Abstract
Introduction
Diverticular disease of the sigmoid colon prevails in Western society. Its presentation may vary greatly per individual patient, from symptomatic diverticulosis to perforated diverticulitis. Since publication of the original Hinchey classification, several modifications and new grading systems have been developed. Yet, new insights in the natural history of the disease, the emergence of the computed tomography scan, and new treatment modalities plead for evolving classifications.
Methods
This article reviews all current classifications for diverticular disease.
Result
A three-stage model is advanced for a renewed and comprehensive classification system for diverticular disease, incorporating up-to-date imaging and treatment modalities.
Keywords: Diverticulitis, Diverticular disease, Classification
Introduction
Diverticular disease of the sigmoid colon is a common condition in Western society. Its presentation among patients may vary from symptomatic diverticulosis to perforated diverticulitis. The incidence for diverticulosis is 33–66%. Of these patients, 10–25% will develop an acute episode of diverticulitis [1]. Although diverticular disease is more common among elderly patients, a dramatic rise of its incidence is seen in the younger age groups [2]. Furthermore, depending on the severity of the disease, the treatments for the various presentations of the disease will differ. Accordingly, diagnostic tools, indications for surgery as well as treatment modalities have been evolving, resulting in more options in the therapy for diverticular disease.
Since Hinchey’s traditional classification for perforated diverticulitis in 1978, several modifications and new grading systems have been presented to display a more contemporary overview of the disease [3]. Unfortunately, these different classifications of diverticular disease have led to conflicting terminology in current literature. Moreover, none of the classifications seem to sufficiently embrace the entire spectrum of the disease. This calls for a thorough review and a new parameter.
The current classifications of diverticular disease are based on clinical, radiological, or operative findings, yet most lack a translation into daily clinical practice. Given a useful classification system ought to guide clinical decision making and management, this review serves to combine the available classifications with current knowledge of practice into a more useful practice parameter for treating diverticular disease.
Methods
An extensive literature analysis was performed using the PubMed database. The following “MeSH” terms were used during the first PubMed search: diverticulitis, classification, and colonic diverticulosis. Only a few classifications for diverticular disease were revealed. In most publications, the results of a clinical study on imaging or treatment modalities are described, and rarely the proposal of a new classification system. A second analysis using manual cross reference search of the bibliographies of relevant articles located studies not found in the first search. The third strategy used the “related article” function in PubMed to select articles not found in above searches. All articles in English, German, and Dutch have been included. A total of nine classifications and modified classifications for diverticular disease were collected.
Classifications
A proper classification system can improve mutual communication between doctors of different specialties and support clinical decision making. This seems indispensible for the management of the wide spectrum of manifestations and many treatment modalities embraced by the term “diverticular disease”. Uniform classification in clear subgroups of diverticular disease could help the clinician in predicting outcomes and prognosis more accurately.
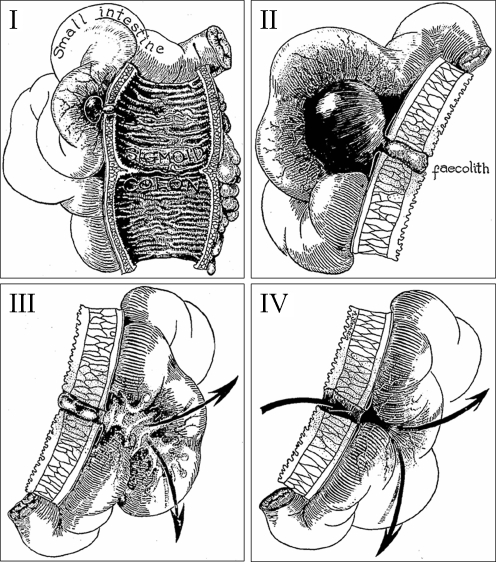
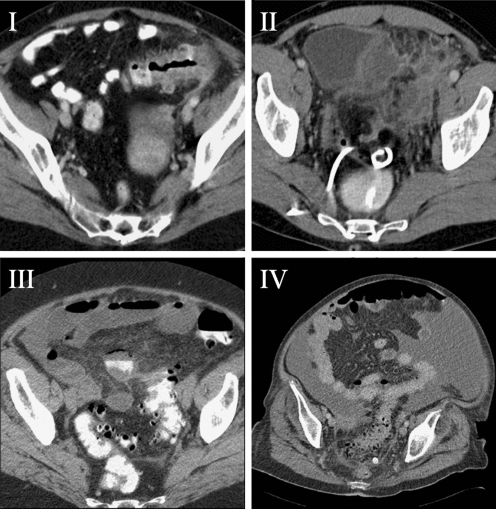
In 1978, Hinchey et al. published their classification for acute diverticulitis [3]. The Hinchey classification has traditionally been used in international literature to distinguish four stages of perforated disease (see Table 1). This most widely used classification was actually based on an earlier clinical division of acute diverticulitis published by Hughes et al. (see Fig. 1) [4]. Since the introduction of the computed tomography (CT scan) in the 1980s, this imaging modality has established itself as the primary diagnostic tool in the assessment of diverticular disease (see Fig. 2). The much more detailed information provided by CT scans led earlier to modifications of the original Hinchey classification. Subcategories could be defined by taking the radiological findings into account. Hence, in 1997, Sher et al. introduced the first modification for distinguishing between a pericolic abscesses (stage I), distant abscesses amendable for percutaneous drainage (stage IIa), and complex abscesses associated with a possible fistula (stage IIb) [5]. This modification also implied the use of new treatment strategies, such as CT-guided percutaneous drainage of abscesses.
