Abstract
To address the childhood obesity epidemic, numerous national agencies have outlined specific school policy recommendations for nutrition and physical activity. The extent to which current policies differ by socioeconomic status and geographic location is yet to be determined. This cross-sectional study examined select school nutrition and physical activity policies by markers for poverty among 209 middle and high schools in Utah (82% response rate). The results show that students’ opportunities to establish healthful dietary and physical activity patterns differed by economic circumstances and geographic location. Schools with the highest percentage of free and reduced-price lunch enrollment and schools in rural areas were both less likely to offer a variety of healthful foods outside of the school meal program (ie, competitive foods and drinks) and intramural activities or physical activity clubs. Schools with highest free and reduced-price lunch enrollment were more likely to allow the purchase of unhealthful snacks during lunchtimes than schools with low enrollment (28.4% vs 7.6%, P=0.01). Schools in rural communities were less likely to promote walking and bicycling to school compared with other locations (47.4% rural vs 67.1% urban and 63.6% suburban, P=0.06). Current school policies related to nutrition and physical activity may not be conducive to reducing the childhood overweight problem among children attending schools in areas with increased risk factors due to poverty or rural location in Utah.
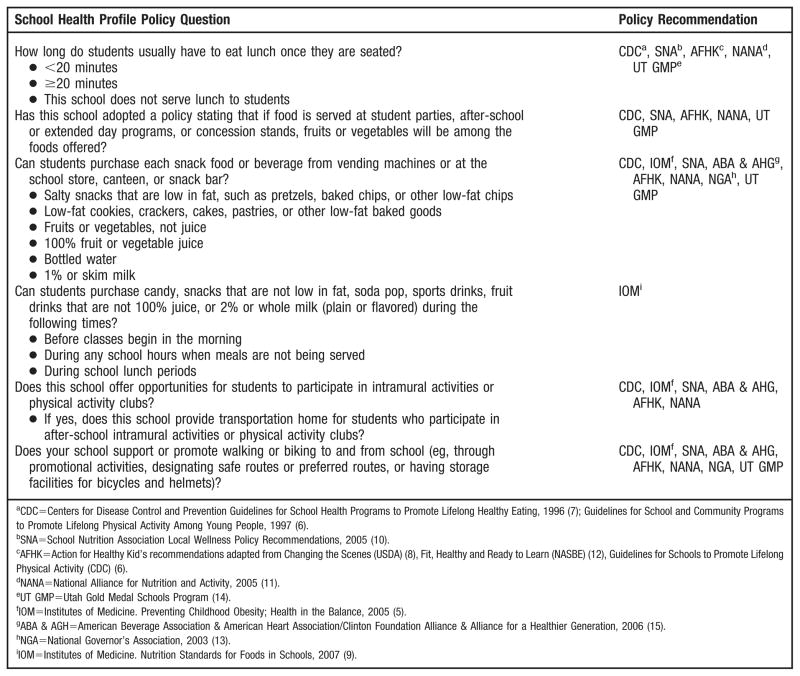
There is widespread consensus among governmental agencies (1), professional associations of dietitians and pediatricians (2,3), and other experts (4,5) that improvements in school nutrition and physical activity policies are needed to address the obesity epidemic among children. Numerous governmental agencies (6–8), federal advisors (9), national (10–13) and local (14) associations, and the food industry (15) have responded to this concern by providing policy recommendations and strategies for schools to embrace. These policy recommendations are based on varying degrees of evidence, but represent the best available to date (5). Examples of the evidence cited include examination of trend data (ie, from 1977 to 2001 the number of children 5 to 15 years of age walking to school decreased from 20.2% to 12.5%) (16), expert panel consensus reports, and outcomes of large-scale school-based trials (ie, Coordinated Approach to Child Health [CATCH]). There is a general consensus among these agencies (Figure) that schools should have policies that ensure that students have access to healthful foods outside of the school meals program, provide adequate time to eat healthful foods with friends, adopt guidelines for foods served as part of school-sponsored events (parties, concession stands, after school), offer intramural activities and physical activity clubs, and promote walking and bicycling to school.
Figure.
Nutrition and Physical Activity Policy Questions from the School Health Profile Questionnaire Utah Data (2006) and Policy Reference.
One recent federal initiative to promote implementation of these and other recommendations is the United States Department of Agriculture (USDA) School Wellness Initiative, which required that school districts participating in federally subsidized child nutrition programs (eg, National School Lunch Program, School Breakfast Program) establish a local wellness policy by school year 2006–2007 (17). To be in compliance, districts must have developed and implemented local policies that include goals for nutrition education, physical activity, and other school-based activities.
