Abstract
Purpose
The Ministry of Health and Welfare recently designated 35 major trauma-specified centers (MTSC). The purpose of this study is to determine changes in patient flow and designated hospitals, and to describe the role of the emergency medical information center (EMIC) in a regional trauma care system.
Methods
Data of trauma patient inter-facility transfer arrangement by one EMIC were reviewed for 2 months before and after the designation of MTSC. The data included success or failure rates of the arrangement, time used for arrangement, and inquiring and accepting facility.
Results
At pre- and post-designation study period, there were 540 and 433 trauma patient inter-facility transfers arranged by EMIC, respectively. The median time used for arrangement decreased from 9.3 to 7.7 minutes (P = 0.007). Arrangement failure rate was 3.5% and 2.5%, respectively, with no significant interval change (P = 0.377). The percentage of inquiring MTSC decreased from 49.1 to 36.9% (P < 0.001). The percentage of accepting MTSC increased from 20.2 to 37.4% (P < 0.001).
Conclusion
With the designation of MTSC, EMIC could arrange inter-facility transfers more quickly. The hospitals wanted more trauma patients after the designation. There would be a concentration of trauma patients to MTSCs in our region. Further studies are needed for scientific evidence on patient outcome.
Keywords: Trauma centers, Information services, Hospital emergency service, Referral and consultation
INTRODUCTION
The Ministry of Health and Welfare designated 35 major trauma-specified centers (MTSC) in April 2010 via preliminary designation in Many 2009, and those are high-level trauma centers in the existing system. With designation of a facility as a trauma center, the government induces the necessary resources and administrative changes to establish a trauma care service within that facility [1]. High-level trauma centers are equipped with workforce, facilities, and instruments to diagnose and treat severely injured patients. But, there was recent social concern on incidences where emergency patients were left to wander large medical facilities with large resources in Daegu. There was delay in finding available facilities due to weak coordination systems for inter-facility transfer.
Construction of regional trauma systems improves outcome of trauma patients [2-4]. To achieve the purpose of a trauma system to get the right patient to the right hospital at the right time, organized and coordinated means of systemic approach is needed [5]. Major injury patients transported to small facilities need to be transferred to high-level trauma centers. But, exhaustion of medical resources in high-level trauma centers due to overcrowding is related to long waits, undesired outcomes of patients, and high social expenses [6,7]. Optimal matching of patient needs with hospital capabilities relies on appropriate transfers into the high-level trauma centers as well as "back-transport" of patients from high-level trauma centers to lowlevel facilities.
Our emergency medical information center (EMIC) has performed structured inter-facility transfer arrangements since 2001. The first purpose of this study is to determine necessary changes of designated hospitals and trauma patient flow in a regional trauma care system. The second purpose is to describe the role of EMIC.
METHODS
Study design
This was a pre-post observational study designed to assess the effect of designation of MTSC on performance of inter-facility transfer arrangements by one EMIC.
The study was deemed exempt from review and informed consent by the institutional review board because of the observational nature of the study.
Study setting and population
Our EMIC has been entrusted to a wide regional emergency center by the Ministry of Health and Welfare in 2001. This EMIC is in charge of urban areas of two cities with populations of 4.7 million. The area has about 5,600 medical facilities with 43 designated emergency medical centers including 4 MTSCs.
The EMIC has performed arrangements for available medical facilities to diverse inquirers of laypersons, ambulance crews and medical providers on a 24 hours/7 days basis. Most are performed by emergency medical technicians under supervision of board-certificated physicians. On performance of the arrangement, basic data of availability of emergency department bed, intensive care unit bed, inward bed, computed tomography, ventilator, etc., are available via internet. The authors' EMIC has secured cellular phone numbers of cooperative physicians on a volunteer basis. They are comprised of diverse specialties in diverse medical facilities.
Emergency medical providers of a transferring facility request inter-facility transfer to the telephone number 1339. Acceptance of transfer is decided by the physicians of each specialty or emergency department of the receiving hospital under mediation of the EMIC workforce. Sometimes, EMIC attempts several calls to find a receiving hospital. Telephone number, call time, and content of calls were recorded automatically. Data of each arrangement case were recorded on the electrical database of EMIC.