Table 1.
Hinchey classification and modified Hinchey classification by Sher et al.
| Hinchey classification [3] | Modified Hinchey classification by Sher et al. [5] | ||
|---|---|---|---|
| I | Pericolic abscess or phlegmon | I | Pericolic abscess |
| II | Pelvic, intraabdominal, or retroperitoneal abscess | IIa | Distant abscess amendable to percutaneous drainage |
| IIb | Complex abscess associated with fistula | ||
| III | Generalized purulent peritonitis | III | Generalized purulent peritonitis |
| IV | Generalized fecal peritonitis | IV | Fecal peritonitis |
Fig. 1.
Hughes classification (Hughes et al. [4], reproduced with permission)
Fig. 2.
CT scan images resembling the four Hughes stages. I Pericolic phlegmon with small associated abscess. II Large intraabdominal abscess. III Small amounts of free air and fluid. IV Massive pneumoperitoneum and free fluid
In 1999, Wasvary et al. published another modification, which since then has been widely adopted (see Table 2) [6]. This modification broadened the original Hinchey classification by not only addressing perforated disease, but also including mild clinical disease (stage 0). Additionally, a difference was made between confined pericolic inflammation or phlegmon (stage Ia) and a confined pericolic abscess (stage Ib).
Table 2.
Modified Hinchey classification by Wasvary et al. and CT findings by Kaiser et al.
| Modified Hinchey classification by Wasvary et al. [6] | CT findings by Kaiser et al. [20] | |
|---|---|---|
| 0 | Mild clinical diverticulitis | Diverticuli ± colonic wall thickening |
| Ia | Confined pericolic inflammation or phlegmon | Colonic wall thickening with pericolic soft tissue changes |
| Ib | Pericolic or mesocolic abscess | Ia changes + pericolic or mesocolic abscess |
| II | Pelvic, distant intraabdominal, or retroperitoneal abscess | Ia changes + distant abscess (generally deep in the pelvis or interloop regions) |
| III | Generalized purulent peritonitis | Free gas associated with localized or generalized ascites and possible peritoneal wall thickening |
| IV | Generalized fecal peritonitis | Same findings as III |
Also in 1999, Köhler et al. published a consensus statement drawn up by the European Association of Endoscopic Surgeons entailing a clinical classification that differentiated symptomatic uncomplicated disease, recurrent symptomatic disease, and complicated disease (see Table 3) [7].
Table 3.
Classification by Köhler et al.
| Classification by Köhler et al. [7] | ||
|---|---|---|
| Symptomatic uncomplicated disease | ||
| Recurrent symptomatic disease | ||
| Complicated disease | ||
| • Hemorrhage | • Fistula | • Purulent and fecal peritonitis |
| • Abscess | • Perforation | • Small bowel obstruction due to post-inflammatory adhesions |
| • Phlegmon | • Stricture | |
In German literature since 1998, the Hansen/Stock classification has been mainly used. This is also a clinical classification accounting for asymptomatic diverticulosis as well as complicated diverticulitis in different stages, depending on the severity of the complications (see Table 4) [8]. These aspects make it probably the most useful classification in clinical practice; however, it has rarely been adopted in international literature. Another German classification published in 1995 by Siewert et al. followed a similar delineation for complicated disease [9].
