Abstract
Objective
To compare the efficacy of cyanoacrylate (tissue glue) placement after surgical removal of impacted mandibular third molars.
Materials and Methods
Thirty patients with bilaterally impacted mandibular third molars were studied in this controlled clinical trial. One side closure after surgical removal of third molar was done with conventional sutures and other side with cyanoacrylate.
Results
The data analysis showed that postoperative bleeding with cyanoacrylate method was less significant than with suturing on the first and second day after surgery. There was no significant difference in the severity of pain between the two methods.
Conclusion
This study suggested that the efficacy of both, cyanoacrylate and suturing in wound closure were similar in the severity of pain, but use of cyanoacrylate showed better hemostasis.
Keywords: Amcrylate, Medicated tissue glue, Polymerization, Hemostasis, Pain
Introduction
Removal of mandibular third molar is routine procedure performed in the dental office. After removal of the impacted mandibular third molar, the conventional method is to suture the surgical wound and let it heal by primary intention. Suturing in this area is not always easy; it takes time and requires good suturing skills. Besides the difficulties one faces during operative procedures with suturing methods, additional second visit is required for removal of suture. To overcome these disadvantages, an alternative to the sutures, plastic adhesives were discovered in 1949 and 10 years later COOVER et al. [1–5] reported their use in surgical procedures.
Cyanoacrylate glue is the general term for the quick-bonding super glues used as two separate liquids, one for pouring into the mold and another used sparingly as a hardener. In the case of cyanoacrylate glue, the hardener is water. If cyanoacrylate glue is placed on a dry surface the glue does not bond with the surface. But with the slightest amount of water, that could include the moisture in the air; the molecules of the glue react and form a tight chain between the two surfaces being bonded. This happens within seconds. Traditional white glues rely on evaporation to form their bonds, but cyanoacrylate glue generates its own heat for faster curing. This heat may damage the soft tissue and hamper its blood supply. To avoid this; manufacturers have incorporated long chains of methyl group due to which the polymerization [6, 7] process is elongated and the rate of heat generation prolongs. Because intraoral mucosa is naturally moist in the presence of saliva, use of cyanoacrylate glue may find itself as an involuntary participant in the bonding process.
Polymerization of the material occurs within 10–15 s. These materials are not absorbable and are sloughed from the surface of the skin and mucosa 7–10 days after adhesive application. These agents are approved for external application only and are not to be used as internal tissue adhesive because of the reactions, toxicity [8] and carcinogenicity. In the maxillofacial field, it has been used for wound closure on extraction sockets, face, sinus perforation in sinus lift [9] gingivectomy, mucogingival flaps, biopsy, superficial oral ulcerations, recurrent multiple Aphthous ulcers and leukemia, and other sites in general surgery like axilla, lungs [10], hearts [11], scalp wounds [4], circumcision [12] and perineum, trocar sites [13], as a heamostatic means to control bleeding from skin graft [14], hair transplant donor sites, cleft lip repair [7, 15] face lifts, blepharoplasty [16], brow lifts and other cosmetic surgeries and to do various anastomoses of intestine, arteries [11] and nerves [17].
This study compares silk with cyanoacrylate for wound closure after the removal of mandibular impacted third molars, evaluating the incidence of postoperative sequel of bleeding and pain. In this study we compared the conventional suturing technique with the application of Amcrylate.
Materials and Methods
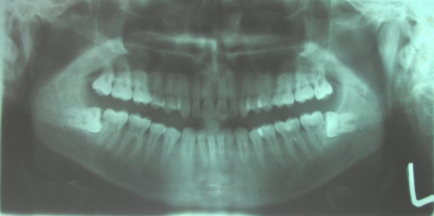
Thirty patients (19 women and 11 men; age range 20 to 32 years) with similar bilateral impacted mandibular third molars were studied in this controlled clinical trial (Fig. 1). Panoramic radiographs were taken to assess the third molar situation. Ortho-pantomograph was taken to assess third molar angulations to the long axis of second molar (Fig. 2). Inclusion criteria–
-
Patients who are having mesio-angularly or horizontally impacted mandibular third molar
(Position B Class II, PELL & GREOGERY classification 1933, with difficulty index-5).