Measurements
Data of trauma patient inter-facility transfer arrangement by our EMIC were reviewed for 2 months before (September and December, 2008) and after (September and December, 2010) the designation of MTSC. The data included success or failure of arrangement, time used for the arrangement, and name of inquiring and accepting facility. We measured the percentage of MTSC hospitals that requested inter-facility transfer in the pre- and post-designation period. We measured the percentage of MTSC hospitals that accepted inter-facility transfer, as well. These processes would describe the trend of patient flow between MTSC hospitals and non-MTSC hospitals in our region. Missing rates of each data component was no more than 3%. Burn patient data were excluded as there is an additional burn transfer system in the region. Asphyxia and drowning patient data were excluded also.
Data analysis
Data were analyzed using PASW 18.0 (SPSS Inc., Chicago, IL, USA). Analyses for continuous and categorical variables were performed using the Student's t-test or Mann-Whitney U test and χ2 test, respectively. All tests for significance were two-tailed with an alpha level of 0.05.
RESULTS
At pre- and post-designation study period, there were 540 and 433 trauma patient inter-facility transfers arranged by EMIC, respectively.
The proportion of male patients in total of both periods was 69.8%. The most common age range was in their 40s (18.5%). The common ages were in the 50s (18.1%), 60s (14.0%), 30s (12.6%), 20s (11.8%), and 10s (9.8%) in sequence.
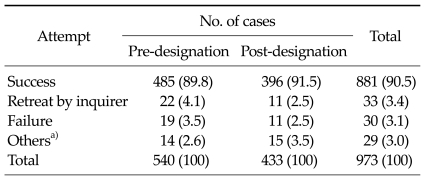
We compared median of time used for arrangement of inter-facility transfer in pre-designation period with postdesignation period. It decreased from 9.3 to 7.7 minutes (P = 0.007). Arrangement failure rate was 3.5% and 2.5%, respectively with no significant interval change (P = 0.377, Table 1).
Table 1.
Results of arrangement attempt of inter-facility transfer
Values are presented as number of cases (%).
a)Missing data.
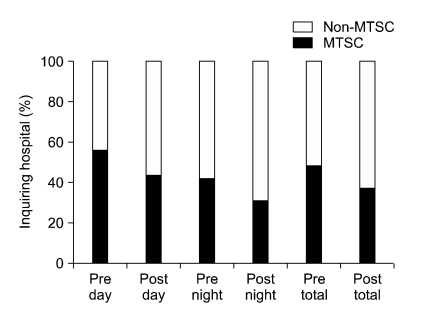
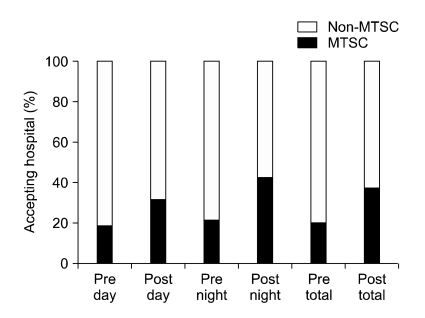
The percentage of inquiring MTSCs decreased after designation from 49.1 to 36.9%. Day and night time showed the same feature (P < 0.001, Fig. 1). The percentage of accepting MTSCs increased after designation from 20.2 to 37.4% (P < 0.001, Fig. 2). Day and night time showed the same feature.
Fig. 1.
Ratio of inquiring hospitals in pre- and post-designation period. MTSC, major trauma-specified center.
Fig. 2.
Ratio of accepting hospitals in pre- and post-designation period. MTSC, major trauma-specified center.