Table 4.
Hansen/Stock and Siewert classification
| Hansen/Stock classification [8] | Siewert et al. [9] | |||
|---|---|---|---|---|
| 0 | Diverticulosis | |||
| I | Acute uncomplicated diverticulitis | |||
| II | Acute complicated diverticulitis | |||
| a | Phlegmon, peridiverticulitis | I | Pericolic abscess or phlegmon | |
| b | Abscess, sealed perforation | II | Pelvic, intraabdominal, or retroperitoneal abscess | |
| c | Free perforation | III | Free perforation | |
| III | Chronic recurrent diverticulitis | |||
Each classification accentuates different aspects of diverticular disease, creating its own strength and limitation. Moreover, some of these classifications appear to be used at random in today’s literature, thereby hampering adequate interpretation and comparison. Despite this variety of classifications, still a few clinical manifestations comprised by “diverticular disease” seem to be lacking; for example recurrent diverticular bleeding and post-inflammatory stenosis.
Clinical presentation
As stated above, Köhler et al. presented a classification for diverticular disease based on the clinical severity and presentation of the disease. Although subjective complaints are obviously difficult to grade, Köhler et al. considered crampy pain in the left lower quadrant, fever, and changes in relief pattern to be symptomatic. One must consider that a large number of patients with complaints of pain in the left lower quadrant, fever, and soiling are probably out of clinical sight, consulting only their general practitioner. Such complaints are considered to be self-limiting, sometimes assisted by antibiotic therapy. Published data on clinical episodes of diverticulitis do not account for these subjective complaints, leading to an underestimation of the real scale of these mild manifestations of diverticular disease. Furthermore, limitations of the clinical diagnosis of diverticulitis have to be regarded [10].
Clinical episodes are characterized by focus on more objective signs, like raised infectious parameters in laboratory tests and typical findings on CT scan or colonoscopy [1]. Yet, this does not discount the initial subjective complaints. It is the combination of specific symptoms that still form the basis for a differential diagnosis and the indication for additional examinations. For instance, impaired passage of a stool is suggestive for a stenosis, in which a colonoscopy can differentiate between post-diverticulitis stenosis or cancer; diverticular bleeding is the most common cause of recurrent rectal blood loss, but again cancer should be ruled out by a colonoscopy; and pneumaturia is pathognomic for a colovesical fistula, usually a CT scan will reveal its pathway. Furthermore, a generalized peritonitis is only diagnosed by physical examination. The combination of the following symptoms should be suspected: an ill patient with fever, absence of peristalsis, very tender abdomen on palpation, relief pain, and défènce musculair. A CT scan is often mandatory in uncovering its cause and confirming the absolute indication for surgery.
When elective surgery for diverticular disease is considered, indications are mainly determined by the impact of symptoms on patients’ lives. Complications such as stenosis, fistula, or recurrent diverticular bleeding are clear indications for an elective sigmoid resection, but also the prevention of perforated diverticulitis by performing an elective sigmoid resection has been standard policy for several decades. Recently, these recommendations have been challenged because new data on the natural history of diverticulitis has shown that most perforations do not occur after recurrences, but at the first attack of acute diverticulitis [11]. Furthermore, conservative management of recurrent non-perforated diverticulitis is associated with low rates of morbidity and mortality. These new insights resulted in a more individualized and conservative approach to mild diverticular disease, making the extent of subjective complaints even more important [2, 12].
Imaging
The original Hinchey classification was based on both clinical and surgical findings. Since then diagnostic tools have widely been improved and new modalities have been developed. The usual tests performed at the acute phase of diverticular disease are the following: water-soluble contrast enema, CT scan, and ultrasound (US). Although US has been proven as a noninvasive, readily available, and well-performing tool for the diagnosis of acute diverticulitis, its drawbacks are the dependency on the level of the examiner’s competence and the fact that images are unreadable for other physicians [13].
In today’s clinical practice regarding diverticular disease, CT scans enhanced with intravenous and intrarectal contrast have, because of their superior sensitivity and specificity up to 100%, replaced contrast enemas as the most important imaging modality [14, 15]. Especially when an associated abscess is suspected, a CT scan can be very helpful to demonstrate its presence. Also, the possibility of direct percutaneous drainage makes it a valuable attribute in the treatment of complicated diverticular disease [16]. In the case of diverticular bleeding, a CT scan enhanced with intravenous contrast (CT angio) may demonstrate a contrast blush, a limitation is that blood loss has to be at least 2 ml/min. Furthermore, it has to be considered that 80% of all diverticular bleeding is self-limiting. The role of interventional radiology is yet to be determined, occasional successes of highly selective arterial embolization are described [17].
