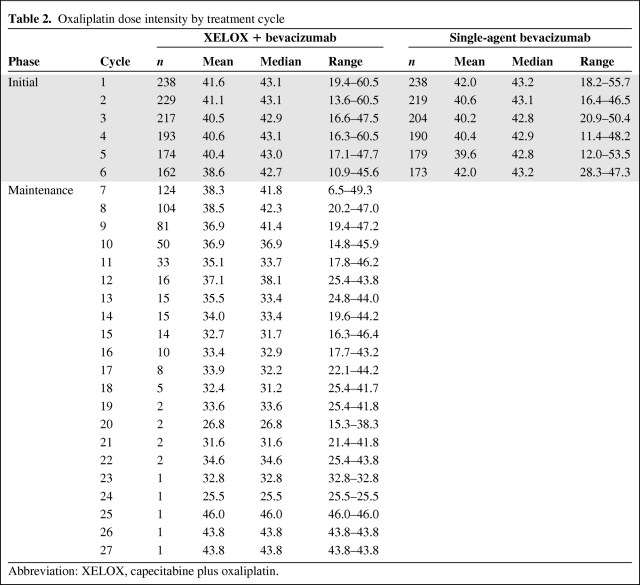
Treatment compliance was similar in both groups, with patients in the combination arm receiving a median of nine cycles (range, 1–49 cycles) and those in the single-agent bevacizumab group receiving a median of 10 cycles (range, 1–54 cycles). The median cumulative doses over the study period were as follows: oxaliplatin, 801.3 mg/m2 and 770.2 mg/m2 in the XELOX plus bevacizumab and single-agent bevacizumab groups, respectively; bevacizumab, 67.5 mg/kg and 74.1 mg/kg, respectively; and capecitabine, 217,156 mg/m2 and 153,456 mg/m2, respectively. Oxaliplatin dose intensity data by cycle for the two treatment groups are shown in Table 2.
Table 2.
Oxaliplatin dose intensity by treatment cycle
Abbreviation: XELOX, capecitabine plus oxaliplatin.
Efficacy
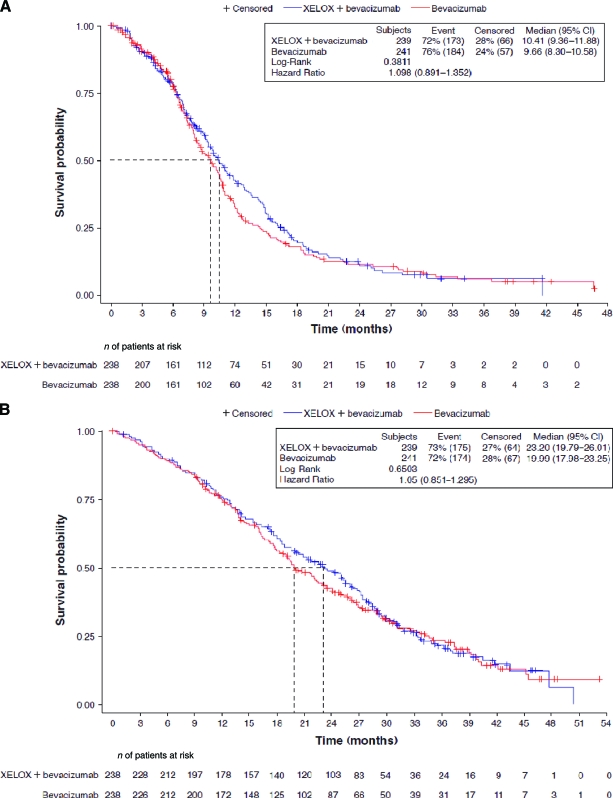
The median follow-up time was 29.0 months (range, 0–53.2 months). The median PFS interval was 10.4 months (95% CI, 9.4–11.9 months) in the XELOX plus bevacizumab group and 9.7 months (95% CI, 8.3–10.6 months) in the single-agent bevacizumab group (HR, 1.10; 95% CI, 0.89–1.35) (Fig. 2A). This difference was not statistically significant (p = .38). However, because the predefined noninferiority limit was 1.32 for the HR for the median PFS time, we could not conclude that single-agent bevacizumab was noninferior to XELOX plus bevacizumab.