No systemic diseases.
Non-smokers.
Not allergic to the drugs or anesthetic agent used in the surgical protocol.
Fig. 1.
Pre-operative
Fig. 2.
Panoramic radiograph
All the cases that were included had good general health and good oral hygiene. Written consent was obtained from the patients and relatives. The surgical procedures were performed by one operator in the oral and maxillofacial surgery department. Patients rinsed with 5% betadine solution, and were given no preoperative drugs. Topical lignocaine jelly was applied and the inferior alveolar, long buccal and lingual nerves were anesthetised with 2% lidocaine hydrochloride with epinephrine 1:200,000 was given (Figs. 1, 2, 3, 4, 5, 6, 7).
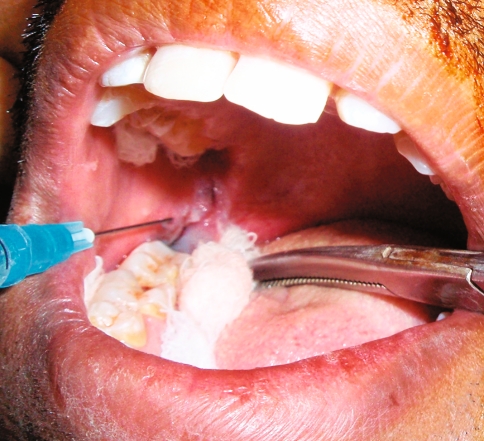
Fig. 3.
Intra-operative sutures
Fig. 4.
Intra-operative isolation for Amcrylate
Fig. 5.
After final placement of Amcrylate
Fig. 6.
One month post-operative sutures
Fig. 7.
One month post-operative Amcrylate
A full-thickness Ward’s incision was raised and flap was reflected. After adequate bone removal, the tooth was removed followed by curettage and toileting of the socket. The flap was repositioned and closed with 3-0 silk in an interrupted fashion on the left side of all patients (Fig. 3). The sutures were removed after 7 days. After 2 weeks, the same procedure was done on the right side and the flap repositioned and was isolated with sterile dry gauze. After adequate isolation, wound was closed by using two thin layers of Amcrylate (Figs. 4 and 5). The 1st layer was put on the incision line by droplet method, followed by another layer after 20 s. In this study the material used was having following specification—(medicated tissue adhesive—Iso Amyl 2-Cynoacrylate, Manufactured by Concord Drugs Ltd, dispensed in ampoules of 0.25, 0.50 and 1 ml).
All the patients received usual postoperative instructions along with application of ice packs at the operated site extraorally. Patients were advised to maintain oral hygiene from the day after surgery and mouthwash with 0.12% chlorhexidine twice daily. All patients were given similar postoperative antibiotics and analgesic (Cap. Amoxicillin 500 mg BD for 5 days and Tab. Diclofenac Sodium 50 mg BD for 3 days). Patients were kept on 1 month follow up (Figs. 6 and 7).
They were also given a pain and bleeding recording form to be completed during the following days. The patients entered the degree of pain (for 5 days) and bleeding (for 3 days) on a daily basis on the form, making reference to predefined values (Tables 1, 2, visual analog scale [VAS]). The pain scale was 5 cm long, subdivided into 5 equal parts, one end corresponding to no pain, the other to extremely severe pain.
Table 1.
Visual analog scale to evaluate pain: reference values given to patients
| 0 No pain | The patient feels well |
| 1 Mild pain | If the patient is distracted he or she does not feel the pain |
| 2 Severe pain | The patient is very disturbed but nevertheless can continue with normal activities |
| 3 Very severe pain | The patient is forced to abandon nor mal activities |
Table 2.