A colonoscopy is indicated when there is doubt about cancer, persisting or recurrent complaints in the left lower quadrant, and suspicion of a stenosis or recurrent blood loss. Colonoscopy enables biopsies for histological diagnosis, and cessation of diverticular bleeding may be attempted by endoscopic measures, such as clipping, coagulation, or adrenaline injections [18]. Follow-up colonoscopy for ruling out malignancy is usually performed 6 weeks after an episode of acute diverticulitis. Routine colonoscopy divulges the majority finds of asymptomatic diverticular disease.
In recent years, magnetic resonance imaging (MRI) has gained popularity, because it lacks the ionizing radiation of a CT scan, yet matches its sensitivity and specificity [19]. Additional advantages of MRI over CT scan are its better visualization of fistulae and the possibility of virtual colonoscopy, thereby making invasive colonoscopy unnecessary. To current date, the availability of the MRI and experienced radiologists are often limited and therefore not suitable for routine use.
The wide use of CT scans initiated modifications to the Hinchey classification, but also several new radiological classifications for diverticular disease were developed. Kaiser et al. have published specific CT findings per modified Hinchey stage (see Table 2), resulting in a guideline for objective observation and reporting of CT scans [20]. The publications on the role of CT scans in diverticular disease by Ambrosetti et al. allocate diverticulitis into severe or moderate disease (see Table 5). In this approach, the CT scan provides the physician guidance in the treatment of acute complications, as well as a prognostic factor in the development of chronic complications after a first conservatively treated episode [21].
Table 5.
CT findings by Ambrosetti et al.
| CT findings by Ambrosetti et al. [21] | |
|---|---|
| Moderate diverticulitis | Localized sigmoid wall thickening (<5 mm) |
| Pericolic fat stranding | |
| Severe diverticulitis | Abscess |
| Extraluminal air | |
| Extraluminal contrast | |
Treatment
The wide spectrum of diverticular disease warrants a differentiated approach to the different manifestations. Treatment options for mild disease, associated abscesses, perforations, bleeding, and post-inflammatory complications are discussed separately. Also, the role of elective or preventive sigmoid resection will be addressed.
Moderate cases of diverticular disease, such as phlegmon or small abscesses, can be treated conservatively. Initial prescriptions are often antibiotics and an easily digestible diet, although no clear evidence exists for both their beneficial actions. Preventive measures are thought to be more successful by several authors, high-fiber diet, and prevention of obesity and treatment of comorbidities are the usual ingredients [22–24]. Newer insights into the pathophysiology of diverticular disease, comparable to inflammatory bowel disease, have led to research on the potentials of 5-aminosalicylic acid (Mesalazine) and probiotics as adjunctive treatments for diverticular disease. Tursi et al. have described promising results, but these medications are still only administered in experimental settings [25, 26].
Large abscesses, if amendable and usually larger than 5 cm, should be good candidates for CT-guided percutaneous drainage [27]. This procedure may relieve symptoms or function as a bridge to (elective) surgery. A purulent or fecal peritonitis results from a perforation and is associated with high morbidity and mortality (10–35%) [28]. In these severe circumstances, acute surgical intervention is warranted. Hartmann’s procedure used to be the treatment of choice for decades, but in recent literature, a few interesting alternatives have emerged. Several authors consider a primary anastomosis a safe option in purulent peritonitis, with or without defunctioning stoma. Even in fecal peritonitis, successful series of primary anastomosis have been published [29]. In 2008, Myers et al. introduced the concept of laparoscopic lavage for purulent peritonitis. This minimal invasive method provided resolution in 87% of patients and a reduction in mortality of up to 25% described for Hartmann’s procedure to 3% for laparoscopic lavage. Since then, several series have been published, but evidence from a randomized controlled trial is still to be awaited [30].