Figure 2.
Progression-free survival (A) and overall survival (B) in the intent-to-treat population.
Abbreviations: CI, confidence interval; XELOX, capecitabine plus oxaliplatin.
There was no statistically significant difference in the median OS times: 23.2 months (95% CI, 19.8–26.0 months) in the XELOX plus bevacizumab group and 20.0 months (95% CI, 18.0–23.3 months) in the single-agent bevacizumab group (HR, 1.05; 95% CI, 0.85–1.30; p = .65) (Fig. 2B).
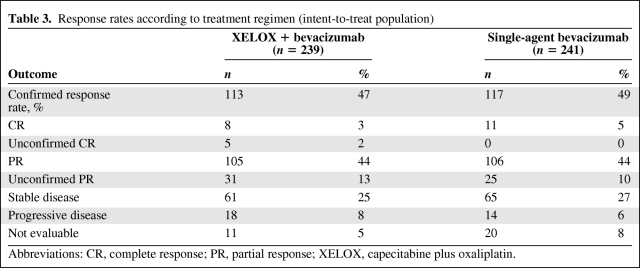
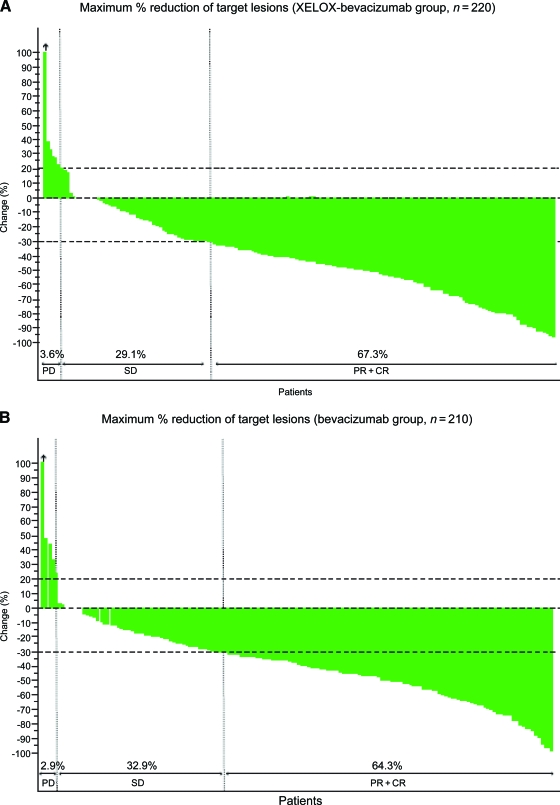
Response to treatment is summarized in Table 3. Confirmed response rates (RRs) were similar in the two treatment groups (47% for XELOX plus bevacizumab versus 49% for single-agent bevacizumab; odds ratio, 0.95; 95% CI, 0.66–1.36). Individual responses to treatment are shown in Figure 3.
Table 3.
Response rates according to treatment regimen (intent-to-treat population)
Abbreviations: CR, complete response; PR, partial response; XELOX, capecitabine plus oxaliplatin.
Figure 3.
Waterfall plot of maximum percentage reduction in target lesions with capecitabine and oxaliplatin (XELOX) plus bevacizumab (n = 220) (A) and with single-agent bevacizumab (n = 210) (B) following six cycles of XELOX plus bevacizumab.
Abbreviations: CR, complete response; PD, progressive disease; PR, partial response; SD, stable disease; XELOX, capecitabine plus oxaliplatin.
The median duration of response was 11.0 months (95% CI, 8.7–12.0 months) in the XELOX plus bevacizumab arm and 8.3 months (95% CI, 7.1–9.5 months) in the single-agent bevacizumab group, which again was not significantly different between groups (HR, 1.17; 95% CI, 0.90–1.54; p = .25). The tumor control rates (RR + SD) were similar in the two arms (73% versus 76%). The median TTR were also similar, at 4.0 months (95% CI, 3.6–4.1 months) in the XELOX plus bevacizumab arm and 3.9 months (95% CI, 3.6–4.1 months) in the single-agent bevacizumab arm (HR, 0.98; 95% CI, 0.78–1.23; p = .86).
