Abstract
Purpose
To assess outcomes of levator resection for the surgical correction of congenital and acquired upper lid ptosis in patients with fair to good levator function and evaluation of the relationship between demographic data and success of this operation.
Methods
In a retrospective study, medical records of patients with blepharoptosis who had undergone levator resection over a 10-year period and were followed for at least 3 months were reviewed.
Results
Overall, 136 patients including 60 (44.1%) male and 76 (55.9%) female subjects with a mean age of 20 ± 13.8 years (range, 2 to 80 years) were evaluated, of whom 120 cases (88.2%) had congenital ptosis and the rest had acquired ptosis. The overall success rate after the first operation was 78.7%. The most common complication after the first operation was undercorrection in 26 cases (19.1%), which was more prevalent among young patients (p = 0.06). Lid fissure and margin reflex distance (MRD1) also increased after levator resection (p < 0.001). Age, sex, type of ptosis, amblyopia, levator function, MRD1, lid fissure and spherical equivalent were not predictive of surgical outcomes of levator resection.
Conclusions
Levator resection has a high rate of success and few complications in the surgical treatment of congenital and acquired upper lid ptosis with fair to good levator function. Reoperation can be effective in most cases in which levator resection has been performed.
Keywords: Blepharoptosis, Levator function, Levator resection
Blepharoptosis is usually indicated by a drooping of the upper eyelid and can occur as a unilateral or bilateral condition. Patients with blepharoptosis may complain of blurred vision, eye-strain and abnormal head posture (chin up position in severe cases). The condition can lead to anisometropia and amblyopia in younger patients. Congenital ptosis always coexists with dysgenesis of the levator muscle, which is substituted with fat and fibrous tissue [1]. Acquired ptosis occurs secondary to a variety of etiologies including those which are aponeurotic (senile), neurogenic and mechanical in nature [2].
Several procedures are available for surgical correction of blepharoptosis including levator resection and frontalis suspension (sling procedure). Levator resection is useful for patients with fair to good levator function (>4 mm) while the sling procedure is reserved for cases with poor levator function (<4 mm). Posterior approach techniques like mullerectomy and Fasanella-Servat can also be used in some cases [3]. Herein we report the outcomes of levator resection surgery for congenital and acquired blepharoptosis with fair to good levator function over a 10-year period in the Oculoplastic Service at Labbafinejad Medical Center, a tertiary referral eye care center.
Materials and Methods
This retrospective study includes consecutive patients who had undergone levator resection over a 10-year period from October 1998 to September 2009. Patients with at least 3 months follow-up were enrolled into the study. All patients had more than 4 mm of levator function. Patients with eye prosthesis, thyroid ophthalmopathy, myastheni a gravis, myopathies, chronic progressive external ophthalmoplegia (CPEO), third nerve palsy, neurofibromatosis, blepharophimosis syndrome and orbital trauma were excluded from the study.
Patients' records were reviewed for variables including age, sex, chief complaint, previous operations, history of amblyopia, visual acuity, lid fissure height, lid margin to reflex distance (MRD1), levator function, lid lag, lagophthalmus, Bell's phenomenon (graded from 1 to 4 for each 25% eye elevation from midline), jaw winking and surgical complications. The operative technique consisted of an incision in the upper lid crease followed by levator dissection, resection and reattachment using polypropilene (Prolene; Ethicon Inc., Somerville, NJ, USA) 6-0, or polyester (Mersilene, Ethicon Inc.) 5-0 mattress sutures with intraoperative adjustment when the procedure was performed under local anesthesia. When the patient was under general anesthesia, the upper lid margin was adjusted near the limbus for levator function of 4 to 8 mm, between the limbus and pupil with 8 to 12 mm of levator function, and near the pupil with levator function greater than 12 mm. Levator resection outcomes were evaluated using MRD1 and lid fissure height during the follow-up. The postoperative outcome was considered successful when MRD1 was 3 to 5 mm with asymmetry of less than 1 mm between the MRD1 of both eyes, an acceptable skin crease and lid margin contour without corneal exposure. Numerical data were expressed using paired/independent t-tests, and the Mann-Whitney test. Categorical variables were compared using the chi-square and Fisher exact tests. Correlations were evaluated using the Pearson and Spearman test. At the last step, in order to evaluate the simultaneous effect of variables on success, we used logistic regression. Statistical analysis was performed using the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA).