Visual analog scale to evaluate bleeding
| 0 No bleeding | The patient does not detect any blood in saliva |
| 1 Oozing | The patient detects slight blood but it is not very noticeable |
| (Patient notices blood over the sutured wound but it doesn’t stay for long) | |
| 2 Accidental low bleeding | The patient has low bleeding sometimes |
| (Patient notices blood over the sutured wound which stays all over the day but does not increase in volume) | |
| 3 Continues low bleeding | The patient has low bleeding often |
| (Patient notices blood with continues increase in volume) |
Table 1 shows the reference values given to patients for pain, and the corresponding clinical situations. The patients also indicated their subjective perception of bleeding on the VAS in a similar fashion. Table 2 shows the reference values given to patients for bleeding, and the corresponding clinical situations.
Results
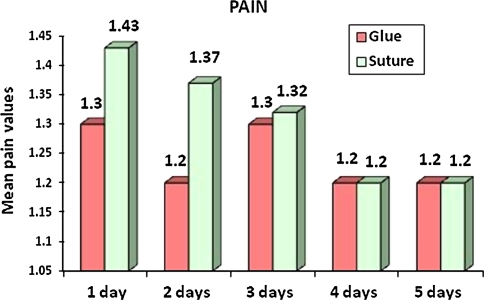
There was significant difference in the severity of pain between the two methods on the right and left sides of the mandible at all times recorded (P < 0.05). The analysis showed that the severity of pain in closure with suture was more in first 3 days and later on it became same but marked elevation in pain have been noted on the second day (Table 3, 4, 5 and Graph 1).
Table 3.
Pain: statistical analysis of data
| Day | Method | N | Mean | SE | Maximum | Minimum |
|---|---|---|---|---|---|---|
| 1 | Glue | 1.3 | 0.085 | 2 | 0 | |
| 30 | ||||||
| Suture | 1.43 | 0.087 | 2 | 0 | ||
| 2 | Glue | 1.2 | 0.078 | 2 | 0 | |
| 30 | ||||||
| Suture | 1.37 | 0.074 | 2 | 0 | ||
| 3 | Glue | 1.3 | 0.064 | 2 | 0 | |
| 30 | ||||||
| Suture | 1.32 | 0.082 | 2 | 0 | ||
| 4 | Glue | 1.2 | 0.085 | 2 | 0 | |
| 30 | ||||||
| Suture | 1.2 | 0.084 | 2 | 0 | ||
| 5 | Glue | 1.2 | 0.082 | 2 | 0 | |
| 30 | ||||||
| Suture | 1.2 | 0.082 | 2 | 0 |
Table 4.
Statistical analysis of pain
| Day | Method | N | Median | Interquartile range |
|---|---|---|---|---|
| 1 | Glue | 1.30 | 1.2 | |
| 30 | ||||
| Suture | 1.39* | 1.3 | ||
| 2 | Glue | 1.2 | 1 | |
| 30 | ||||
| Suture | 1.36* | 1 | ||
| 3 | Glue | 1.3 | 1 | |
| 30 | ||||
| Suture | 1.3 | 1 | ||
| 4 | Glue | 1.2 | 1 | |
| 30 | ||||
| Suture | 1.2 | 1 | ||
| 5 | Glue | 1.2 | 1 | |
| 30 | ||||
| Suture | 1.2 | 1 |
* Significant, P < 0.05
Table 5.
Bleeding: statistical analysis of data
| Day | Method | N | Mean | SE | Maximum | Minimum |
|---|---|---|---|---|---|---|
| 1 | Glue | 0 | 0 | 0 | 0 | |
| 30 | ||||||
| Suture | 0.17 | 0.0013 | 1 | 0 | ||
| 2 | Glue | 0 | 0 | 0 | 0 | |
| 30 | ||||||
| Suture | 0 | 0 | 0 | 0 | ||
| 3 | Glue | 0 | 0 | 0 | 0 | |
| 30 | ||||||
| Suture | 0 | 0 | 0 | 0 |
Graph 1.