The proportions of patients receiving second and further lines of therapy were similar in the two groups: 72% and 74% of patients in the XELOX plus bevacizumab and single-agent bevacizumab groups, respectively, received second-line therapy; 41% and 42%, respectively, received third-line therapy; and 17% of patients in both groups received four or more lines of therapy. Twenty-nine patients (12%) in the XELOX plus bevacizumab group underwent salvage surgery (liver, n = 26; lung, n = 2; other sites, n = 1), 22 of whom had an R0 resection; 25 patients (10%) in the single-agent bevacizumab arm had salvage surgery (liver, n = 19; lung, n = 3; other sites, n = 3), 15 of whom had an R0 resection. The median time to surgery was 6.7 months (range, 3.1–30.0 months) in the XELOX plus bevacizumab group and 8.8 months (range, 3.8–17.6 months) in the single-agent bevacizumab group.
Safety
Patients discontinued the study for the following reasons: disease progression in 112 patients (47%) in the XELOX plus bevacizumab group and 127 patients (53%) in the single-agent bevacizumab group and premature withdrawal in 124 (52%) and 112 (46%) patients, respectively. The most common reasons for premature withdrawal were toxicity/adverse events or intercurrent illness in 51 patients (41%) in the XELOX plus bevacizumab group and 52 patients (46%) in the single-agent bevacizumab group, surgery in 35 (28%) and 28 (25%) patients, respectively, death in 12 (10%) and nine (8%) patients, respectively, and the patient's decision in 13 (10%) and five (4%) patients, respectively. Three patients in the XELOX plus bevacizumab group and two patients in the single-agent bevacizumab group remain on treatment.
Oxaliplatin doses were reduced or suspended in 11.5% of cycles in the XELOX plus bevacizumab arm and 4.8% of cycles in the single-agent bevacizumab arm, primarily as a result of peripheral neuropathy (52%). Capecitabine doses were reduced or suspended in 7.9% of cycles in the XELOX plus bevacizumab arm and 12.3% of cycles in the single-agent bevacizumab arm, with the most common causes being hand–foot syndrome (17%) and diarrhea (25%). Bevacizumab doses were suspended in 2.9% of cycles in both treatment arms, primarily as a result of weight loss (42%).
During the maintenance phase, oxaliplatin doses were reduced in 20% of patients in the XELOX plus bevacizumab group, primarily as a result of peripheral neuropathy (65%). Capecitabine doses were reduced in 19% of patients, the most common causes of which were hand–foot syndrome (33%) and diarrhea (18%).
Treatment-related grade 3 or 4 adverse events were reported in 132 patients (55%) in the XELOX plus bevacizumab group and 114 patients (47%) in the single-agent bevacizumab group. Serious treatment-related adverse events were reported in 34 patients (14%) in the XELOX plus bevacizumab group and 47 patients (20%) in the single-agent bevacizumab group.
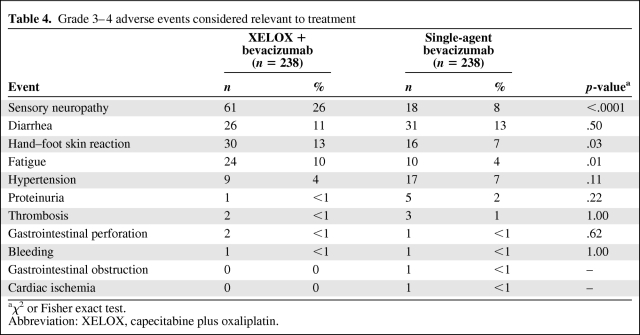
Grade 3 or 4 adverse events related to treatment are summarized in Table 4. Sensory neuropathy, hand–foot syndrome, and fatigue were statistically significantly more common in patients in the XELOX plus bevacizumab group than in the single-agent bevacizumab group, whereas there was a trend toward a higher incidence of hypertension in the single-agent bevacizumab group (not statistically significant).
Table 4.
Grade 3–4 adverse events considered relevant to treatment
aχ2 or Fisher exact test.
Abbreviation: XELOX, capecitabine plus oxaliplatin.
