SUMMARY
Objective
To summarize literature on the concurrent and predictive validity of MRI-based measures of osteoarthritis (OA) structural change.
Methods
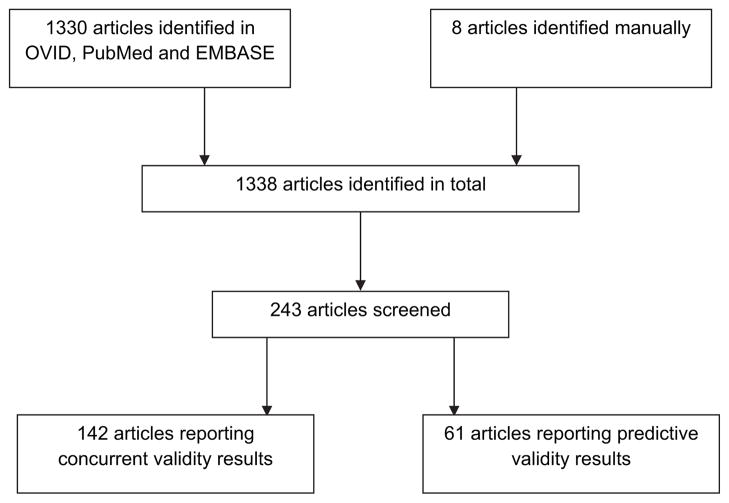
An online literature search was conducted of the OVID, EMBASE, CINAHL, PsychInfo and Cochrane databases of articles published up to the time of the search, April 2009. 1338 abstracts obtained with this search were preliminarily screened for relevance by two reviewers. Of these, 243 were selected for data extraction for this analysis on validity as well as separate reviews on discriminate validity and diagnostic performance. Of these 142 manuscripts included data pertinent to concurrent validity and 61 manuscripts for the predictive validity review. For this analysis we extracted data on criterion (concurrent and predictive) validity from both longitudinal and cross-sectional studies for all synovial joint tissues as it relates to MRI measurement in OA.
Results
Concurrent validity of MRI in OA has been examined compared to symptoms, radiography, histology/pathology, arthroscopy, CT, and alignment. The relation of bone marrow lesions, synovitis and effusion to pain was moderate to strong. There was a weak or no relation of cartilage morphology or meniscal tears to pain. The relation of cartilage morphology to radiographic OA and radiographic joint space was inconsistent. There was a higher frequency of meniscal tears, synovitis and other features in persons with radiographic OA. The relation of cartilage to other constructs including histology and arthroscopy was stronger. Predictive validity of MRI in OA has been examined for ability to predict total knee replacement (TKR), change in symptoms, radiographic progression as well as MRI progression. Quantitative cartilage volume change and presence of cartilage defects or bone marrow lesions are potential predictors of TKR.
Conclusion
MRI has inherent strengths and unique advantages in its ability to visualize multiple individual tissue pathologies relating to pain and also predict clinical outcome. The complex disease of OA which involves an array of tissue abnormalities is best imaged using this imaging tool.
Keywords: Osteoarthritis, Magnetic resonance imaging, Validity
Introduction
Magnetic Resonance Imaging (MRI) is being developed as a method to assess joint morphology in osteoarthritis (OA), with the goal of providing a sensitive non-invasive tool for the study of healthy and diseased states, and a means of assessing the effectiveness of interventions for osteoarthritis. Traditionally structural assessment of OA has relied upon the plain radiograph which has capacity to image the joint space and osteophytes1. MRI has many advantages in visualizing the joint, and recent efforts are yielding a variety of approaches that offer the potential for monitoring this prevalent synovial joint disease2. Because OA is a disease of the whole synovial joint, not just the cartilage, measurements of structure need to be seen broadly and capture important anatomic features, including osteophytes, effusions, meniscal tears, subchondral bone architectural changes or ligamentous instability, in addition to cartilage loss2. There is an abundant literature describing the concurrent validity of MRI as it relates to comparable constructs such as histology and radiography but little if any effort has been made to systematically summarize this literature.
Similarly the merits of any OA structural assessment will undoubtedly be assessed for their clinical relevance. There are multiple determinants of pain and functional limitation in OA and there may be many more unknown3. Many studies have examined whether the loss of structural integrity is in some way the physical correlate of these symptoms. Traditionally most epidemiologic studies have relied upon plain radiography to define disease. The major limitation of this method is that measures of symptoms correlate poorly with x-ray features. Less than 50% of people with evidence of OA on plain radiographs have symptoms related to these findings4. Uncertainty as to whether measurements of MRI structure alone will adequately reflect what structure connotes, or whether other metrics of structure should also be considered, need to be systematically evaluated. The relationships between structure and pain and/or function and between structure and future outcomes (e.g., arthroplasty) are critical in determining the clinical relevance of MRI.
In psychometrics, validity refers to the degree to which a study accurately reflects or assesses the specific concept that the researcher is attempting to measure. There are many types of validity of which one, criterion validity, is used to demonstrate the accuracy of a measure or procedure by comparing it with another measure or procedure which has been demonstrated to be valid. There is a contention in the OA field about the validity of a number of biomarkers and clinical endpoints and their inclusion here is in an effort to be comprehensive and does not diminish the credible concerns about the lack of well validated clinical endpoints5. If the test data and criterion data are collected at the same time, this is referred to as concurrent validity evidence. If the test data is collected first in order to predict criterion data collected at a later point in time, then this is referred to as predictive validity evidence. The purpose of this systematic review was to summarize the OA MRI literature with regards to both concurrent and predictive validity.
Material and methods
Systematic literature search details
An online literature search was conducted using the OVID MEDLINE (1945–), EMBASE (1980–) and Cochrane databases (1998–) to identify the articles published up to April 2009, with the search entries “MRI”, and “osteoarthritis”, “osteoarthritides”, “osteoarthrosis”, “osteoarthroses”, “degenerative arthritis”, “degenerative arthritides”, or “osteoarthritis deformans”. The abstracts of the 1330 citations received with this search were then preliminarily screened for relevance by two reviewers (KH and DJH). For this preliminary search, all articles which used MRI, in some form, on patients with osteoarthritis of the knee, hip, or hand were included. Although review articles were not included (see Inclusion/exclusion criteria), citations found in any review articles which were not already included in our preliminary search were screened for possible inclusion in this study. This added 7 more relevant studies to our search. One further article was added, before publication, by one of authors of this meta-analysis bringing the preliminary total to 1338.
Inclusion/exclusion criteria
Only studies published in English were included. Studies presenting non-original data were excluded, such as reviews, editorials, opinion papers, or letters to the editor. Studies with questionable clinical relevance and those using non-human subjects or specimens were excluded. Studies in which rheumatoid, inflammatory, or other forms of arthritis were included in the OA datasets were excluded, as well as general joint-pertinent MRI studies not focused on OA. Studies with no extractable, numerical data were excluded. Only those articles which had some measure of diagnostic performance were included. Any duplicates which came up in the preliminary search were excluded. Of the preliminary 1338 abstracts, 243 were selected for data extraction (Fig. 1).
Fig. 1.
Flow chart of the screening process for articles included in the systematic review.
Data abstraction
Two reviewers (KH and LM) independently abstracted the following data: (1) patient demographics; (2) MRI make, sequences and techniques used, tissue types viewed; (3) study type and funding source; (4) details on rigor of study design to construct the Downs methodological quality score6; (5) MRI reliability/reproducibility data; (6) MRI diagnostic measures and performance; (7) gold standard measures against which the MRI measure was evaluated; (8) treatment and MRI measures (when appropriate).
The Downs methodological quality score6 collects a profile of scores for both randomized trials and observational studies in terms of quality of reporting, internal validity (bias and confounding), power, external validity so that the overall study quality score reflects all of these elements. Answers were scored 0 (No) or 1 (Yes), except for one item in the Reporting subscale, which scored 0–2 and the single item on power, which was scored 0–5. The possible range is from 0 to 27 where 0 represents poor quality and 27 optimal quality.
We used a data abstraction tool constructed in EpiData (Entry version 2.0 Odense, Denmark) and more than one reviewer undertook the data abstraction. The data collection forms were designed to target the objectives of the review, and were piloted prior to conducting the study.
The outcomes for psychometric properties on MRI were examined using the OMERACT filter7,8. The specific focus of this review is upon the truth domain: is the measure truthful, does it measure what it intends to measure? More specifically we were interested in criterion validity; for both the concurrent [Does it agree (by independent and blind comparison) with a measure that reflects the same concept] and predictive [Does it predict (by independent and blind comparison) a future ‘gold standard’] validity of MRI in OA. If the test data and criterion data are collected at the same time, this is referred to as concurrent validity evidence. If the test data is collected first in order to predict criterion data collected at a later point in time, then this is referred to as predictive validity evidence.
It is critical to delineate what we mean by the various terms used, as current usage is often incorrect, and this ambiguity may stem from an incorrect understanding of appropriate definitions. Whilst there are several definitions that have been proposed9–13, the brief synthesis of some working definitions is as follows:
biological marker (biomarker)— a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes or pharmacologic responses to a therapeutic agent.
clinical endpoint—a clinically meaningful measure of how a patient feels, functions, or survives.
For the purposes of this analysis, MRI (the biomarker) is directly compared both to clinical endpoints (symptoms, total knee replacement (TKR)) as well as other biomarkers (including radiography, CT, histology, arthroscopy, alignment). The presentation of the data in the results reflects presentation of clinical endpoints before comparison with other biomarkers.
There is some overlap in the manuscripts for which data is extracted for these two types of validity. The large majority of studies for concurrent validity were cross-sectional studies although some longitudinal studies reported cross-sectional results and thus are included in the concurrent validity data. There is no attempt made to create summary estimates as the validity effect measures [i.e., odds ratio (OR), Beta coefficient, r, P-value of difference] used in this literature are very heterogeneous.
Results
Concurrent validity (Table I)
Table I.
Summary table of studies reporting data on concurrent validity of MRI in OA
| Reference: Author, Journal, Year, PMID |
Whole sample size |
No. of cases |
No. of controls |
Age, yrs, mean(SD), range | No. (%) of females | Quantitative cartilage |
Compositional techniques |
Semi-quantitative | Cartilage | Synovium | Bone | Bone marrow lesions |
Meniscus | Ligament | Study design |
Score of methodological quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chan WP; American Journal of Roentgenology; 1991; 189204036 |
20 | 20 | 0 | 58(Range: 42–73) | 11 | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 6 |
| McAlindon TE; Annals of the Rheumatic Diseases; 1991; 199486190 |
12 | No | No | Yes | Yes | Yes | Yes | No | Yes | No | Case control | 3 | ||||
| Li KC; Magnetic Resonance Imaging; 1988; 339872891 |
10 | 10 | 0 | (Range: 33–78) | 9(90%) | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective |
4 |
| Fernandez-Madrid F; Magnetic Resonance Imaging; 1994; 793465692 |
92 | 52 | 40 | Controls: 49(15), (Rang: 22–78); OA patients: 55(14), (Range: 25–86) |
60 | No | No | Yes | Yes | Yes | No | No | Yes | No | Cross-sectional | 11 |
| Karvonen RL; Journal of Rheumatology; 1994; 796607527 |
92 | 52 | 40 | Reference: 49(15), (Range: 22–78); All OA patients: 55(14), (Range: 25 –86); Bilateral OA: 53(13), (Range: 25–73) |
60 | Yes | No | No | Yes | No | Yes | No | No | No | Case control | 11 |
| Peterfy CG; Radiology; 1994; 802942093 | 8 | 5 | 3 | 62(Range: 45–82) | 4(50%) | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 4 |
| Blackburn WD Jr; Journal of Rheumatology; 1994; 803539237 | 33 | 33 | 0 | 62.7(9.1), (Range: 44–79) | 17 | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 6 |
| Broderick LS; American Journal of Roentgenology; 1994; 827370061 | 23 | 13 | 10 | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 4 | ||
| Miller TT; Radiology; 1996; 881655294 | 384 | 47(Range: 14–88) | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 8 | |||
| Dupuy DE; Academic Radiology; 1996; 895918157 | 7 | TKA patients: (Range: 64–75); Asymptomatic: 35(Range: 25–35) | 3 | Yes | No | No | Yes | No | No | No | No | No | Other | 6 | ||
| Kenny C; Clinical Orthopaedics & Related Research; 1997; 918621595 | 136 | No | No | Yes | No | No | No | No | Yes | No | Case control | 6 | ||||
| Breitenseher MJ; Acta Radiologica; 1997; 933224896 | 60 | 12 | 48 | 37(14.3), (Range: 15–68) | 30(50%) | No | No | Yes | No | No | No | No | Yes | No | Cross-sectional | 5 |
| Ostergaard M; British Journal of Rheumatology; 1997; 940286097 | 46 | 14 | 47 | 70(Range: 24–85) | No | No | No | No | Yes | No | No | No | No | Cross-sectional | 7 | |
| Trattnig S; Journal of Computer Assisted Tomography; 1998; 944875498 | 20 | 20 | 0 | 72.2(Range: 62–82) | 18 | No | No | Yes | Yes | No | No | No | No | No | Other | 8 |
| Kawahara Y; Acta Radiologica; 1998; 952944062 | 72 | 58(Range: 41–74) | 46 | No | No | Yes | Yes | No | No | No | No | No | Other | 6 | ||
| Drape JL; Radiology; 1998; 964679263 | 43 | 43 | 0 | 63(Range: 53–78) | 30 | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 5 |
| Eckstein F; Clinical Orthopaedics & Related Research; 1998; 967804256 | 8 | 0 | 8 | 50.6(Range: 39–64) | Yes | No | No | Yes | No | No | No | No | No | Other | 7 | |
| Uhl M; European Radiology; 1998; 972442358 | 22 | (Range: 50–72) | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 5 | |||
| Boegard T; Acta Radiologica - Supplementum; 1998; 975912199 | 61 | No | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective |
5 | ||||
| Bachmann GF; European Radiology; 1999; 993339964 | 320 | 29.3(8.7), (Range: 13–56) | 122 | No | No | Yes | Yes | No | No | No | Yes | No | Cross-sectional | 7 | ||
| Cicuttini F; Osteoarthritis & Cartilage; 1999; 10329301100 | 28 | Males: 40.4(Range: 42–58); Females: 31.2(8.6); | 11 | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 7 | ||
| Boegard T; Annals of the Rheumatic Diseases; 1999; 10343536101 | 58 | Women: 40.4(Range: 42–58); Men: 57(49.5), (Range: 41–57) | 29 | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 6 | ||
| Adams JG; Clinical Radiology; 1999; 1048421644 | 62 | 32 | 30 | No | No | Yes | Yes | No | No | No | Yes | No | Case control | 8 | ||
| Pham XV; Revue du Rhumatisme; 1999; 10526380102 | 10 | 10 | 10 | 67.2(7.34), (Range: 57–80) | 6 | No | No | Yes | No | No | No | No | No | Yes | Cross-sectional | 13 |
| Gale DR; Osteoarthritis & Cartilage; 1999; 1055885043 | 291 | 233 | 58 | No | No | No | No | No | No | No | Yes | No | Case control | 10 | ||
| Kladny B; International Orthopaedics; 1999; 1065329059 | 26 | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 6 | ||||
| Zanetti M; Radiology; 2000; 10831707103 | 16 | 16 | 0 | 67(Range: 43–79) | 15 | Yes | No | No | Yes | No | Yes | Yes | No | No | Cross-sectional | 6 |
| Jones G; Arthritis & Rheumatism; 2000; 11083279104 | 92 | 92 | 0 | Boys: 12.8(2.7); Girls: 12.6(2.9) | 43 | Yes | No | No | Yes | No | Yes | No | No | No | Cross-sectional | 13 |
| McCauley TR; American Journal of Roentgenology; 2001; 11159074105 | 193 | 40(Range: 11–86) | 83 | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 8 | ||
| Wluka AE; Annals of the Rheumatic Diseases; 2001; 11247861106 | 81 | 42 | 39 | Cases: 58(6.1); Controls: 56(5.4) | 81(100%) | Yes | No | Yes | Yes | No | No | No | No | No | Case control | 16 |
| Felson DT; Annals of Internal Medicine; 2001; 1128173614 | 401 | 401 | 0 | 66.8 | No | No | Yes | No | No | No | Yes | No | No | Cross-sectional | 13 | |
| Hill CL; Journal of Rheumatology; 2001; 1140912715 | 458 | 433 | 25 | 67 | (34%) | No | No | Yes | No | Yes | No | No | No | No | Case control | 13 |
| Kawahara Y; Journal of Computer Assisted Tomography; 2001; 11584226107 | 35 | 57(Range: 33–70) | 23 | No | No | Yes | Yes | No | No | No | Yes | No | Cross-sectional | 8 | ||
| Arokoski JP; Annals of the Rheumatic Diseases; 2002; 11796401108 | 57 | 27 | 30 | Cases: 56.2(4.9), (Range: 47–64); Controls: 56.3(4.5), (Range: 47–64) | 0 | Yes | No | No | No | No | No | No | No | No | Case control | 8 |
| Bergin D; Skeletal Radiology; 2002; 11807587109 | 60 | 30 | 30 | Cases: 50; Controls: 57 | No | No | Yes | No | No | No | No | Yes | Yes | Case control | 9 | |
| Beuf O; Arthritis & Rheumatism; 2002; 11840441110 | 46 | 18 | 28 | Mild OA: 68(9.1); Severe OA: 70(6.3) | 17 | Yes | No | No | No | No | No | No | No | No | Case control | 5 |
| Arokoski MH; Journal of Rheumatology; 2002; 12375331111 | 57 | 27 | 30 | Cases: 56.2(4.9), (Range: 47–64); Controls: 56.3(4.5), (Range: 47–64) | 0 | Yes | No | No | Yes | No | No | No | No | No | Case control | 8 |
| Bhattacharyya T; Journal of Bone & Joint Surgery - American Volume; 2003; 1253356516 | 203 | 154 | 49 | Cases: 65; Controls: 67 | No | No | Yes | No | No | No | No | Yes | No | Case control | 9 | |
| Link TM; Radiology; 2003; 1256312817 | 50 | 50 | 0 | 63.7(11.5), (Range: 43–81) | 30 | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 6 |
| Tiderius CJ; Magnetic Resonance in Medicine; 2003; 12594751112 | 17 | 50(Range: 35–70) | 4 | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 6 | ||
| Cicuttini FM; Arthritis & Rheumatism; 2003; 1263242128 | 252 | 60.2(10) | 157962%) | Yes | No | No | Yes | No | Yes | No | No | No | Cross-sectional | 9 | ||