Professional organizations agree that all children should have equal access to programs that promote optimal dietary and physical activity habits while at school regardless of socioeconomic status (18,19). However, the extent to which school policies in socioeconomically deprived areas are comparable to policies in areas with fewer socioeconomic challenges is yet to be determined. Previous studies have identified associations between schools serving a higher proportion of children with lower socioeconomic status and increased energy provided by the school lunch (20), overall poorer school meal nutrient profiles (21), and fewer healthful food advertisements at school (ie, salads, fruits, and reduced-fat milk) (22).
The purpose of this cross-sectional study was to review whether select school nutrition and physical activity policies reported by middle and high school principals in Utah’s 2006 School Health Profiles survey differed by economic and geographic indicators at the school-district level (eg, free or reduced-price lunch enrollment, geographic location, and school size). The hypothesis, based on review of the literature, was that districts with higher free and reduced-price lunch enrollment or rurally located schools would have fewer of the recommended nutrition and activity policies in place.
METHODS
Data collected through the 2006 Utah School Health Profiles (Profiles) were used to analyze school nutrition and physical activity policies by free and reduced-price lunch enrollment and geographic location. Profiles is a biennial self-administered mail survey of principals at public schools that include one or more of grades 6 through 12. Profiles data are used to assess school health policies and education related to physical activity, competitive foods, tobacco prevention, violence prevention, and human immunodeficiency virus/acquired immunodeficiency syndrome prevention. Participation is voluntary and confidential. The Centers for Disease Control and Prevention’s Division of Adolescent and School Health at the National Center for Chronic Disease Prevention and Health Promotion oversees methodology, questionnaire development, and analysis of Profiles data (23).
In spring 2006, Profiles questionnaires were mailed to principals of all 256 regular public secondary schools in Utah. Written reminders and follow-up phone calls were used to ensure an adequate response rate (82%). Results were weighted to adjust for differing patterns of nonresponse. The institutional review board at the Utah Department of Health approved Profiles data collection under “public health authority,” and the University of Utah’s institutional review board approved this secondary data analysis.
Data Preparation and Analysis
The Figure identifies the select nutrition and physical activity questions used for analysis. Rural/urban location, percentage of minority enrollment, school size, and free and reduced-price lunch enrollment are not collected as part of the Utah Profiles questionnaire. This information is publicly available, by district and school, on the Utah State Office of Education Web site (24). To maintain confidentiality of the Profiles respondents, categorical demographic indicators were used instead of actual values. For example, district-level free and reduced-price lunch enrollment (range=0% to 72%) was recreated as tertiles and reassigned low (0% to 30%), medium (31% to 44%), and high (45% to 72%) participation values. Free and reduced-price lunch eligibility is established by the federal government and includes children of households living at or below 130% of the poverty level. Geographic location was established at the district level using the Utah State Office of Education designations. These categories have been used elsewhere in conjunction with Utah school districts (25). Although schools were categorized by size, this variable was excluded from the analysis due to a high correlation with location (r=0.78, P<0.01). Due to the low percentage of nonwhite or Hispanic students in most Utah schools, this variable was not analyzed.
Percentages and confidence bounds were calculated for nutrition and physical activity policies by free/reduced-price lunch enrollment and location, and a logit transformation was applied to the confidence limits to produce asymmetric bounds. χ2 tests were used to determine significant differences in policies by low free and reduced-price lunch enrollment and geographic location. Pairwise comparisons between categories and tests of significance were made using linear contrasts of the percentage estimates corresponding to different levels of school lunch enrollment and location. Low free and reduced-price lunch enrollment and urban geographic location served as the referent group for comparisons. All analyses were done using SAS software for Windows (SAS 9.1.3 Service Pack 4, SAS Institute Inc, Cary, NC, 2003).
RESULTS AND DISCUSSION
School Characteristics
A total of 209 principals from public middle, junior, and senior high schools returned Profiles surveys (82% response rate). Of Utah’s 40 school districts, 38 were represented by at least one school. Overall, 46.9% of schools had a low percentage of free or reduced-price lunch enrollment (0% to 30%), 34.0% had a medium percentage (31% to 44%), and 19.1% had a high percentage (45% to 72%). Approximately one third (29.7%) of schools were located in rural areas, 30.1% were located in suburban areas, and 40.2% were located in urban areas. White, non-Hispanic enrollment ranged from 42% to 98% among schools, with a median enrollment of 88%.