Adverse events resulting in death occurred in 11 patients (5%) in the XELOX plus bevacizumab group and 17 patients (7%) in the single-agent bevacizumab group. Deaths were considered remotely, possibly, or probably related to treatment in four patients in the XELOX plus bevacizumab group (gastrointestinal perforation, n = 2; enteritis, n = 1; death not otherwise specified, n = 1) and eight patients in the single-agent bevacizumab group (gastrointestinal perforation, n = 1; rectal perforation, n = 1; diarrhea, n = 1; gastrointestinal/other, n = 2; cardiopulmonary arrest, n = 1; gastrointestinal obstruction, n = 1; death not otherwise specified, n = 1). Four deaths in the XELOX plus bevacizumab group and six in the single-agent bevacizumab group occurred within 60 days of the last treatment administration.
Discussion
New chemotherapeutic and biologic agents, which prolong survival in patients with mCRC, present physicians with new challenges. With the availability of these agents, patients may require treatment for longer periods than ever before, which calls into question the optimum sequence and duration of treatment. Recent studies in patients with mCRC have investigated a variety of approaches to treatment, including intermittent chemotherapy [19], stop-and-go therapy [18, 21, 24, 25], and low-intensity maintenance strategies [20, 21], with the aim of reducing the burden of treatment for patients. The present study is, however, the first study to investigate the role of maintenance with a biological agent alone as part of the treatment regimen.
The results from this study indicate that noninferiority in terms of the PFS interval cannot be confirmed for single-agent bevacizumab maintenance compared with XELOX plus bevacizumab maintenance after induction therapy with six cycles of XELOX plus bevacizumab, because the upper limit of the 95% CI was greater than the prespecified limit of 1.32. However, a detriment in the median PFS duration of >3 weeks can be excluded. The PFS results obtained in both arms of our study are consistent with data reported from other studies using combinations of chemotherapy with bevacizumab [9, 10, 26] or with cetuximab or panitumumab in the wild-type KRAS population [27–29].
Additionally, in our study, there were no statistically significant differences in the median OS time or confirmed RR between patients who received single-agent bevacizumab and those who received XELOX plus bevacizumab. These findings mirror those from other studies using less intensive maintenance chemotherapy, such as 5-FU alone, after initial therapy. Indeed, this approach was used in the Optimized Leucovorin-Fluorouracil-Oxaliplatin (OPTIMOX)1 study, which demonstrated that oxaliplatin could be discontinued without adverse consequences after six cycles of 5-FU, leucovorin, and oxaliplatin (FOLFOX) in patients with mCRC [21].
Interestingly, the results obtained in the control arm of the MACRO study (with XELOX plus bevacizumab until progression) compare favorably with those obtained in a previous study performed by our TTD group using XELOX alone [1], with a longer median PFS duration (10.4 months versus 8.9 months), longer median OS time (23.2 months versus 18.1 months), and higher confirmed RR (47% versus 37%). The current findings are also comparable with those from other trials and observational studies [9, 10, 14, 15, 17].
One of the major issues with long-term therapy for patients with mCRC is the cumulative neuropathy associated with oxaliplatin use, hence the need to limit the dose administered over the treatment continuum. In the present study, grade 3 or 4 sensory neuropathy was statistically significantly less common in patients who received maintenance therapy with single-agent bevacizumab than in those who received XELOX plus bevacizumab (8% versus 26% of patients; p < .0001). Analysis of the dose intensity of oxaliplatin in the maintenance XELOX plus bevacizumab group indicated that patients continued to receive this component of treatment during the maintenance phase. There were also statistically significantly lower incidences of hand–foot syndrome and fatigue in the single-agent bevacizumab group, although the incidences of hypertension and diarrhea were numerically, but not statistically significantly, greater in these less intensively treated patients.
Another issue to be addressed with long-term therapy is the rate of discontinuation from such treatment plans. Despite the use of single-agent bevacizumab as maintenance therapy, the rate of discontinuation was ∼50% of patients in both arms of the study. Interestingly, a substantial proportion of discontinuations was related to surgery that was either planned or performed, including resection of primary tumors and metastases, which was a protocol-specified reason for withdrawal from the study. This is an aspect of maintenance treatment that warrants further examination in clinical trials.