| Cicuttini FM; Clinical & Experimental Rheumatology; 2003; 12673893113 | 81 | 42 | 39 | ERT: 58(6.1); Controls: 56(5.4) | 81(100%) | Yes | No | No | Yes | No | Yes | No | No | No | Case control | 12 |
| Sowers MF; Osteoarthritis & Cartilage; 2003; 1280147818 | 120 | 60 | 60 | no OAK, no Pain: 45(0.8); OAK, no Pain: 46(0.6); No OAK, Pain: 47(0.8); OAK and Pain: 47(0.7) | (100%) | No | No | Yes | Yes | No | No | Yes | No | No | Case control | 11 |
| McGibbon CA; Osteoarthritis & Cartilage; 2003; 1281461160 | 4 | No | No | Yes | Yes | No | No | No | No | No | Other | 5 | ||||
| Cicuttini FM; Clinical & Experimental Rheumatology; 2003; 1284605046 | 157 | 157 | 0 | 62(10) | (62%) | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 10 |
| Felson DT; Annals of Internal Medicine; 2003; 1296594151 | 256 | 256 | 0 | Followed: 66.2(9.4); Not followed: 67.8(9.6) | (38.3%) | No | No | Yes | No | No | No | Yes | No | No | Longitudinal prospective |
11 |
| Tarhan S; Clinical Rheumatology; 2003; 14505208114 | 74 | 58 | 16 | OA Patients: 57.4(8.5), (Range: 45–75); Healthy controls: 59.1(5.8), (Range: 46–77) | 60 | Yes | No | Yes | Yes | Yes | No | No | No | No | Case control | 8 |
| Hill CL; Arthritis & Rheumatism; 2003; 1455808919 | 451 | 427 | Knee pain/ROA/Male: 68.3; Knee pain/ROA/Female: 65; No knee pain/ROA/Male: 66.8; No knee pain/ROA/Female: 66.1 | No | No | Yes | No | No | No | Yes | No | No | Cross-sectional | 10 | ||
| Kim YJ; Journal of Bone & Joint Surgery - American Volume; 2003; 14563809115 | 43 | 30(Range: 11–47); Median = 31 | 40 | No | Yes | No | Yes | No | No | No | No | No | Other | 5 | ||
| Lindsey CT; Osteoarthritis & Cartilage; 2004; 1472386829 | 74 | 33 | 21 | Controls: 34.2(12.5); OA1 (KL1/2): 62.7(10.9); OA2(KL3/4): 66.6(11.6) | 39 | Yes | No | No | Yes | No | Yes | No | No | No | Case control | 8 |
| Jones G; Osteoarthritis & Cartilage; 2004; 1472387647 | 372 | 186 | 186 | 45(Range: 26–61) | Yes | No | No | Yes | No | Yes | No | No | No | Case control | 9 | |
| Raynauld JP; Arthritis & Rheumatism; 2004; 1487249048 | 32 | 32 | 0 | 62.9(8.2) | (74%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
10 |
| Wluka AE; Annals of the Rheumatic Diseases; 2004; 1496296020 | 132 | 132 | 0 | 63.1(Range: 41–86) | 71(54%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
10 |
| Cicuttini F; Rheumatology; 2004; 1496320152 | 117 | 117 | 0 | 67(10.6) | (58%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
12 |
| Peterfy CG; Osteoarthritis & Cartilage; 2004; 14972335116 | 19 | 19 | 0 | 61(8) | 4 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Other | 5 |
| Graichen H; Arthritis & Rheumatism; 2004; 15022323117 | 21 | 21 | 0 | 70.6(7.7), (Range: 58–86) | 17 | Yes | No | No | Yes | No | Yes | No | No | No | Cross-sectional | 6 |
| Dashti M; Scandinavian Journal of Rheumatology; 2004; 15163109118 | 174 | 117 | 57 | 61.6(9.5) | 123(70.7%) | Yes | No | No | Yes | No | No | No | No | No | Case control | 11 |
| Arokoski JP; Journal of Clinical Densitometry; 2004; 15181262119 | 57 | 27 | 30 | Cases: 56.2(4.9), Range: (47–64); Controls: 56.3(4.5), (Range: 47–64) | 0 | No | Yes | No | No | No | No | No | No | No | Case control | 9 |
| Dunn TC; Radiology; 2004; 15215540120 | 55 | 48 | 7 | Healthy: 38(Range: 22–71); Mild OA: 63(Range: 46–81); Severe OA: 67 (Range: 43–88) | 30 | No | Yes | No | Yes | No | No | No | No | No | Case control | 8 |
| Regatte RR; Academic Radiology; 2004; 15217591121 | 14 | 6 | 8 | Asymptomatic: 33.5(Range: 22–45); Symptomatic: 45.5(Range: 28–63) | 2 | No | Yes | No | Yes | No | No | No | No | No | Case control | 7 |
| Baysal O; Swiss Medical Weekly; 2004; 15243849122 | 65 | 65 | 0 | 53.1(7), (Range: 45–75) | 65(100%) | Yes | No | Yes | Yes | No | Yes | No | No | No | Cross-sectional | 7 |
| Lerer DB; Skeletal Radiology; 2004; 15316679123 | 205 | 46.5(Range: 15–88); Median = 46 | 113 | No | No | Yes | Yes | No | No | No | Yes | No | Cross-sectional | 6 | ||
| Berthiaume MJ; Annals of the Rheumatic Diseases; 2005; 1537485578 | 32 | Yes | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective |
10 | ||||
| King KB; Magnetic Resonance Imaging; 2004; 15527998124 | 16 | 16 | 0 | Males: Median = 58.5, (11.3), (Range: 43–76); Females: Median = 70 (14.4), (Range: 46–88) | 8(50%) | Yes | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 7 |
| Carbone LD; Arthritis & Rheumatism; 2004; 15529367125 | 818 | Non-users: 74.8(2.94); Antiresportive users: 74.8(2.9) | 818(100%) | No | No | Yes | Yes | Yes | Yes | No | No | No | Cross-sectional | 11 | ||
| Cicuttini F; Journal of Rheumatology; 2004; 15570649126 | 123 | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
6 | ||||
| Wluka AE; Annals of the Rheumatic Diseases; 2005; 1560174238 | 149 | 68 | 81 | Normal: 57(5.8); OA: 63(10.3) | 1499(100%) | No | No | No | No | No | Yes | No | No | No | Longitudinal Prospective |
13 |
| Ding C; Osteoarthritis & Cartilage; 2005; 1572788549 | 372 | 162 | 210 | No cartilage defects: 43.6(7.1); Any cartilage defect: 47(6.1) | (56.5%) | Yes | No | Yes | Yes | No | No | No | No | No | Case control | 9 |
| Hill CL; Arthritis & Rheumatism; 2005; 1575106445 | 433 | 360 | 73 | Cases males: 68.2; Cases females: 65; Control males: 66.8; Control females: 65.8 | 143 | No | No | Yes | No | No | No | No | No | Yes | Case control | 12 |
| Kornaat PR; European Radiology; 2005; 15754163127 | 205 | 205 | 0 | Median = 60; (Range: 43–77) | 163(80%) | No | No | Yes | Yes | No | No | Yes | Yes | No | Cross-sectional | 8 |
| Zhai G; Arthritis & Rheumatism; 2005; 15818695128 | 151 | 23 | 128 | Men: 64(8.1); Women: 62(7.7) | 72 | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 8 |
| Cicuttini F; Osteoarthritis & Cartilage; 2005; 1592263450 | 28 | 28 | 0 | 62.8(9.8) | (57%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
10 |
| Blankenbaker DG; Skeletal Radiology; 2005; 15940487129 | 247 | 74 | 173 | 44 | 126 | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 6 |
| Huh YM; Korean Journal of Radiology; 2005; 15968151130 | 94 | 73 | 21 | RA group: 49.2 (Range: 37–76), Median = 48; OA group: 57.8 (Range: 40–80), Median = 58 | 73 | No | No | Yes | No | Yes | No | No | No | No | Longitudinal Retrospective |
7 |
| von Eisenhart-Roth; Annals of the Rheumatic Diseases; 2006; 15975965131 | 26 | 26 | 0 | 70.4(7.6), (Range: 58–86) | 20 | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 5 |
| Tan AL; Arthritis & Rheumatism; 2005; 16052535132 | 58 | 40 | 18 | Early OA: 56 (Range: 49–69); Chronic OA: 60 (Range: 51–68); Hand OA: 60 (Range: 46–72); | 44 | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Cross-sectional | 7 |
| Lo GH; Arthritis & Rheumatism; 2005; 16145676133 | 268 | 80 | 188 | No BMLs: 64.8(8.5); Medial BMLs: 68.3(7); Lateral BMLs: 66.6(9.5) | (59%) | No | No | Yes | No | No | No | Yes | No | No | Cross-sectional | 10 |
| Li X; Magnetic Resonance in Medicine; 2005; 16155867134 | 19 | 9 | 10 | Cases: Median = 52, (Range: 18–72); Controls: Median = 30, (Range: 22–74) | 8 | No | Yes | No | Yes | No | No | No | No | No | Case control | 7 |
| Rhodes LA; Rheumatology; 2005; 16188949135 | 35 | 35 | 0 | Median = 63; (Range: 49–77) | 23 | No | No | Yes | No | Yes | No | No | No | No | Cross-sectional | 9 |
| Williams A; Arthritis & Rheumatism; 2005; 1625502432 | 31 | 31 | 0 | 67(10.4), 9 (Range: 45–86) | 24(77%) | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 9 |
| Loeuille D; Arthritis & Rheumatism; 2005; 16255041136 | 39 | 39 | 0 | 56.4(12.71) | (56.4%) | No | No | Yes | No | Yes | No | No | No | No | Cross-sectional | 10 |
| Roos EM; Arthritis & Rheumatism; 2005; 16258919137 | 30 | 45.8(3.3) | 10(33.3%) | No | Yes | No | Yes | No | No | No | No | No | Randomized controlled trial |
17 | ||
| Hunter DJ; Journal of Rheumatology; 2005; 1626570253 | 132 | 162 | 0 | 33.5(9.7) | (44.2%) | No | No | Yes | Yes | No | Yes | No | Yes | Yes | Cross-sectional | 8 |
| Nojiri T; Knee Surgery, Sports Traumatology, Arthroscopy; 2006; 1639556433 | 28 | 9 | 21 | 40.3(Range: 16–74) | 17 | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 7 |
| Kimelman T; Invest Radiol; 2006; 16428993138 | 7 | 4 | 3 | Healthy controls: 23; OA cases: 56 | 4 | No | Yes | No | Yes | No | No | No | No | No | Other | 6 |
| Sengupta M; Osteoarthritis & Cartilage; 2006; 16442316139 | 217 | 217 | 0 | 67.3(9.1) | (30%) | No | No | Yes | Yes | Yes | Yes | Yes | No | No | Cross-sectional | 7 |
| Hunter DJ; Arthritis & Rheumatism; 2006; 1650893081 | 257 | 257 | 0 | 66.6(9.2), (Range: 47–93) | (41.6%) | No | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective |
10 |
| Hunter DJ; Arthritis & Rheumatism; 2006; 1664603783 | 217 | 217 | 0 | 66.4(9.4) | (44%) | No | No | Yes | Yes | No | No | Yes | No | No | Longitudinal Prospective |
10 |
| Grainger AJ; European Radiology; 2007; 16685505140 | 43 | 43 | 0 | 64(Range: 48–75) | 19 | No | No | Yes | No | Yes | No | No | Yes | No | Cross-sectional | 8 |
| Cashman PM; IEEE Transactions on Nanobioscience; 2002; 16689221141 | 27 | 10 | 17 | OA patients: (Range: 45–73); Similar age controls: (Range: 50–65); Young healthy controls: (Range: 21–32); | 8(29.6%) | Yes | No | No | Yes | No | No | No | No | No | Other | 6 |
| Torres L; Osteoarthritis & Cartilage; 2006; 1671331021 | 143 | 143 | 0 | 70(10) | (78%) | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cross-sectional | 9 |
| Kornaat PR; Radiology; 2006; 1671446322 | 205 | 97 | 103 | 60 (Range: 43–77) | 163(80%) | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Cross-sectional | 9 |
| Bamac B; Saudi Medical Journal; 2006; 16758050142 | 46 | 36 | 10 | Cases: 41.9 (Range: 20–67); Controls: 39.7 (Range: 21–66) | 25 | No | No | No | No | No | No | No | Yes | No | Case control | 8 |
| Boks SS; American Journal of Sports Medicine; 2006; 16861575143 | 134 | 136 | 132 | 40.8(Range: 18.8–63.8) | No | No | Yes | Yes | No | No | No | Yes | Yes | Cross-sectional | 7 | |
| Koff MF; Osteoarthritis & Cartilage; 2007; 1694931334 | 113 | 113 | 0 | 56(11), (Range: 33–82) | 84 | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 8 |
| Nakamura M; Magnetic Resonance Imaging; 2006; 1707133639 | 63 | 51.8 (Range: 40–59) | 42 | No | No | Yes | No | No | No | No | Yes | No | Cross-sectional | 6 | ||
| Folkesson J; IEEE Transactions on Medical Imaging; 2007; 17243589144 | 139 | 56(Range: 22–79) | (59%) | Yes | No | No | Yes | No | No | No | No | No | Other | 7 | ||
| Li X; Osteoarthritis & Cartilage; 2007; 1730736535 | 26 | 10 | 16 | Healthy: 41.3 (Range: 22–74); OA patients: 55.9 (37–72) | 11 | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Case control | 7 |
| Iwasaki J; Clinical Rheumatology; 2007; 17322963145 | 26 | 26 | 0 | 63.8(Rang: 49–82) | 18 | No | No | No | No | No | No | No | No | No | Cross-sectional | 5 |
| Dam EB; Osteoarthritis & Cartilage; 2007; 1735313231 | 139 | Evaluation set: 55(Range: 21–78); Scan-rescan set: 61 (Range: 26–75) | (54.5%) | Yes | No | No | Yes | No | No | No | No | No | Other | 9 | ||
| Tiderius CJ; Magnetic Resonance in Medicine; 2007; 17390362146 | 18 | 10 | 8 | Controls: 28(Range: 20–47); Cases: 39 (Range: 25–58) | No | Yes | No | Yes | No | No | No | No | No | Case control | 6 | |
| Baranyay FJ; Seminars in Arthritis & Rheumatism; 2007; 17391738147 | 297 | 297 | 58(5.5) | (63%) | Yes | No | No | Yes | No | No | Yes | No | No | Cross-sectional | 16 | |
| Issa SN; Arthritis & Rheumatism; 2007; 1739422554 | 146 | 146 | 0 | 70 | 109 | No | No | Yes | Yes | No | Yes | Yes | Yes | No | Cross-sectional | 8 |
| Hanna F; Menopause; 2007; 17413649148 | 176 | 0 | 176 | 52.3(6.6), (Range: 40–67) | 176(100%) | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 13 |
| Hunter DJ; Annals of the Rheumatic Diseases; 2008; 1747299523 | 71 | 67.9(9.3) | (28.2%) | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Other | 8 | ||
| Hill CL; Annals of the Rheumatic Diseases; 2007; 1749109624 | 270 | 270 | 0 | 66.7(9.2) | 112 | No | No | Yes | Yes | Yes | No | No | No | No | Longitudinal Prospective |
9 |
| Qazi AA; Osteoarthritis & Cartilage; 2007; 17493841149 | 71 | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 8 | ||||
| Lammentausta E; Osteoarthritis & Cartilage; 2007; 17502160150 | 14 | 55(18) | 2 | No | Yes | No | Yes | No | Yes | No | No | No | Other | 5 | ||
| Guymer E; Osteoarthritis & Cartilage; 2007; 17560134151 | 176 | 0 | 176 | 52.3(6.6) | 176(100%) | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Cross-sectional | 11 |
| Nishii T; Osteoarthritis & Cartilage; 2008; 17644363152 | 33 | 23 | 10 | Volunteers: 34(Range: 23–51); Patients: 40(Range: 22–69) | 33(1005) | No | Yes | No | Yes | No | No | No | No | No | Case control | 8 |
| Janakiramanan N; Journal of Orthopaedic Research; 2008; 1776345155 | 202 | 74 | 128 | 61(9) | (73%) | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 11 |
| Lo GH; Osteoarthritis & Cartilage; 2008; 17825586153 | 845 | 170 | 63.6(8.8) | (58%) | No | No | Yes | No | No | No | No | Yes | No | Cross-sectional | 10 | |
| Davies-Tuck M; Osteoarthritis & Cartilage; 2008; 17869546154 | 100 | 100 | 0 | 63.3(10.2) | 61(61%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective |
11 |
| Qazi AA; Academic Radiology; 2007; 17889338155 | 159 | (Range: 21–81) | No | No | Yes | Yes | No | No | No | No | No | Other | 8 | |||
| Folkesson J; Academic Radiology; 2007; 17889339156 | 71 | 56(Range: 22–79) | (59%) | No | No | No | No | No | No | No | No | No | Other | 7 | ||
| Englund M; Arthritis & Rheumatism; 2007; 1805020140 | 310 | 102 | 208 | Cases: 62.9(8.3); Controls: 61.2(8.3) | 211(68%) | No | No | Yes | No | No | No | No | Yes | No | Case control | 15 |
| Kamei G; Magnetic Resonance Imaging; 2008; 18083319157 | 37 | 27 | 0 | Cartilage defect: 51.6(Range: 42–61); No cartilage defect: 54.5(Range: 45–61) | 20 | No | No | Yes | Yes | No | No | No | Yes | No | Case control | 7 |
| Li W; Journal of Magnetic Resonance Imaging; 2008; 18183573158 | 29 | 19 | 10 | OA subjects: 61.7(Range: 40–86); Controls: 31 (Range: 18–40) | 19 | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 5 |
| Amin S; Osteoarthritis & Cartilage; 2008; 1820362986 | 265 | 265 | 67(9) | (43%) | No | No | Yes | Yes | No | No | No | Yes | Yes | Longitudinal Prospective |
11 | |
| Taljanovic MS; Skeletal Radiology; 2008; 18274742159 | 19 | 19 | 0 | 66 | 8 | No | Yes | No | No | No | No | No | No | No | Case control | 8 |
| Oda H; Journal of Orthopaedic Science; 2008; 18274849160 | 161 | 58.5(Range: 11–85) | 98 | No | No | Yes | No | Yes | No | No | Yes | Yes | Cross-sectional | 8 | ||
| Hanna FS; Arthritis Research & Therapy; 2008; 18312679161 | 176 | 52.3(6.6) | (100%) | Yes | No | No | Yes | No | No | No | No | No | Cross-sectional | 10 | ||
| Reichenbach S; Osteoarthritis & Cartilage; 2008; 1836741541 | 964 | 217 | 747 | 63.3 | (57%) | No | No | Yes | Yes | No | Yes | No | No | No | Cross-sectional | 8 |
| Petterson SC; Medicine & Science in Sports & Exercise; 2008; 18379202162 | 123 | 123 | 0 | 64.9(8.5) | 67 | No | No | No | No | No | No | No | No | No | Case control | 11 |
| Bolbos RI; Osteoarthritis & Cartilage; 2008; 18387828163 | 32 | 16 | 16 | Cases: 47.2(11.54), (Range: 29–72); Controls: 36.3(10.54), (Range: 27–56) | 14 | Yes | Yes | No | Yes | No | Yes | No | No | No | Case control | 7 |
| Quaia E; Skeletal Radiology; 2008; 18404267164 | 35 | 35 | 0 | 42(17), (Range: 22–67) | 14 | No | Yes | No | Yes | No | No | No | No | No | Other | 6 |
| Folkesson J; Magnetic Resonance in Medicine; 2008; 1850684542 | 245 | 143 | KL0: 48(Range: 21–78); KL1: 62(Range: 37–81); KL2: 67(Range: 47–78); KL3&4: 68(Range: 58–78) | No | No | No | Yes | No | No | No | No | No | Other | 12 | ||
| Mills PM; Osteoarthritis & Cartilage; 2008; 18515157165 | 49 | 25 | 24 | APMM: 46.8(5.3); Controls: 43.6(6.6) | 18(36.7%) | Yes | No | Yes | Yes | No | No | No | No | No | Case control | 12 |
| Dore D; Osteoarthritis & Cartilage; 2008; 18515160166 | 50 | 50 | 64.5(7.1) | 23 | Yes | No | Yes | Yes | No | Yes | No | No | No | Cross-sectional | 9 | |
| Mutimer J; Journal of Hand Surgery; 2008; 18562375167 | 20 | 20 | 0 | 47 (Range: 26–69) | 9 | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 6 |
| Amin S; Journal of Rheumatology; 2008; 18597397168 | 192 | 192 | 69(9) | 0. | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 10 | |
| Li X; Journal of Magnetic Resonance Imaging; 2008; 18666183169 | 38 | 13 | 25 | Healthy: 28.5 (Range: 20–34); Knee OA or injury: 37.4 (Range: 20–66) | 10 | Yes | No | No | Yes | No | No | Yes | No | No | Other | 7 |
| Pelletier JP; Osteoarthritis & Cartilage; 2008; 1867238625 | 27 | 1 | 64.1(9.6) | 14 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Other | 9 | |
| Stahl R; European Radiology; 2009; 18709373170 | 37 | 17 | 20 | Mild OA: 54(9.98); Healthy control: 33.6(9.44) | 19 | No | Yes | Yes | Yes | No | No | No | No | No | Case control | 10 |
| Brem MH; Acta Radiologica; 2008; 18720084171 | 23 | 23 | 0 | 55.5(10.3) | 8 | No | No | Yes | No | No | No | Yes | No | No | Other | 6 |
| Lancianese SL; Bone; 2008; 18755303172 | 4 | 80(14) | 3 | No | No | No | No | No | Yes | No | No | No | Cross-sectional | 5 | ||
| Englund M; New England Journal of Medicine; 2008; 1878410026 | 991 | 171 | 62.3(8.6), (Range: 50.1–90.5) | 565(57%) | No | No | Yes | No | No | No | No | Yes | No | Cross-sectional | 10 | |
| Mamisch TC; Magnetic Resonance in Medicine; 2008; 18816842173 | 26 | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 7 | ||||
| Rauscher I; Radiology; 2008; 18936315174 | 60 | 37 | 23 | Healthy controls: 34.1(10); Mild OA: 52.5(10); Severe OA: 61.6(11.6) | 32 | No | Yes | No | Yes | No | No | No | Yes | No | Case control | 9 |
| Li W; Journal of Magnetic Resonance Imaging; 2009; 19161210175 | 31 | 17 | 14 | OA patients: 61.8(Range: 40–86); Healthy controls: 29.2(Range: 18–40) | 21 | No | Yes | No | Yes | No | No | No | No | No | Case control | 7 |
| Choi JW; Journal of Computer Assisted Tomography; 2009; 19188805176 | 36 | 39.7(Range: 8–69) | 21 | No | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Retrospective |
7 | ||
| Chen YH; Journal of Computer Assisted Tomography; 2008; 19204464177 | 96 | 25 | 71 | OA patients: 56; Non-OA: 46 | No | No | Yes | Yes | No | No | No | Yes | No | Case control | 8 |
The analysis included data from 142 manuscripts. The mean Downs criteria score for these manuscripts was 8.3 (range 3–17). What follows below are important excerpts from this data pertaining to different aspects of concurrent validity. The data is further summarized in Table II to discretely identify the associations examined and those where a significant association was found.