School Nutrition Policies
Most schools (88.4%) reported policies allowing students 20 minutes or more to eat lunch once they were seated. Allowing 20 minutes or more to eat lunch occurred more often among schools in rural settings (95.9%) than in urban (84.5%, P=0.02) settings. Only one fifth (20.2%) of schools reported having policies stating that fruits or vegetables are offered at student parties, after-school or extended-day programs, or concession stands. Availability of these policies did not vary by enrollment in free/reduced-price school lunch programs or by location.
Of all healthful snack foods tested through Profiles questions, bottled water (96.5%) and salty low-fat snacks (89.3%) were most likely to be offered for purchase in school vending machines and stores. Less than half of the schools offered fruits or vegetables (39.6%) or 1% or fat-free milk (49.3%) outside of the school lunch and breakfast meals. Most healthful snacks or drinks were more likely to be available in urban schools and schools with low free/reduced-price lunch enrollment compared with in rural schools or high free/reduced-price lunch enrollment schools (Table). Differences in availability of healthful snacks and drinks were significant for salty snacks that are low in fat, low-fat baked goods, and 1% or fat-free milk. Of schools with high free/reduced-price lunch enrollment, only 75.8% offered salty snacks that are low in fat, whereas almost 90% of medium free/reduced-price lunch enrollment schools (86.7%, P= 0.04) and nearly 100% of low free/reduced-price lunch enrollment schools offered this food option (96.7%, P=0.01). Low-fat baked goods were available in only 61.3% of schools with high free/reduced-price lunch enrollment compared with 87.7% (P= 0.01) of low-enrollment schools. Less than one third (30.2%) of schools with high free/reduced-price lunch enrollment offered 1% or fat-free milk, compared with more than half of low-enrollment schools (56.8%, P<0.01).
Table.
School-adopted nutrition and physical activity policies by school district–level free/reduced-price lunch enrollment and location
| Free/Reduced-Price Lunch Enrollment
|
Geographic Location
|
|||||
|---|---|---|---|---|---|---|
| Low | Medium | High | Urban | Suburban | Rural | |
| ←% (confidence interval)→ | ←% (confidence interval)→ | |||||
| Nutrition-related policies | ||||||
| Students have 20 minutes or more to eat lunch. | 86.5 (77.6–92.2) | 90.7 (80.7–95.8) | 88.6 (72.9–95.7) | 84.5 (74.5–91.0) | 85.9 (74.1–92.8) | 95.9** (85.0–99.0) |
| Fruits and vegetables are available at all school sponsored events. | 18.1 (11.3–27.6) | 21.1 (12.8–32.8) | 23.6 (12.2–40.9) | 25.7 (17.1–36.6) | 13.9 (7.0–25.5) | 19.6 (10.8–32.9) |
| Student can purchase from vending machines or at the school store, canteen, or snack bar: | ||||||
| Salty snacks that are low in fat | 96.7 (90.2–98.9) | 86.7* (75.5–93.3) | 75.8* (58.3–87.5) | 94.9 (87.0–98.1) | 96.7 (87.7–99.2) | 73.9** (59.9–84.3) |
| Low-fat baked goods | 87.7 (78.6–92.6) | 77.8 (65.8–86.5) | 61.3* (44.0–76.2) | 79.8 (69.4–87.3) | 89.6 (78.6–95.3) | 67.3 (53.3–78.8) |
| Fruits or vegetables | 43.0 (33.1–53.4) | 38.2 (27.1–50.6) | 34.4 (20.4–51.8) | 40.0 (29.8–51.2) | 40.9 (29.1–54.0) | 37.9 (25.8–51.7) |
| 100% fruit or vegetable juice | 84.1 (75.1–90.2) | 79.1 (67.1–87.5) | 72.1 (54.4–84.8) | 88.6 (79.4–94.0) | 81.7 (69.8–89.7) | 67.1** (53.2–78.5) |
| Bottled water | 97.9 (91.8–99.5) | 97.3 (89.5–99.3) | 91.6 (76.8–97.3) | 96.2 (88.8–98.8) | 100.0 | 93.3 (83.4–97.5) |
| 1% or skim milk (plain or flavored) | 56.8 (46.5–66.6) | 49.9 (38.0–61.8) | 30.2* (17.3–47.3) | 60.0 (48.9–70.2) | 45.5 (33.2–58.3) | 39.0** (26.7–52.7) |
| Students can purchase candy; snacks that are not low in fat; soda, sport drinks, or fruit drinks that are not 100% juice; or 2% or whole milk during school lunch period. | 7.6 (3.7–15.3) | 9.4 (4.2–19.6) | 28.4* (15.8–45.6) | 11.6 (6.1–20.9) | 4.9 (1.6–14.3) | 21.1 (12.0–34.5) |
| Physical Activity–related policies | ||||||
| Intramural activities or physical activity clubs are offered. | 82.4 (73.4–88.8) | 70.8 (58.9–80.4) | 61.8* (45.8–75.6) | 80.5 (70.4–87.7) | 82.7 (71.3–90.2) | 59.0** (46.2–70.6) |