In order to prevent complicated disease after two episodes of acute diverticulitis, it has been considered good practice for years to perform elective sigmoid resection after two episodes of symptomatic diverticulitis and even doing so after one episode in the younger patients [31]. These recommendations drawn up by the American Society of Colorectal Surgeons in 2000 have recently been challenged. It is now thought that after a conservatively treated episode, diverticular disease usually follows a rather benign course and that complications occur mostly at first presentation [10, 32, 33]. Therefore, elective sigmoid resections should be restricted for use in treating complicated disease, such as symptomatic stenosis, fistulas to a hollow organ, or recurrent diverticular bleeding. Furthermore, recent publications on the natural course of diverticular disease suggest applying early elective sigmoid resection in high-risk patients, such as the use of immune suppression therapy, having chronic renal failure, or collagen–vascular diseases. The management of diverticular disease in young patients remains controversial. A more hazardous course has been suggested. In contrast, opponents account the longer lifespan responsible for more recurrences and complications and thereby a higher cumulative risk of emergency surgery. An individual approach, weighing symptoms and peri-operative risks on a case by case basis, seems the most appropriate policy [34, 35].
Since the mid-1990s, laparoscopic sigmoid resections for diverticular disease have gained popularity. Several retrospective series after laparoscopic sigmoid resections suggested improvements in minor complication rates, earlier resumption of food, and shorter hospital stay [36–38]. In January 2009, these beneficial effects were confirmed by a randomized controlled trial; the short-term results showed that a laparoscopic approach delivered a significant 15.4% reduction in major morbidity, less pain, shorter hospitalization, and improved quality of life at the cost of a longer operating time [39]. After 6 months follow-up, the reduction in major morbidity accumulated to 27% [40]. Therefore, laparoscopic sigmoid resection may well be the procedure of choice for patients requiring elective resection for diverticular disease.
Discussion and a proposal of a new classification
This review of the current classification systems for a condition as complex as diverticular disease raises the question: Is there a need for another classification? We acknowledge that the introduction of still another classification could be even more confusing. Consequently, the aim of this review is not to add another modification or new classification, but to combine the existing classifications and make a comprehensive translation of the findings for use in daily clinical practice. By doing so, new imaging and treatment modalities are to be incorporated. The clinical applicability of this three-stage model has yet to be addressed by means of prospective data and expert panel validation.
We propose three stages of differentiating diverticular disease: A—uncomplicated, B—chronic complicated, and C—acute complicated (see Table 6). We thereby address clinical findings (“Clinical presentation”), radiological findings (“Imaging”), and treatment modalities (“Treatment”) in different paragraphs. This stepwise approach resembles clinical decision making and forms the basis for a practice parameter on diverticular disease (see Table 6).
Table 6.
Proposed classification
| Classification | Clinical presentation | Imaging | Treatment | |
|---|---|---|---|---|
| A | Uncomplicated disease | Conservative treatment | ||
| • Pain in left lower quadrant | CT scan or US | Treatment acute episode | ||
| • Fever | • Phlegmon | • Antibioticsa | ||
| • Changes in relief pattern | • Small abscess in bowel wall | • Low residue dieta | ||
| Colonoscopy | Prevention | |||
| • Diverticulosis | • Fibers | |||
| • Inflammation | • Prevention of obesity | |||
| • Treatment of comorbidity | ||||
| • Mesalazinea | ||||
| B | Chronic complicated disease | Elective intervention | ||
| • Impaired passage of stool | CT scan | Sigmoid resection with primary anastomosis | ||
| • Presence of fistula | • Stenosis | • Open | ||
| • Recurrent rectal blood loss | • Fistula | • Laparoscopically | ||
| • Incapacitating complaints | Colonoscopy | |||
| • High-risk patients | • Stenosis | |||
| • Fistula | ||||
| • Blood in diverticula | ||||
| C | Acute complicated disease | Acute intervention | ||
| 1 | • Fever | CT scan | Percutaneous drainage | |
| • Painful mass | • Large abscesses (>5 cm) | |||
| 2 | • Ileus | CT scan | Sigmoid resection with primary anastomosis | |
| 3 | • Massive rectal blood loss | • Intestinal obstruction | Hartmann’s procedure | |
| CT angio | Sigmoid resection with primary anastomosis | |||
| • Contrast blush | • Open | |||
| Colonoscopy | • Laparoscopically | |||
| • Active diverticular bleeding | Endoscopic interventiona | |||
| Endovascular coilinga | ||||
| 4 | • Generalized peritonitis | CT scan | Diagnostic laparotomy/laparoscopy | |
| • Pneumoperitoneum | • Resection with primary anastomosis | |||
| • Extraluminal contrast | • Hartmann’s procedure | |||
| • Free fluid | • Lavage and drainagea | |||
aExperimental or non-evidence-based treatment
The three stages A, B, and C is in accordance with the clinical classification as devised by Köhler et al. and the German Hansen/Stock classification. An important difference is that since indications for elective resection no longer depend on the number of episodes, there is no further need to distinguish between “symptomatic uncomplicated disease” and “recurrent symptomatic disease”. Furthermore, the category of “complicated disease” found in both Köhler and Hansen/Stock classifications embraces all possible complications of diverticular disease, both moderate and severe, and so may be confusing. In this classification, complications are certified by severity and therapeutic options.