Bar diagram showing the severity of pain in 1st to 5th post operative day using sutures and Amcrylate
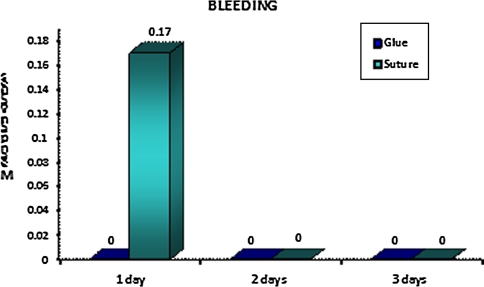
The data analysis showed that postoperative bleeding with the cyanoacrylate adhesive method was less significant than with suturing on the first and second days after surgery (P < 0.05); however, the bleeding index showed no significant difference (P < 0.05) between the two methods on the third day [Tables 5, 6 and Graph 2]. Patients were unable to make any significant remarks over the bleeding on 3rd postoperative day
Table 6.
Bleeding: statistical analysis of data
| Day | Method | N | Median | Interquartile range |
|---|---|---|---|---|
| 1 | Glue | 1.30 | 0 | |
| 30 | ||||
| Suture | 1 | 1 | ||
| 2 | Glue | 0 | 0 | |
| 30 | ||||
| Suture | 0 | 0 | ||
| 3 | Glue | 0 | 0 | |
| 30 | ||||
| Suture | 0 | 0 |
Graph 2.
Diagram showing the bleeding from 1st to 3rd post operative day using sutures and Amcrylate
Discussion
The severity of pain and bleeding are indicators of a patient’s comfort during the postoperative period after third molar removal. Cyanoacrylate can be used for mucosal closure. This adhesive can eliminate the need for suture placement and suture removal.
In 2006, Waite and Cherala [2] demonstrated good results and fewer complications after third molar surgery with the sutureless method. These studies examined open wound or small foramenae with the suturing method resulting in better drainage and reduced pain, although in our study, the pain experienced by the tissue glue group was less as compared to that of the suture group patients on second postoperative day. The same was noted by Ellis et al. in 1993 where the cyanoacrylate group experienced reduced pain after wound closure. The results of our study showed the marked significant difference in the severity of pain in both the groups for first 3 days, where the severity was found to be maximum on 2nd day in sutured group. On the 4th and 5th day, there were no significant difference in both the groups. This may be due to the less tissue handling and less tissue inflammation in Amcrylate group. Regarding bleeding, the Amcrylate group was found to be superior significantly, as no signs of bleeding were seen, but in sutured group at least 5 out of 30 had complained and they reported with blood ooze from sutured wound on 1st postoperative day. The reason found was they didn’t follow postoperative instructions effectively and two of them smoked cigarettes one kept on spitting while other two used straw to have juice. Although patients were informed not to use the operated site for chewing on the first postoperative day they had food lodgment over the sutures and they tried to clean them by rinse, which was not advised for 36 h after sutures were placed. No significant difference seen in both groups on 2nd and 3rd postoperative day.
However, the skin adhesives have limitations in certain clinical situations like,
When too much of lateral tension across the wound is present.
Where dry surface cannot be achieved.
Infected surgical site.
Large dead spaces underneath the closure.
Our study concluded that cyanoacrylate is a better alternative for intaoral minor surgical procedures as tissue glue, was found to be haemostatic in nature, was helpful in reduction of pain and patients need not visit again for suture removal. Even this procedure was comfortable for the surgeon.