| Transportation for intramural activities or physical activity clubs is offered. | 19.6 (12.1–30.0) | 22.5 (12.9–36.4) | 59.2* (39.2–76.6) | 24.0 (15.2–35.7) | 19.5 (10.8–32.8) | 42.5 (27.6–59.0) |
| Walking or bicycling to and from school is promoted. | 60.4 (50.3–69.6) | 59.9 (48.0–70.8) | 58.6 (42.5–73.0) | 67.1 (56.4–76.3) | 63.6 (50.9–74.6) | 47.7** (35.4–60.3) |
Significantly (P<0.05) different than low free and reduced-price lunch enrollment schools.
Significantly (P<0.05) different than urban schools.
More than one in five schools (22.2%) reported that students could purchase unhealthful snacks before classes. Schools with a high percentage of free/reduced-price lunch enrollment (28.4%) were much more likely to allow the purchase of unhealthful snacks during lunch than schools with low enrollment (7.6%, P=0.01). Rural schools were less likely than urban schools to offer salty snacks that are low in fat, 100% fruit or vegetable juice, and 1% or fat-free milk (Table).
Other studies report differences between food environments at school by socioeconomic circumstances of children. A study among three secondary schools (n=74, children age 11 to 12 years) in England identified that the school with the highest percentage eligible for free school meals was associated with poorer nutrient values from the school lunch menus (21). Conversely, a survey among foodservice professionals in Pennsylvania (n=228) identified that percentage of high school students eligible for free/reduced-price lunches was associated with fewer ala carte sales and increased average daily participation in the school lunch program (26).
One other study reporting on geographic differences found conflicting evidence examining school lunch offerings. A 5-day examination of the school lunch menus in two Mississippi school districts comparing them with the national guidelines revealed that regular school lunch meals from urban school cafeterias provided more energy than meals from the rural school district for kindergarten through grade 12 (mean=1,308 vs 977 calories) (20). Both school districts had a majority of students who qualify for free and reduced-price lunches, and all levels exceeded recommendations for energy, fat, protein, and sodium.
School Physical Activity Policies
Schools with high free/reduced-price lunch enrollment were less likely to have intramural activities or physical activity clubs than were schools with low free/reduced-price lunch enrollment (61.8% vs 82.5%, P=0.04). Similarly, rural schools (59.0%) were less likely to offer opportunities for physical activity than were urban schools (80.5%, P<0.01). Among schools that reported having intramural activities or physical activity clubs, those with a high percentage of free/reduced-price lunch enrollment (59.2%) were more likely to report providing transportation to those activities than were schools with a low percentage of free/reduced-price lunch enrollment (19.6%, P<0.01). More than half of all schools (59.9%) reported supporting or promoting walking or bicycling to and from school, although fewer schools in rural settings (47.7%) reported promoting these activities than did schools in urban settings (67.1%, P=0.02) (Table). Similar to these study results, the Trial of Activity for Adolescent Girls study (a multicenter, group randomized trial in six states) found that participation in the free and reduced-price lunch program was negatively associated with school support for physical activity (27).
The findings in the current study are subject to several limitations. First, these data do not describe student behavior, but show critical issues related to ensuring equal access to opportunities to establish healthful lifestyle patterns in the school setting. Additionally, because this study is based on secondary data analysis, select nutrition- and physical activity–related policies (rather than a comprehensive review) were used to characterize school policies. District-level data instead of school-level data were used for the independent variables. Profiles data were self-reported by school principals and not verified by other sources. Lastly, confidence intervals are large due to small numbers of survey respondents.