DISCUSSION
The concept of trauma system has evolved from 'injured patients to nearest facilities quickly' to 'severely injured patients to definitive care facilities quickly' to 'right patients to right facilities in right time' [8]. Before the 1970s, trauma patients were transported to nearest facilities without field triage. In the 1970's, major injury patients began to be concentrated in high-level trauma centers according to exclusive trauma system [1]. The system was based on the concept that better outcomes would result from more experienced facilities with large volume of injured patients where trauma teams provide coordinated resuscitation, evaluation, and definitive operative management [1]. The acute care facilities should be categorized according to their ability to provide trauma care, and patients are distributed to each level of trauma care facilities according to severity. But in reality, minor injury patients were concentrated to high-level trauma centers also due to overtriage in prehospital and inter-facility transfer level. Overcrowding of the high-level trauma centers resulted in exhaustion of medical resources of the centers, waste of social resources, and worse outcome. Some trauma centers did not want more patients [9-11]. The trauma registry that enables comparison of outcome in regions with different trauma systems brought forth the evolution of the trauma system. In the 1990's, the concept of an inclusive trauma system was introduced. It was designed to care for all injured patients in a given geographical area and therefore all acute care facilities are expected to participate in such trauma systems [12]. In an inclusive trauma system, there should be collaboration between government, emergency medical services, and acute care facilities [13]. But the inclusion system also has theoretical disadvantages [12]. Spreading the volume of trauma care among more centers may diminish provider experience and efficiency of care in high-level centers. Inclusive systems may also delay definitive care for patients that instead should have been triaged directly from the injury scene or transferred after initial evaluation at smaller facilities to the high-level centers. For policy based on scientific evidence, application of one of both systems in a regional level needs to be individualized according to patient outcome.
This study is related to 2 components of trauma systems. The first is facility infrastructure. The change of designated hospitals in our region would be reflected on inter-facility transfer patterns. The second is inter-facility transfer systems. The World Health Organization and other authors have assessed the maturity of trauma systems of a community with the existence of essential components [2,14]. Many of the components including facility verification and accreditation are established with legislative and administrative governmental support. In a mature trauma system, written protocols of inter-facility transfer, policies describing the type of trauma patients that should (or should not) be transferred to non-trauma designated facilities, and assessment of emergency department compliance with trauma transfer criteria exist formally. In formal trauma systems, theoretically, receiving facilities are decided on according to the trauma system itself. But in practice, there should be agreement on inter-facility transfer between transferring and receiving physicians and requires several tries to find final receiving center [9]. Recently there has been consensus that the existing formal system is not adequate and coordination in system-level organization is needed [7].
EMIC for coordination is a relatively new concept. Epley et al. [9] reported an organized system combining an information center with a formal inter-facility transfer system. Before activity of the center, the interval from transfer decision by a transferring physician to decision acceptation of the receiving physician was 30.5 minutes, conservatively. In fact, it could be 1 to 2 hours with anecdotal cases of 6 and 12 hours. With activity of the center, it decreased to 10.0 minutes. Necessity of coordination has been described in other time-critical conditions as well. Coordinators with single telephone numbers decreased time to balloon angioplasty in transferred ST elevation myocardial infarction patients [15,16]. Notification to receiving neurologists via our EMIC decreased door-to-drug time in transferred acute cerebral infarction patients [17].
Our results showed that the request for inter-facility transfer by the designated hospitals decreased, and the acceptance increased. It would reflect internal changes of MTSCs on treatment of trauma patients.
Our study has limitations. Like other studies on trauma systems, our results can not be generalized. There could be regions where most designated facilities are severely overcrowded, and do not want to treat more trauma patients. The second is that our study is not related to patient outcome. Concentration of trauma patients to MTSCs may have a positive or negative effect on the outcome of a region. The study by Epley et al. [9] was also criticized due to lack of outcome results. But, decision of the outcome was not the purpose of our study. The trauma registry, more extensive than the current form, was proposed to resolve scientific gaps on outcome study of inter-facility transfer of trauma patients [18]. With the registry data, the outcome study for comparison of each trauma system would also become easier. The third is that inter-facility transfer is not the only way of receiving trauma patients. But, we believe that the attitude of the MTSCs on trauma patients would be similar for the patients via other methods.
In conclusion, with designation of MTSC, EMIC could arrange inter-facility transfer more quickly. The hospitals wanted more trauma patients after the designation. There would be concentration of trauma patients to MTSCs in our region. Further studies are needed for scientific evidence on patient outcome.
