Abstract
Purpose
To evaluate the transconjunctival preseptal approach for time required for exposure, adequacy of exposure, intraoperative and postoperative complications.
Materials and Methods
Materials for this study involved 15 cases of maxillofacial injuries with orbital floor and infraorbital rim fracture.
Results
The average exposure time taken for placement of incision till the exposure of the fracture was 21 min. Exposure obtained for fracture site was adequate in all cases, for the reduction of orbital floor and internal fixation of infraorbital rim. No cases had intraoperative and postoperative complications. In all cases postoperative esthetic outcome was satisfactory.
Conclusion
The transconjunctival preseptal approach is most effective surgical access to infraorbital rim and orbital floor and even to medial orbital wall. This approach is surgically similar in providing exposure and access, but aesthetically superior to other approaches and has minimal complications. There are no disadvantages to transconjunctival preseptal approach, if performed meticulously with sound knowledge of anatomy of periorbital tissues.
Keywords: Transconjunctival approach, Orbital floor, Infraorbital rim
Introduction
The most commonly used approaches to infraorbital rim and orbital floor are subciliary, subtarsal, infraorbital rim and transconjunctival approach. The infraorbital incision can heal well with meticulous wound closure, but the approach is associated with prolonged lower eyelid pretarsal edema. The subciliary incision rarely leaves a noticeable scar but has significant instance of temporary lower eyelid retraction that often results in permanently severely inflamed and injured tissue [1].
There is a current trend towards more central placement of incisions with respect to the globe, which provides nearly equal access and improved esthetics. Successful utilization of these approaches is dependent on surgeon’s appreciation of the relationship between eyelid/periorbital anatomy and lid/ocular function [2]. The transconjunctival approach was first described in 1924 by Bourget for the removal of lower eyelid fat [3]. Several authors have proposed that the transconjunctival approach decreases the risk of postoperative eyelid retraction, which varies from scleral show to persistent ectropion. These studies have shown a lower incidence of ectropion using a transconjunctival compared with a subciliary approach for the treatment of orbital trauma [4, 5].
The ability to reach the periosteum through a transconjunctival incision further allows access to a great portion of orbit. The lateral canthotomy allows the periosteum to be elevated superiorly for repair of fracture of frontozygomatic suture. Present study was undertaken to evaluate the various advantages of this approach mentioned in the literature like minimal scar, decreased possibility of eyelid retraction or ectropion.
Materials and Methods
Fifteen cases (6 females and 9 males) with orbital floor and infraorbital rim fractures were treated with transconjunctival preseptal approach; additionally lateral canthotomy was used in 5 cases which were associated with zygomatic fractures. The average age of the patients was 28 years and all the procedures were unilateral. The following patients were excluded from the surgery (1) acute and chronic conjunctival diseases (2) previous history of surgery for retinal detachment. In all 15 patients, time required for exposure, adequacy of exposure, intraoperative and postoperative complications, esthetic results from using the transconjunctival preseptal approach were analysed. The average follow up was 14 months.
Results
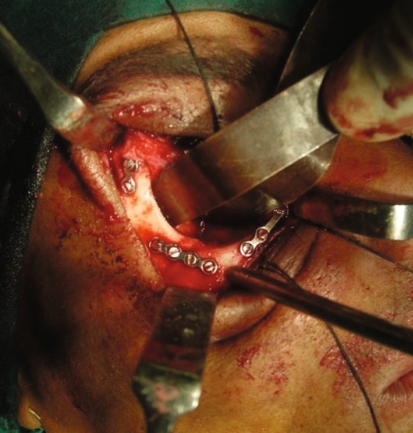
All the patients after exploration through the transconjunctival preseptal approach, the orbital floor fracture reduction was done with infraorbital osteosynthesis (Fig. 1). In 5 cases fixation was done in frontozygomatic suture after extension of incision with lateral canthotomy and in four patients medial orbital fixation was done (Figs. 1, 2, 3).
Fig. 1.