References
- 1.Ghoreishian M, Gheisari R, Fayazi M. Tissue adhesive and suturing for closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e14–e16. doi: 10.1016/j.tripleo.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Waite P, Cherala S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. J Oral Maxillofac Surg. 2006;64:669–673. doi: 10.1016/j.joms.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Singer AJ, Quinn JV, Hollander JE. The cyanoacrylate topical skin adhesives. Am J Emerg Med. 2008;26:490–496. doi: 10.1016/j.ajem.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Morton RJ, Gibson MF, Sloan JP. The use of histoacryl tissue adhesive for the primary closure of scalp wounds. Arch Emerg Med. 1988;5:110–112. doi: 10.1136/emj.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kulkarni S. Healing of periodontal flaps when closed with silk sutures and N-butyl cyanoacrylate: a clinical and histological study. Indian J Dental Res. 2007;18(2):72–77. doi: 10.4103/0970-9290.32424. [DOI] [PubMed] [Google Scholar]
- 6.Toriumi DM, O’Grady K, Desai D, Bagal A. Use of octyl-2-cyanoacrylate for skin closure in facial plastic surgery. Plast Reconstr Surg. 1998;102(6):2209–2219. doi: 10.1097/00006534-199811000-00062. [DOI] [PubMed] [Google Scholar]
- 7.Daniel Knott P, Zins JE, Banbury J, Djohan R, Yetman RJ, Papay F. A comparison of dermabond tissue adhesive and sutures in the primary repair of the congenital cleft lip. Ann Plast Surg. 2007;58(2):121–125. doi: 10.1097/01.sap.0000232984.68797.62. [DOI] [PubMed] [Google Scholar]
- 8.Dean M Toriumi; Wasim F Raslan, Michael Friedman, M. Eugene Tardy, Jr. (1991) Variable histotoxicity of histoacryl when used in a subcutaneous site: an experimental study. Laryngoscope 101: 339–343 [DOI] [PubMed]
- 9.Choi B-H, Kim B-Y, Huh J-Y, Lee S-H, Zhu S-J, Jung J-H, Li J. Cyanoacrylate adhesive for closing sinus membrane perforations during sinus lifts. J Cranio-Maxillofacial Surg. 2006;34:505–509. doi: 10.1016/j.jcms.2006.07.859. [DOI] [PubMed] [Google Scholar]
- 10.Petrovsky BV, Gigaury VS, Milonov OB, Perelman MI, Mlinchik VE, Gotye SV, Safarov IS. MD Surgical application of tissue adhesives. World J Surg. 1980;4:331–356. doi: 10.1007/BF02393395. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan M, Bozkurt S, Kut MS, Kullu S, Demirtas MM. Histopathological effects of ethyl 2-cyanoacrylate tissue adhesive following surgical application: an experimental study. Eur J Cardiothorac Surg. 2004;25:167–172. doi: 10.1016/j.ejcts.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 12.Arunachalam P, King PA, Orford J. A prospective comparison of tissue glue versus sutures for circumcision. Pediatr Surg Int. 2003;19:18–19. doi: 10.1007/s00383-002-0893-1. [DOI] [PubMed] [Google Scholar]
- 13.Rosin D, Rosenthal RJ, Kuriansky J, Brasesco O, Shabtai M, Ayalon A. Closure of laparoscopic trocar site wounds with cyanoacrylate tissue glue: a simple technical solution. J Laparoendosc Adv Surg Tech. 2001;11(3):157. doi: 10.1089/10926420152389305. [DOI] [PubMed] [Google Scholar]
- 14.Adler N, Nachumovsky S, Meshulam-Derazon S, Ad-El D (2007) Skin graft fixation with cyanoacrylate tissue adhesive in burn patients. BURNS 33:803 [DOI] [PubMed]
- 15.Mourougayan V. Sutureless skin closure for cleft lip repair. Cleft Palate-Craniofacial J. 2006;43(6):656–658. doi: 10.1597/05-171. [DOI] [PubMed] [Google Scholar]
- 16.Perin LF, Helene A, Jr, Fraga MF. Sutureless closure of the upper eyelids in blepharoplasty: use of octyl-2-cyanoacrylate. Aesthet Surg J. 2009;29:87–92. doi: 10.1016/j.asj.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Elgazzar RF, Abdulmajeed I, Mutabbakani M. Cyanoacrylate glue versus suture in peripheral nerve reanastomosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;104:465–472. doi: 10.1016/j.tripleo.2007.01.019. [DOI] [PubMed] [Google Scholar]