A potential criticism of the trial could be that it was not sufficiently powered to answer the question about noninferiority. Although the primary endpoint of this study was not met and noninferiority of single-agent bevacizumab versus XELOX plus bevacizumab could not be claimed, the results suggest that maintenance therapy with single-agent bevacizumab may be an appropriate treatment option following induction treatment with XELOX plus bevacizumab in patients with mCRC. These findings provide further support for the deintensification of therapy in patients with mCRC while maintaining administration of a well-tolerated agent after the initial intensive treatment phase. Chemotherapy-free maintenance treatment has the potential to offer patients better quality of life (QoL) than more intensive treatment, although well-conducted QoL studies are required to demonstrate this.
Our trial suggests that a maintenance strategy with single-agent bevacizumab after induction with XELOX plus bevacizumab for six cycles may be a valid option in this setting, without compromising the PFS interval, OS time, RR, duration of response, or surgical treatment of metastases, with an important lower incidence of certain toxicities, such as neuropathy, hand–foot syndrome, and fatigue.
Information from ongoing studies evaluating maintenance treatment with bevacizumab after standard chemotherapy in mCRC patients (Double Inhibition, Reintroduction, Erlotinib, Avastin, metastatic CRC study (DREAM), Capecitabine, Irinotecan, Oxaliplatin study (CAIRO)-3, Arbeitsgemeinschaft Internistische Onckologie Groups (AIO)-ML21768 studies) will be important in determining how best to optimize efficacy and minimize side effects in this patient population. Each of these studies includes a QoL assessment as a secondary endpoint and will help quantify the benefits for patients of more versus less intensive maintenance regimens.
In conclusion, although the MACRO study did not meet its primary endpoint of noninferiority, the results suggest that single-agent bevacizumab after six cycles of XELOX plus bevacizumab may be a potential alternative to continued XELOX plus bevacizumab for patients with mCRC.
See the accompanying commentary on pages 9–10 of this issue.
Acknowledgments
The physicians listed below cared for the patients in this study. The authors thank them for their cooperation and support: E. Aranda and A. Gómez. (H. Reina Sofía); B. Massutí and A. Yuste (H. General Universitario de Alicante); E. Díaz Rubio and J. Sastre (H. Universitario Clínico San Carlos); A. Abad (ICO. H. Germans Trias i Pujol); M. Valladares (C. H. Universitario Juan Canalejo); F. Rivera (H. Marqués de Valdecilla); Ma J. Safont (H. General Universitario de Valencia); P. Martínez de Prado (H. de Basurto); M. Gallén (H. del Mar); E. González (H. Virgen de las Nieves); M. Benavides (H. Universitario Carlos Haya); E. Marcuello (H. Santa Creu i Sant Pau); C. Fernández-Martos(Instituto Valenciano de Oncología); F. Losa (H. General de L'Hospitalet); P. Escudero (H. C. Universitario Lozano Blesa); A. Cervantes (H. Clínico de Valencia); A. Arrivi (F. H. Son Llatzer); R. Dueñas (H. Ciudad de Jaén); A. Lacasta (H. de Donostia); M. Llanos (H. Universitario de Canarias); A. López-Ladrón (H. Nuestra Señora de Valme); A. Anton (H. Miguel Servet); J. Ma. Tabernero (H. Universitari Vall d'Hebrón); J. Remón (H. de Mataró); C. Martín and S. Albiol (H. del Espíritu Santo); J. Ma. Vicent and A. Galán (H. de Sagunto); H. Manzano (H. Son Dureta); J. Alfaro (C. Sanitari de Terrasa); Ma. J. Gómez (H. Puerta del Mar); T. García (H. Morales Meseguer); A. Velasco (H. Universitario de la Princesa); J. L. García López (H. Ramón y Cajal); D. Almenar (H. Dr. Peset); R. Vera (H. de Navarra); E. Jiménez (H. Jerez de la Frontera); A. Carrato and A. Rodriguez Lescure (H. General Universitario de Elche); J. L. García Puche (H. Clínico San Cecilio); J. García-Foncillas (C. Universitaria de Navarra); V. Alberola (H. Arnau de Vilanova); M. Constenla (Complejo Hospitalario Pontevedra); A. Etxeberría (Instituto Oncológico); P. Bueso (H. de Barbastro); T. Checa (I. de Oncología Corachàn); E. Cabrera, L. del Río, and A. Oltra (H. Virgen de los Lirios); A. Ruiz (H. de Fuenlabrada); C. Alonso (H. General de Albacete).