Table II.
Summary of Concurrent Validity of MRI in OA
| Outcome of interest | Number of studies examining this outcome | Number of studies finding significant associations (P < .05) |
|---|---|---|
| Symptoms | 21 studies | 13 of 21 (62%) |
| Radiographic features | 43 studies | 39 of 43 (90%) |
| Radiographic joint space | 9 studies | 9 of 9 (100%) |
| Alignment | 10 studies | 9 of 10 (90%) |
| CT | 4 studies | 4 of 4 (100%) |
| Histology/Pathology | 5 studies | 3 of 5 (60%) |
| Arthroscopy | 7 studies | 5 of 7 (71%) |
Relation to symptoms
21 studies examined the concurrent relation of MRI findings in OA to symptoms. Of these, 62% demonstrated a statistically significant association, defined as P < 0.05. Bone marrow lesions were found in 272 of 351 (77.5%) persons with painful knees compared with 15 of 50 (30%) persons with no knee pain (P < 0.001). Large lesions were present almost exclusively in persons with knee pain (35.9% vs 2%; P < 0.001). After adjustment for severity of radiographic disease, effusion, age, and sex, lesions and large lesions remained associated with the occurrence of knee pain [odds ratio, 3.31 (95% confidence interval (CI), 1.54–7.41)]. Using the same analytical approach, large lesions were also strongly associated with the presence of pain [odds ratio, 5.78 (CI, 1.04–111.11)]. Among persons with knee pain, bone marrow lesions were not associated with pain severity14.
After adjusting for the severity of radiographic OA, there was a difference between those with and without knee pain in prevalence of moderate or larger effusions (P < 0.001) and synovial thickening, independent of effusion (P < 0.001). Among those with small (grade 1) or no knee (grade 0) effusion, those with knee pain had a prevalence of synovial thickening of 73.6% compared to 21.4% of those without knee pain (P < 0.001). There was a significant difference in visual analogue scale (VAS) pain scores in those with synovial thickening compared to those without synovial thickening, after adjustment for radiographic severity, size of effusion, age, sex, and BMI. The mean pain score in those with synovial thickening after adjustment for radiographic severity and size of effusion was 47.2 mm [standard error (SE) 6.0], compared to 28.2 mm (SE 2.8) in those without synovial thickening (P = 0.006)15.
A medial or lateral meniscal tear was a very common finding in the asymptomatic subjects (prevalence, 76%) but was more common in the patients with symptomatic osteoarthritis (91%) (P < 0.005). There was no significant difference with regard to the pain or WOMAC score between the patients with and those without a medial or lateral meniscal tear in the osteoarthritic group (P = 0.8 to 0.9 for all comparisons)16.
Significant differences between WOMAC scores were found for the grades of cartilage lesions (P < 0.05) but not bone marrow edema pattern, and ligamentous and meniscal lesions17.
Bone marrow lesions >1 cm were more frequent (OR = 5.0; 95% CI = 1.4, 10.5) in the painful knee OA group than all other groups. While the frequency of BME lesions was similar in the painless OA and painful OA groups, there were more lesions, >1 cm, in the painful OA group. Full-thickness cartilage defects occurred frequently in painful OA. Women with radiographic OA, full-thickness articular cartilage defects, and adjacent subchondral cortical bone defects were significantly more likely to have painful knee OA than other groups (OR = 3.2; 95% CI = 1.3, 7.6)18.
Peripatellar lesions (prepatellar or superficial infrapatellar) were present in 12.1% of the patients with knee pain and ROA, in 20.5% of the patients with ROA and no knee pain, and in 0% of subjects with neither ROA nor knee pain (P = 0.116). However, other periarticular lesions (including bursitis and iliotibial band syndrome) were present in 14.9% of patients with both ROA and knee pain, in only 3.9% of patients with ROA but no knee pain, and in 0% of the group with no knee pain and no ROA (P = 0.004)19.
More severe symptoms relating to knee OA (pain, stiffness, and function) are weakly inversely related to tibial cartilage volume. Patients with lower cartilage volume had more severe symptoms of knee OA than those with higher cartilage volume20.
The increase in median pain from median quantile regression, adjusting for age and BMI, was significant for bone attrition (1.91, 95% CI 0.68, 3.13), bone marrow lesions (3.72, 95% CI 1.76, 5.68), meniscal tears (1.99, 95% CI 0.60, 3.38), and grade 2 or 3 synovitis/effusion vs grade 0 (9.82, 95% CI 0.38, 19.27). The relationship with pain severity was of borderline significance for osteophytes and cartilage morphology and was not significant for bone cysts or meniscal subluxation. When compared to the pain severity in knees with high scores for both bone attrition and bone marrow lesions (median pain severity 40 mm), knees with high attrition alone (30 mm) were not significantly different, but knees with high bone marrow lesion without high attrition scores (15 mm) were significantly less painful21.
A large joint effusion was associated with pain (OR, 9.99; 99% CI: 1.28, 149) and stiffness (OR, 4.67; 99% CI: 1.26, 26.1). The presence of an osteophyte in the patellofemoral compartment (OR, 2.25; 99% CI: 1.06, 4.77) was associated with pain. All other imaging findings, including focal or diffuse cartilaginous abnormalities, subchondral cysts, bone marrow edema, subluxation of the meniscus, meniscal tears, or Baker cysts, were not associated with symptoms22.
Maximal bone marrow lesion (BML) size on the Boston Leeds Osteoarthritis Score (BLOKS) scale had a positive linear relation with VAS pain (P for linear trend = 0.04)23.
No correlation of baseline synovitis with baseline pain score (r = 0.09, P = 0.17)24.
No relation between baseline synovitis score and VAS pain score (r = 0.11, P = 0.60)25.
In the group of persons with radiographic evidence of osteoarthritis (Kellgren–Lawrence grade 2 or higher), the prevalence of a meniscal tear was 63% among those with knee pain, aching, or stiffness on most days and 60% among those without these symptoms (P = 0.75); the corresponding prevalences in the group without radiographic evidence of osteoarthritis were 32% and 23% (P = 0.02). The majority of the meniscal tears – 180 of 297 (61%) were in subjects who had not had any pain, aching, or stiffness in the previous month26.
Relation to radiographic features
43 studies examined the concurrent relation of MRI findings in OA to radiographic features. Of these, 90% demonstrated a statistically significant association, defined as P < 0.05.
Relation of quantitative cartilage morphometry measures to radiographic abnormalities
Significant differences in lateral and medial femorotibial cartilage thickness were found between those with and without radiographic OA. Significant cartilage thinning could be detected by MRI in patients with OA, even when the joint space was normal radiographically27.
For every increase in grade of lateral tibiofemoral osteophytes the lateral tibial cartilage volume was significantly reduced by 255 mm3, after adjustment. There was a reduction of 77 mm3 in medial tibial cartilage volume for every increase in grade of medial tibiofemoral osteophytes, but this finding was only of borderline statistical significance28.
Cartilage volume and thickness were less in patients with OA compared to normal controls (P < 0.1)29.
Kellgren and Lawrence (KLG)2 participants displayed, on average, thicker cartilage than healthy controls in the medial femorotibial compartment [particularly anterior subregion of the medial tibia (MT) and peripheral (external, internal) subregions of the medial femur], and in the lateral femur. KLG3 participants displayed significantly thinner cartilage than KLG0 participants in the medial weight-bearing femur (central subregion), in the external subregion of the MT, and in the internal subregion of the lateral tibia30.
Mean cartilage signal intensity provided a clear separation of healthy from KLG1 (P = 0.0009). Quantification of cartilage homogeneity by entropy was able to clearly 11 separate healthy from OA subjects (P = 0.0003). Furthermo121re, entropy was also able to separate healthy from KL 1 subjects (P = 0.0004)31.
Relation of other MRI measures to radiographic abnormalities
Significant difference (P = 0.002) in the average T(1rho) within patellar and femoral cartilage between controls (45.04 ± 2.59 ms) and osteoarthritis patients (53.06 ± 4.60 ms). A significant correlation was found between T(1rho) and T(2); however, the difference of T(2) was not statistically significant between controls and osteoarthritis patients31.
Trend toward a lower dGEMRIC index with increasing KLG; the spared compartments of knees with a KLG grade 2 had a higher dGEMRIC index than those of knees with a KLG grade 4 (mean 425 msec vs 371 msec; P < 0.05)32.
All cases demonstrating decreased T1 values on dGEMRIC, showed abnormal arthroscopic or direct viewing findings. The diagnosis of damage in articular cartilage was possible in all 16 cases with radiographic KLG 1 on dGEMRIC, while the intensity changes were not found in 10 of 16 cases on Proton density Weighted Image (PDWI)33.
No differences of T2 values were found across the stages of OA (P = 0.25), but the factor of BMI did have a significant effect P < 0.0001) on T2 value34.
Average T(1rho) and T(2) values were significantly increased in OA patients compared with controls [52.04 ± 2.97 ms vs 45.53 ± 3.28 ms with P = 0.0002 for T(1rho), and 39.63 ± 2.69 ms vs 34.74 ± 2.48 ms with P = 0.001 for T(2)]. Increased T(1rho) and T(2) values were correlated with increased severity in radiographic and MR grading of OA. T(1rho) has a larger range and higher effect size than T(2), 3.7 vs 3.035.
Statistically significant correlation between radiography and MR cartilage loss in the medial (r 0.7142, P .0001) and lateral compartments (r = 0.4004, P .0136). Significant correlations also found between radiographic assessment of sclerosis and osteophytes and those found on MRI36.
Patients in whom plain radiographs, MRI, and arthroscopy were compared, the plain radiographs and MRI significantly underestimated the extent of cartilage abnormalities37.
Presence of synovial thickening was more likely with increasing KLG, from 24.0% in those with KLG 0–78.3% in those with LG 3/4 (P < 0.001)15.
Higher KLG was correlated with a higher frequency of meniscal tears (r = 0.26, P < 0.001)16.
KLG correlated significantly (P < 0.05) with the grade of cartilage lesions, and a substantially higher percentage of bone marrow and meniscal lesions with higher KLG found on MR images17.
Women with osteoarthritis had larger medial and lateral tibial plateau bone area [mean (SD): 1850 (240) mm2 and 1279 (220) mm2, respectively] than healthy women [1670 (200) mm2 and 1050 (130) mm2] (P < 0.001 for both differences). For each increase in grade of osteophyte, an increase in bone area was seen of 146 mm2 in the medial compartment and 102 mm2 in the lateral compartment38.
Statistically significant correlations were observed between the medial tibial spur classification on X-ray, the medial meniscal displacement rate on MRI and the medial meniscal signal change classification on MRI39.
Meniscal damage was mostly present in knees with OA and demonstrates a relation to KLG40.
Bone attrition of the tibiofemoral joint, scored >1, was found in 228 MRIs (23.6%) and in 55 radiographs (5.7%). Moderate to strong correlation between MRIs and radiographs for bone attrition of the tibiofemoral joint (r = 0.50, P < 0.001)41.
Surface curvature of articular cartilage for both the fine- and coarse-scale estimates were significantly higher in the OA population compared with the healthy population, with P < 0.001 and P < 0.001, respectively42.
The prevalence of meniscal damage was significantly higher among subjects with radiographic evidence of tibiofemoral osteoarthritis (KLG 2 or higher) than among those without such evidence (82% vs 25%, P < 0.001), and the prevalence increased with a higher KLG (P < 0.001 for trend). Among persons with radiographic evidence of severe osteoarthritis (KLG 3 or 4 in their right knee), 95% had meniscal damage26.
Relation to radiographic joint space width
Nine studies examined the concurrent relation of MRI findings in OA to radiographic joint space. Of these, 100% demonstrated a statistically significant association, defined as P < 0.05.
Strong correlation between the degree of medial meniscal subluxation and the severity of medial joint space narrowing (JSN) (r = 0.56, P = 0.0001)43.
Meniscal extrusion identified in all 32 patients with JSN (KLG 1–4). Definite thinning or loss of articular cartilage was identified in only 15 of the 32 cases. In 17 patients with radiographic JSN (KLG 1–3) and meniscal extrusion, no loss of articular cartilage was observed. A statistically significant correlation (P < 0.001) was observed between KLG and degree of meniscal extrusion and cartilage thinning on MRI44.
For each increase in grade of JSN, tibial plateau bone area increased by 160 mm2 in the medial compartment and 131 mm2 in the lateral compartment (significance of regression coefficients all P < 0.001)38.
Persons with symptomatic knee OA with ACL rupture had more severe radiologic OA (P < 0.0001) and were more likely to have medial JSN (P < 0.0001) than a control sample45.
Compartments of the knee joint without JSN had a higher dGEMRIC index than those with any level of narrowing (mean 408 msec vs 365 msec; P = 0.001). In knees with 1 unnarrowed (spared) and 1 narrowed (diseased) compartment, the dGEM-RIC index was greater in the spared vs the diseased compartment (mean 395 msec vs 369 msec; P = 0.001)32.
Grade of JSN as measured on skyline and lateral patellofemoral radiographs was inversely associated with patella cartilage volume. After adjusting for age, gender and body mass index, for every increase in grade of skyline JSN (0–3), the patella cartilage volume was reduced by 411 mm3. For every increase in lateral patellofemoral JSN grade (0–3), the adjusted patella cartilage volume was reduced by 125 mm3. The relationship was stronger for patella cartilage volume and skyline JSN (r = −0.54, P < 0.001) than for lateral patellofemoral JSN (r = −0.16, P = 0.015)46.
Grade one medial JSN was associated with substantial reductions in cartilage volume at both the medial and lateral tibial and patellar sites within the knee (adjusted mean difference 11–13%, all P < 0.001)47.
Cartilage volume in the medial compartment and the narrowest JSW obtained by radiography at baseline in 31 knee OA patients, revealed that some level of correlation exists between these two measurements (r = 0.46, P < 0.007)48.
Knee cartilage defects are inconsistently associated with JSN after adjustment for osteophytes but consistently with knee cartilage volume (beta: −0.27 to −0.70/ml; OR: 0.16–0.56/ml, all P < 0.01 except for OR at lateral tibial cartilage site P = 0.06)49.
Moderate, but statistically significant, correlation between JSW and femoral and tibial cartilage volumes in the medial tibiofemoral joint, which was strengthened by adjusting for medial tibial bone size (R = 0.58–0.66, P = 0.001)50.