Results
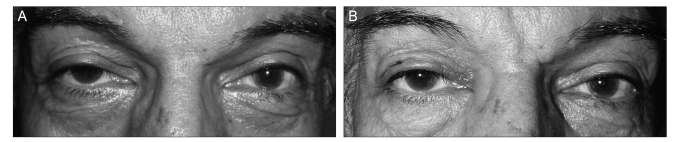
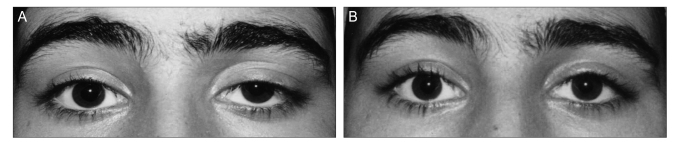
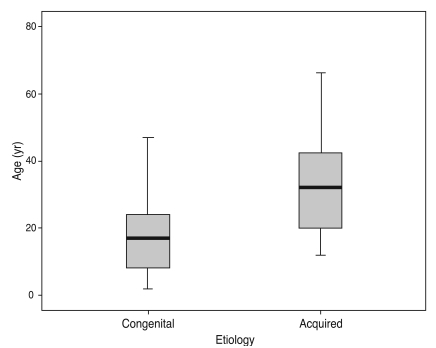
During the 10-year period of the study, 200 patients underwent levator resection (Figs. 1 and 2). One hundred and thirty six subjects (60 [44.1%] male; mean age, 20 ± 13.8; range, 2 to 80 years) with at least 3 months follow up (mean, 14.5 ± 21.4 months) were enrolled for the purpose of this study. All of the patients were Caucasian. The enrolled subjects included 120 cases (88.2%) of congenital ptosis and 16 (11.8%) cases of acquired ptosis. Patients' type of ptosis was defined with history or the time of onset. The mean age of patients with congenital ptosis (18.1 ± 11.8 years) was significantly less than that in acquired ptosis (34.5 ± 18.8 years) (t-test, p < 0.001) (Fig. 3). Most patients had unilateral blepharoptosis (90.5%; 73 [53.7%] left eyes and 50 [36.8%] right eyes). Ten (7.4%) patients had a history of levator resection at other facilities, 11 (8.1%) patients had extraocular muscle dysfunction (superior and inferior rectus muscle restriction), and 7 (5.1%) patients had a history of strabismus surgery before levator resection. Five (3.6%) had a history of intraocular surgery and 1 (0.7%) had a history of ptosis and strabismus surgery. One patient (0.7%) had a miotic pupil, 6 patients (4.4%) had jaw winking, and 4 patients (2.9%) complained of lid lag before surgery. All patients had good tear condition as assessed by tear meniscus thickness before the operation. Out of 92 subjects in whom Bell's phenomenon was measured, 68 patients (82.9%) were normal (3+, 4+) while 14 cases (17.1%) had a weak Bell's phenomenon (1+, 2+). The mean grade of Bell's phenomenon was 3.3 ± 0.9 and no significant difference was observed between the Bell's grade of the right and left eyes (paired t-test, p = 0.30).
Fig. 1.
Preoperative and postoperative photograph of patient with acquired ptosis.
Fig. 2.
Preoperative and postoperative photograph of patient with congenital ptosis.
Fig. 3.
Operation age distribution among patients with congenital and acquired ptosis.