TTD Data Center: I. Ruiz de Mena and S. Rodríguez; Statistics and Data Management: Pivotal: N. Martin and J.J. García; Monitoring: Dynamic Solutions: A. Ríos and A. Sotés; Sponsors: Roche: B. Bendahmane and G. Garcia; Sanofi-Aventis: O. Diez and X. Marfí.
Supported by the Spanish Cooperative Group for the Treatment of Digestive Tumors (TTD), Madrid, Spain. Financial support for this research trial was provided by Roche and Sanofi-Aventis.
Presented in part at the 2010 American Society of Clinical Oncology Annual Meeting, June 4–8, 2010, Chicago, IL, and the 12th World Congress on Gastrointestinal Cancer, June 30–July 3, 2010, Barcelona, Spain.
Footnotes
- (C/A)
- Consulting/advisory relationship
- (RF)
- Research funding
- (E)
- Employment
- (H)
- Honoraria received
- (OI)
- Ownership interests
- (IP)
- Intellectual property rights/inventor/patent holder
- (SAB)
- Scientific advisory board
Author Contributions
Conception/Design: Eduardo Díaz-Rubio, Enrique Aranda
Provision of study material or patients: Eduardo Díaz-Rubio, Auxiliadora Gómez-España, Bartomeu Massuti, Javier Sastre, Albert Abad, Manuel Valladares, Fernando Rivera, María J. Safont, Purificación Martínez de Prado, Manuel Gallén, Encarnación González, Eugenio Marcuello, Manuel Benavides, Carlos Fernández-Martos, Ferrán Losa, Pilar Escudero, Antonio Arrivi, Andrés Cervantes, Rosario Dueñas, Amelia López-Ladrón, Adelaida Lacasta, Marta Llanos, Jose M. Tabernero, Antonio Antón, Enrique Aranda
Collection and/or assembly of data: Eduardo Díaz-Rubio, Auxiliadora Gómez-España, Bartomeu Massuti, Javier Sastre, Albert Abad, Manuel Valladares, Fernando Rivera, María J. Safont, Purificación Martínez de Prado, Manuel Gallén, Encarnación González, Eugenio Marcuello, Manuel Benavides, Carlos Fernández-Martos, Ferrán Losa, Pilar Escudero, Antonio Arrivi, Andrés Cervantes, Rosario Dueñas, Amelia López-Ladrón, Adelaida Lacasta, Marta Llanos, Jose M. Tabernero, Antonio Antón, Enrique Aranda
Data analysis and interpretation: Eduardo Díaz-Rubio, Enrique Aranda
Manuscript writing: Eduardo Díaz-Rubio, Auxiliadora Gómez-España, Bartomeu Massuti, Javier Sastre, Albert Abad, Manuel Valladares, Fernando Rivera, María J. Safont, Purificación Martínez de Prado, Manuel Gallén, Encarnación González, Eugenio Marcuello, Manuel Benavides, Carlos Fernández-Martos, Ferrán Losa, Pilar Escudero, Antonio Arrivi, Andrés Cervantes, Rosario Dueñas, Amelia López-Ladrón, Adelaida Lacasta, Marta Llanos, Jose M. Tabernero, Antonio Antón, Enrique Aranda
Final approval of manuscript: Eduardo Díaz-Rubio, Auxiliadora Gómez-España, Bartomeu Massuti, Javier Sastre, Albert Abad, Manuel Valladares, Fernando Rivera, María J. Safont, Purificación Martínez de Prado, Manuel Gallén, Encarnación González, Eugenio Marcuello, Manuel Benavides, Carlos Fernández-Martos, Ferrán Losa, Pilar Escudero, Antonio Arrivi, Andrés Cervantes, Rosario Dueñas, Amelia López-Ladrón, Adelaida Lacasta, Marta Llanos, Jose M. Tabernero, Antonio Antón, Enrique Aranda
The authors take full responsibility for the content of the paper but thank Lee Miller (Miller Medical Communications, supported by Roche Farma S.A.) for copyediting/proofreading (e.g., grammatical assistance, stylistic suggestions to outline or draft), editorial assistance (e.g. preparing references, fact checking, labelling illustrations or tables), and production assistance (e.g., assembling tables, graphs, figures, photos, or other illustrations).
