Abstract
Background
Genioplasty is often performed to esthetically improve patient’s profiles in the lower facial third. Many factors account for the variability in soft tissue response like dissection technique, magnitude and direction of movement and stability of the genial segment. Optimum treatment planning thus requires an understanding of the soft tissue response to various genial procedures.
Aims and Objective
To determine the stability, ratio of hard and soft tissues and changes in the lower facial profile after advancement genioplasty.
Materials and Methods
Ten patients were evaluated cephalometrically for the soft tissue changes in relation to hard tissues after advancement genioplasty. Pre operative, immediate post operative and 6 months post operative lateral cephalogram were taken. Pre operative tracings were superimposed with post operative cephalograms to produce a composite tracing. Changes in the osseous tissues are assessed and related to the net changes in the soft tissues.
Results
The ratio of horizontal changes of osseous to soft tissues was found to be 1:0.89. The mean resorption was 0.85 mm (10.7%). The vertical changes are minimal and non significant. There are significant changes in the soft tissue profile such as decrease in the soft tissue thickness, facial convexity angle, lower facial submental angle and increase in mentolabial sulcus depth.
Conclusion
The standard advancement genioplasty procedure by inferior osteotomy of the chin with broadest musculo–periosteal pedicle with rigid internal fixation was followed. The soft tissue response is almost equal to the bony movement. The stability of the hard tissues is good with minimum amount of resorption so as to achieve more predictable results.
Keywords: Genioplasty, Soft tissue changes, Cephalometry, Prediction
Introduction
Osteotomies to correct deformities and anomalies of maxillo-mandibular complex produce changes in the shape and position of the soft tissues [1]. Although the dental and skeletal relationships are the strongest indicators of a perceived need for surgery, the soft tissue profile has emerged as perhaps the most important consideration for planning surgery and assessing treatment outcomes.
Hofer in 1942 was the first to describe the horizontal genial osteotomy through extraoral approach which was later modified by Trauner and Obwegesser in 1957 through intraoral approach. Since then the symphysis has been exposed both intraorally and extraorally for osteotomy of inferior border of mandible to advance, reduce, widen, narrow, lengthen or shorten the chin [2].
Despite of fact that genioplasty has been considered a very stable procedure there are many factors that account for the variability in soft tissue response like the dissection technique, magnitude of movement, the amount of soft tissue degloving. Stability of the mobilized segment is affected by suprahyoid musculature and perimandibular connective tissue attachments, osseous remodeling and resorption patterns [3].
Optimal treatment planning thus requires an understanding of the soft tissue response to various genial procedures. Evaluation of submental-cervical esthetics is also vital in the treatment planning. Cephalometric tracing superimposition continuously plays an important role in evaluation of treatment, progress and surgical outcomes in the orthognathic surgeries [4].
The three fold purpose of this study is to assess changes in the bony architecture and position after horizontal mandibular osteotomy, to relate these changes to net changes in the soft tissue profile and to develop predictive criteria for treatment planning.
Materials and Methods
This study pertaining to correction of obvious chin deformity and enhancement of facial esthetics was conducted on the patients reporting to the Department of Oral and Maxillofacial Surgery, PMNM Dental College and Hospital, Bagalkot.
The study was conducted on 10 patients with the informed consent of the patient as well as clearance from the ethical committee of the institution. The age group of the patients ranged from 21 to 25 years; with a mean of 22 years. Out of 10 patients, 6 were females and 4 were males. All patients underwent exclusively advancement genioplasty by horizontal inferior osteotomy of the chin retaining the broadest musculo-periosteal pedicle with rigid internal fixation. The mean follow up period was 9.2 months, ranging from 6 to 12 months.
Criteria for Selection of Patients
Patients presenting with retrognathic chin for which surgical intervention is necessary.
Patients with their completed growth.
Patients with natural dentition supporting the lips.
No history of congenital deformities, syndromes and other systemic diseases.
Patients who do not require any concurrent surgery in the mandible at the time of genioplasty.
The pre operative diagnosis of chin deficiency was assessed on lateral cephalograms using COGS (Cephalometrics for Orthognathic surgeries) analysis by Burstone et al. [5]. Treatment planning was done according to the diagnosis.