The original Hinchey classification for perforated diverticulitis and its modifications are mainly represented in stage C. Large abscesses (C1) and perforated disease (C4) are severe complications, but also massive diverticular (C3) bleeding and total bowel obstruction (C2) are entitled to acute interventions. In large abscesses, if amendable and usually larger than 5 cm, CT- or US-guided percutaneous drainage should be attempted as final treatment or bridge to surgery. Massive diverticular bleeding might be approached endoscopically (clipping, coagulation, or adrenaline injections) or even endovascular (coiling), but in most centers, a (laparoscopic) sigmoid resection is probably the final resolution. When a general peritonitis is suspected on physical examination, confirmed by CT scan, surgical intervention is warranted. According to current literature, a safe strategy might be to primarily perform a diagnostic laparoscopy. In the case of a purulent peritonitis, either (laparoscopic) sigmoid resection with primary anastomosis (with or without defunctioning stoma) or even laparoscopic lavage may be considered in selected cases. When fecal contamination is discovered, Hartmann’s procedure is still considered the safest option, but in select cases, a primary anastomosis (with or without defunctioning stoma) might be a safe alternative.
In most classifications, post-inflammatory changes like stenosis or fistulas are not included. Patients may have serious complaints, but interventions can usually be postponed to an elective setting. Stage B includes non-acute complications of diverticular disease, such as symptomatic stenosis, fistulas to hollow organ, recurrent (self-limiting) diverticular bleeding, and incapacitating complaints. This last group of patients covers mainly those young patients who are incapacitated by recurrent attacks and hospital admissions, which prevent them from having normal working careers and social life. In addition, high-risk patients, such as those immune compromised, using of NSAIDs and other immune suppressants or experiencing chronic renal failure, might be good candidates for early elective sigmoid resection. The planning of an elective operation makes it possible to do a proper preoperative work-up to prevent unwelcome surprises during surgery. In cases of stenosis or recurrent rectal blood loss, it is advisable to perform a colonoscopy to rule out cancer. CT scan is of superior diagnostic value in case of stenosis or fistula. During preoperative planning of complex fistula, MRI might have some benefit over CT scan. Stage B disease forms indications for elective sigmoid resections, preferably laparoscopically.
Stage A contains symptomatic uncomplicated disease. Patients with subclinical complaints or recurrent hospital admission should not be considered differently because both groups will fully recover with conservative measures. Acute episodes of stage A diverticulitis can mostly be resolved with antibiotics and a low residue diet. Recurrent episodes usually follow a benign course and risks of complications are low. At presentation, a CT scan or US (provided an experienced radiologist is available) has to be performed to rule out complicated disease. Moreover, these baseline findings are crucial if the patient deteriorates during conservative treatment. Small amounts of mucus or blood loss are generic signs of inflammation, whereby colonoscopy has to rule out other inflammatory bowel diseases or colon cancer. After a first attack, preventive measures have to be taken into account, such as high-fiber diet, weight loss, and treatment of comorbid conditions. In the near future, the prescription of Mesalazine might be added to this preventive strategy.