CONCLUSIONS
Utah secondary school districts with the highest percentage of free and reduced-price lunch enrollment, as well as Utah rural districts, offered fewer healthful food choices from vending machines and school stores. Schools with high free/reduced-price lunch enrollment had higher access to competitive foods and beverages during lunch-time. Rural schools had fewer opportunities for intramural activities and activity clubs and fewer policies that support walking and bicycling to school. Rural districts also offered fewer unhealthful choices (data not shown).
Nationwide, school-based studies are just beginning to emerge that associate differences in the school food and activity environment by economic circumstances. Research on school environments and their association with behavior are just as sparse. Student self-reported demographic and behavioral data from one middle school in Missouri (n=955) identified ethnicity and economic status as determinants of consumption behaviors. Those eligible for free/reduced-price lunches were 2.6 times more likely (95% confidence interval=1.4 to 4.6) to frequently use the vending machines than were those who were not eligible. However, it is not clear whether these students were buying only unhealthful foods (28). Limited access to healthful foods and physical activity opportunities among schools located in rural locations seems especially important in light of recent studies that have found that the increasing obesity epidemic among children and adolescents disproportionately affects children living in rural areas (29,30). A critical examination of the school food and physical activity environments serving predominantly underserved children and families should be a national priority.
The USDA School Wellness Initiative, a federal mandate requiring school districts to develop local school wellness policies, demonstrates the political will to address the childhood obesity epidemic by promoting healthful eating and activity patterns at school. This initiative is unique in that it offers flexibility to develop policies best suited for each district or school. The extent to which this initiative will impact schools representing children from lower-income families, various geographic locations, and racial and ethnic diversity is yet to be determined.
More recently, an evaluation of the language used in School Board–approved wellness policy documents in Utah suggests that the School Wellness Initiative may have positively impacted schools with the highest free and reduced-price lunch enrollment. Districts with the highest free/reduced-price lunch enrollment had significantly more mandatory (vs recommended) nutrition and activity policies (mean=9.2) than did schools with medium (mean=4.7) and lowest (mean=7.1) participation. Urban school districts were more likely to have mandatory competitive food policies (mean=2.3) than rural (mean=0.93) and suburban (mean=0.83) school districts (25).
School policy improvements in socioeconomically disadvantaged areas are of particular concern because no funding has been provided to implement or evaluate the USDA School Wellness Initiative (31). The findings of this study illustrate an urgent need for a national review of policies adopted as a result of the School Wellness Initiative.
Acknowledgments
This work was funded by the National Cancer Institute (grant no. 1K07 CA114314).
The authors wish to acknowledge the contributions to this manuscript by Karen Nellist, Epidemiologist at Utah Department of Health, and Nancy Brener, PhD, Health Scientist at the Centers for Disease Control and Prevention.
References
- 1.US Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2. Washington, DC: US Government Printing Office; Nov, 2000. [Google Scholar]
- 2.Pilant V. Position of the American Dietetic Association: Local support for nutrition integrity in schools. J Am Diet Assoc. 2006;106:122–133. doi: 10.1016/j.jada.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics. Soft drinks in schools. Pediatrics. 2004;113:152–154. [PubMed] [Google Scholar]
- 4.Nicklas T, Johnson R. Dietary guidance for healthy children aged 2 to 11 years. J Am Diet Assoc. 2004;104:660–677. doi: 10.1016/j.jada.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 5.Koplan J, Liverman C, Kraak V. Preventing Childhood Obesity: Health in the Balance. Washington, DC: National Academy of Sciences; 2005. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Guidelines for school and community programs to promote lifelong physical activity among young people. MMWR Recomm Rep. 1997;46:1–36. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Guidelines for school health programs to promote lifelong healthy eating. MMWR. 1996;45:1–33. [PubMed] [Google Scholar]
- 8.US Department of Agriculture. [Accessed July 3, 2007];Changing the Scene: Improving the School Nutrition Environment. 2000 http://teamnutrition.usda.gov/Resources/changing.html.
- 9.Stallings V, Yaktine A Institutes of Medicine. Leading the Way toward Healthier Youth. Washington, DC: The National Academies Press; 2007. Nutrition Standards for Foods in Schools. [Google Scholar]
- 10.School Nutrition Association. [Accessed July 3, 2007];Local Wellness Policy Recommendations. 2005 :1–11. http://www.schoolnutrition.org/uploadedFiles/SchoolNutrition.org/Child_Nutrition/Local_School_Wellness_Policies/SNALocalWellnessPolicyGuidelinesFinal.pdf.