Routine standard lateral cephalograms were taken following standard lateral cephalometric norms as follows: (1) pre operatively one week before surgery; (2) immediate post operatively one week after surgery, (3) late post operatively after minimum of 6 months follow up (Figs. 1, 2, 3).
Fig. 1.
Preoperative lateral cephalogram
Fig. 2.
Immediate post operative lateral cephalogram
Fig. 3.
Long term post operative lateral cephalogram
Surgical Procedure
All the cases were operated under general anesthesia with naso-endotracheal intubation following aseptic technique. A classical translabial incision through the lower lip mucosa midway between the depth of the labial vestibule and vermilion border of the lower lip extending from the first premolar to the first premolar was placed. A broad soft tissue pedicle is maintained to the anterior and inferior surfaces of the genial segment by detaching only enough periosteum from it to facilitate the planned horizontal osteotomy and repositioning of the segment.
A midline vertical reference line is inscribed into the mid sagittal plane of the symphysis across the area of planned osteotomy. Mental nerve and the contiguous soft tissue flap is retracted and protected. The horizontal osteotomy cut was extended laterally and posteriorly using bur or saw blade. After completing the osteotomy, the inferior segment pedicled to geniohyoid and digastric muscles is advanced according to the preoperative cephalometric planning.
The repositioned genial segment is fixed to the body of the mandible with bone screws and chin plates. A two layered closure of the soft tissue is achieved with interrupted 3-0 chromic catgut suture to approximate periosteum, muscle and submucosa, 3-0 mersilk suture to close the mucosal incision.
Method of Analysis
Evaluation of the cephalometric changes of hard and soft tissues of the chin area was done by Park et al. [6] method of analysis. The pre operative cephalograms were traced on 0.3 mm thick translucent acetate tracing paper with 0.3 mm lead pencil. It is then superimposed on the immediate post operative and follow up cephalogram along unaltered mandibular landmarks like lingual border of symphysis, inferior mandibular border, ramus, restorations, brackets of teeth and cranial land marks like basion, nasion, sella. This produced a single composite tracing for each patient that allowed serial observation and measurement of positional changes of hard and soft tissues of the chin.
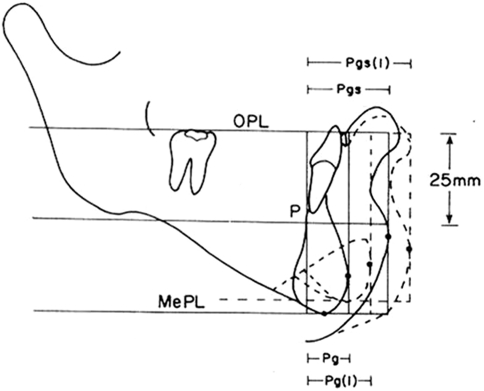
The pre operative tracing includes the following reference lines, planes and measurements (Fig. 4).
OPL (Occlusal plane)––a horizontal plane tangent to the uppermost convex area of a definite radiopaque body (dental filling, orthodontic band or bracket) of the most posterior tooth and of the orthodontic bracket of the most anterior tooth of the mandible.
MePL (Menton horizontal plane)––a horizontal plane parallel to OPL and tangent to hard tissue menton (Me).
P (Point p; Posterior reference point)––a point where perpendicular line to OPL and MePL crosses the posterior aspect of the inner (lingual) cortex of the symphysis 25 mm below the OPL.
Pg (Hard tissue Pogonion)––the most anterior point on the symphysis of mandible tangent to a perpendicular line drawn from OPL.
Pgs (Soft tissue Pogonion)––the most anterior point of the soft tissue chin tangent to a perpendicular line drawn from OPL.
Me (Hard tissue Menton)––the most inferior point of the symphysis of the mandible.
Si (Mento-labial sulcus)––the point of greatest concavity in the midline between lower lip (Li) and chin (Pg).
Li (Labrale inferius)––a point indicating the mucocutaneous border of the lower lip.
G (Glabella)––the most prominent point in the mid sagittal plane of the forehead.
Sn (Sub nasale)––the point at which the nasal septum merges with the upper cutaneous lip in the mid sagittal plane.