JSN seen on both medial and lateral radiographs of the tibiofemoral joint was inversely associated with the respective tibial cartilage volume. This inverse relationship was strengthened with adjustment for age, sex, body mass index (BMI), and bone size. After adjustment for these confounders, for every increase in JSN grade (0–3), the medial tibial cartilage volume was reduced by 257 mm3 (95% CI 193–321) and the lateral tibial cartilage volume by 396 mm3 (95% CI 283–509). The relationship between mean cartilage volume and radiologic grade of JSN was linear28.
Relation to alignment
10 studies examined the concurrent relation of MRI findings in OA to alignment. Of these, 90% demonstrated a statistically significant association, defined as P < 0.05.
Valgus-aligned knees tended to have lower dGEMRIC values laterally, and varus-aligned knees tended to have lower dGEMRIC values medially; as a continuous variable, alignment correlated with the lateral: medial dGEMRIC ratio (Pearson’s R = 0.43, P = 0.02)32.
Limbs with varus alignment, especially if marked (≥7 degrees), had a remarkably high prevalence of medial lesions compared with limbs that were neutral or valgus (74.3% vs 16.4%; P < 0.001 for relation between alignment and medial lesions). Conversely, limbs that were neutral or valgus had a much higher prevalence of lateral lesions than limbs that were in the most varus group (29.5% vs 8.6%; P = 0.002 for alignment and lateral lesions)51.
Medial tibial and femoral cartilage volumes increased as the angle decreased (i.e., was less varus). Similarly, in the lateral compartment there was an inverse association at baseline between tibial and femoral cartilage volumes and the measured knee angle52.
The main univariate determinants of varus alignment in decreasing order of influence were medial bone attrition, medial meniscal degeneration, medial meniscal subluxation, and medial tibiofemoral cartilage loss. Multivariable analysis revealed that medial bone attrition and medial tibiofemoral cartilage loss explained more of the variance in varus malalignment than other variables. The main univariate determinants of valgus malalignment in decreasing order of influence were lateral tibiofemoral cartilage loss, lateral osteophyte score, and lateral meniscal degeneration53.
Correlation between medial meniscal displacement rate on MRI and the femorotibial angle (r = 0.398)39.
Worsening in the status of each medial lesion cartilage morphology, subarticular bone marrow lesions, meniscal tear, meniscal subluxation, and bone attrition was associated with greater varus malalignment54.
For every one degree increase in a valgus direction, there was an associated reduced risk of the presence of cartilage defects in the medial compartment of subjects with knee OA (P = 0.02). Moreover, for every one degree increase in a valgus direction, there was an associated increased risk of the presence of lateral cartilage defects in the OA group (P = 0.006)55.
Relation to CT
Four studies examined the concurrent relation of MRI findings in OA to CT. Of these, 100% demonstrated a statistically significant association, defined as P < 0.05. MR frequently showed tricompartmental cartilage loss when radiography and CT showed only bicompartmental involvement in the medial and patellofemoral compartments. In the lateral compartment, MR showed a higher prevalence of cartilage loss (60%) than radiography (35%) and CT (25%) did. In the medial compartment, CT and MR showed osteophytes in 100% of the knees, whereas radiography showed osteophytes in only 60%. Notably, radiography often failed to show osteophytes in the posterior medial femoral condyle. On MR images, meniscal degeneration or tears were found in all 20 knees studied. Partial and complete tears of the anterior cruciate ligament were found in three and seven patients, respectively. MR is more sensitive than radiography and CT for assessing the extent and severity of osteoarthritic changes and frequently shows tricompartmental disease in patients in whom radiography and CT show only bicompartmental involvement. MR imaging is unique for evaluating meniscal and ligamentous disease related to osteoarthritis36.
Strong linear relationship (r = 0.998) between MRI imaging and CT arthrography. The mean absolute volume deviation between magnetic resonance imaging and computed tomography arthrography was 3.3%56.
Relation to histology/pathology
Five studies examined the concurrent relation of MRI findings in OA to histology/pathology. Of these, 60% demonstrated a statistically significant association, defined as P < 0.05. Observed measurements of MRI volume of articular cartilage correlated with actual weight and volume displacement measurements with an accuracy of 82%–99% and linear correlation coefficients of 0.99 (P = 2.5e-15) and 0.99 (P = 4.4e-15)57.
The signal behavior of hyaline articular cartilage does not reflect the laminar histologic structure. Osteoarthrosis and cartilage degeneration are visible on MR images as intra-cartilaginous signal changes, superficial erosions, diffuse cartilage thinning, and cartilage ulceration58.
Comparison of data on cartilage thickness measurements with MRI with corresponding histological sections in the middle of each sector revealed a very good magnetic resonance/anatomic correlation (r = 0.88)59.
Correlation between MRI Noyes grading scores and Mankin grading scores of natural lesions was moderately high (r = 0.7) and statistically significant (P = 0.001)60.
Relation to arthroscopy
Seven studies examined the concurrent relation of MRI findings in OA to arthroscopy. Of these, 71% demonstrated a statistically significant association, defined as P < 0.05.
Moderate correlation between imaged cartilage scores and the arthroscopy scores (Pearson correlation coefficient = 0.40)37.
Spearman rank linear correlation between arthroscopic and MR cartilage grading was highly significant (P < 0.002) for each of the six articular regions evaluated. The MR and arthroscopic grades were the same in 93 (68%) of 137 joint surfaces, they were the same or differed by one grade in 123 surfaces (90%), and they were the same or differed by one or two grades in 129 surfaces (94%)61.
The overall sensitivity and specificity of MR in detecting chondral abnormalities were 60.5% (158/261) and 93.7% (89/95) respectively. MR imaging was more sensitive to the higher grade lesions: 31.8% (34/107) in grade 1; 72.4% (71/98) in grade 2; 93.5% (43/46) in grade 3; and 100% (10/10) in grade 4. The MR and arthroscopic grades were the same in 46.9% (167/356), and differed by no more than 1 grade in 90.2% (321/356) and 2 grades in 99.2% (353/356). The correlation between arthroscopic and MR grading scores was highly significant with a correlation coefficient of 0.705 (P < 0.0001)62.
Statistically significant correlation between the SFA-arthroscopic score and the SFA-MR score (r = 0.83) and between the SFA-arthroscopic grade and the SFA-MR grade (weighted kappa = 0.84). The deepest cartilage lesions graded with arthroscopy and MR imaging showed correlation in the medial femoral condyle (weighted kappa = 0.83) and in the medial tibial plateau (weighted kappa = 0.84)63.
Magnetic resonance imaging was in agreement with arthroscopy in 81% showing more degeneration but less tears of menisci than arthroscopy. Using a global system for grading the total damage of the knee joint into none, mild, moderate, or severe changes, agreement between arthroscopy and MRI was found in 82%64.
Predictive validity (Table III)
Table III.
Summary table of studies reporting data on predictive validity of MRI in knee OA
| Reference: Author, Journal, Year, PMID | Whole sample size | No. of cases | No. of controls | Age, yrs, Mean(SD), Range | No. (%)of females | Quantitative cartilage | Compositional techniques | Semi-quantitative | Cartilage | Synovium | Bone | Bone marrow lesions | Meniscus | Ligament | Study design | Score of methodological quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boegard TL; Osteoarthritis & Cartilage; 2001; 11467896178 | 47 | Women: Median = 50, (Range: 42–57); Men: Median = 50, (Range: 41–57) | 25(53.2%) | No | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective | 9 | ||
| Wluka AE; Arthritis & Rheumatism; 2002; 12209510179 | 123 | 123 | 0 | 63.1(10.6) | 71 | Yes | No | No | Yes | No | Yes | No | No | No | Longitudinal Prospective | 14 |
| Cicuttini FM; Journal of Rheumatology; 2002; 12233892180 | 21 | 8 | 13 | Case: 41.3(13.2); Controls: 49.2(17.8) | 14(66.7%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Retrospective | 13 |
| Biswal S; Arthritis & Rheumatism; 2002; 1242822876 | 43 | 4 | 39 | 54.4(Range: 17–65) | 21 | No | No | Yes | Yes | No | No | Yes | Yes | Yes | Longitudinal Retrospective | 8 |
| Cicuttini F; Journal of Rheumatology; 2002; 12465162181 | 110 | 110 | 0 | 63.2(10.2) | 66 | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 12 |
| Pessis E; Osteoarthritis & Cartilage; 2003; 12744942182 | 20 | 20 | 63.9(9) | 13 | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Longitudinal Prospective | 12 | |
| Felson DT; Annals of Internal Medicine; 2003; 1296594151 | 256 | 156 | 0 | Followed: 66.2(9.4); Not followed: 67.8(9.6) | (38.3%) | No | No | Yes | No | No | No | Yes | No | No | Longitudinal Prospective | 11 |
| Cicuttini FM; Arthritis & Rheumatism; 2004; 1473060477 | 117 | 117 | 63.7(10.2) | (58.1%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 9 | |
| Wluka AE; Annals of the Rheumatic Diseases; 2004; 1496296020 | 132 | 132 | 0 | 63.1(Range: 41–86) | 71(54%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 10 |
| Cicuttini F; Rheumatology; 2004; 1496320152 | 117 | 117 | 0 | 67(10.6) | (58%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 12 |
| Cicuttini FM; Ann Rheum Dis; 2004; 1511571465 | 123 | 123 | 0 | Joint replacement: 64.1(9.3); No joint replacement: 63.1(10.3) | 65(52.8%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 11 |
| Dashti M; Scandinavian Journal of Rheumatology; 2004; 15163109118 | 174 | 117 | 57 | 61.6(9.5) | 123(70.7%) Yes | No | No | Yes | No | No | No | No | No | Case control | 11 | |
| Cicuttini FM; Journal of Rheumatology; 2004; 15229959183 | 102 | 102 | 0 | 63.8(10.1) | (63%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 10 |
| Berthiaume MJ; Annals of the Rheumatic Diseases; 2005; 1537485578 | 32 | Yes | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective | 10 | ||||
| Cicuttini F; Journal of Rheumatology; 2004; 15570649126 | 123 | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 6 | ||||
| Cubukcu D; Clinical Rheumatology; 2005; 15599642184 | 40 | 40 | HA group: 52.6(7.16); Saline group: 57.6(2.77) | 24(60%) | No | No | Yes | Yes | No | Yes | No | Yes | Yes | Randomized controlled trial | 15 | |
| Ozturk C; Rheumatol Int; 2006;15703953185 | 47 | 47 | 0 | HA-only group: 58(7.7); HA&Cortico group: 58.1(10.3) | 39(97.5%) | No | No | Yes | Yes | No | No | Yes | No | No | Randomized controlled trial | 17 |
| Wang Y; Arthritis Res Ther; 2005; 15899054186 | 126 | 126 | 63.6(10.1) | 68 | No | No | No | No | No | Yes | No | No | No | Longitudinal Prospective | 12 | |
| Cicuttini F; Osteoarthritis & Cartilage; 2005; 1592263450 | 28 | 28 | 0 | 62.8(9.8) | (57%) | Yes | No | No | Yes | No | No | No | No | No | Longitudinal Prospective | 10 |
| Wluka AE; Rheumatology; 2005; 1603008466 | 126 | 126 | 0 | 63.6(10.1) | 68(54%) | Yes | No | Yes | Yes | No | Yes | No | No | No | Longitudinal Prospective | 14 |
| Garnero P; Arthritis & Rheumatism; 2005; 16145678187 | 377 | 377 | 0 | 62.5(8.1) | (76%) | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 11 |
| Wang Y; Rheumatology; 2006; 1618894779 | 124 | 124 | 0 | Females: 57.1(5.8); Males: 52.5(13.2) | 81(65.3%) | No | No | Yes | Yes | No | Yes | No | No | No | Longitudinal Prospective | 11 |
| Phan CM; European Radiology; 2006; 1622253368 | 40 | 34 | 6 | 57.7(15.6), (Range: 28–81) | 16 | No | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Longitudinal Prospective | 7 |
| Hayes CW; Radiology; 2005; 16251398188 | 117 | 117 | 115 | No OA, No Pain: 44.6(10.7); OA, No Pain: 16.2(0.8); No OA, Pain: 47(0.7); OA&Pain: 47.1(0.8) | (100%) | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Longitudinal Prospective | 13 |
| Wang Y; Journal of Rheumatology; 2005; 16265703189 | 40 | 0 | 40 | 52.3(13) | 0 | Yes | No | No | Yes | No | Yes | No | No | No | Longitudinal Prospective | 11 |
| Ding C; Arthritis & Rheumatism; 2005; 1632033980 | 325 | 45.2(6.5) | 190 | Yes | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 10 | ||
| Bruyere O; Annals of the Rheumatic Diseases; 2006; 16396978190 | 62 | 62 | 0 | 64.9(10.3) | 49 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Longitudinal Prospective | 10 |
| Katz JN; Osteoarthritis & Cartilage; 2006; 1641321069 | 83 | 61(11), (Range: 45–89) | 50(60%) | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Longitudinal Prospective | 9 | ||
| Raynauld JP; Arthritis Research & Therapy; 2006; 1650711972 | 110 | 110 | 0 | 62.4(7.5) | (64%) | Yes | No | Yes | Yes | No | No | Yes | Yes | No | Longitudinal Prospective | 11 |
| Hunter DJ; Arthritis & Rheumatism; 2006; 1650893081 | 257 | 257 | 0 | 66.6(9.2), (Range: 47–93) | (41.6%) | No | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective | 10 |
| Ding C; Archives of Internal Medicine; 2006; 1656760582 | 325 | Decrease defects: 45.4(6.4); Stable defects: 44.2(7.1); Increase defects: 46.1(5.9) | (58.1%) | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 14 | ||
| Brandt KD; Rheumatology; 2006; 16606655191 | 30 | 20 | 10 | 62 | 29 | No | No | No | No | Yes | No | No | No | No | Other | 10 |
| Hunter DJ; Arthritis & Rheumatism; 2006; 1664603783 | 217 | 217 | 0 | 66.4(9.4) | (44%) | No | No | Yes | Yes | No | No | Yes | No | No | Longitudinal Prospective | 10 |
| Wluka AE; Arthritis Research & Therapy; 2006; 16704746192 | 105 | 105 | 0 | All eligible: 62.5 (10.7); MRI at FU: 63.8(10.6); Lost to FU: 61.6(11.3) | 59(53%) | Yes | No | No | Yes | No | Yes | No | No | No | Longitudinal Prospective | 17 |
| Hunter DJ; Osteoarthritis & Cartilage; 2007; 16857393193 | 127 | 127 | 67(9.05) | (46.7%) | No | Yes | No | Yes | No | No | No | No | No | Cross-sectional | 12 | |
| Bruyere O; Osteoarthritis & Cartilage; 2007; 1689046173 | 62 | 62 | 0 | 64.9(10.3) | 46 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Longitudinal Prospective | 10 |
| Amin S; Annals of the Rheumatic Diseases; 2007; 17158140194 | 196 | 196 | 0 | 68(9) | 0 | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 13 |
| Nevitt MC; Arthritis & Rheumatism; 2007; 1746912674 | 80 | 39 | 0 | 73.5(3.1) | (63.6%) | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 10 |
| Hill CL; Annals of the Rheumatic Diseases; 2007; 1749109624 | 270 | 270 | 0 | 66.7(9.2) | 112 | No | No | Yes | Yes | Yes | No | No | No | No | Longitudinal Prospective | 9 |
| Pelletier JP; Arthritis Research & Therapy; 2007; 1767289171 | 110 | 110 | 0 | Q1 greatest loss global: 63.7(7.2); Q4 least loss gobal: 61.3(7.5); Q1 greatest loss_medial: 64.1 (7.4); Q1 least loss_medial: 61.6(7.8) | (68.3%) | No | No | Yes | Yes | No | No | Yes | Yes | No | Longitudinal Prospective | 15 |
| Davies-Tuck ML; Osteoarthritis & Cartilage; 2008; 17698376195 | 117 | 117 | 0 | 63.7(10.2) | 68(58%) | Yes | No | Yes | Yes | No | Yes | No | No | No | Longitudinal Prospective | 14 |
| Raynauld JP; Annals of the Rheumatic Diseases; 2008; 1772833384 | 107 | 107 | 0 | 62.4(7.5) | (64%) | Yes | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Retrospective | 15 |
| Felson DT; Arthritis & Rheumatism; 2007; 1776342770 | 330 | 110 | 220 | Cases: 62.9(8.3); Controls: 61.2(8.4) | 211(63.9%) | No | No | Yes | No | No | Yes | Yes | No | No | Case control | 12 |
| Kornaat PR; European Radiology; 2007; 17823802196 | 182 | 71 | 59(Range: 43–76) | 157(80%) | No | No | Yes | No | No | No | Yes | No | No | Longitudinal Prospective | 8 | |
| Hunter DJ; Arthritis Research & Therapy; 2007; 17958892197 | 160 | 80 | 80 | 67(9) | (46%) | No | No | Yes | Yes | No | No | No | No | No | Case control | 11 |
| Englund M; Arthritis & Rheumatism; 2007; 1805020140 | 310 | 102 | 208 | Cases: 62.9(8.3) | 211(68.1%) | No | No | Yes | No | No | No | No | Yes | No | Case control | 15 |
| Davies-Tuck ML; Osteoarthritis & Cartilage; 2008; 1809384785 | 74 | 0 | 74 | Meniscal tear: 58.8(6); No meniscal tear: 55.5(4.3) | 74(100%) | No | Yes | Yes | Yes | No | Yes | No | Yes | No | Longitudinal Prospective | 13 |
| Hernandez-Molina G; Arthritis & Rheumatism; 2008; 18163483198 | 258 | 258 | 0 | 66.6(9.2) | (42.6%) | No | No | Yes | Yes | No | No | Yes | No | Yes | Longitudinal Prospective | 11 |
| Teichtahl AJ; Osteoarthritis & Cartilage; 2009; 18194873199 | 99 | 99 | 0 | 63 (10) | (60%) | Yes | No | No | Yes | No | Yes | No | No | No | Longitudinal Prospective | 14 |
| Amin S; Osteoarthritis & Cartilage; 2008; 1820362986 | 265 | 265 | 67(9) | (43%) | No | No | Yes | Yes | No | No | No | Yes | Yes | Longitudinal Prospective | 11 | |
| Teichtahl AJ; Obesity; 2008; 18239654200 | 297 | 297 | 58(5.5) | 186 | Yes | No | Yes | Yes | No | Yes | No | No | No | Longitudinal Prospective | 14 | |
| Blumenkrantz G; Osteoarthritis & Cartilage; 2008; 18337129201 | 18 | 8 | 10 | Cases: 55.7(7.3); Controls: 57.6(6.2) | 18(100%) | No | Yes | Yes | Yes | No | No | No | No | No | Case control | 12 |
| Song IH; Annals of the Rheumatic Diseases; 2009; 18375537202 | 41 | 41 | 65(6.7) | 26 | No | No | Yes | No | No | No | No | No | Yes | Randomized controlled trial | 14 | |
| Scher C; Skeletal Radiology; 2008; 1846386567 | 65 | 65 | 0 | OA-only: 49.3 (Range: 28–75); OA&BME group: 53.5(35–82) | No | No | Yes | Yes | No | No | Yes | No | No | Longitudinal Retrospective | 10 | |
| Sharma L; Arthritis & Rheumatism; 2008; 1851277787 | 153 | 153 | 0 | 66.4(11) | Yes | No | Yes | Yes | No | No | No | Yes | No | Longitudinal Prospective | 11 | |
| Owman H; Arthritis & Rheumatism; 2008; 18512778203 | 15 | 9 | 7 | 50(Range: 35–70) | No | Yes | No | Yes | No | No | No | No | No | Longitudinal Prospective | 10 | |
| Madan-Sharma R; Skeletal Radiology; 2008; 1856681375 | 186 | 74 | 112 | 60.2(Range: 43–76) | 150 | No | No | Yes | Yes | No | No | Yes | Yes | No | Longitudinal Prospective | 11 |
| Amin S; Journal of Rheumatology; 2008; 18597397168 | 192 | 192 | 69(9) | No | No | Yes | Yes | No | No | No | No | No | Cross-sectional | 10 | ||
| Pelletier JP; Osteoarthritis & Cartilage; 2008; 1867238625 | 27 | 1 | 64.1(9.6) | 14 | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Other | 9 | |
| Amin S; Arthritis & Rheumatism; 2009; 19116936204 | 265 | 265 | 0 | 67(9) | No | No | Yes | Yes | No | No | No | No | No | Longitudinal Prospective | 16 | |
The analysis included data from 61 manuscripts of which 1 pertains to the hip and the remainder to the knee. The mean Downs criteria score for these manuscripts was 11.5 (range 6–17). What follows below are important excerpts from this data pertaining to different aspects of predictive validity. The data is further summarized in Table IV to discretely identify the associations examined and those where a significant association was found.