Preoperative evaluations showed that increasing levator function was associated with greater lid fissure (Pearson correlation, r = 0.329, p < 0.001) and MRD1 (Pearson correlation, r = 0.320, p < 0.001). Mean levator function was lower in congenital (9.7 ± 3.8 mm), as compared to acquired, ptosis (11.0 ± 3.6 mm). There was no correlation between age and levator function (Pearson correlation, p = 0.13). We found no difference between male and female subjects in mean lid crease position (t-test, 5.6 vs. 5.8 mm, p = 0.80), but older patients had higher lid creases (Pearson correlation, r = 0.275, p = 0.01).
General anesthesia was used in 48 patients (35.3%) and the remaining 88 patients (64.7%) were operated on under local anesthesia. The mean age of patients operated on under general anesthesia (10.2 ± 9.5 years) was less than those receiving local anesthesia (25.7 ± 12.1 years) (t-test, p < 0.001).
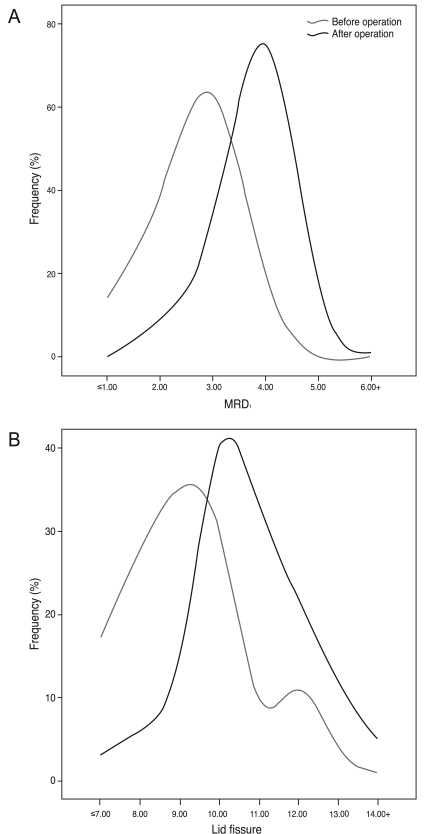
Levator resection increased MRD1 and lid fissure postoperatively. Mean MRD1 increased from 2.2 ± 0.85 mm to 3.5 ± 0.78 mm (paired t-test, p < 0.001) and the lid fissure improved from 8.9 ± 1.6 mm to 10.5 ± 1.5 mm (paired t-test, p < 0.001) in final evaluations after levator resection (Fig. 4).
Fig. 4.
(A) Margin reflex distance (MRD1) distribution before and after surgery. (B) Lid fissure distribution before and after surgery.
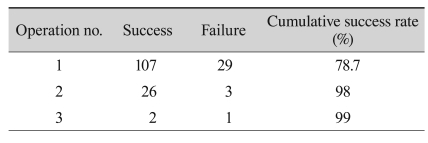
The overall success rate for the first surgery was 78.7% (congenital, 78.3%; acquired, 81.3%). The success rate increased after the second and third operation (Table 1). Twenty-nine patients (21.3%) underwent a second surgery; of those, 26 cases (19.1%) were due to undercorrection and 3 cases (2.2%) were due to overcorrection. Three (2.2%) subjects also underwent a 3rd procedure to treat undercorrection. The execution of a reoperation depended on outcomes and patients' willingness for another intervention.
Table 1.