In conclusion, this manuscript provides an overview of current classification systems for diverticular disease. The proposed three-stage model provides a renewed and comprehensive classification system for diverticular disease, incorporating up-to-date imaging and (future) treatment modalities.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057–2066. doi: 10.1056/NEJMcp073228. [DOI] [PubMed] [Google Scholar]
- 2.Etzioni DA, Mack TM, Beart RW, Jr, et al. Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 3.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 4.Hughes ES, Cuthbertson AM, Carden AB. The surgical management of acute diverticulitis. Med J Aust. 1963;50(1):780–782. [PubMed] [Google Scholar]
- 5.Sher ME, Agachan F, Bortul M, et al. Laparoscopic surgery for diverticulitis. Surg Endosc. 1997;11:264–267. doi: 10.1007/s004649900340. [DOI] [PubMed] [Google Scholar]
- 6.Wasvary H, Turfah F, Kadro O, et al. Same hospitalization resection for acute diverticulitis. Am Surg. 1999;65:632–635. [PubMed] [Google Scholar]
- 7.Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13:430–436. doi: 10.1007/s004649901007. [DOI] [PubMed] [Google Scholar]
- 8.Hansen O, Graupe F, Stock W. Prognostic factors in perforating diverticulitis of the large intestine. Chirurg. 1998;69:443–449. doi: 10.1007/s001040050436. [DOI] [PubMed] [Google Scholar]
- 9.Siewert JR, Huber FT, Brune IB. Early elective surgery of acute diverticulitis of the colon. Chirurg. 1995;66:1182–1189. [PubMed] [Google Scholar]
- 10.Lameris W, van Randen A, van Gulik TM, et al. A clinical decision rule to establish the diagnosis of acute diverticulitis at the emergency department. Dis Colon Rectum. 2010;53:896–904. doi: 10.1007/DCR.0b013e3181d98d86. [DOI] [PubMed] [Google Scholar]
- 11.Chapman J, Davies M, Wolff B, et al. Complicated diverticulitis: is it time to rethink the rules? Ann Surg. 2005;242:576–581. doi: 10.1097/01.sla.0000184843.89836.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133–142. doi: 10.1002/bjs.4873. [DOI] [PubMed] [Google Scholar]
- 13.Liljegren G, Chabok A, Wickbom M, et al. Acute colonic diverticulitis: a systematic review of diagnostic accuracy. Colorectal Dis. 2007;9:480–488. doi: 10.1111/j.1463-1318.2007.01238.x. [DOI] [PubMed] [Google Scholar]
- 14.Ambrosetti P, Jenny A, Becker C, et al. Acute left colonic diverticulitis—compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum. 2000;43:1363–1367. doi: 10.1007/BF02236631. [DOI] [PubMed] [Google Scholar]
- 15.Cho KC, Morehouse HT, Alterman DD, et al. Sigmoid diverticulitis: diagnostic role of CT—comparison with barium enema studies. Radiology. 1990;176:111–115. doi: 10.1148/radiology.176.1.2191360. [DOI] [PubMed] [Google Scholar]
- 16.Brandt D, Gervaz P, Durmishi Y, et al. Percutaneous CT scan-guided drainage vs. antibiotherapy alone for Hinchey II diverticulitis: a case-control study. Dis Colon Rectum. 2006;49:1533–1538. doi: 10.1007/s10350-006-0613-3. [DOI] [PubMed] [Google Scholar]
- 17.Tan KK, Nallathamby V, Wong D, et al. Can superselective embolization be definitive for colonic diverticular hemorrhage? An institution’s experience over 9 years. J Gastrointest Surg. 2010;14:112–118. doi: 10.1007/s11605-009-1069-2. [DOI] [PubMed] [Google Scholar]
- 18.Pilichos C, Bobotis E. Role of endoscopy in the management of acute diverticular bleeding. World J Gastroenterol. 2008;14:1981–1983. doi: 10.3748/wjg.14.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heverhagen JT, Sitter H, Zielke A, et al. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum. 2008;51:1810–1815. doi: 10.1007/s10350-008-9330-4. [DOI] [PubMed] [Google Scholar]
- 20.Kaiser AM, Jiang JK, Lake JP, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100:910–917. doi: 10.1111/j.1572-0241.2005.41154.x. [DOI] [PubMed] [Google Scholar]
- 21.Ambrosetti P, Becker C, Terrier F. Colonic diverticulitis: impact of imaging on surgical management—a prospective study of 542 patients. Eur Radiol. 2002;12:1145–1149. doi: 10.1007/s00330-001-1143-y. [DOI] [PubMed] [Google Scholar]