Table IV.
Summary of Predictive Validity of MRI in OA
| Outcome of interest | Number of studies examining this outcome | Number of studies finding significant associations (P < .05) |
|---|---|---|
| Joint replacement | 3 studies | 3 of 3 (100%) |
| Change in symptoms | 6 studies | 5 of 6 (83%) |
| Radiographic progression | 8 studies | 5 of 8 (63%) |
| MRI progression | 19 studies | 16 of 19 (84%) |
Prediction of joint replacement
Three studies examined the predictive relation of MRI findings to joint replacement. Of these, 100% demonstrated a statistically significant association, defined as P < 0.05.
One study investigated the relation of change in quantitative cartilage volume to risk of knee replacement. For every 1% increase in the rate of tibial cartilage loss there was a 20% increase risk of undergoing a knee replacement at four years (95% CI, 10%–30%). Those in the highest tertile of tibial cartilage loss had 7.1 (1.4–36.5) higher odds of undergoing a knee replacement than those in the lowest tertile. Change in bone area also predicted risk of TKR OR 12 (95% CI 1–14)65.
Higher total cartilage defect scores (8–15) were associated with a 6.0-fold increased risk of joint replacement over 4 yr compared with those with lower scores (2–7) (95% CI 1.6, 22.3), independently of potential confounders66.
A separate smaller study investigated the relation of bone marrow lesions (assessed semi-quantitatively) to need for TKR. Subjects who had a bone marrow lesion were 8.95 times as likely to progress rapidly to a TKA when compared to subjects with no BME (P = 0.016). There was no relation of TKR with meniscal tear or cartilage loss67.
Prediction of change in symptoms
Six studies examined the predictive relation of MRI findings to change in symptoms. Of these, 83% demonstrated a statistically significant association, defined as P < 0.05.
Weak associations between worsening of symptoms of OA and increased cartilage loss: pain [r(s) = 0.28, P = 0.002], stiffness [r(s) = 0.17, P = 0.07], and deterioration in function [r(s) = 0.21, P = 0.02]20.
Small study did not find a significant relation between changes in WOMAC scores with the amount of cartilage loss and the change in BME (P > 0.05)68.
Multivariate analyses of knee pain 1 year following arthroscopic partial meniscectomy demonstrated that medial tibial cartilage damage accounting for 13% of the variability in pain scores69.
The BOKS study examined the relationship between longitudinal fluctuations in synovitis with change in pain and cartilage in knee osteoarthritis. Change in summary synovitis score was correlated with the change in pain (r = 0.21, P = 0.0003). An increase of one unit in summary synovitis score resulted in a 3.15-mm increase in VAS pain score (0–100 scale). Effusion change was not associated with pain change. Of the three locations for synovitis, changes in the infrapatellar fat pad were most strongly related to pain change24.
A nested case-control study examined if enlarging BMLs are associated with new knee pain. Case knee was defined as absence of knee pain at baseline but presence of knee pain both times at follow-up. Controls were selected randomly from among knees with absence of pain at baseline. Among case knees, 54 of 110 (49.1%) showed an increase in BML score within a compartment, whereas only 59 of 220 control knees (26.8%) showed an increase (P < 0.001 by chi-square test). A BML score increase of at least 2 units was much more common in case knees than in control knees (27.5% vs 8.6%; adjusted odds ratio 3.2, 95% CI 1.5–6.8)70.
Increases in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and patient global scores over time are associated with change in cartilage volume of the medial tibial plateau and medial femoral condyle71.
Weak association of cartilage volume loss with less knee pain. Medial cartilage volume loss and simultaneous pain change at 24 months (beta coefficient −0.45, P = 0.03) and SF-36 physical components (beta coefficient 0.22, P = 0.04)72.
Prediction of radiographic progression
Eight studies examined the predictive relation of MRI findings to radiographic progression. Of these, 63% demonstrated a statistically significant association, defined as P < 0.05.
No significant association between reduction in JSW and cartilage volume (R < 0.13). Trend toward a significant association between change in medial tibiofemoral cartilage volume and joint replacement at 4 years (OR = 9.0, P = 0.07) but not change in medial tibiofemoral JSW (OR = 1.1, P = 0.92)50.
No correlation between the cartilage volume loss changes (either by using absolute or percentage values) and the JSW changes at 24 months (global cartilage volume, r = 0.11; medial compartment cartilage volume, r = 0.19)72.
Medial femorotibial JSN after 1 year, assessed by radiography, was significantly correlated with a loss of medial tibial cartilage volume (r = 0.25, P = 0.046) and medial tibial cartilage thickness (r = 0.28, P = 0.025), over the same period73.
Higher baseline composite cartilage scores and increases in composite cartilage scores during follow-up were moderately correlated with greater joint space loss (r = 0.33, P = 0.0002 and r = 0.26, P = 0.01, respectively)74.
Loss in JSW correlated with the loss of cartilage volume on the central weight-bearing area of the condyles and the plateaus as well as on the medial compartment71.
Study examined the relation of MRI features at baseline with radiographically determined JSN in the medial compartment of the knee after 2 years in a group of patients with symptomatic osteoarthritis. A significant association was observed for meniscal tears (RR 3.57; CI 1.08–10.0) and meniscal subluxation (RR 2.73; CI 1.20–5.41), between KL < 2 and meniscal subluxation (RR 11.3; CI 2.49–29.49) and KL ≥ 2 and meniscus tears (RR 8.91; CI 1.13–22.84) and radiographic JSN 2 years later75.
Prediction of MRI progression
Nineteen studies examined the predictive relation of MRI findings to MRI progression. Of these, 84% demonstrated a statistically significant association, defined as P < 0.05.
Patients who had sustained meniscal tears showed a higher average rate of progression of cartilage loss (22%) than that seen in those who had intact menisci (14.9%) (P ≤ 0.018). Anterior cruciate ligament (ACL) tears had a borderline significant influence P ≤ 0.06) on the progression of cartilage pathology. Lesions located in the central region of the medial compartment were more likely to progress to more advanced cartilage pathology (progression rate 28%; P ≤ 0.003) than lesions in the anterior (19%; P ≤ 0.564) and posterior (17%; P ≤ 0.957) regions or lesions located in the lateral compartment (average progression rate 15%; P ≤ 0.707). Lesions located in the anterior region of the lateral compartment showed less progression of cartilage degradation (6%; P ≤ 0.001). No specific grade of lesion identified at baseline had a predilection for more rapid cartilage loss (P ≤ 0.93)76.
There was a significant correlation between the degree of loss of tibial cartilage and the degree of loss of femoral cartilage, in both tibiofemoral joints (r = 0.81, P < 0.001 at the medial tibiofemoral joint; r = 0.71, P < 0.001 at the lateral tibiofemoral joint)77.
A highly significant difference in global cartilage volume loss was observed between severe medial meniscal tear and absence of tear [mean (SD), −10.1 (2.1)% v −5.1 (2.4)%, P = 0.002]. An even greater difference was found between the medial meniscal changes and medial compartment cartilage volume loss [−14.3 (3.0)% in the presence of severe tear v −6.3 (2.7)% in the absence of tear; P < 0.0001]. Similarly, a major difference was found between the presence of a medial meniscal extrusion and loss of medial compartment cartilage volume [−15.4 (4.1)% in the presence of extrusion v −4.5 (1.7)% with no extrusion; P < 0.001]78.
Annual patellar cartilage loss was highest in those with defects compared with no defects (5.5% vs 3.2%, P = 0.01). Tibial cartilage loss was not associated with defects in the medial (4.6% vs 5.8%, P = 0.42) or lateral (4.7% vs 6.5%, P = 0.21) tibial cartilages66.
Baseline cartilage defect score was negatively associated with the progression of cartilage defects in each compartment (all P < 0.001)79.
Baseline cartilage defect scores at the medial tibia, lateral tibia, and patella had a dose-response association with the annual rate of change in knee cartilage volume at the corresponding site (beta = −1.3% to −1.2% per grade; P < 0.05 for all comparisons). In addition, an increase in knee cartilage defect score (change of more than or equal to 1) was associated with higher rates of knee cartilage volume loss at all sites (beta = −1.9% to −1.7% per year; P < 0.01 for all comparisons). Furthermore, a decrease in the knee cartilage defect score (change of less than or equal to −1) was associated with an increase in knee cartilage volume at all sites (beta = 1.0%–2.7% per year; P < 0.05 for all comparisons)80.
Predictors of fast progression included the presence of severe meniscal extrusion (P = 0.001), severe medial tear (P = 0.005), medial and/or lateral bone edema (P = 0.03), high body mass index (P < 0.05, fast vs slow), weight (P < 0.05, fast vs slow) and age (P < 0.05 fast vs slow)72.
In the medial tibiofemoral joint, each measure of meniscal malposition was associated with an increased risk of cartilage loss. There was also a strong association between meniscal damage and cartilage loss81.
A worsening in cartilage defect score was significantly associated with tibiofemoral osteophytes (OR, 6.22 and 6.04 per grade), tibial bone area (OR, 1.24 and 2.07 per square centimeter), and cartilage volume (OR, 2.91 and 1.71 per ml in the medial tibiofemoral and patellar compartments)82.
Knee compartments with a higher baseline BML score had greater cartilage loss. An increase in BMLs was strongly associated with further worsening of the cartilage score83.
Despite cartilage loss occurring in over 50% of knees, synovitis was not associated with cartilage loss in either tibiofemoral or patellofemoral compartment24.
Significant correlations were seen between the loss of cartilage volume and edema size change in the medial condyle (−0.40, P = 0.0001) and the medial tibial plateau (−0.23, P = 0.03), and the changes in cyst size in the medial condyle (−0.29, P = 0.01). A multivariate analysis showed that the edema size change was strongly and independently associated with medial cartilage volume loss (−0.31, P = 0.0004)84.
Medial meniscal tear was associated with 103 mm(2) greater tibial plateau bone area within the medial (95% CI 6.2, 200.3; P = 0.04) and a lateral meniscal tear with a 120 mm(2) greater area within the lateral compartment (95% CI 45.5, 195.2; P = 0.002)85.
Adjusting for age, body mass index, gender and baseline cartilage scores, complete ACL tear increased the risk for cartilage loss at the medial tibiofemoral compartment (OR: 1.8, 95% CI: 1.1, 3.2). However, following adjustment for the presence of medial meniscal tears, no increased risk for cartilage loss was further seen (OR: 1.1, 95% CI: 0.6, 1.8)86.
Medial meniscal damage predicted medial tibial cartilage volume loss and tibial and femoral denuded bone increase, while varus malalignment predicted medial tibial cartilage volume and thickness loss and tibial and femoral denuded bone increase. Lateral meniscal damage predicted every lateral outcome87.
A positive correlation was found between the global severity of synovitis at baseline and the loss of cartilage volume at 60 days (P < 0.03)25.
Discussion
The performance of MRI as an outcome measure in OA has been extensively studied providing strong support for both its concurrent and predictive validity.
As outlined in this review numerous studies have examined the relation of MRI to related constructs such as symptom measures, plain radiography, histology and arthroscopy. These studies demonstrate the following:
Inconsistent relation of structural features to symptoms with 13 of 21 studies finding a significant relation. Generally strong relation of large bone marrow lesions, moderate relation of synovitis and effusion and weak relation of cartilage volume/thickness to presence of pain. No relation of meniscal tears to presence of pain.
In general there was an inconsistent relation of cartilage volume and thickness and compositional measures to presence of radiographic OA. Higher frequency of meniscal tears, synovitis, increased bone area, increased bone attrition/curvature in persons with radiographic OA. Radiographic change insensitive to early changes found on MRI. 39 of 43 studies found significant associations between MRI and radiographic features.
There was a strong relation of meniscal subluxation and increased subchondral bone area to reduced radiographic joint space. Inconsistent (but generally moderate) relation of reduced cartilage volume and thickness to reduced radiographic joint space. Nine of nine studies found significant associations between MRI and radiographic joint space.
In general there was a strong correlation of cartilage volume measures to histologic findings. Three of five studies found significant relation of MRI to histology/pathology.
Moderate to strong relation of arthroscopic findings to cartilage and meniscal findings on MRI with five of seven studies finding a significant association
Strong relation of CT arthrography to MRI cartilage volume with all four studies examining this relation finding a significant association.
An important obstacle to biomarker validation and qualification is the adequate delineation of a gold standard. Unlike other diseases where surrogate endpoints exist, OA does not have a clear gold standard clinical endpoint and further is a remarkably heterogeneous disease. Therefore, the ‘clinical endpoint’ is more difficult to establish. A number of experts in the field have advocated that joint replacement be the clinical outcome of interest but due to constraints over comorbidities, insurance status and a number of other factors that influence determining if a person receives a joint replacement, alternate suggestions have been recommended including the use of virtual TKR (vTKR)88. This is a composite endpoint that includes domains of pain, physical function and joint structure on X-rays89. At this point it remains to be validated and as a consequence the constituent literature in this review does not include this endpoint to establish the predictive validity of MRI.
This work may be susceptible to publication bias as there was no effort made to search either clinical trial registries or meeting abstracts for potential unpublished studies that might tend to invalidate the MRI biomarkers examined.
The literature on the predictive validity of MRI in OA demonstrated the following:
Quantitative cartilage volume change and presence of cartilage defects or bone marrow lesions are potential predictors of TKR. Three of three studies found a significant relation.
Inconsistent but generally weak relation of cartilage loss to symptom change. Moderate relation of BML change to incident symptoms and pain change. Weak relation of change in synovitis to change in pain. Five of six studies found significant association between MRI and change in symptoms.
At best a weak relation between change in cartilage thickness and change in joint space. Five of eight studies found a significant relation.
Presence of meniscal damage, cartilage defects and BMLs predicts MRI progression. 16 of 19 studies found a significant relation.
Some MRI biomarkers correlate with some other biomarkers. Moreover in a limited number of studies some MRI biomarkers correlate with clinical endpoints and/or predict clinical outcomes Future research should be directed toward improving the predictive validity of current structural measures as they relate to important clinical outcomes so their role as surrogate outcomes can be substantiated. In addition, studies to improve the precision of assessment of structural features more closely related to symptom change such as BMLs and synovitis are warranted.
Acknowledgments
Role of funding source
The OARSI FDA OA Initiative received financial support from the following professional organization:
American College of Rheumatology
Additionally the OARSI FDA OA Initiative received financial support from the following companies:
Amgen
ArthroLab
AstraZeneca
Bayer Healthcare
Chondrometrics
CombinatoRx
Cypress BioScience
DePuy Mitek
Expanscience 4QImaging
Genevrier/IBSA
Genzyme
King (Alpharma) Merck
Merck Serono NicOx
Pfizer
Rottapharm
Smith & Nephew Wyeth
While individuals from pharmaceutical, biotechnology and device companies actively participated in on-going working group discussions, due to the conflict of interest policy enacted by OARSI, these individuals were not allowed to vote on the final recommendations made by OARSI to the Food and Drug Administration.
We recognize the invaluable support of Valorie Thompson for administrative and editorial support and OARSI for their invaluable support of this activity. This analysis and literature review was undertaken to facilitate discussions and development of recommendations by the Assessment of Structural Change Working group for the OARSI FDA Initiative. The members of the working group were: Philip Conaghan, MB, BS, PhD (Chair), David Hunter, MBBS, PhD, Jeffrey Duryea, PhD, Garry Gold, MD, Steven Mazzuca, PhD, Jean Francis Maillefert, MD, Timothy Mosher, MD, Hollis Potter, MD, David Felson, MD, Ali Guermazi, MD, Helen Keen, MD, Gayle Lester, PhD, Wayne Tsuji, MD, John Randle, PhD, Felix Eckstein, MD, Erika Schneider, PhD, Elena Losina, PhD, Sarah Kingsbury, PhD, William Reichman, PhD, Jean Pierre Pelletier, MD, Saara Totterman, MD, PhD, Rose Maciewicz, PhD, Bernard Dardzinski, PhD, Mona Wahba, MD, Marie Pierre Hellio Le Graverand-Gastineau, MD, PhD, DSc, Elisabeth Morris, DVM, Jeffrey Kraines, MD, Lucio Rovati, MD, Don Dreher, MD, PhD, James Huckle, PhD, Mary-Ann Preston, PhD, Brooks Story, PhD.
Footnotes
Author contributions
DJH conceived and designed the study, drafted the manuscript and takes responsibility for the integrity of the work as a whole, from inception to finished article. EL and WZ were also involved in the design of the study. All authors contributed to acquisition of the data. All authors critically revised the manuscript and gave final approval of the article for submission.
The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Conflict of interest statement
David Hunter receives research or institutional support from DonJoy, NIH, and Stryker.