Number of surgeries and success rate
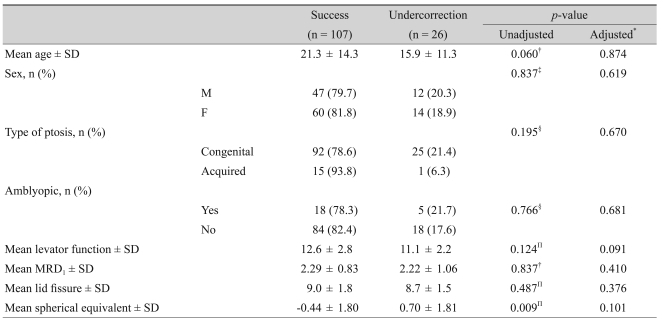
Table 2 shows the comparative results of demographic and clinical characteristics between successful and undercorrected cases after surgery. Success rates of levator resection were comparable in acquired versus congenital ptosis (Fisher's exact test, 93.8% vs. 78.6%, p = 0.30). We did not find any correlation between surgical success and parameters including age, sex, levator function, preoperative value of MRD1 and lid fissure in logistic regression analyses (Table 2). The type of anesthesia also did not affect success rates (chi-square test, 86.4% vs. 77.1% for local versus general anesthesia, respectively, p = 0.2).
Table 2.
Multiple regression analysis between procedures that resulted in success and undercorrection
MRD1 = margin reflex distance.
*Based on logistic regression; †Based on Mann-Whitney test; ‡Based on chi-Square; §Based on Fisher exact test; ∥Based on t-test.
Vision was evaluated by a Snellen chart in all subjects, except in 8 cases in whom it was measured qualitatively. Amblyopia was present in 24 patients (18%) before surgery. Refractive error (spherical equivalent) did not change significantly after levator resection (paired t-test, 0.07 diopters [D] before surgery vs. -0.05 D after surgery p = 0.30). The mean spherical equivalent before surgery was significantly different between the group in which the procedure was a success and the group in which the procedure resulted in undercorrection (t-test, p = 0.009). Preoperative presence of amblyopia and spherical equivalent were not significantly associated with surgical success (Table 2).
In all cases, no intraoperative complications occurred. The most common postoperative complication after the first operation was undercorrection, which was observed in 26 cases (19.1%). In patients with congenital ptosis, undercorrection was present in only 0.8%, and the exposure keratopathy and entropion were observed in 3.3% and 1.7%, respectively. There were no cases of overcorretion and other complications such as notching and ectropion in either the congenital or acquired ptosis patients.
Discussion
Blepharoptosis is a common eyelid problem. In treating these cases, the degree of levator function determines the choice of the operation. Levator resection is employed for cases with good levator function while frontalis sling is reserved for patients with poor levator function. Many surgeons prefer levator resection in eyes with levator function greater than 4 mm and most of them believe that levator resection yields a better lid contour and position as compared to frontalis sling [4].
Levator resection outcomes are not absolutely predictable. The overall success rate after an initial surgery in our series was 78.7%; success rates increased after the second and/or third procedures. This suggests that a second and third operation can be effective in most patients that undergo levator resection, but the decision to reoperate should be customized.
In our study, age, sex, type of ptosis, amblyopia, levator function, MRD1, lid fissure and spherical equivalent were not predictors for levator resection outcomes. In a retrospective study, Cates and Tyers [5] performed levator resection in 100 patients less than 7 years of age with congenital ptosis and having a levator function of at least 4 mm. They reported a 75% success rate, which was defined as a postoperative lid margin position within 1 mm of normal. In that study, the most common complication was undercorrection (19%), and overcorrection was much less common (7%). They found that the preoperative amount of levator function was the strongest predictor of a favorable outcome following levator resection surgery. Berlin and Vestal [6] reported a 69% success rate in 58 cases of congenital ptosis, in which success was also defined as a lid margin position within 1 mm of its desired level. Blomgren and Holmstrom [7] published a 52% success rate in cases having a single operation in 55 eyelids. In a report by Jordan and Anderson [8] on 228 cases of levator resection, the success rate was 43%, within the same criteria. In a study by Press and Hubner [9], an 82% success rate was reported in 44 children over 6 years of age with levator function less than 2 mm. Most studies suggest that levator function and ptosis level before surgery are correlated with the outcomes of levator resection. In our study however, preoperative levator function and ptosis level were not significantly associated with the surgical outcomes. On the other hand, our findings showed that undercorrection was the most common complication (19.1%), a finding similar to previous reports.