Gns (Soft tissue Gnathion)––the constructed midpoint between soft tissue pogonion and soft tissue menton.
C (Cervical point)––the inner most point between the submental area and the neck.
Fig. 4.
Park’s method of analysis
The measurements analyzed were as follows:
Horizontal position of the hard tissue chin (P–Pg)––the distance from the point P to hard tissue pogonion (Pg) parallel to occlusal plane (OPL).
Vertical position of inferior aspect of the hard tissue chin (OPL–MePL)––the perpendicular distance from the occlusal plane (OPL) to menton horizontal plane (MePL).
Horizontal position of the soft tissue chin (P–Pgs)––distance from point p to soft tissue pogonion (Pgs) parallel to occlusal plane (OPL).
Overall horizontal thickness of the soft tissue chin (Pg–Pgs)––the distance from hard tissue pogonion (Pg) to soft tissue pogonion (Pgs) parallel to occlusal plane (OPL).
Soft tissue facial convexity angle (G–Sn–Pgs) (Fig. 5)
Mentolabial sulcus depth [Si–(Li–Pgs)] (Fig. 6)
Lower facial submental angle (Li–Gns–C) (Fig. 7)
Fig. 5.
Facial convexity angle
Fig. 6.
Mentolabial sulcus depth
Fig. 7.
Lower facial submental angle
The displacements of these points resulting following surgery was derived by calculating the difference between preoperative and, the immediate post-operative, minimum 6 months post-operative positions. Pre operative measurements were marked as T1, immediate post operative as T2, follow up post operative as T3. The immediate post-surgical changes of soft tissues were not assessed due to the presence of edema.
Immediate surgical changes of hard/soft tissues—T2–T1
Follow up post operative changes of hard/soft tissues—T3–T1
Relapse or resorption of hard tissues—T2–T3
Follow up post operative hard to soft tissue changes—ratio of T3–T1
Statistical Analysis
After collection of data, it was entered into Microsoft Excel 2000 and converted into SPSS version 11.0 software and statistical analysis was done by using unpaired t test and paired t test.
Results
Skeletal Changes
Mean surgical advancement at Pg was 7.92 mm, 6 months after surgery. Mean relapse at Pg was 0.85 mm representing 10.7% of surgical advancement. A change in surgical result of 2 mm or more was considered clinically significant. According to this cut off value, no patient had clinically significant relapse at Pg after follow up.
The remodeling and resorption patterns at upper anterior osteotomy point and lower posterior osteotomy point has not influenced Pg. Most of these horizontal remodeling changes took place posteriorly in first 3–4 months. Post operative changes thereafter were small. Mean changes in vertical plane as a result of surgery were minor. The vertical position of menton (Me) did not, show statistically significant changes. At the anterior osteotomy point the remodeling changes showed minor superior movement which may be due to bone depositions above osteotomy plane.
Soft Tissue Changes
During the immediate post operative period there were large changes in the soft tissues due to postoperative swelling and it gradually declined till T3. Several significant net changes (T3–T1) could be observed as a result of surgery. PgS was relocated 6.35 mm in the anterior direction. Upper lip and lower lip showed no significant horizontal changes during the period.
At T3 the mentolabial fold showed a net deepening of 1.14 mm as a result of treatment.
The soft tissue thickness, Pg–PgS, demonstrated a small but significant decrease of 0.92 mm.
A reduction in facial convexity demonstrated a decrease of 6.64° in the angle of G–Sn–PgS at T3.
The lower facial submental angle (Li–GnS–C) showed a net decrease of 17°.
The mean vertical soft tissue changes were non significant at the end of observation period.
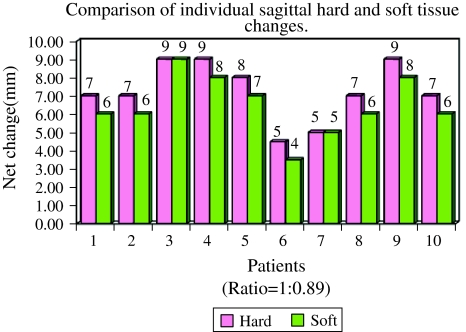
Relationship Between Soft Tissue and Hard Tissue Movements
Net changes (T3–T1) in the mandibular soft tissue landmarks were found to correlate with movement of their corresponding bony structures. The mean percentage of the net changes (T3–T1) of P–Pg to P–PgS is 7.07:6.35 = 1:0.89. (Table 1)
Table 1.