Plate fixation at infraorbital rim, frontozygomatic suture and medial orbital wall
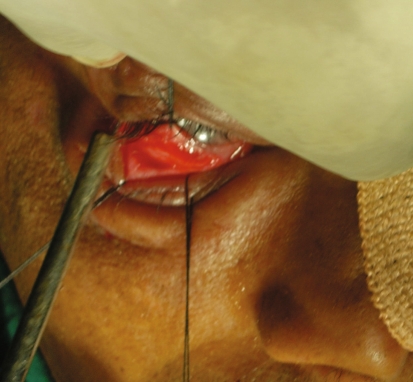
Fig. 2.
Incision made 3 mm below the tarsal plate on the medial aspect and in line with the punctum
Fig. 3.
Exposure of the frontozygomatic suture and infraorbital rim after extension of incision with lateral canthotomy
The average exposure time required for exposure of fracture site was 21 min (Table 1). The adequacy of exposure of fracture site was excellent in 10 cases and satisfactory in 5 cases. No patients had intraoperative complications. Postoperatively no permanent complications were encountered in any of the patients, except one patient who had scleral show of 1 mm, which resolved within 3 months. Esthetic outcome was satisfactory in all cases.
Table 1.
Treatment outcome
| Sl. No. | Associated fracture along with orbital floor and infraorbital rim fracture | Age/sex | Incision | Adequacy of exposure | Time taken | Intraoperative complications | Post operative complications | ||
|---|---|---|---|---|---|---|---|---|---|
| Transient | Permanent | Requiring treatment | |||||||
| 1 | LE-I | 26/F | TPA | Satisfactory | 24 | None | None | None | None |
| 2 | LE-II | 28/M | TPA | Satisfactory | 23 | None | None | None | None |
| 3 | ZMC | 27/M | TPA+LC | Excellent | 23 | None | None | None | None |
| 4 | LE-I | 25/F | TPA | Excellent | 22 | None | None | None | None |
| 5 | ZMC | 24/F | TPA | Satisfactory | 21 | None | None | None | None |
| 6 | LE-I | 28/M | TPA | Excellent | 22 | None | None | None | None |
| 7 | LE-II | 29/M | TPA | Excellent | 21 | None | None | None | None |
| 8 | ZMC | 30/M | TPA+LC | Excellent | 21 | None | Scleral show | None | None |
| 9 | LE-II | 27/F | TPA | Satisfactory | 22 | None | None | None | None |
| 10 | ZMC | 26/F | TPA+LC | Excellent | 20 | None | None | None | None |
| 11 | LE-I | 30/M | TPA | Satisfactory | 20 | None | None | None | None |
| 12 | ZMC | 31/M | TPA | Excellent | 20 | None | None | None | None |
| 13 | ZMC | 32/M | TPA+LC | Excellent | 19 | None | None | None | None |
| 14 | LE-II | 29/M | TPA | Excellent | 19 | None | None | None | None |
| 15 | ZMC | 28/F | TPA+LC | Excellent | 18 | None | None | None | None |
LE-I lefort-I fracture, LE-II lefort-II fracture, ZMC zygomatic complex fracture, TPA transconjunctival preseptal approach, LC lateral canthotomy, F female, M male
Discussion
McCord and Moses popularized transconjunctival surgery in the mid 1970s using “swinging lower eyelid flap” [1]. Tessier was first to advocate transconjunctival approach, to expose the orbital floor for treatment of congenital disease and trauma in 1973 [3]. The ability to reach the periosteum through a transconjunctival incision allows access to a great portion of orbit. The lateral canthotomy allows the periosteum to be elevated superiorly for repair of fracture of frontozygomatic suture.
There are two different routes for the transconjunctival approach: retroseptal and preseptal [6]. Many authors use retroseptal approach in blepharoplasty procedures and in treatment of orbital fractures, because of direct access to the orbital floor [4, 7]. However, reconstruction of the bony orbit has different goals than transconjunctival blepharoplasty. The advantage of the direct exposure of the orbital fat in a lower-lid blepharoplasty, [8] is a disadvantage in fracture repositioning.
Other disadvantages of the retroseptal approach are:
Additional disturbances of the intraorbital connective framework and
Additional scar in the anterior part of the intraorbital fat system, which could influence the eye movements and can participate in the development of an enopthalmos [6].
