Abstract
Purpose
The purpose of this study was to compare the analgesic efficacy of a single-dose of preoperative intravenous tramadol versus diclofenac in preventing pain after third molar surgery.
Materials and Methods
Fifty patients undergoing elective third molar surgery were randomly assigned into one of the two groups (25 in each group): Group 1 received diclofenac 75 mg, and Group 2 received tramadol 50 mg intravenously preoperatively before the surgery. After injection of the study drugs, the impacted third molars were removed under local anesthetic agent.
Results
The difference in postoperative pain was assessed by four primary end-points: pain intensity as measured by a 100 mm visual analogue scale hourly for 12 h, median time to rescue analgesic, postoperative acetaminophen consumption, and patient’s global assessment. Throughout the 12 h investigation period, patients reported significantly lower pain intensity scores in the diclofenac versus tramadol group (P = 0.0001, Mann–Whitney U-test). Patients also reported significantly longer median time to rescue analgesic (10 vs. 8 h, P < 0.05, Student t test), lesser postoperative acetaminophen consumption (P < 0.05, Student t test) for the diclofenac versus tramadol group.
Conclusion
Preoperative intravenous diclofenac 75 mg is more effective than tramadol 50 mg in the prevention of postoperative dental pain.
Keywords: Preemptive analgesia, Diclofenac, Tramadol
Introduction
Preemptive analgesia comprises of an analgesic intervention which is started before nociception. It is more effective than the same intervention commenced afterwards and its advantageous effect would outlast the pharmacological duration of action of the analgesic concerned. The aim of such treatment is to prevent the central nervous system from reaching a hyperexcitable state known as central sensitization or the wind-up phenomenon, in which it responds excessively to afferent inputs [1].
The dental impaction pain model has become one of the primary models used in developing analgesic drugs, as it provides a readily available healthy population and a relatively uniform surgical procedure confined to one area of the body [2].
Tramadol is a synthetic analogue of codeine. It is a central analgesic with a low affinity for opioid receptors. Much of its action is due to inhibition of the neuronal uptake of norepinephrine and serotonin at synapses in the descending inhibitory pain pathways. The side effect profile of tramadol appears to be more acceptable to ambulatory surgical patients compared with the traditional opioids [3].
The diclofenac is an inhibitor of cyclo-oxygenase, the key enzyme involved in the metabolism of arachidonic acid into various prostaglandin mediators of inflammation and pain [4]. Diclofenac is a phenylacetic acid derivative belonging to the carboxylic acid class of NSAIDs. It has been used successfully in the treatment of postoperative pain after oral surgery [5]. The present study was performed to compare the analgesic efficacy of preoperative intravenous tramadol versus diclofenac in preventing postoperative pain following third molar surgery.
Materials and Methods
Fifty patients who required elective surgical removal of impacted mandibular third molars in an out-patient setting participated in the study. All patients were ASA I over 18 years old and had at least one impacted third molar based on orthopantomogram evidence. All patients had no infection, pain or other problems in the week before the surgery. Patients were excluded, if they had a history of hypersensitivity to diclofenac and tramadol. Allocations of treatment regimens were randomized and double blind.
Restricted randomization was used to decide the treatment regime. An independent investigator gave either diclofenac or tramadol preoperatively according to the randomized cards. The study drugs, diclofenac and tramadol (1 ml formulation), were diluted to 2 ml with saline. Both solutions were prepared in an identical syringe by the independent investigator. An intravenous administration of study drugs was done into the antecubital fossa or dorsum of the hand of all patients. For the diclofenac group, a single bolus dose of diclofenac 75 mg was given intravenously before the surgery. For the tramadol group, a single bolus dose of tramadol 50 mg was given intravenously before the surgery. An inferior dental nerve block was given with local anaesthetic 2% lidocaine with 1:100,000 epinephrine for the regional anesthesia. The surgical removal of the impacted mandibular third molar was then completed with a standardized technique by the surgeon. Demographic and surgical data, including age, weight, gender, duration of surgery, and amount of local anesthetic used was recorded.
Pain Assessments
Analgesic efficacy was assessed on the basis of four key end-points:
The pain intensity in the form of visual analogue scale (VAS): patients were asked to record on a plain serial 100 mm VAS, the pain intensity every hour for 12 h after the surgery. Anchor points were 0: no pain and 100: worst pain possible. Serial VAS recorded over the 12 h investigation periods were compiled into a graph of pain (mm) versus time (h).