Osseous and soft tissue changes
| Variable | T2–T1 | T2–T3 | T3–T1 | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Hard tissue | ||||||
| (A) Horizontal | ||||||
| P–Pg | −7.92 | 2.0 | 0.85 | 0.24 | −7.07 | 1.78 |
| (B) Vertical | ||||||
| OPL–MePL | 0.28 | 1.52 | 0.50 | 0.76 | 0.21 | 2.11 |
| Soft tissue | ||||||
| (A) Horizontal | ||||||
| P–PgS | −6.35 | 1.84 | ||||
| Pg–PgS | −0.92 | 0.18 | ||||
| (B) Dimensional | ||||||
| G–Sn–PgS | −6.64 | 2.64 | ||||
| Si–(Li–PgS) | 1.14 | 0.89 | ||||
| Li–GnS–C | −17 | 8.56 | ||||
| Hard vs. Soft | ||||||
| Horizontal | ||||||
| P–Pg/P–PgS | 7.07/6.35 = 1:0.89 | |||||
Discussion
Like any other maxillofacial osteotomy, osteotomy of the inferior border of the mandible can be adversely affected by two completely different mechanisms firstly the skeletal instability, where the advanced genial segment changes in position prior to osseous union, thereby rapidly altering the surgical outcome. The second being osseous remodeling, where the advanced genial segment is slowly recontoured during the remodeling process, and is much slower pathway by which the final result may differ from the immediate post surgical outcome [7].
Some of the studies were against the use of pogonion as a reference point to study the exact measurements of genial segment because bony remodeling would invalidate any conclusion about skeletal stability [8]. Defreitas et al. [7] and several other studies described the pogonion as an important point to be assessed in a genioplasty study as it is the unaltered bony land mark of the chin prominence.
The pedicled advancement genioplasty should be considered as the standard method as the amount of bone resorption is less and likelihood of reduced post-operative infection [9]. In the present study all the patients underwent minimal soft tissue stripping with broad attachment of lingual soft tissue. There was no incidence of post-operative infection in any patient. Mild transient mental nerve paresthesia was noticed in three patients which may be due to retraction and was recovered in due follow up [10]. Lingual hematoma was noticed in two patients which subsided within a week. Post operative healing was uneventful and satisfactory [11].
The mentalis muscle is important because it is the sole elevator of the lower lip and chin and it provides the major vertical support for the lip. If this muscle is either not functioning or not precisely repositioned after surgery, the result may be extremely unaesthetic because of chin ptosis or “witch’s chin” and possible lip incompetence [12]. No such complications were encountered in our study.
Post operatively bone resorption was seen at the sharp superior edge of the osseous segment created by surgery. The sites of bone depositions are anterior surface of the mandible above the osteotomy and posterior-inferior aspect of the genial segment without apparent effects on soft tissue pogonion. The angle and sharp edges become rounded off. The remodeling patterns of the advanced segment never showed any evidence of inferior rotation or bodily displacement in the post operative evaluation of our study, which correlates with the previous studies [4, 6, 7, 13–17].
Initially wiring procedures were used to stabilize the osteotomized segments [9]. Rigid fixation techniques were introduced in an attempt to decrease the post surgical relapse rate. In the present study all the patients were treated with rigid fixation and showed mean relapse of 10.7% i.e. 0.85 mm which is minimum when compared to Van Sickels et al. and Mc Donnnel et al. who observed 0.92 mm and 2.8 mm of relapse.
The fixation devices for genioplasty should be placed in the areas of bony deposition. The plates used for fixation in our study were placed in the areas of bone deposition and as a result none of the patients complained of pain or discomfort with or without palpation of the region.