Advantages of the preseptal transconjunctival approach are:
Minimal lateral scar
excellent patient acceptance, and
Decreased chances of eyelid retraction or ectropion [5].
Thus the purpose of this study was to evaluate the clinical efficacy of the transconjunctival preseptal approach for treatment of infraorbital rim and orbital floor fracture.
Holtmann B., Wray R.C., Little A.G. compared the transconjunctival, subciliary, subtarsal lid crease and orbital rim incisions for orbital trauma access. The incisions were rated for speed of access, complications, and scar appearance. The rim and subtarsal lid crease incisions were the fastest, with average skin-to-fracture exposure time of 5–8 min. The subciliary incision was developed in 15 min, whereas the transconjunctival incision took 20 min to complete [9]. Surgical access was judged satisfactory in all cases.
In our experience the mean average time required for exposure was 21 min. This approach takes longer time to perform than other approaches. Exposure was considered adequate for fixation in all cases, which can be correlated to above study. However, surgical technique is comparatively difficult to all operators at least initially.
Hadeed et al. [10] believed that based on thorough understanding of the eyelid and orbital anatomy along with a precise surgical technique, the transconjunctival approach with lateral canthotomy offers a simple alternative to the subciliary technique. It provides the surgeon with superb exposure to the orbital floor, infraorbital rim, lower two thirds of the medial wall, lateral wall and lateral rim. This gives access for repair of zygomatic orbital complex fractures, orbital floor exploration and elevation of simple depressed zygomatic arch fractures.
Ilankovan et al. [11] put forward that simultaneous visualization of the infraorbital rim and lateral orbital rim is of great advantage of this technique as opposed to any other method.
In our study exposure obtained in all cases was adequate for visualization and management of infraorbital rim and orbital floor. In 5 cases transconjunctival preseptal approach was supplemented with the lateral canthotomy to get adequate exposure of the frontozygomatic suture.
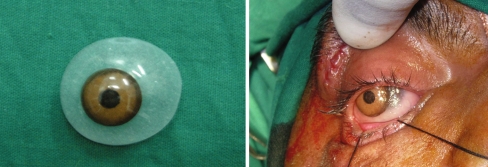
In all our cases we used plastic corneal shield to protect the globe (Fig. 4). No cases had Intraoperative complications such as corneal abrasion, tearing (button holing) of eyelid or damage to the lacrimal system. This could be correlated to earlier studies done by many authors [5, 6, 12].
Fig. 4.
Placement of the corneal shield
Most common postoperative complications of orbital bony surgery are lower eyelid retraction. In subciliary approach, a high incidence of eyelid retraction has been reported. Many authors have proposed that the transconjunctival approach decreases the incidence [4, 6, 11, 12]. Wray et al. [4] reported a 42% of incidence of ectropion after the subciliary approach compared with no ectropion after the transconjunctival approach. In the study of Appling et al. [5], the incidence of permanent scleral show was 28% after the subciliary approach and 3% after transconjunctival approach. Manson et al. [13], quoted ectropion and scleral show occur in inverse proportion to the experience of the operator.
Subtarsal approach gives more rapid and direct approach to the orbital floor and infraorbital rim fractures, but the rate of scleral show and/or ectropion ranges from 2.7 to 7.7% in the literature [14, 15]. The reported rate of perceiving noticeable scar was 2.2% [15].
In our study no permanent postoperative complications were noted in any of the cases such as cicatricial scarring, entropion, lid malposition and conjunctival granuloma. This finding was consistent with the observations of most authors.
Many authors confirmed that lateral canthotomy leads to minimum of scar tissue, and the range of complication is very low [4, 5, 12]. In this study the lateral canthotomy incision scar was bare minimum initially and it healed well in a few weeks without any objectionable scarring.
In our study frost suture was placed postoperatively, we believed use of frost suture produces superior traction, which encourages the lower eyelid redraping in proper anatomic position (Fig. 5).
Fig. 5.