Other authors declared no conflict of interest
References
- 1.Kellgren JH, Lawrence JS. Atlas of standard radiographs. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 2.Guermazi A, Burstein D, Conaghan P, Eckstein F, Hellio Le Graverand-Gastineau MP, Keen H, et al. Imaging in osteoarthritis. Rheum Dis Clin North Am. 2008;34:645–87. doi: 10.1016/j.rdc.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365:965–73. doi: 10.1016/S0140-6736(05)71086-2. [Review] [100 refs] [DOI] [PubMed] [Google Scholar]
- 4.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27:1513–7. [PubMed] [Google Scholar]
- 5.Hunter DJ, Losina E, Guermazi A, Burstein D, Lassere MN, Kraus V. A pathway and approach to biomarker validation and qualification for osteoarthritis clinical trials. Curr Drug Targets. 2010;11:536–45. doi: 10.2174/138945010791011947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boers M, Brooks P, Strand CV, Tugwell P. The OMERACT filter for outcome measures in rheumatology. J Rheumatol. 1998;25:198–9. [PubMed] [Google Scholar]
- 8.Lassere M. A users guide to measurement in medicine. Osteoarthritis Cartilage. 2006;14(Suppl 1):10–4. doi: 10.1016/j.joca.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 9.Goodsaid FM, Frueh FW, Mattes W. Strategic paths for biomarker qualification. Toxicology. 2008;245:219–23. doi: 10.1016/j.tox.2007.12.023. [Review] [14 refs] [DOI] [PubMed] [Google Scholar]
- 10.Wagner JA. Overview of biomarkers and surrogate endpoints in drug development. Dis Markers. 2002;18:41–6. doi: 10.1155/2002/929274. [Review] [21 refs] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NIH-FDA Conference. Biomarkers and surrogate endpoints: advancing clinical research and applications. Abstracts Dis Markers. 1998;14:187–334. doi: 10.1155/1998/698239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lesko LJ, Atkinson AJ., Jr Use of biomarkers and surrogate endpoints in drug development and regulatory decision making: criteria, validation, strategies. Annu Rev Pharmacol Toxicol. 2001;41:347–66. doi: 10.1146/annurev.pharmtox.41.1.347. [Review] [61 refs] [DOI] [PubMed] [Google Scholar]
- 13.Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [Review] [29 refs] [DOI] [PubMed] [Google Scholar]
- 14.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–9. doi: 10.7326/0003-4819-134-7-200104030-00007. [see comments] [DOI] [PubMed] [Google Scholar]
- 15.Hill CL, Gale DG, Chaisson CE, Skinner K, Kazis L, Gale ME, et al. Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis. J Rheumatol. 2001;28:1330–7. [PubMed] [Google Scholar]
- 16.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9. doi: 10.2106/00004623-200301000-00002. [see comment] [DOI] [PubMed] [Google Scholar]
- 17.Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226:373–81. doi: 10.1148/radiol.2262012190. [DOI] [PubMed] [Google Scholar]
- 18.Sowers MF, Hayes C, Jamadar D, Capul D, Lachance L, Jannausch M, et al. Magnetic resonance-detected sub-chondral bone marrow and cartilage defect characteristics associated with pain and X-ray-defined knee osteoarthritis. Osteoarthritis Cartilage. 2003;11:387–93. doi: 10.1016/s1063-4584(03)00080-3. [DOI] [PubMed] [Google Scholar]
- 19.Hill CL, Gale DR, Chaisson CE, Skinner K, Kazis L, Gale ME, et al. Periarticular lesions detected on magnetic resonance imaging: prevalence in knees with and without symptoms. Arthritis Rheum. 2003;48:2836–44. doi: 10.1002/art.11254. [DOI] [PubMed] [Google Scholar]
- 20.Wluka AE, Wolfe R, Stuckey S, Cicuttini FM. How does tibial cartilage volume relate to symptoms in subjects with knee osteoarthritis? Ann Rheum Dis. 2004;63:264–8. doi: 10.1136/ard/2003.007666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torres L, Dunlop DD, Peterfy C, Guermazi A, Prasad P, Hayes KW, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006;14:1033–40. doi: 10.1016/j.joca.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 22.Kornaat PR, Bloem JL, Ceulemans RY, Riyazi N, Rosendaal FR, Nelissen RG, et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology. 2006;239:811–7. doi: 10.1148/radiol.2393050253. [DOI] [PubMed] [Google Scholar]
- 23.Hunter DJ, Lo GH, Gale D, Grainger AJ, Guermazi A, Conaghan PG. The reliability of a new scoring system for knee osteoarthritis MRI and the validity of bone marrow lesion assessment: BLOKS (Boston Leeds Osteoarthritis Knee Score) Ann Rheum Dis. 2008;67:206–11. doi: 10.1136/ard.2006.066183. [Review] [28 refs] [DOI] [PubMed] [Google Scholar]
- 24.Hill CL, Hunter DJ, Niu J, Clancy M, Guermazi A, Genant H, et al. Synovitis detected on magnetic resonance imaging and its relation to pain and cartilage loss in knee osteoarthritis. Ann Rheum Dis. 2007;66:1599–603. doi: 10.1136/ard.2006.067470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pelletier JP, Raynauld JP, Abram F, Haraoui B, Choquette D, Martel-Pelletier J. A new non-invasive method to assess synovitis severity in relation to symptoms and cartilage volume loss in knee osteoarthritis patients using MRI. Osteoarthritis Cartilage. 2008;16(Suppl 3):S8–13. doi: 10.1016/j.joca.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 26.Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–15. doi: 10.1056/NEJMoa0800777. [see comment] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karvonen RL, Negendank WG, Teitge RA, Reed AH, Miller PR, Fernandez-Madrid F. Factors affecting articular cartilage thickness in osteoarthritis and aging. J Rheumatol. 1994;21:1310–8. [PubMed] [Google Scholar]
- 28.Cicuttini FM, Wluka AE, Forbes A, Wolfe R, Cicuttini FM, Wluka AE, et al. Comparison of tibial cartilage volume and radiologic grade of the tibiofemoral joint. Arthritis Rheum. 2003;48:682–8. doi: 10.1002/art.10840. [DOI] [PubMed] [Google Scholar]
- 29.Lindsey CT, Narasimhan A, Adolfo JM, Jin H, Steinbach LS, Link T, et al. Magnetic resonance evaluation of the interrelationship between articular cartilage and trabecular bone of the osteoarthritic knee. Osteoarthritis Cartilage. 2004;12:86–96. doi: 10.1016/j.joca.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 30.Hellio Le Graverand MP, Buck RJ, Wyman BT, Vignon E, Mazzuca SA, Brandt KD, et al. Subregional femorotibial cartilage morphology in women–comparison between healthy controls and participants with different grades of radiographic knee osteoarthritis. Osteoarthritis Cartilage. 2009;17:1177–85. doi: 10.1016/j.joca.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Dam EB, Folkesson J, Pettersen PC, Christiansen C. Automatic morphometric cartilage quantification in the medial tibial plateau from MRI for osteoarthritis grading. Osteoarthritis Cartilage. 2007;15:808–18. doi: 10.1016/j.joca.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 32.Williams A, Sharma L, McKenzie CA, Prasad PV, Burstein D. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage in knee osteoarthritis: findings at different radiographic stages of disease and relationship to malalignment. Arthritis Rheum. 2005;52:3528–35. doi: 10.1002/art.21388. [DOI] [PubMed] [Google Scholar]
- 33.Nojiri T, Watanabe N, Namura T, Narita W, Ikoma K, Suginoshita T, et al. Utility of delayed gadolinium-enhanced MRI (dGEMRIC) for qualitative evaluation of articular cartilage of patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:718–23. doi: 10.1007/s00167-005-0013-6. [DOI] [PubMed] [Google Scholar]
- 34.Koff MF, Amrami KK, Kaufman KR. Clinical evaluation of T2 values of patellar cartilage in patients with osteoarthritis. Osteoarthritis Cartilage. 2007;15:198–204. doi: 10.1016/j.joca.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 35.Li X, Benjamin MC, Link TM, Castillo DD, Blumenkrantz G, Lozano J, et al. In vivo T(1rho) and T(2) mapping of articular cartilage in osteoarthritis of the knee using 3 T MRI. Osteoarthritis Cartilage. 2007;15:789–97. doi: 10.1016/j.joca.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chan WP, Lang P, Stevens MP, Sack K, Majumdar S, Stoller DW, et al. Osteoarthritis of the knee: comparison of radiography, CT, and MR imaging to assess extent and severity. AJR Am J Roentgenol. 1991;157:799–806. doi: 10.2214/ajr.157.4.1892040. [DOI] [PubMed] [Google Scholar]
- 37.Blackburn WD, Jr, Bernreuter WK, Rominger M, Loose LL. Arthroscopic evaluation of knee articular cartilage: a comparison with plain radiographs and magnetic resonance imaging. J Rheumatol. 1994;21:675–9. [PubMed] [Google Scholar]
- 38.Wluka AE, Wang Y, Davis SR, Cicuttini FM. Tibial plateau size is related to grade of joint space narrowing and osteophytes in healthy women and in women with osteoarthritis. Ann Rheum Dis. 2005;64:1033–7. doi: 10.1136/ard.2004.029082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakamura M, Sumen Y, Sakaridani K, Exham H, Ochi M. Relationship between the shape of tibial spurs on X-ray and meniscal changes on MRI in early osteoarthritis of the knee. Magn Reson Imaging. 2006;24:1143–8. doi: 10.1016/j.mri.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 40.Englund M, Niu J, Guermazi A, Roemer FW, Hunter DJ, Lynch JA, et al. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum. 2007;56:4048–54. doi: 10.1002/art.23071. [DOI] [PubMed] [Google Scholar]
- 41.Reichenbach S, Guermazi A, Niu J, Neogi T, Hunter DJ, Roemer FW, et al. Prevalence of bone attrition on knee radiographs and MRI in a community-based cohort. Osteoarthritis Cartilage. 2008;16:1005–10. doi: 10.1016/j.joca.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Folkesson J, Dam EB, Olsen OF, Karsdal MA, Pettersen PC, Christiansen C. Automatic quantification of local and global articular cartilage surface curvature: biomarkers for osteoarthritis? Magn Reson Med. 2008;59:1340–6. doi: 10.1002/mrm.21560. [DOI] [PubMed] [Google Scholar]
- 43.Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage. 1999;7:526–32. doi: 10.1053/joca.1999.0256. [DOI] [PubMed] [Google Scholar]
- 44.Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54:502–6. doi: 10.1016/s0009-9260(99)90846-2. [DOI] [PubMed] [Google Scholar]
- 45.Hill CL, Seo GS, Gale D, Totterman S, Gale ME, Felson DT. Cruciate ligament integrity in osteoarthritis of the knee. Arthritis Rheum. 2005;52:794–9. doi: 10.1002/art.20943. [DOI] [PubMed] [Google Scholar]
- 46.Cicuttini FM, Wang YY, Forbes A, Wluka AE, Glisson M. Comparison between patella cartilage volume and radiological assessment of the patellofemoral joint. Clin Exp Rheumatol. 2003;21:321–6. [PubMed] [Google Scholar]
- 47.Jones G, Ding C, Scott F, Glisson M, Cicuttini F. Early radiographic osteoarthritis is associated with substantial changes in cartilage volume and tibial bone surface area in both males and females. Osteoarthritis Cartilage. 2004;12:169–74. doi: 10.1016/j.joca.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 48.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, Labonte F, Beaudoin G, de Guise JA, et al. Quantitative magnetic resonance imaging evaluation of knee osteoarthritis progression over two years and correlation with clinical symptoms and radiologic changes. Arthritis Rheum. 2004;50:476–87. doi: 10.1002/art.20000. [DOI] [PubMed] [Google Scholar]
- 49.Ding C, Garnero P, Cicuttini F, Scott F, Cooley H, Jones G, et al. Knee cartilage defects: association with early radiographic osteoarthritis, decreased cartilage volume, increased joint surface area and type II collagen breakdown. Osteoarthritis Cartilage. 2005;13:198–205. doi: 10.1016/j.joca.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 50.Cicuttini F, Hankin J, Jones G, Wluka A. Comparison of conventional standing knee radiographs and magnetic resonance imaging in assessing progression of tibiofemoral joint osteoarthritis. Osteoarthritis Cartilage. 2005;13:722–7. doi: 10.1016/j.joca.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 51.Felson DT, McLaughlin S, Goggins J, Lavalley MP, Gale ME, Totterman S, et al. Bone marrow edema and its relation to progression of knee osteoarthritis. Ann Intern Med. 2003;139:330–6. doi: 10.7326/0003-4819-139-5_part_1-200309020-00008. [DOI] [PubMed] [Google Scholar]
- 52.Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford) 2004;43:321–4. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 53.Hunter DJ, Zhang Y, Niu J, Tu X, Amin S, Goggins J, et al. Structural factors associated with malalignment in knee osteoarthritis: the Boston osteoarthritis knee study. J Rheumatol. 2005;32:2192–9. [see comment] [PubMed] [Google Scholar]
- 54.Issa SN, Dunlop D, Chang A, Song J, Prasad PV, Guermazi A, et al. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum. 2007;57:398–406. doi: 10.1002/art.22618. [DOI] [PubMed] [Google Scholar]
- 55.Janakiramanan N, Teichtahl AJ, Wluka AE, Ding C, Jones G, Davis SR, et al. Static knee alignment is associated with the risk of unicompartmental knee cartilage defects. J Orthop Res. 2008;26:225–30. doi: 10.1002/jor.20465. [DOI] [PubMed] [Google Scholar]
- 56.Eckstein F, Schnier M, Haubner M, Priebsch J, Glaser C, Englmeier KH, et al. Accuracy of cartilage volume and thickness measurements with magnetic resonance imaging. Clin Orthop Relat Res. 1998;(352):137–48. [PubMed] [Google Scholar]
- 57.Dupuy DE, Spillane RM, Rosol MS, Rosenthal DI, Palmer WE, Burke DW, et al. Quantification of articular cartilage in the knee with three-dimensional MR imaging. Acad Radiol. 1996;3:919–24. doi: 10.1016/s1076-6332(96)80299-6. [DOI] [PubMed] [Google Scholar]
- 58.Uhl M, Ihling C, Allmann KH, Laubenberger J, Tauer U, Adler CP, et al. Human articular cartilage: in vitro correlation of MRI and histologic findings. Eur Radiol. 1998;8:1123–9. doi: 10.1007/s003300050519. [DOI] [PubMed] [Google Scholar]
- 59.Kladny B, Martus P, Schiwy-Bochat KH, Weseloh G, Swoboda B. Measurement of cartilage thickness in the human knee-joint by magnetic resonance imaging using a three-dimensional gradient-echo sequence. Int Orthop. 1999;23:264–7. doi: 10.1007/s002640050367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McGibbon CA, Trahan CA. Measurement accuracy of focal cartilage defects from MRI and correlation of MRI graded lesions with histology: a preliminary study. Osteoarthritis Cartilage. 2003;11:483–93. doi: 10.1016/s1063-4584(03)00078-5. [DOI] [PubMed] [Google Scholar]
- 61.Broderick LS, Turner DA, Renfrew DL, Schnitzer TJ, Huff JP, Harris C. Severity of articular cartilage abnormality in patients with osteoarthritis: evaluation with fast spin-echo MR vs arthroscopy. AJR Am J Roentgenol. 1994;162:99–103. doi: 10.2214/ajr.162.1.8273700. [DOI] [PubMed] [Google Scholar]
- 62.Kawahara Y, Uetani M, Nakahara N, Doiguchi Y, Nishiguchi M, Futagawa S, et al. Fast spin-echo MR of the articular cartilage in the osteoarthrotic knee. Correlation of MR and arthroscopic findings. Acta Radiol. 1998;39:120–5. doi: 10.1080/02841859809172164. [DOI] [PubMed] [Google Scholar]
- 63.Drape JL, Pessis E, Auleley GR, Chevrot A, Dougados M, Ayral X. Quantitative MR imaging evaluation of chondropathy in osteoarthritic knees. Radiology. 1998;208:49–55. doi: 10.1148/radiology.208.1.9646792. [DOI] [PubMed] [Google Scholar]
- 64.Bachmann GF, Basad E, Rauber K, Damian MS, Rau WS. Degenerative joint disease on MRI and physical activity: a clinical study of the knee joint in 320 patients. Eur Radiol. 1999;9:145–52. doi: 10.1007/s003300050646. [DOI] [PubMed] [Google Scholar]
- 65.Cicuttini FM, Jones G, Forbes A, Wluka AE. Rate of cartilage loss at two years predicts subsequent total knee arthroplasty: a prospective study. Ann Rheum Dis. 2004;63:1124–7. doi: 10.1136/ard.2004.021253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wluka AE, Ding C, Jones G, Cicuttini FM. The clinical correlates of articular cartilage defects in symptomatic knee osteoarthritis: a prospective study. Rheumatology (Oxford) 2005;44:1311–6. doi: 10.1093/rheumatology/kei018. [DOI] [PubMed] [Google Scholar]
- 67.Scher C, Craig J, Nelson F. Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skeletal Radiol. 2008;37:609–17. doi: 10.1007/s00256-008-0504-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Phan CM, Link TM, Blumenkrantz G, Dunn TC, Ries MD, Steinbach LS, et al. MR imaging findings in the follow-up of patients with different stages of knee osteoarthritis and the correlation with clinical symptoms. Eur Radiol. 2006;16:608–18. doi: 10.1007/s00330-005-0004-5. [DOI] [PubMed] [Google Scholar]
- 69.Katz JN, Meredith DS, Lang P, Creel AH, Yoshioka H, Neumann G, et al. Associations among preoperative MRI features and functional status following arthroscopic partial meniscectomy. Osteoarthritis Cartilage. 2006;14:418–22. doi: 10.1016/j.joca.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 70.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 71.Pelletier JP, Raynauld JP, Berthiaume MJ, Abram F, Choquette D, Haraoui B, et al. Risk factors associated with the loss of cartilage volume on weight-bearing areas in knee osteoarthritis patients assessed by quantitative magnetic resonance imaging: a longitudinal study. Arthritis Res Ther. 2007;9:R74. doi: 10.1186/ar2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, Beaudoin G, Choquette D, Haraoui B, et al. Long term evaluation of disease progression through the quantitative magnetic resonance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthritis Res Ther. 2006;8:R21. doi: 10.1186/ar1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bruyere O, Genant H, Kothari M, Zaim S, White D, Peterfy C, et al. Longitudinal study of magnetic resonance imaging and standard X-rays to assess disease progression in osteoarthritis. Osteoarthritis Cartilage. 2007;15:98–103. doi: 10.1016/j.joca.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 74.Nevitt MC, Peterfy C, Guermazi A, Felson DT, Duryea J, Woodworth T, et al. Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum. 2007;56:1512–20. doi: 10.1002/art.22557. [DOI] [PubMed] [Google Scholar]