The soft tissue profile change seen as the effect of advancement of genial segment has been studied differently by various authors. The ratio of horizontal changes for osseous to soft tissues range from 1:0.6 to 1:1 in the literature [4, 6, 8, 10, 15, 18]. In our study the mean ratio of horizontal change is 1:0.89 which correlates with the literature. Although mild individual variations are noted in our study which may be associated with the scar contracture seen in post operative period (Graph 1). Hence always an overcorrection should be planned to the actual advancement to overcome the relapse and soft tissue change.
Graph 1.
Hard and soft tissue changes
The osteotomy slope angle should be determined initially in the prediction stage itself so as to have desired horizontal and vertical movements of the chin especially with large chin advancements. Van Sickel et al. found 0.78 mm of mean vertical movement but it is of only 0.21 mm in our study which is statistically insignificant.
To describe the overall horizontal soft tissue profile of the patient the angle of facial convexity is evaluated. Our result showed a decrease of 6.6° in the facial convexity angle which is in contrast with Scheideman and Legan et al. who showed 2.7° decrease.
The shape of the labiomental fold is influenced by all the factors that control lower lip contour and soft tissue chin contour. A direct correlation was found between the change in mentolabial sulcus depth and the amount of advancement of chin. Shaughnessy et al. demonstrated net increase of the mentolabial sulcus depth by 1.8 mm, which correlates the present study with an increase of 1.14 mm (Fig. 8, 9).
Fig. 8.

Preoperative case 1
Fig. 9.

Post operative case 1
With the larger advancements there is increase in stretching of soft tissue pedicle which produces thinning of soft tissue overlying pogonion. Polido and Bell observed a mean decrease of 1.3 mm whereas Shaughnessy et al. observed a mean decrease of 0.86 mm in the post operative soft tissue thickness. In present study it is decreased by 0.92 mm.
The chin throat angle which is demonstrated as lower facial submental angle decreased by 17° correlating with Gallagher et al. showing decrease of 22.7° (Table 2).
Table 2.
Comparison with various studies
| S. No. | Authors | Year | Results (Pg:Pgs) |
|---|---|---|---|
| 1 | Bell and Dann | 1973 | 1 : 0.60 |
| 2 | Mc Donnell et al. | 1977 | 1 : 0.75 |
| 3 | Busquets and Sassouni | 1981 | 1 : 0.80 |
| 4 | Gallagher d. M et al. | 1984 | 1 : 0.87 |
| 5 | Tulsane | 1987 | 1 : 0.73 |
| 6 | Park et al. | 1989 | 1 : 0.94 |
| 7 | Polido et al. | 1991 | 1 : 0.88 |
| 8 | De Freitas et al. | 1992 | 1 : 0.90 |
| 9 | Kremanov and Kahnberg | 1992 | 1 : 0.93 |
| 10 | Polido and Bell | 1993 | 1 : 0.83 |
| 11 | Van Sickels et al. | 1994 | 1 : 0.92 |
| 12 | Talebzadeh and Pogrel | 2001 | 1 : 0.75 |
| 13 | Veltkamp et al. | 2002 | 1 : 0.92 |
| 14 | Shaughnessy et al. | 2006 | 1 : 0.89 |
| 15 | Present study | 2009 | 1 : 0.89 |
Conclusion
The standard advancement genioplasty by inferior horizontal osteotomy of the chin with broadest musculo–periosteal pedicle using internal rigid fixation was followed. The stability of the hard tissues is good with minimum amount of resorption so as to achieve more predictable results. Very few studies like the current study have evaluated the soft tissue changes on exclusively horizontal advancement genioplasty without combining with other mandibular or maxillary procedures. The soft tissue response is almost equal to the bony movement. In the present study along with the soft tissues of the chin, the lower facial profile was also meticulously evaluated. Cephalometric analysis continuously plays an important role to assess the osseous and soft tissue changes in the orthognathic surgeries which give predictive criteria for oral and maxillofacial surgeon in the treatment planning.