Placement of frost suture
The transconjunctival preseptal approach is most effective surgical access to infraorbital rim and orbital floor and even to medial orbital wall. This approach is surgically similar in providing exposure and access, but aesthetically superior to other approaches and has minimal complications. Potential advantages of this approach negate the longer time taken for this approach. There are no disadvantages to transconjunctival preseptal approach, if performed meticulously with sound knowledge of anatomy of periorbital tissues (Fig. 6).
Fig. 6.
Preoperative and postoperative photograph after 1 year follow-up
References
- 1.Wesley RE. Transconjunctival approaches to the lower lid and orbit. J Oral Maxillofac Surg. 1998;56:66–69. doi: 10.1016/S0278-2391(98)90918-1. [DOI] [PubMed] [Google Scholar]
- 2.Eppley BL, Custer PL, Sadove AM. Cutaneous approaches to the orbital skeleton and periorbital structures. J Oral Maxillofac Surg. 1990;48:842–854. doi: 10.1016/0278-2391(90)90344-2. [DOI] [PubMed] [Google Scholar]
- 3.Lorenz HP, Longaker MT, Kawamoto HK. Primary and secondary orbit surgery: the transconjunctival approach. Plast Reconstr Surg. 1999;103:1124–1128. doi: 10.1097/00006534-199904040-00003. [DOI] [PubMed] [Google Scholar]
- 4.Wray RC, Holtmann B, Ribaudo JM, Keiter J, Weeks PM. A comparison of conjunctival and subciliary incisions for orbital fractures. Br J Plast Surg. 1977;30:142–145. doi: 10.1016/0007-1226(77)90009-1. [DOI] [PubMed] [Google Scholar]
- 5.Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg. 1993;119:1000–1007. doi: 10.1001/archotol.1993.01880210090012. [DOI] [PubMed] [Google Scholar]
- 6.Baumann A, Ewers R. Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg. 2001;59:287–291. doi: 10.1053/joms.2001.20997. [DOI] [PubMed] [Google Scholar]
- 7.Manganello-Souza LC, Freitas RR. Transconjunctival approach to zygomatic and orbital floor fractures. Int J Oral Maxillofac Surg. 1997;26:31–34. doi: 10.1016/S0901-5027(97)80843-0. [DOI] [PubMed] [Google Scholar]
- 8.Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 1991;88:215–220. doi: 10.1097/00006534-199108000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Holtmann B, Wray RC, Little AG. A randomized comparison of four incisions for orbital fractures. Plast Reconstr Surg. 1981;67:731–735. doi: 10.1097/00006534-198106000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Hadeed H, Ziccardi VB, Sotereanos GC, Patterson GT. Lateral canthotomy transconjunctival approach to the orbit. Oral Surg Oral Med Oral Pathol. 1992;73:526–530. doi: 10.1016/0030-4220(92)90089-9. [DOI] [PubMed] [Google Scholar]
- 11.Ilankovan V. Transconjunctival approach to the infraorbital region: a cadaveric and clinical study. Br J Oral Maxillofac Surg. 1991;29:169–173. doi: 10.1016/0266-4356(91)90031-Y. [DOI] [PubMed] [Google Scholar]
- 12.Waite PD, Carr DD. The transconjunctival approach for treating orbital trauma. J Oral Maxillofac Surg. 1991;49:499–503. doi: 10.1016/0278-2391(91)90174-K. [DOI] [PubMed] [Google Scholar]
- 13.Manson PN, Ruas E, Iliff N, Yaremchuk M. Single eyelid incision for exposure of the zygomatic bone and orbital reconstruction. Plast Reconstr Surg. 1987;79:120–126. [PubMed] [Google Scholar]
- 14.Wilson S, Ellis E., III Surgical approaches to the infraorbital rim and orbital floor: The case for the subtarsal approach. J Oral Maxillofac Surg. 2006;64:104–107. doi: 10.1016/j.joms.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 15.Baqain ZH, Malkawi Z, Hadidi A, Rajab LD. Subtarsal approach for orbital floor reapair: a long-term follow-up of 12 cases in a Jordanian teaching hospital. J Oral Maxillofac Surg. 2008;66:45–50. doi: 10.1016/j.joms.2007.03.031. [DOI] [PubMed] [Google Scholar]