- 75.Madan-Sharma R, Kloppenburg M, Kornaat PR, Botha-Scheepers SA, Le Graverand MP, Bloem JL, et al. Do MRI features at baseline predict radiographic joint space narrowing in the medial compartment of the osteoarthritic knee 2 years later? Skeletal Radiol. 2008;37:805–11. doi: 10.1007/s00256-008-0508-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Biswal S, Hastie T, Andriacchi TP, Bergman GA, Dillingham MF, Lang P. Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum. 2002;46:2884–92. doi: 10.1002/art.10573. [DOI] [PubMed] [Google Scholar]
- 77.Cicuttini FM, Wluka AE, Wang Y, Stuckey SL, Cicuttini FM, Wluka AE, et al. Longitudinal study of changes in tibial and femoral cartilage in knee osteoarthritis. Arthritis Rheum. 2004;50:94–7. doi: 10.1002/art.11483. [see comment] [DOI] [PubMed] [Google Scholar]
- 78.Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–63. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang Y, Ding C, Wluka AE, Davis S, Ebeling PR, Jones G, et al. Factors affecting progression of knee cartilage defects in normal subjects over 2 years. Rheumatology (Oxford) 2006;45:79–84. doi: 10.1093/rheumatology/kei108. [DOI] [PubMed] [Google Scholar]
- 80.Ding C, Cicuttini F, Scott F, Boon C, Jones G. Association of prevalent and incident knee cartilage defects with loss of tibial and patellar cartilage: a longitudinal study. Arthritis Rheum. 2005;52:3918–27. doi: 10.1002/art.21474. [DOI] [PubMed] [Google Scholar]
- 81.Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 82.Ding C, Cicuttini F, Scott F, Cooley H, Boon C, Jones G. Natural history of knee cartilage defects and factors affecting change. Arch Intern Med. 2006;166:651–8. doi: 10.1001/archinte.166.6.651. [DOI] [PubMed] [Google Scholar]
- 83.Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP, et al. Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum. 2006;54:1529–35. doi: 10.1002/art.21789. [DOI] [PubMed] [Google Scholar]
- 84.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, Abram F, Choquette D, Haraoui B, et al. Correlation between bone lesion changes and cartilage volume loss in patients with osteoarthritis of the knee as assessed by quantitative magnetic resonance imaging over a 24-month period. Ann Rheum Dis. 2008;67:683–8. doi: 10.1136/ard.2007.073023. [DOI] [PubMed] [Google Scholar]
- 85.Davies-Tuck ML, Martel-Pelletier J, Wluka AE, Pelletier JP, Ding C, Jones G, et al. Meniscal tear and increased tibial plateau bone area in healthy post-menopausal women. Osteoarthritis Cartilage. 2008;16:268–71. doi: 10.1016/j.joca.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 86.Amin S, Guermazi A, Lavalley MP, Niu J, Clancy M, Hunter DJ, et al. Complete anterior cruciate ligament tear and the risk for cartilage loss and progression of symptoms in men and women with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:897–902. doi: 10.1016/j.joca.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, et al. Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58:1716–26. doi: 10.1002/art.23462. [DOI] [PubMed] [Google Scholar]
- 88.Gossec L, Hawker G, Davis AM, Maillefert JF, Lohmander LS, Altman R, et al. OMERACT/OARSI initiative to define states of severity and indication for joint replacement in hip and knee osteoarthritis. J Rheumatol. 2007;34:1432–5. [12 refs] [PubMed] [Google Scholar]
- 89.Ornetti P, Brandt K, Hellio Graverand M, Hochberg M, Hunter D, Kloppenburg M, et al. OARSI-OMERACT definition of relevant radiological progression in hip/knee osteoarthritis. Osteoarthritis Cartilage. 2009 Jul;17(7):856–63. doi: 10.1016/j.joca.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McAlindon TE, Watt I, McCrae F, Goddard P, Dieppe PA. Magnetic resonance imaging in osteoarthritis of the knee: correlation with radiographic and scintigraphic findings. Ann Rheum Dis. 1991;50:14–9. doi: 10.1136/ard.50.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Li KC, Higgs J, Aisen AM, Buckwalter KA, Martel W, McCune WJ. MRI in osteoarthritis of the hip: gradations of severity. Magn Reson Imaging. 1988;6:229–36. doi: 10.1016/0730-725x(88)90396-7. [DOI] [PubMed] [Google Scholar]
- 92.Fernandez-Madrid F, Karvonen RL, Teitge RA, Miller PR, Negendank WG. MR features of osteoarthritis of the knee. Magn Reson Imaging. 1994;12:703–9. doi: 10.1016/0730-725x(94)92194-6. [DOI] [PubMed] [Google Scholar]
- 93.Peterfy C, van Dijke C, Janzen D, Gluer C, Namba R, Majumdar S, et al. Quantification of articular cartilage in the knee with pulsed saturation transfer subtraction and fat-suppressed MR imaging: optimization and validation. Radiology. 1994;192:485–91. doi: 10.1148/radiology.192.2.8029420. [DOI] [PubMed] [Google Scholar]
- 94.Miller TT, Staron RB, Koenigsberg T, Levin TL, Feldman F. MR imaging of Baker cysts: association with internal derangement, effusion, and degenerative arthropathy. Radiology. 1996;201:247–50. doi: 10.1148/radiology.201.1.8816552. [see comment] [DOI] [PubMed] [Google Scholar]
- 95.Kenny C. Radial displacement of the medial meniscus and Fairbank’s signs. Clin Orthop Relat Res. 1997;(339):163–73. doi: 10.1097/00003086-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 96.Breitenseher MJ, Trattnig S, Dobrocky I, Kukla C, Nehrer S, Steiner E, et al. MR imaging of meniscal subluxation in the knee. Acta Radiol. 1997;38:876–9. doi: 10.1080/02841859709172428. [DOI] [PubMed] [Google Scholar]
- 97.Ostergaard M. Different approaches to synovial membrane volume determination by magnetic resonance imaging: manual versus automated segmentation. Br J Rheumatol. 1997;36:1166–77. doi: 10.1093/rheumatology/36.11.1166. [DOI] [PubMed] [Google Scholar]
- 98.Trattnig S, Huber M, Breitenseher MJ, Trnka HJ, Rand T, Kaider A, et al. Imaging articular cartilage defects with 3D fat-suppressed echo planar imaging: comparison with conventional 3D fat-suppressed gradient echo sequence and correlation with histology. J Comput Assist Tomogr. 1998;22:8–14. doi: 10.1097/00004728-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 99.Boegard T. Radiography and bone scintigraphy in osteoarthritis of the knee–comparison with MR imaging. Acta Radiol. 1998;418:7–37. Supplementum. [PubMed] [Google Scholar]
- 100.Cicuttini F, Forbes A, Morris K, Darling S, Bailey M, Stuckey S. Gender differences in knee cartilage volume as measured by magnetic resonance imaging. Osteoarthritis Cartilage. 1999;7:265–71. doi: 10.1053/joca.1998.0200. [DOI] [PubMed] [Google Scholar]
- 101.Boegard T, Rudling O, Dahlstrom J, Dirksen H, Petersson IF, Jonsson K. Bone scintigraphy in chronic knee pain: comparison with magnetic resonance imaging. Ann Rheum Dis. 1999;58:20–6. doi: 10.1136/ard.58.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pham XV, Monteiro I, Judet O, Sissakian JF, Plantin P, Aegerter P, et al. Magnetic resonance imaging changes in periarticular soft tissues during flares of medial compartment knee osteoarthritis. Preliminary study in 10 p. tients. Rev Rhum Engl Ed. 1999;66:398–403. [PubMed] [Google Scholar]
- 103.Zanetti M, Bruder E, Romero J, Hodler J. Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology. 2000;215:835–40. doi: 10.1148/radiology.215.3.r00jn05835. [DOI] [PubMed] [Google Scholar]
- 104.Jones G, Glisson M, Hynes K, Cicuttini F. Sex and site differences in cartilage development: a possible explanation for variations in knee osteoarthritis in later life. Arthritis Rheum. 2000;43:2543–9. doi: 10.1002/1529-0131(200011)43:11<2543::AID-ANR23>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 105.McCauley TR, Kornaat PR, Jee WH. Central osteophytes in the knee: prevalence and association with cartilage defects on MR imaging. AJR Am J Roentgenol. 2001;176:359–64. doi: 10.2214/ajr.176.2.1760359. [DOI] [PubMed] [Google Scholar]
- 106.Wluka AE, Davis SR, Bailey M, Stuckey SL, Cicuttini FM. Users of oestrogen replacement therapy have more knee cartilage than non-users. Ann Rheum Dis. 2001;60:332–6. doi: 10.1136/ard.60.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kawahara Y, Uetani M, Fuchi K, Eguchi H, Hashmi R, Hayashi K. MR assessment of meniscal movement during knee flexion: correlation with the severity of cartilage abnormality in the femorotibial joint. J Comput Assist Tomogr. 2001;25:683–90. doi: 10.1097/00004728-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 108.Arokoski JP, Arokoski MH, Jurvelin JS, Helminen HJ, Niemitukia LH, Kroger H. Increased bone mineral content and bone size in the femoral neck of men with hip osteoarthritis. Ann Rheum Dis. 2002;61:145–50. doi: 10.1136/ard.61.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bergin D, Keogh C, O’Connell M, Rowe D, Shah B, Zoga A, et al. Atraumatic medial collateral ligament oedema in medial compartment knee osteoarthritis. Skeletal Radiol. 2002;31:14–8. doi: 10.1007/s002560100418. [DOI] [PubMed] [Google Scholar]
- 110.Beuf O, Ghosh S, Newitt DC, Link TM, Steinbach L, Ries M, et al. Magnetic resonance imaging of normal and osteoarthritic trabecular bone structure in the human knee. Arthritis Rheum. 2002;46:385–93. doi: 10.1002/art.10108. [DOI] [PubMed] [Google Scholar]
- 111.Arokoski MH, Arokoski JP, Haara M, Kankaanpaa M, Vesterinen M, Niemitukia LH, et al. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J Rheumatol. 2002;29:2185–95. [PubMed] [Google Scholar]
- 112.Tiderius CJ, Olsson LE, Leander P, Ekberg O, Dahlberg L. Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) in early knee osteoarthritis. Magn Reson Med. 2003;49:488–92. doi: 10.1002/mrm.10389. [DOI] [PubMed] [Google Scholar]
- 113.Cicuttini FM, Wluka AE, Wang Y, Stuckey SL, Davis SR. Effect of estrogen replacement therapy on patella cartilage in healthy women. Clin Exp Rheumatol. 2003;21:79–82. [PubMed] [Google Scholar]
- 114.Tarhan S, Unlu Z. Magnetic resonance imaging and ultrasonographic evaluation of the patients with knee osteoarthritis: a comparative study. Clin Rheumatol. 2003;22:181–8. doi: 10.1007/s10067-002-0694-x. [DOI] [PubMed] [Google Scholar]
- 115.Kim YJ, Jaramillo D, Millis MB, Gray ML, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003;85-A:1987–92. doi: 10.2106/00004623-200310000-00019. [DOI] [PubMed] [Google Scholar]
- 116.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–90. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 117.Graichen H, Eisenhart-Rothe R, Vogl T, Englmeier KH, Eckstein F. Quantitative assessment of cartilage status in osteoarthritis by quantitative magnetic resonance imaging: technical validation for use in analysis of cartilage volume and further morphologic parameters. Arthritis Rheum. 2004;50:811–6. doi: 10.1002/art.20191. [DOI] [PubMed] [Google Scholar]
- 118.Dashti M, Wluka AE, Geso M, Davis SR, Stuckey S, Cicuttini FM. Relationship between the area of cartilage shown on the magnetic resonance imaging middle-slice image of the medial and lateral tibial cartilages with cartilage volume and grade of osteoarthritis over time. Scand J Rheumatol. 2004;33:87–93. doi: 10.1080/03009740310004612. [DOI] [PubMed] [Google Scholar]
- 119.Arokoski JP, Arokoski MH, Vainio P, Kroger H, Jurvelin JS. Estimation of femoral head bone density using magnetic resonance imaging: comparison between men with and without hip osteoarthritis. J Clin Densitom. 2004;7:183–91. doi: 10.1385/jcd:7:2:183. [DOI] [PubMed] [Google Scholar]
- 120.Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232:592–8. doi: 10.1148/radiol.2322030976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Regatte RR, Akella SV, Wheaton AJ, Lech G, Borthakur A, Kneeland JB, et al. 3D-T1rho-relaxation mapping of articular cartilage: in vivo assessment of early degenerative changes in symptomatic osteoarthritic subjects. Acad Radiol. 2004;11:741–9. doi: 10.1016/j.acra.2004.03.051. [DOI] [PubMed] [Google Scholar]
- 122.Baysal O, Baysal T, Alkan A, Altay Z, Yologlu S. Comparison of MRI graded cartilage and MRI based volume measurement in knee osteoarthritis. Swiss Med Wkly. 2004;134:283–8. doi: 10.4414/smw.2004.10546. [DOI] [PubMed] [Google Scholar]
- 123.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–74. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 124.King KB, Lindsey CT, Dunn TC, Ries MD, Steinbach LS, Majumdar S. A study of the relationship between molecular biomarkers of joint degeneration and the magnetic resonance-measured characteristics of cartilage in 16 symptomatic knees. Magn Reson Imaging. 2004;22:1117–23. doi: 10.1016/j.mri.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 125.Carbone LD, Nevitt MC, Wildy K, Barrow KD, Harris F, Felson D, et al. The relationship of antiresorptive drug use to structural findings and symptoms of knee osteoarthritis. Arthritis Rheum. 2004;50:3516–25. doi: 10.1002/art.20627. [see comment] [DOI] [PubMed] [Google Scholar]
- 126.Cicuttini F, Morris KF, Glisson M, Wluka AE. Slice thickness in the assessment of medial and lateral tibial cartilage volume and accuracy for the measurement of change in a longitudinal study. J Rheumatol. 2004;31:2444–8. [PubMed] [Google Scholar]
- 127.Kornaat PR, Watt I, Riyazi N, Kloppenburg M, Bloem JL. The relationship between the MRI features of mild osteoarthritis in the patellofemoral and tibiofemoral compartments of the knee. Eur Radiol. 2005;15:1538–43. doi: 10.1007/s00330-005-2691-3. [DOI] [PubMed] [Google Scholar]
- 128.Zhai G, Cicuttini F, Srikanth V, Cooley H, Ding C, Jones G. Factors associated with hip cartilage volume measured by magnetic resonance imaging: the Tasmanian older adult cohort study. Arthritis Rheum. 2005;52:1069–76. doi: 10.1002/art.20964. [DOI] [PubMed] [Google Scholar]
- 129.Blankenbaker DG, De Smet AA, Fine JP. Is intra-articular pathology associated with MCL edema on MR imaging of the non-traumatic knee? Skeletal Radiol. 2005;34:462–7. doi: 10.1007/s00256-005-0931-x. [DOI] [PubMed] [Google Scholar]
- 130.Huh YM, Kim S, Suh JS, Song H, Song K, Shin KH. The role of popliteal lymph nodes in differentiating rheumatoid arthritis from osteoarthritis by using CE 3D FSPGR MR imaging: relationship of the inflamed synovial volume. Korean J Radiol. 2005;6:117–24. doi: 10.3348/kjr.2005.6.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.von Eisenhart-Rothe R, Graichen H, Hudelmaier M, Vogl T, Sharma L, Eckstein F. Femorotibial and patellar cartilage loss in patients prior to total knee arthroplasty, heterogeneity, and correlation with alignment of the knee. Ann Rheum Dis. 2006;65:69–73. doi: 10.1136/ard.2005.038869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tan AL, Grainger AJ, Tanner SF, Shelley DM, Pease C, Emery P, et al. High-resolution magnetic resonance imaging for the assessment of hand osteoarthritis. Arthritis Rheum. 2005;52:2355–65. doi: 10.1002/art.21210. [DOI] [PubMed] [Google Scholar]
- 133.Lo GH, Hunter DJ, Zhang Y, McLennan CE, LaValley MP, Kiel DP, et al. Bone marrow lesions in the knee are associated with increased local bone density. Arthritis Rheum. 2005;52:2814–21. doi: 10.1002/art.21290. [DOI] [PubMed] [Google Scholar]
- 134.Li X, Han ET, Ma CB, Link TM, Newitt DC, Majumdar S. In vivo 3T spiral imaging based multi-slice T(1rho) mapping of knee cartilage in osteoarthritis. Magn Reson Med. 2005;54:929–36. doi: 10.1002/mrm.20609. [DOI] [PubMed] [Google Scholar]
- 135.Rhodes LA, Grainger AJ, Keenan AM, Thomas C, Emery P, Conaghan PG. The validation of simple scoring methods for evaluating compartment-specific synovitis detected by MRI in knee osteoarthritis. Rheumatology. 2005;44:1569–73. doi: 10.1093/rheumatology/kei094. [DOI] [PubMed] [Google Scholar]
- 136.Loeuille D, Chary-Valckenaere I, Champigneulle J, Rat AC, Toussaint F, Pinzano-Watrin A, et al. Macroscopic and microscopic features of synovial membrane inflammation in the osteoarthritic knee: correlating magnetic resonance imaging findings with disease severity. Arthritis Rheum. 2005;52:3492–501. doi: 10.1002/art.21373. [DOI] [PubMed] [Google Scholar]
- 137.Roos EM, Dahlberg L, Roos EM, Dahlberg L. Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four-month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheum. 2005;52:3507–14. doi: 10.1002/art.21415. [DOI] [PubMed] [Google Scholar]
- 138.Kimelman T, Vu A, Storey P, McKenzie C, Burstein D, Prasad P. Three-dimensional T1 mapping for dGEMRIC at 3. 0 T using the look locker method. Invest Radiol. 2006;41:198–203. doi: 10.1097/01.rli.0000195842.49255.ea. [DOI] [PubMed] [Google Scholar]
- 139.Sengupta M, Zhang YQ, Niu JB, Guermazi A, Grigorian M, Gale D, et al. High signal in knee osteophytes is not associated with knee pain. Osteoarthritis Cartilage. 2006;14:413–7. doi: 10.1016/j.joca.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 140.Grainger AJ, Rhodes LA, Keenan AM, Emery P, Conaghan PG. Quantifying peri-meniscal synovitis and its relationship to meniscal pathology in osteoarthritis of the knee. Eur Radiol. 2007;17:119–24. doi: 10.1007/s00330-006-0282-6. [DOI] [PubMed] [Google Scholar]