Median time to remedication: time to remedication is defined as the time from the end of surgery until the intake of rescue medication became necessary for the patient. Once a subject received a rescue medication (paracetamol 500 mg) the time of this event was recorded and the subject was excluded from further pain intensity measurements.
Total analgesic consumption: total amount of analgesic (paracetamol tablets) consumed during the full recovery period (5 days) was recorded.
Global assessment: patients were asked to provide an overall evaluation of the efficacy of the analgesic with regard to pain on a four point categorical scale, at the end of the trial. The categories of scale were 0: poor, 1: fair, 2: good and 3: excellent. Excellent: minimum pain versus poor: maximum pain.
Results
Of the 50 patients entered into the study, six were excluded from the analysis due to incomplete information. Thus, data was obtained from 44 patients. Demographic details of the patients and operation time recorded in the investigation are shown in Table 1. The age of the subjects ranged from 20 to 38 years with a mean (±SD) age (yrs) of 26.57 (±5.6) in diclofenac group and 25.76 (±4.1) in tramadol group (Table 1). The male: female ratio is 14:9 for diclofenac group and 18:3 for tramadol group. Both groups were balanced for the demographic variables and there was no significant difference (Student t test, P > 0.05) between the two groups for operating time and amount of local anesthetic used for the surgery.
Table 1.
Demographic details and operation data of patients evaluated in the comparative study of the use of tramadol and diclofenac for the prevention of postoperative pain
| Variables | Diclofenac group | Tramadol group |
|---|---|---|
| Number of subject | 25 | 25 |
| Number of dropouts | 2 | 4 |
| Male:Female | 14:9 | 18:3 |
| Age (years) | 26.57 ± 5.6a | 25.76 ± 4.1a |
| Weight (kg) | 65.91 ± 6.9a | 64.43 ± 6.8a |
| Amount of local anesthesia used (ml) | 5.2 ± 0.7a | 5.4 ± 0.2a |
| Mean operation time (min) | 34.96 ± 3.7a | 32.04 ± 5.2a |
aWhen appropriate, results are expressed as mean ± SD, No significant difference between (P > 0.05) the two group in demographic details
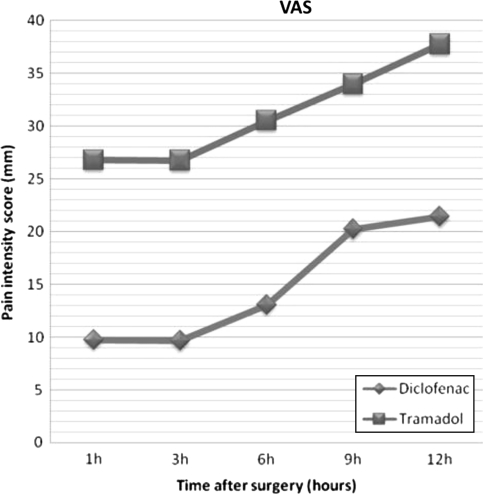
The mean pain intensity scores for VAS scores throughout the 12 h investigation period are shown in Table 2 and Graph 1. Patients in the diclofenac group experienced significantly less pain throughout the 12 h investigation period, than when they received tramadol (Mann–Whitney U-test, P = 0.0001) (Fig. 1). The diclofenac group reported a longer time to rescue analgesic (median 10.0 h) compared with the tramadol group (median 8.0 h) (Student t test, P < 0.05). The mean time to rescue analgesic for the diclofenac group was 10.76 h after surgery as compared with the 7.6 h for the tramadol group. Hence, the results showed that diclofenac provided approximately 3 h longer duration of preventive analgesia compared with tramadol (Table 2).
Table 2.
Operation details and efficacy parameters recorded in the investigation for tramadol and diclofenac group for prevention of postoperative pain
| Variables | Diclofenac group | Tramadol group | P value |
|---|---|---|---|
| VAS (mm) | 21.43 ± 6.3 | 37.76 ± 9.9 | <0.05 |
| Mean time to rescue analgesic (h) | 10.76 ± 2.0 | 7.6 ± 2.5 | <0.05 |
| Median time to rescue analgesic (h) | 10 | 8 | <0.05 |
| Total analgesic consumption (tablets) | 5.72 ± 0.29 | 7.74 ± 0.28 | <0.05 |
| Global assessment scores | Good (52.2%) | Fair (61.9%) | >0.05a |
Results are expressed mean ± SD where applicable
aSignificant difference between diclofenac and tramadol groups except for global patient assessment scores
Fig. 1.