- 22.Aldoori WH, Giovannucci EL, Rockett HR, et al. A prospective study of dietary fiber types and symptomatic diverticular disease in men. J Nutr. 1998;128:714–719. doi: 10.1093/jn/128.4.714. [DOI] [PubMed] [Google Scholar]
- 23.Dobbins C, Defontgalland D, Duthie G, et al. The relationship of obesity to the complications of diverticular disease. Colorectal Dis. 2006;8:37–40. doi: 10.1111/j.1463-1318.2005.00847.x. [DOI] [PubMed] [Google Scholar]
- 24.Strate LL, Liu YL, Aldoori WH, et al. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 2009;136:115–122. doi: 10.1053/j.gastro.2008.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comparato G, Fanigliulo L, Cavallaro LG, et al. Prevention of complications and symptomatic recurrences in diverticular disease with mesalazine: a 12-month follow-up. Dig Dis Sci. 2007;52:2934–2941. doi: 10.1007/s10620-007-9766-8. [DOI] [PubMed] [Google Scholar]
- 26.Tursi A. New physiopathological and therapeutic approaches to diverticular disease of the colon. Expert Opin Pharmacother. 2007;8:299–307. doi: 10.1517/14656566.8.3.299. [DOI] [PubMed] [Google Scholar]
- 27.Ambrosetti P, Chautems R, Soravia C, et al. Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum. 2005;48:787–791. doi: 10.1007/s10350-004-0853-z. [DOI] [PubMed] [Google Scholar]
- 28.Oomen JL, Engel AF, Cuesta MA. Mortality after acute surgery for complications of diverticular disease of the sigmoid colon is almost exclusively due to patient related factors. Colorectal Dis. 2006;8:112–119. doi: 10.1111/j.1463-1318.2005.00848.x. [DOI] [PubMed] [Google Scholar]
- 29.Vermeulen J, Akkersdijk GP, Gosselink MP, et al. Outcome after emergency surgery for acute perforated diverticulitis in 200 cases. Dig Surg. 2007;24:361–366. doi: 10.1159/000107719. [DOI] [PubMed] [Google Scholar]
- 30.Myers E, Hurley M, O’Sullivan GC, et al. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97–101. doi: 10.1002/bjs.6024. [DOI] [PubMed] [Google Scholar]
- 31.Wong WD, Wexner SD, Lowry A, et al. Practice parameters for the treatment of sigmoid diverticulitis–supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290–297. doi: 10.1007/BF02258291. [DOI] [PubMed] [Google Scholar]
- 32.Salem TA, Molloy RG, O’Dwyer PJ. Prospective, five-year follow-up study of patients with symptomatic uncomplicated diverticular disease. Dis Colon Rectum. 2007;50:1460–1464. doi: 10.1007/s10350-007-0226-5. [DOI] [PubMed] [Google Scholar]
- 33.Collins D, Winter DC. Elective resection for diverticular disease: an evidence-based review. World J Surg. 2008;32:2429–2433. doi: 10.1007/s00268-008-9705-7. [DOI] [PubMed] [Google Scholar]
- 34.Morris CR, Harvey IM, Stebbings WS, et al. Epidemiology of perforated colonic diverticular disease. Postgrad Med J. 2002;78:654–658. doi: 10.1136/pmj.78.925.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klarenbeek BR, Samuels M, van der Wal MA, et al. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670–674. doi: 10.1097/SLA.0b013e3181d3447d. [DOI] [PubMed] [Google Scholar]
- 36.Alves A, Panis Y, Slim K, et al. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92:1520–1525. doi: 10.1002/bjs.5148. [DOI] [PubMed] [Google Scholar]
- 37.Dwivedi A, Chahin F, Agrawal S, et al. Laparoscopic colectomy vs. open colectomy for sigmoid diverticular disease. Dis Colon Rectum. 2002;45:1309–1314. doi: 10.1007/s10350-004-6415-6. [DOI] [PubMed] [Google Scholar]
- 38.Senagore AJ, Duepree HJ, Delaney CP, et al. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45:485–490. doi: 10.1007/s10350-004-6225-x. [DOI] [PubMed] [Google Scholar]
- 39.Klarenbeek BR, Veenhof AA, Bergamaschi R, et al. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg. 2009;249:39–44. doi: 10.1097/SLA.0b013e31818e416a. [DOI] [PubMed] [Google Scholar]
- 40.Klarenbeek BR, Bergamaschi R, Veenhof AA, et al. Laparoscopic versus open sigmoid resection for diverticular disease: follow-up assessment of the randomized control Sigma trial. Surg Endosc. 2011;25:1121–1126. doi: 10.1007/s00464-010-1327-0. [DOI] [PubMed] [Google Scholar]