- 141.Cashman PM, Kitney RI, Gariba MA, Carter ME. Automated techniques for visualization and mapping of articular cartilage in MR images of the osteoarthritic knee: a base technique for the assessment of microdamage and submicro damage. IEEE Trans Nanobioscience. 2002;1:42–51. doi: 10.1109/tnb.2002.806916. [DOI] [PubMed] [Google Scholar]
- 142.Bamac B, Ozdemir S, Sarisoy HT, Colak T, Ozbek A, Akansel G. Evaluation of medial and lateral meniscus thicknesses in early osteoarthritis of the knee with magnetic resonance imaging. Saudi Med J. 2006;27:854–7. [PubMed] [Google Scholar]
- 143.Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006;34:1984–91. doi: 10.1177/0363546506290189. [DOI] [PubMed] [Google Scholar]
- 144.Folkesson J, Dam EB, Olsen OF, Pettersen PC, Christiansen C. Segmenting articular cartilage automatically using a voxel classification approach. IEEE Trans Med Imaging. 2007;26:106–15. doi: 10.1109/TMI.2006.886808. [DOI] [PubMed] [Google Scholar]
- 145.Iwasaki J, Sasho T, Nakagawa K, Ogino S, Ochiai N, Moriya H. Irregularity of medial femoral condyle on MR imaging serves as a possible indicator of objective severity of medial-type osteoarthritic knee-a pilot study. Clin Rheumatol. 2007;26:1705–8. doi: 10.1007/s10067-007-0578-1. [DOI] [PubMed] [Google Scholar]
- 146.Tiderius CJ, Jessel R, Kim YJ, Burstein D. Hip dGEMRIC in asymptomatic volunteers and patients with early osteoarthritis: the influence of timing after contrast injection. Magn Reson Med. 2007;57:803–5. doi: 10.1002/mrm.21190. [DOI] [PubMed] [Google Scholar]
- 147.Baranyay FJ, Wang Y, Wluka AE, English DR, Giles GG, Sullivan RO, et al. Association of bone marrow lesions with knee structures and risk factors for bone marrow lesions in the knees of clinically healthy, community-based adults. Semin Arthritis Rheum. 2007;37:112–8. doi: 10.1016/j.semarthrit.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 148.Hanna F, Teichtahl AJ, Bell R, Davis SR, Wluka AE, O’Sullivan R, et al. The cross-sectional relationship between fortnightly exercise and knee cartilage properties in healthy adult women in midlife. Menopause. 2007;14:830–4. doi: 10.1097/gme.0b013e31802f316b. [see comment] [DOI] [PubMed] [Google Scholar]
- 149.Qazi AA, Folkesson J, Pettersen PC, Karsdal MA, Christiansen C, Dam EB. Separation of healthy and early osteoarthritis by automatic quantification of cartilage homogeneity. Osteoarthritis Cartilage. 2007;15:1199–206. doi: 10.1016/j.joca.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 150.Lammentausta E, Kiviranta P, Toyras J, Hyttinen s, Kiviranta I, Nieminen MT, et al. Quantitative MRI of parallel changes of articular cartilage and underlying trabecular bone in degeneration. Osteoarthritis Cartilage. 2007;15:1149–57. doi: 10.1016/j.joca.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 151.Guymer E, Baranyay F, Wluka AE, Hanna F, Bell RJ, Davis SR, et al. A study of the prevalence and associations of subchondral bone marrow lesions in the knees of healthy, middle-aged women. Osteoarthritis Cartilage. 2007;15:1437–42. doi: 10.1016/j.joca.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 152.Nishii T, Tanaka H, Sugano N, Sakai T, Hananouchi T, Yoshikawa H. Evaluation of cartilage matrix disorders by T2 relaxation time in patients with hip dysplasia. Osteoarthritis Cartilage. 2008;16:227–33. doi: 10.1016/j.joca.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 153.Lo GH, Niu J, McLennan CE, Kiel DP, McLean RR, Guermazi A, et al. Meniscal damage associated with increased local sub-chondral bone mineral density: a Framingham study. Osteoarthritis Cartilage. 2008;16:261–7. doi: 10.1016/j.joca.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Davies-Tuck M, Teichtahl AJ, Wluka AE, Wang Y, Urquhart DM, Cui J, et al. Femoral sulcus angle and increased patella facet cartilage volume in an osteoarthritic population. Osteoarthritis Cartilage. 2008;16:131–5. doi: 10.1016/j.joca.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 155.Qazi AA, Dam EB, Nielsen M, Karsdal MA, Pettersen PC, Christiansen C. Osteoarthritic cartilage is more homogeneous than healthy cartilage: identification of a superior region of interest colocalized with a major risk factor for osteoarthritis. Acad Radiol. 2007;14:1209–20. doi: 10.1016/j.acra.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 156.Folkesson J, Dam EB, Olsen OF, Christiansen C. Accuracy evaluation of automatic quantification of the articular cartilage surface curvature from MRI. Acad Radiol. 2007;14:1221–8. doi: 10.1016/j.acra.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 157.Kamei G, Sumen Y, Sakaridani K. Evaluation of cartilage defect at medial femoral condyle in early osteoarthritis of the knee. Magn Reson Imaging. 2008;26:567–71. doi: 10.1016/j.mri.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 158.Li W, Scheidegger R, Wu Y, Vu A, Prasad PV. Accuracy of T1 measurement with 3-D look-locker technique for dGEMRIC. J Magn Reson Imaging. 2008;27:678–82. doi: 10.1002/jmri.21244. [DOI] [PubMed] [Google Scholar]
- 159.Taljanovic MS, Graham AR, Benjamin JB, Gmitro AF, Krupinski EA, Schwartz SA, et al. Bone marrow edema pattern in advanced hip osteoarthritis: quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skeletal Radiol. 2008;37:423–31. doi: 10.1007/s00256-008-0446-3. [DOI] [PubMed] [Google Scholar]
- 160.Oda H, Igarashi M, Sase H, Sase T, Yamamoto S. Bone bruise in magnetic resonance imaging strongly correlates with the production of joint effusion and with knee osteoarthritis. J Orthop Sci. 2008;13:7–15. doi: 10.1007/s00776-007-1195-1. [DOI] [PubMed] [Google Scholar]
- 161.Hanna FS, Bell RJ, Cicuttini FM, Davison SL, Wluka AE, Davis SR. High sensitivity C-reactive protein is associated with lower tibial cartilage volume but not lower patella cartilage volume in healthy women at mid-life. Arthritis Res Ther. 2008;10:R27. doi: 10.1186/ar2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Petterson SC, Barrance P, Buchanan T, Binder-Macleod S, Snyder-Mackler L. Mechanisms underlying quadriceps weakness in knee osteoarthritis. Med Sci Sports Exerc. 2008;40:422–7. doi: 10.1249/MSS.0b013e31815ef285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bolbos RI, Zuo J, Banerjee S, Link TM, Ma CB, Li X, et al. Relationship between trabecular bone structure and articular cartilage morphology and relaxation times in early OA of the knee joint using parallel MRI at 3 T. Osteoarthritis Cartilage. 2008;16:1150–9. doi: 10.1016/j.joca.2008.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Quaia E, Toffanin R, Guglielmi G, Ukmar M, Rossi A, Martinelli B, et al. Fast T2 mapping of the patellar articular cartilage with gradient and spin-echo magnetic resonance imaging at 1. 5 T: validation and initial clinical experience in patients with osteoarthritis. Skeletal Radiol. 2008;37:511–7. doi: 10.1007/s00256-008-0478-8. [DOI] [PubMed] [Google Scholar]
- 165.Mills PM, Wang Y, Cicuttini FM, Stoffel K, Stachowiak GW, Podsiadlo P, et al. Tibio-femoral cartilage defects 3–5 years following arthroscopic partial medial meniscectomy. Osteoarthritis Cartilage. 2008;16:1526–31. doi: 10.1016/j.joca.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 166.Dore D, Ding C, Jones G. A pilot study of the reproducibility and validity of measuring knee subchondral bone density in the tibia. Osteoarthritis Cartilage. 2008;16:1539–44. doi: 10.1016/j.joca.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 167.Mutimer J, Green J, Field J. Comparison of MRI and wrist arthroscopy for assessment of wrist cartilage. J Hand Surg Eur Vol. 2008;33:380–2. doi: 10.1177/1753193408090395. [DOI] [PubMed] [Google Scholar]
- 168.Amin S, Goggins J, Niu J, Guermazi A, Grigoryan M, Hunter DJ, et al. Occupation-related squatting, kneeling, and heavy lifting and the knee joint: a magnetic resonance imaging-based study in men. J Rheumatol. 2008;35:1645–9. [PMC free article] [PubMed] [Google Scholar]
- 169.Li X, Ma BC, Bolbos RI, Stahl R, Lozano J, Zuo J, et al. Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 Tesla. J Magn Reson Imaging. 2008;28:453–61. doi: 10.1002/jmri.21437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Stahl R, Luke A, Li X, Carballido-Gamio J, Ma CB, Majumdar S, et al. T1rho, T2 and focal knee cartilage abnormalities in physically active and sedentary healthy subjects versus early OA patients–a 3. 0-Tesla MRI study. Eur Radiol. 2009;19:132–43. doi: 10.1007/s00330-008-1107-6. [DOI] [PubMed] [Google Scholar]
- 171.Brem MH, Schlechtweg PM, Bhagwat J, Genovese M, Dillingham MF, Yoshioka H, et al. Longitudinal evaluation of the occurrence of MRI-detectable bone marrow edema in osteoarthritis of the knee. Acta Radiol. 2008;49:1031–7. doi: 10.1080/02841850802339413. [DOI] [PubMed] [Google Scholar]
- 172.Lancianese SL, Kwok E, Beck CA, Lerner AL. Predicting regional variations in trabecular bone mechanical properties within the human proximal tibia using MR imaging. Bone. 2008;43:1039–46. doi: 10.1016/j.bone.2008.07.247. [DOI] [PubMed] [Google Scholar]
- 173.Mamisch TC, Dudda M, Hughes T, Burstein D, Kim YJ. Comparison of delayed gadolinium enhanced MRI of cartilage (dGEMRIC) using inversion recovery and fast T1 mapping sequences. Magn Reson Med. 2008;60:768–73. doi: 10.1002/mrm.21726. [DOI] [PubMed] [Google Scholar]
- 174.Rauscher I, Stahl R, Cheng J, Li X, Huber MB, Luke A, et al. Meniscal measurements of T1rho and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology. 2008;249:591–600. doi: 10.1148/radiol.2492071870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Li W, Du H, Scheidegger R, Wu Y, Prasad PV. Value of pre-contrast T(1) for dGEMRIC of native articular cartilage. J Magn Reson Imaging. 2009;29:494–7. doi: 10.1002/jmri.21658. [DOI] [PubMed] [Google Scholar]
- 176.Choi JW, Chung HW, Ahn JH, Yoon YC. Central hole tear of the discoid meniscus of the knee in magnetic resonance imaging: mimicking the bucket-handle tear. J Comput Assist Tomogr. 2009;33:155–9. doi: 10.1097/RCT.0b013e318166d6a7. [DOI] [PubMed] [Google Scholar]
- 177.Chen YH, Carrino JA, Raman SP, Morrison WB, Fayad LM. Atraumatic lateral collateral ligament complex signal abnormalities by magnetic resonance imaging in patients with osteoarthrosis of the knee. J Comput Assist Tomogr. 2008;32:982–6. doi: 10.1097/RCT.0b013e3181635e39. [DOI] [PubMed] [Google Scholar]
- 178.Boegard TL, Rudling O, Petersson IF, Jonsson K. Magnetic resonance imaging of the knee in chronic knee pain. A 2-year follow-up. Osteoarthritis Cartilage. 2001;9:473–80. doi: 10.1053/joca.2001.0414. [DOI] [PubMed] [Google Scholar]
- 179.Wluka AE, Stuckey S, Snaddon J, Cicuttini FM. The determinants of change in tibial cartilage volume in osteoarthritic knees. Arthritis Rheum. 2002;46:2065–72. doi: 10.1002/art.10460. [DOI] [PubMed] [Google Scholar]
- 180.Cicuttini FM, Forbes A, Yuanyuan W, Rush G, Stuckey SL. Rate of knee cartilage loss after partial meniscectomy. J Rheumatol. 2002;29:1954–6. [PubMed] [Google Scholar]
- 181.Cicuttini F, Wluka A, Wang Y, Stuckey S, Cicuttini F, Wluka A, et al. The determinants of change in patella cartilage volume in osteoarthritic knees. J Rheumatol. 2002;29:2615–9. [PubMed] [Google Scholar]
- 182.Pessis E, Drape JL, Ravaud P, Chevrot A, Dougados M, Ayral X. Assessment of progression in knee osteoarthritis: results of a 1 year study comparing arthroscopy and MRI. Osteoarthritis Cartilage. 2003;11:361–9. doi: 10.1016/s1063-4584(03)00049-9. [DOI] [PubMed] [Google Scholar]
- 183.Cicuttini FM, Wluka AE, Hankin J, Stuckey S. Comparison of patella cartilage volume and radiography in the assessment of longitudinal joint change at the patellofemoral joint. J Rheumatol. 2004;31:1369–72. [PubMed] [Google Scholar]
- 184.Cubukcu D, Ardic F, Karabulut N, Topuz O, Hylan GF. 20 efficacy on articular cartilage quality in patients with knee osteoarthritis: clinical and MRI assessment. Clin Rheumatol. 2005;24:336–41. doi: 10.1007/s10067-004-1043-z. [DOI] [PubMed] [Google Scholar]
- 185.Ozturk C, Atamaz F, Hepguler S, Argin M, Arkun R. The safety and efficacy of intraarticular hyaluronan with/without corticosteroid in knee osteoarthritis: 1-year, single-blind, randomized study. Rheumatol Int. 2006;26:314–9. doi: 10.1007/s00296-005-0584-z. [DOI] [PubMed] [Google Scholar]
- 186.Wang Y, Wluka AE, Cicuttini FM, Wang Y, Wluka AE, Cicuttini FM. The determinants of change in tibial plateau bone area in osteoarthritic knees: a cohort study. Arthritis Res Ther. 2005;7:R687–93. doi: 10.1186/ar1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Garnero P, Peterfy C, Zaim S, Schoenharting M. Bone marrow abnormalities on magnetic resonance imaging are associated with type II collagen degradation in knee osteoarthritis: a three-month longitudinal study. Arthritis Rheum. 2005;52:2822–9. doi: 10.1002/art.21366. [DOI] [PubMed] [Google Scholar]
- 188.Hayes CW, Jamadar DA, Welch GW, Jannausch ML, Lachance LL, Capul DC, et al. Osteoarthritis of the knee: comparison of MR imaging findings with radiographic severity measurements and pain in middle-aged women. Radiology. 2005;237:998–1007. doi: 10.1148/radiol.2373041989. [DOI] [PubMed] [Google Scholar]
- 189.Wang Y, Ebeling PR, Hanna F, O’Sullivan R, Cicuttini FM. Relationship between bone markers and knee cartilage volume in healthy men. J Rheumatol. 2005;32:2200–4. [PubMed] [Google Scholar]
- 190.Bruyere O, Collette J, Kothari M, Zaim S, White D, Genant H, et al. Osteoarthritis, magnetic resonance imaging, and biochemical markers: a one year prospective study. Ann Rheum Dis. 2006;65:1050–4. doi: 10.1136/ard.2005.045914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Brandt KD, Mazzuca SA, Buckwalter KA. Acetaminophen, like conventional NSAIDs, may reduce synovitis in osteoarthritic knees. Rheumatology (Oxford) 2006;45:1389–94. doi: 10.1093/rheumatology/kel100. [DOI] [PubMed] [Google Scholar]
- 192.Wluka AE, Forbes A, Wang Y, Hanna F, Jones G, Cicuttini FM. Knee cartilage loss in symptomatic knee osteoarthritis over 4. 5 years. Arthritis Res Ther. 2006;8:R90. doi: 10.1186/ar1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hunter DJ, LaValley M, Li J, Zhang Y, Bauer D, Nevitt M, et al. Urinary pentosidine does not predict cartilage loss among subjects with symptomatic knee OA: the BOKS Study. Osteoarthritis Cartilage. 2007;15:93–7. doi: 10.1016/j.joca.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 194.Amin S, Niu J, Guermazi A, Grigoryan M, Hunter DJ, Clancy M, et al. Cigarette smoking and the risk for cartilage loss and knee pain in men with knee osteoarthritis. Ann Rheum Dis. 2007;66:18–22. doi: 10.1136/ard.2006.056697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Davies-Tuck ML, Wluka AE, Wang Y, Teichtahl AJ, Jones G, Ding C, et al. The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:337–42. doi: 10.1016/j.joca.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 196.Kornaat PR, Kloppenburg M, Sharma R, Botha-Scheepers SA, Le Graverand MP, Coene LN, et al. Bone marrow edema-like lesions change in volume in the majority of patients with osteoarthritis; associations with clinical features. Eur Radiol. 2007;17:3073–8. doi: 10.1007/s00330-007-0711-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Hunter DJ, Li J, LaValley M, Bauer DC, Nevitt M, DeGroot J, et al. Cartilage markers and their association with cartilage loss on magnetic resonance imaging in knee osteoarthritis: the Boston Osteoarthritis Knee Study. Arthritis Res Ther. 2007;9:R108. doi: 10.1186/ar2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Hernandez-Molina G, Guermazi A, Niu J, Gale D, Goggins J, Amin S, et al. Central bone marrow lesions in symptomatic knee osteoarthritis and their relationship to anterior cruciate ligament tears and cartilage loss. Arthritis Rheum. 2008;58:130–6. doi: 10.1002/art.23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Teichtahl AJ, Wluka AE, Cicuttini FM. Frontal plane knee alignment is associated with a longitudinal reduction in patella cartilage volume in people with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:851–4. doi: 10.1016/j.joca.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 200.Teichtahl AJ, Wang Y, Wluka AE, Szramka M, English DR, Giles GG, et al. The longitudinal relationship between body composition and patella cartilage in healthy adults. Obesity (Silver Spring) 2008;16:421–7. doi: 10.1038/oby.2007.37. [DOI] [PubMed] [Google Scholar]
- 201.Blumenkrantz G, Stahl R, Carballido-Gamio J, Zhao S, Lu Y, Munoz T, et al. The feasibility of characterizing the spatial distribution of cartilage T(2) using texture analysis. Osteoarthritis Cartilage. 2008;16:584–90. doi: 10.1016/j.joca.2007.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Song IH, Althoff CE, Hermann KG, Scheel AK, Knetsch T, Burmester GR, et al. Contrast-enhanced ultrasound in monitoring the efficacy of a bradykinin receptor 2 antagonist in painful knee osteoarthritis compared with MRI. Ann Rheum Dis. 2009;68:75–83. doi: 10.1136/ard.2007.080382. [DOI] [PubMed] [Google Scholar]
- 203.Owman H, Tiderius CJ, Neuman P, Nyquist F, Dahlberg LE. Association between findings on delayed gadolinium-enhanced magnetic resonance imaging of cartilage and future knee osteoarthritis. Arthritis Rheum. 2008;58:1727–30. doi: 10.1002/art.23459. [DOI] [PubMed] [Google Scholar]
- 204.Amin S, Baker K, Niu J, Clancy M, Goggins J, Guermazi A, et al. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis Rheum. 2009;60:189–98. doi: 10.1002/art.24182. [DOI] [PMC free article] [PubMed] [Google Scholar]