ACKNOWLEDGEMENTS
The authors wish to express appreciation to the information processing engineer of our EMIC for providing data.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Boyd DR, Cowley RA. Comprehensive regional trauma/emergency medical services (EMS) delivery systems: the United States experience. World J Surg. 1983;7:149–157. doi: 10.1007/BF01655923. [DOI] [PubMed] [Google Scholar]
- 2.Mann NC, Mackenzie E, Teitelbaum SD, Wright D, Anderson C. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005;58:136–147. doi: 10.1097/01.ta.0000151181.44658.0a. [DOI] [PubMed] [Google Scholar]
- 3.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Guss DA, Meyer FT, Neuman TS, Baxt WG, Dunford JV, Jr, Griffith LD, et al. The impact of a regionalized trauma system on trauma care in San Diego County. Ann Emerg Med. 1989;18:1141–1145. doi: 10.1016/s0196-0644(89)80048-4. [DOI] [PubMed] [Google Scholar]
- 5.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979;114:455–460. doi: 10.1001/archsurg.1979.01370280109016. [DOI] [PubMed] [Google Scholar]
- 6.Harrington DT, Connolly M, Biffl WL, Majercik SD, Cioffi WG. Transfer times to definitive care facilities are too long: a consequence of an immature trauma system. Ann Surg. 2005;241:961–966. doi: 10.1097/01.sla.0000164178.62726.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glickman SW, Kit Delgado M, Hirshon JM, Hollander JE, Iwashyna TJ, Jacobs AK, et al. Defining and measuring successful emergency care networks: a research agenda. Acad Emerg Med. 2010;17:1297–1305. doi: 10.1111/j.1553-2712.2010.00930.x. [DOI] [PubMed] [Google Scholar]
- 8.Sasser SM, Hunt RC, Sullivent EE, Wald MM, Mitchko J, Jurkovich GJ, et al. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009;58(RR-1):1–35. [PubMed] [Google Scholar]
- 9.Epley EE, Stewart RM, Love P, Jenkins D, Siegworth GM, Baskin TW, et al. A regional medical operations center improves disaster response and inter-hospital trauma transfers. Am J Surg. 2006;192:853–859. doi: 10.1016/j.amjsurg.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 10.Esposito TJ, Crandall M, Reed RL, Gamelli RL, Luchette FA. Socioeconomic factors, medicolegal issues, and trauma patient transfer trends: is there a connection? J Trauma. 2006;61:1380–1386. doi: 10.1097/01.ta.0000242862.68899.04. [DOI] [PubMed] [Google Scholar]
- 11.Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? Am J Surg. 2009;198:e35–e38. doi: 10.1016/j.amjsurg.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Position paper on trauma care systems. Third National Injury Control Conference April 22-25, 1991, Denver, Colorado. J Trauma. 1992;32:127–129. [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services, Health Resources and Services Administration. Washington DC: US Department of Health and Human Services; 2006. [cited 2011 July 1]. Model trauma system planning and evaluation. Available from: http://www.kstrauma.org/download/ModelTraumaSystemPlanningandEvaluation.pdf. [Google Scholar]
- 14.World Health Organization. Geneva: WHO; c2011. [cited 2011 July 1]. Trauma system maturity index [Internet] Available from: http://www.who.int/violence_injury_prevention/services/traumacare/maturity_index/en/index.html. [Google Scholar]
- 15.Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007;116:729–736. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 16.Henry TD, Unger BT, Sharkey SW, Lips DL, Pedersen WR, Madison JD, et al. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005;150:373–384. doi: 10.1016/j.ahj.2005.01.059. [DOI] [PubMed] [Google Scholar]
- 17.Kim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, et al. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009;16:1331–1335. doi: 10.1111/j.1468-1331.2009.02762.x. [DOI] [PubMed] [Google Scholar]
- 18.Lossius HM, Kristiansen T, Ringdal KG, Rehn M. Interhospital transfer: the crux of the trauma system, a curse for trauma registries. Scand J Trauma Resusc Emerg Med. 2010;18:15. doi: 10.1186/1757-7241-18-15. [DOI] [PMC free article] [PubMed] [Google Scholar]