References
- 1.Díaz-Rubio E, Tabernero J, Gómez-España A, et al. Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: Final Report of the Spanish Cooperative Group for the Treatment of Digestive Tumors trial. J Clin Oncol. 2007;25:4224–4230. doi: 10.1200/JCO.2006.09.8467. [DOI] [PubMed] [Google Scholar]
- 2.Porschen R, Arkenau HT, Kubicka S, et al. Phase III study of capecitabine plus oxaliplatin compared with fluorouracil and leucovorin plus oxaliplatin in metastatic colorectal cancer: A final report of the AIO Colorectal Study Group. J Clin Oncol. 2007;25:4217–4223. doi: 10.1200/JCO.2006.09.2684. [DOI] [PubMed] [Google Scholar]
- 3.Cassidy J, Clarke S, Díaz-Rubio E, et al. Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folinic acid plus oxaliplatin as first-line therapy for metastatic colorectal cancer. J Clin Oncol. 2008;26:2006–2012. doi: 10.1200/JCO.2007.14.9898. [DOI] [PubMed] [Google Scholar]
- 4.Hochster HS, Hart LL, Ramanathan RK, et al. Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: Results of the TREE Study. J Clin Oncol. 2008;26:3523–3529. doi: 10.1200/JCO.2007.15.4138. [DOI] [PubMed] [Google Scholar]
- 5.Martoni AA, Pinto C, Di Fabio F, et al. Capecitabine plus oxaliplatin (XELOX) versus protracted 5-fluorouracil venous infusion plus oxaliplatin (PVI-FOX) as first-line treatment in advanced colorectal cancer: A GOAM phase II randomised study (FOCA trial) Eur J Cancer. 2006;42:3161–3168. doi: 10.1016/j.ejca.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 6.Arkenau HT, Arnold D, Cassidy J, et al. Efficacy of oxaliplatin plus capecitabine or infusional fluorouracil/leucovorin in patients with metastatic colorectal cancer: A pooled analysis of randomized trials. J Clin Oncol. 2008;26:5910–5917. doi: 10.1200/JCO.2008.16.7759. [DOI] [PubMed] [Google Scholar]
- 7.Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 8.Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: A new paradigm for combination therapy. Nat Med. 2001;7:987–989. doi: 10.1038/nm0901-987. [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 10.Saltz LB, Clarke S, Díaz-Rubio E, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: A randomized phase III study. J Clin Oncol. 2008;26:2013–2019. doi: 10.1200/JCO.2007.14.9930. [DOI] [PubMed] [Google Scholar]
- 11.Giantonio BJ, Catalano PJ, Meropol NJ, et al. Eastern Cooperative Oncology Group Study E3200. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: Results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25:1539–1544. doi: 10.1200/JCO.2006.09.6305. [DOI] [PubMed] [Google Scholar]
- 12.Kabbinavar F, Hurwitz HI, Fehrenbacher L, et al. Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol. 2003;21:60–65. doi: 10.1200/JCO.2003.10.066. [DOI] [PubMed] [Google Scholar]
- 13.Kabbinavar FF, Hambleton J, Mass RD, et al. Combined analysis of efficacy: The addition of bevacizumab to fluorouracil/leucovorin improves survival for patients with metastatic colorectal cancer. J Clin Oncol. 2005;23:3706–3712. doi: 10.1200/JCO.2005.00.232. [DOI] [PubMed] [Google Scholar]
- 14.Grothey A, Sugrue MM, Purdie DM, et al. Bevacizumab beyond first progression is associated with prolonged overall survival in metastatic colorectal cancer: Results from a large observational cohort study (BriTE) J Clin Oncol. 2008;26:5326–5334. doi: 10.1200/JCO.2008.16.3212. [DOI] [PubMed] [Google Scholar]