References
- 1.Lines PA, Steinhauser EW. Soft tissue changes in relationship to movement of hard tissues in orthognathic surgery: a preliminary report. J Oral Surg. 1974;32:891–896. [Google Scholar]
- 2.Bell WH. Modern practice in orthognathic and reconstructive surgery. WB Saunders. 1992;3:2439–2488. [Google Scholar]
- 3.Van sickels JE, Smith CV, Tiner BD, Jones DL. Hard and soft tissue predictability with advancement genioplasties. Oral Surg Oral Med Oral Pathol. 1994;77(3):218–221. doi: 10.1016/0030-4220(94)90288-7. [DOI] [PubMed] [Google Scholar]
- 4.McDonnell JP, McNeill RW, West RA. Advancement genioplasty: a retrospective cephalometric analysis of osseous and soft tissue changes. J Oral Surg. 1977;35:640–647. [PubMed] [Google Scholar]
- 5.Burstone CJ, James RB, Legan H, et al. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269–277. [PubMed] [Google Scholar]
- 6.Park HS, Ellis E, Fonseca RJ, Reynolds ST, Mayo KH. A retrospective study of advancement genioplasty. Oral Surg Oral Med Oral Pathol. 1989;67:481–489. doi: 10.1016/0030-4220(89)90261-2. [DOI] [PubMed] [Google Scholar]
- 7.Defreitas CE, Ellis-iii E, Sinn DP. A retrospective study of advancement genioplasty using a special bone plate. J Oral Maxillofac Surg. 1992;50:340–346. doi: 10.1016/0278-2391(92)90393-E. [DOI] [PubMed] [Google Scholar]
- 8.Davis WH, Davis CL, Daly BW. Long term bony and soft tissue stability following advancement genioplasty. J Oral Maxillofac Surg. 1988;46:731–735. doi: 10.1016/0278-2391(88)90119-X. [DOI] [PubMed] [Google Scholar]
- 9.Vedtofte P, Nattestad A, Hjorting-Hansen E, Svendsen H. Bone resorption after advancement genioplasty: pedicled and non-pedicled grafts. J Cranio Maxillofac Surg. 1991;19:102–107. doi: 10.1016/S1010-5182(05)80571-2. [DOI] [PubMed] [Google Scholar]
- 10.Nishioka GJ, Mason M, sickels JE. Neurosensory disturbance associated with the anterior mandibular horizontal osteotomy. J Oral Maxillofac Surg. 1988;46:107–110. doi: 10.1016/0278-2391(88)90260-1. [DOI] [PubMed] [Google Scholar]
- 11.Lindquist CC, Obeid G. Complications of genioplasty done alone or in combination with sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol. 1988;66:13–16. doi: 10.1016/0030-4220(88)90057-6. [DOI] [PubMed] [Google Scholar]
- 12.Strauss RA, Abubaker AO. Genioplasty: a case for advancement osteotomy. J Oral Maxillofac Surg. 2000;58:783–787. doi: 10.1053/joms.2000.7266. [DOI] [PubMed] [Google Scholar]
- 13.Bell WH, Dann JJ. Correction of dentofacial deformities by surgery in the anterior part of the jaws. Am J Orthod. 1973;64(2):162–187. doi: 10.1016/S0002-9416(73)90308-4. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher DM, Bell WH, Storum KA. Soft tissue changes associated with advancement genioplasty performed concomitantly with superior repositioning of the maxilla. J Oral Maxillofac Surg. 1984;42:238–242. doi: 10.1016/0278-2391(84)90455-5. [DOI] [PubMed] [Google Scholar]
- 15.Polido WD, Regis LDC, Bell WH. Bone resorption, stability and soft-tissue changes following large chin advancements. J Oral Maxillofac Surg. 1991;49:251–256. doi: 10.1016/0278-2391(91)90214-7. [DOI] [PubMed] [Google Scholar]
- 16.Trauner R, Obwegeser H (1957) The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty––Part I and II. Oral Surg Oral Med Oral Pathol 10(7): 677–689; 10(8): 787–792 [DOI] [PubMed]
- 17.Shaughnessy S, Mobarak KA, Hogevold HE, et al. Long-term skeletal and soft tissue responses after genioplasty. Am J Orthod Dentofacial Orthop. 2006;130:8–17. doi: 10.1016/j.ajodo.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 18.Talebzadeh N, Pogrel MA. Long-term hard and soft tissue relapse rate after genioplasty. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:153–156. doi: 10.1067/moe.2001.112392. [DOI] [PubMed] [Google Scholar]