Mean pain intensity scores (in mm) as recorded on a 100 mm VAS throughout the 12 h investigation period for the diclofenac and tramadol treated group
The total postoperative analgesic consumption (paracetamol 500 mg) for the diclofenac group (mean, Table 2) was also significantly less than the tramadol group (mean, Table 2) (Student t test, P < 0.05). Patient’s overall assessment of the surgery in relation to pain is shown in Table 2. The distribution of scores shows that more patients in the diclofenac group 52.2% scored the surgery as good and in tramadol group 61.9% patients scored the surgery as fair.
Both intraoperative and postoperative subjective observations were done by the surgeon for any complications due to the study drugs. No significant intraoperative and postoperative complications were seen for both groups of patients. There were no cases of postoperative bleeding associated with diclofenac, and no cases of vomiting associated with tramadol at the doses given in this study. Adverse effects were mild and did not require any specific treatment.
Discussion
Analgesia after impacted third molar surgery is necessarily a balance between achieving adequate pain relief, whilst causing minimum side effects. The concept of “preemptive analgesia” is that the degree and intensity of post injury pain can be reduced by the use of local anesthetic injections or analgesic drugs during the pre-injury period [5]. The combination of a relatively short-acting local anesthetic and a long-acting analgesic as a postoperative pain control regimen seems superior to the use of a long-acting local anesthetic alone [6]. The results from our study show that preoperative intravenous diclofenac could provide a median analgesic duration of 10 h. This is comparable with the duration of analgesia after bupivacaine infiltration. Hyrkas et al. [7] achieved, in their study, an almost pain-free postoperative period by combining normal and sustained-release diclofenac derivatives and bupivacaine, without increasing the incidence of side effect. This study shows that preoperative intravenous diclofenac is better than tramadol in preventing postoperative third molar surgical pain. The median analgesic duration of 9 h is clinically significant as pain for this type of procedure is usually most severe between 6 and 8 h after the surgery [1]. When tramadol was administered preoperatively in this study, it had a median analgesic duration of 8 h.
Hyrkas et al. [4], in their study, has given a single dose of 75 mg diclofenac sodium or saline (placebo) intravenously before operation. Preoperative intravenous administration of diclofenac gave greater pain relief than placebo for the first 3 h (three way ANOVA) after operation. The comparison of preoperative intravenous ketorolac versus tramadol was done by Ong and Tan [2] for the control of pain after third molar surgery. Throughout the 12 h investigation period, patients reported significantly lower pain intensity scores in the ketorolac versus tramadol group (P = 0.05, Mann–Whitney U-test). Patients also reported significantly longer median time to rescue analgesic (9.0 vs. 7.0 h, P = 0.007, log rank test), lesser postoperative acetaminophen consumption (P = 0.02, Mann–Whitney U-test) and better global assessment (P = 0.01) for ketorolac versus tramadol group. In the present study, the median analgesic duration of tramadol was 8 h, which is comparable to above study.
Wuolijoki et al. [8] treated ninety five patients, undergoing surgical removal of third molar with diclofenac or placebo, administered double-blind either pre- or postoperatively. In their study preoperatively administered 75 mg diclofenac sodium reduced pain more effectively than postoperatively administered diclofenac. They concluded that preoperative administration of diclofenac produces more effective pain relief than postoperative administration. By contrast a recent study by Putland and McCluskey [9] has shown that intravenous tramadol was more effective in reducing postoperative pain than ketorolac in laparoscopic surgery.
Tramadol is a suitable analgesic for use in day-care oral surgery. However, third molar tooth extractions are associated with considerable postoperative inflammation, and it could be argued that non steroidal anti-inflammatory drugs are more appropriate for such surgery than tramadol, which lacks anti-inflammatory actions. Medve et al. [10] suggested that combination of tramadol and acetaminophen was superior to tramadol or acetaminophen alone with respect to pain relief and intensity and duration of analgesia in the treatment of dental pain.