In this study, congenital ptosis accounted for 88.2% of cases and the majority of patients were teenagers with unilateral ptosis. Delayed intervention in congenital ptosis may reflect late referral to an ophthalmologist or that surgeons prefer to postpone the operation. Advantages of late intervention for upper lid ptosis include better cooperation by older subjects, improved success rates and the possibility of using local anesthesia. The main indication for operating on children less than 3 years of age is to prevent amblyopia [4]. Lee et al. [10] suggested that in patients with no risk of amblyopia, the operation can be postponed, so that more accurate levator function measurements can be obtained. Levator resection did not affect refractive error in patients without amblyopia in our study. In this study, 4.4% of patients had jaw winking, a finding which is comparable to that seen in other studies (8%, Lee et al. [10]).
In conclusion, levator resection has a high success rate with few complications in the surgical treatment of both congenital and acquired upper lid ptosis in patients with fair to good levator function. Undercorrection was the most common complication, which is a result similar to that found in previous reports. Reoperation can be effective in most cases. Age, sex, type of ptosis, amblyopia, levator function, MRD1, lid fissure and spherical equivalent were not predictors for favorable outcomes of levator resection in this study.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Whitehouse GM, Grigg JR, Martin FJ. Congenital ptosis: results of surgical management. Aust N Z J Ophthalmol. 1995;23:309–314. doi: 10.1111/j.1442-9071.1995.tb00181.x. [DOI] [PubMed] [Google Scholar]
- 2.Chen W. Ptosis (blepharoptosis) In: Chen W, Khan JA, McCord CD, editors. Color atlas of cosmetic oculofacial surgery. 1st ed. Philadelphia: Butterworth-Heinemann; 2004. pp. 188–205. [Google Scholar]
- 3.Tyers AG, Collin JR. Muller's muscle shortening. In: Tyers AG, Collin JR, editors. Colour atlas of ophthalmic plastic surgery. 3rd ed. Oxford: Butterworth-Heinemann; 2008. pp. 190–195. [Google Scholar]
- 4.Keyhani K, Ashenhurst ME. Modified technique and ptosis clamp for surgical correction of congenital pediatric ptosis by anterior levator resection. Facial Plast Surg. 2007;23:156–161. doi: 10.1055/s-2007-984554. [DOI] [PubMed] [Google Scholar]
- 5.Cates CA, Tyers AG. Outcomes of anterior levator resection in congenital blepharoptosis. Eye (Lond) 2001;15(Pt 6):770–773. doi: 10.1038/eye.2001.247. [DOI] [PubMed] [Google Scholar]
- 6.Berlin AJ, Vestal KP. Levator aponeurosis surgery. A retrospective review. Ophthalmology. 1989;96:1033–1036. [PubMed] [Google Scholar]
- 7.Blomgren I, Holmstrom H. Anterior levator resection in congenital genuine blepharoptosis. A follow-up of 55 operated eyelids. Scand J Plast Reconstr Surg. 1986;20:189–195. doi: 10.3109/02844318609006318. [DOI] [PubMed] [Google Scholar]
- 8.Jordan DR, Anderson RL. The aponeurotic approach to congenital ptosis. Ophthalmic Surg. 1990;21:237–244. [PubMed] [Google Scholar]
- 9.Press UP, Hubner H. Maximal levator resection in the treatment of unilateral congenital ptosis with poor levator function. Orbit. 2001;20:125–129. doi: 10.1076/orbi.20.2.125.2631. [DOI] [PubMed] [Google Scholar]
- 10.Lee V, Konrad H, Bunce C, et al. Aetiology and surgical treatment of childhood blepharoptosis. Br J Ophthalmol. 2002;86:1282–1286. doi: 10.1136/bjo.86.11.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]