- 15.Kozloff M, Yood MU, Berlin J, et al. Clinical outcomes associated with bevacizumab-containing treatment of metastatic colorectal cancer: The BRiTE observational cohort study. The Oncologist. 2009;14:862–870. doi: 10.1634/theoncologist.2009-0071. [DOI] [PubMed] [Google Scholar]
- 16.Kozloff MF, Berlin J, Flynn PJ, et al. Clinical outcomes in elderly patients with metastatic colorectal cancer receiving bevacizumab and chemotherapy: Results from the BRiTE observational cohort study. Oncology. 2010;78:329–339. doi: 10.1159/000320222. [DOI] [PubMed] [Google Scholar]
- 17.Van Cutsem E, Rivera F, Berry S, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: The BEAT study. Ann Oncol. 2009;20:1842–1847. doi: 10.1093/annonc/mdp233. [DOI] [PubMed] [Google Scholar]
- 18.Maughan TS, James RD, Kerr DJ, et al. Medical Research Council Colorectal Cancer Group. Comparison of intermittent and continuous palliative chemotherapy for advanced colorectal cancer: A multicentre randomised trial. Lancet. 2003;361:457–464. doi: 10.1016/s0140-6736(03)12461-0. [DOI] [PubMed] [Google Scholar]
- 19.Labianca R, Sobrero A, Isa L, et al. Italian Group for the Study of Gastrointestinal Cancer–GISCAD. Intermittent versus continuous chemotherapy in advanced colorectal cancer: A randomised ‘GISCAD’ trial. Ann Oncol. 2011;22:1236–1242. doi: 10.1093/annonc/mdq580. [DOI] [PubMed] [Google Scholar]
- 20.Grothey A, Hart L, Rowland K, et al. Intermittent oxaliplatin (oxali) administration and time-to-treatment failure (TTF) in metastatic colorectal cancer (mCRC): Final results of the phase III CONcePT trial [abstract 4010] J Clin Oncol. 2008;26(15 suppl):180. [Google Scholar]
- 21.Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: A randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-go fashion in advanced colorectal cancer—a GERCOR study. J Clin Oncol. 2006;24:394–400. doi: 10.1200/JCO.2005.03.0106. [DOI] [PubMed] [Google Scholar]
- 22.Chibaudel B, Maindrault-Goebel F, Lledo G, et al. Can chemotherapy be discontinued in unresectable metastatic colorectal cancer? The GERCOR OPTIMOX2 Study. J Clin Oncol. 2009;27:5727–5733. doi: 10.1200/JCO.2009.23.4344. [DOI] [PubMed] [Google Scholar]
- 23.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors: European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 24.Adams R, Wilson R, Seymour M, et al. Intermittent versus continuous oxaliplatin-based combination chemotherapy in patients with advanced colorectal cancer: A randomized non-inferiority trial (MRC COIN) [abstract 15LBA] Eur J Cancer. 2009;(suppl 7):259. [Google Scholar]
- 25.Tveit K, Guren T, Glimelius B, et al. Randomized phase III study of 5-fluorouracil/folinate/oxaliplatin given continuously or intermittently with or without cetuximab, as first-line treatment of metastatic colorectal cancer: The NORDIC VII study ( NCT00145314), by the Nordic Colorectal Cancer Biomodulation Group [abstract 365] J Clin Oncol. 2011;29(suppl 4):10. [Google Scholar]
- 26.Tol J, Koopman M, Cats A, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360:563–572. doi: 10.1056/NEJMoa0808268. [DOI] [PubMed] [Google Scholar]
- 27.Van Cutsem E, Khöne CH, Hiltre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1408–1417. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 28.Bokemeyer C, Bondarenko I, Makhson A, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27:663–671. doi: 10.1200/JCO.2008.20.8397. [DOI] [PubMed] [Google Scholar]
- 29.Douillard JY, Siena S, Cassidy J, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: The PRIME study. J Clin Oncol. 2010;28:4697–4705. doi: 10.1200/JCO.2009.27.4860. [DOI] [PubMed] [Google Scholar]