Diclofenac has significant anti-inflammatory and analgesic activities. When administered preoperatively, diclofenac gave better pain relief than postoperative administration of diclofenac, indicating that early inhibition of the inflammation resulting from operative trauma provides best pain relief. Intravenous preoperative drug administration is the simplest way to ensure optimum plasma drug levels at the time of surgical intervention. Because of extensive first-pass metabolism, an intravenous infusion of 75 mg of diclofenac corresponds roughly to the recommended daily oral dose of 150 mg, i.e., tolerance is likely to be better after intravenous than after oral administration [8].
In theory, the strategy of administering the analgesic before surgery, will pre-position the drug at the surgical site and establish effective blood levels for maximum analgesic effect. These predict not only less pain during the initial postoperative period, but also lower the intensity of pain during the days after the surgery. By reducing the pain during recovery, fewer analgesics will be consumed, resulting in fewer drug adverse events, complicating the post-operative course and delaying patient’s return to normal activities [2].
According to Blum the incidence of dry socket after the removal of mandibular third molar is ranges from 1 to 45%. A significantly higher incidence of dry socket occurring in female due to increased use of contraceptives. The incidence of dry socket is more in smokers [11]. The occurrence of dry socket after surgery can interfere with the results of the study.
Conclusion
This study shows that intravenous diclofenac provides better preventive analgesic efficacy than tramadol when given preoperatively for third molar surgery. The reduction of postoperative pain is significantly long to control the peak postoperative pain at 6–8 h for impacted third molar surgery.
Contributor Information
Manish Kumar Pandit, Phone: +91970215950, Email: drmanish23@gmail.com.
Suhas Godhi, Phone: +919899450488, Email: drgodhi@gmail.com.
Amit B. Lall, Phone: +919810007011, Email: dr_abl@yahoo.com
References
- 1.Ong KS, Seymour RA, Chen FG, Ho VCL. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg. 2004;33:771–776. doi: 10.1006/ijom.2003.0515. [DOI] [PubMed] [Google Scholar]
- 2.Ong KS, Tan JML. Preoperative intravenous tramadol versus ketorolac for preventing postoperative pain after third molar surgery. Int J Oral Maxillofac Surg. 2004;33:274–278. doi: 10.1006/ijom.2003.0515. [DOI] [PubMed] [Google Scholar]
- 3.Olmedo MV, Gálvez R, Vallecillo M. Double-blind parallel comparison of multiple doses of ketorolac, ketoprofen and placebo administered orally to patients with postoperative dental pain. Pain. 2001;90:135–141. doi: 10.1016/S0304-3959(00)00396-1. [DOI] [PubMed] [Google Scholar]
- 4.Hyrkas T, Ylipaavalnicmi P, Oikarinen VJ, Paakkari I. Preoperative intravenous diclofenac for postoperative pain prevention in outpatients. Br J Oral Maxillofac Surg. 1993;31:351–354. doi: 10.1016/0266-4356(93)90189-4. [DOI] [PubMed] [Google Scholar]
- 5.Zacharias M, Hunter K, Baker AB. Effectiveness of preoperative analgesics on postoperative dental pain: a study. Anesth Prog. 1996;43:92–96. [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenquist JB, Nystrom E. Long acting analgesic or long acting local anesthetic in controlling immediate postoperative pain after lower third molar surgery. Anesth Prog. 1987;1:6–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Hyrkas T, Ylipaavainiemi P, Oikarinen VJ, Paakkari I. Effective postoperative pain prevention through administration of bupivacaine and diclofenac. Anesth Prog. 1994;41:6–10. [PMC free article] [PubMed] [Google Scholar]
- 8.Wuolijoki E, Oikarinen VJ, Ylipaavainiemi P, Hampf G, Tolvanen M. Effective postoperative pain control by preoperative injection of diclofenac. Eur J Clin Pharmacol. 1987;32:249–252. doi: 10.1007/BF00607571. [DOI] [PubMed] [Google Scholar]
- 9.Putland AJ, McCluskey A. The analgesic efficacy of tramadol versus ketorolac in day-case laparoscopic sterilization. Anesthesia. 1999;54:382–385. doi: 10.1046/j.1365-2044.1999.00739.x. [DOI] [PubMed] [Google Scholar]
- 10.Medve RA, Wang J, Karim R. Tramadol and acetaminophen tablets in dental pain. Anesth Prog. 2001;48:79–81. [PMC free article] [PubMed] [Google Scholar]
- 11.Blum R. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002;31:309–317. doi: 10.1054/ijom.2002.0263. [DOI] [PubMed] [Google Scholar]