- 11.National Alliance for Nutrition and Activity. [Accessed July 3, 2007];Model Local School Wellness Policies on Physical Activity and Nutrition. 2005 :1–26. http://www.schoolwellnesspolicies.org/resources/NANAWellnessPolicies.pdf.
- 12.National Association of State Boards of Education. Fit, Healthy and Ready to Learn: A School Healthy Policy Guideline. [Accessed July 3, 2007];Policies to Encourage Physical Activity and Healthy Eating. http://www.nasbe.org/HealthySchools/fithealthy.html.
- 13.VanLandeghem K. National Governors Association. Preventing Obesity in Youth through School-Based Efforts. Center for Best Practices Issue Brief; 2003. [Accessed July 3, 2007]. http://www.nga.org/Files/pdf/022603PREVENTING.pdf. [Google Scholar]
- 14.Utah Department of Health. Gold Medal Schools Program. Program Heart Disease and Stroke Prevention; Salt Lake City: [Accessed July 3, 2007]. http://www.hearthighway.org/gms/index.html. [Google Scholar]
- 15.Alliance for a Healthier Generation. Healthy Schools Program. School Beverage and Competitive Food Guidelines; [Accessed October 9, 2007]. http://www.healthiergeneration.org/default.aspx. [Google Scholar]
- 16.Sturm R. Childhood obesity—What we can learn from existing data on societal trends. Prev Chronic Dis. 2005;2:1–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Child Nutrition and WIC Reauthorization Act. United States Department of Agriculture; 2004. [Accessed July 3, 2007]. Public Law 108–2981. http://www.fns.usda.gov/tn/Healthy/wellnesspolicy.html. [Google Scholar]
- 18.Stang J, Taft B, Flatt M. Position of the American Dietetic Association: Child and adolescent food and nutrition programs. J Am Diet Assoc. 2006;106:1467–1475. doi: 10.1016/j.jada.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 19.Lund J. Appropriate practices for middle school physical education. [Accessed July 3, 2007];A position statement of the National Association for Sports and Physical Education Development by the Middle School and Secondary School Physical Education Council. 2001 http://www.aaheerd.org/NASE/peappropriatepractice/AppropriatePracticesforMS.pdf.
- 20.Addison C, Jenkins B, White M, Young L. Examination of the food and nutrient content of school lunch menus of two school districts in Mississippi. Int J Environ Res Public Health. 2006;3:278–285. doi: 10.3390/ijerph2006030034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gould R, Russell J, Barker M. School lunch menus and 11 to 12 year old children’s food choice in three secondary schools in England—Are the nutritional standards being met? Appetite. 2006;46:86–92. doi: 10.1016/j.appet.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Maher A, Wilson N, Signal L. Advertising and availability of ‘obesogenic’ foods around New Zealand secondary schools: A pilot study. N Z Med J. 2005;118:U1556. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Healthy Youth! Data & Statistics. [Accessed July 3, 2007];School Health Profiles. 2006 http://www.cdc.gov/healthyyouth/profiles/index.htm.
- 24.Utah Department of Education. Utah Education Information Annual Report. Salt Lake City, UT: Utah Department of Education; 2006. [Accessed July 3, 2007]. http://www.schools.utah.gov/schoolinfo.htm. [Google Scholar]
- 25.Metos J, Nanney M. The strength of school wellness policies: One state’s experience. J Sch Health. 2007;77:362–372. doi: 10.1111/j.1746-1561.2007.00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Probart C, McDonnell E, Hartman T, Weirich E, Bailey-Davis L. Factors associated with the offering and sale of competitive foods and school lunch participation. J Am Diet Assoc. 2006;106:242–247. doi: 10.1016/j.jada.2005.10.031. [DOI] [PubMed] [Google Scholar]
- 27.Young D, Felton G, Grieser M, Elder JP, Johnson C, Lee JS, Kubik MY. Policies and opportunities for physical activity in middle school environments. J Sch Health. 2007;77:41–47. doi: 10.1111/j.1746-1561.2007.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finn D, Nanney MS. Risk factors for frequent competitive food consumption at one suburban public middle school. Abstract presented at the American Public Health Association 133rd Annual Meeting; Philadelphia, PA. December 10, 2005. [Google Scholar]
- 29.Miech R, Kumanyika S, Stettler N, Link B, Phelan J, Chang V. Trends in the association of poverty with overweight among US adolescents, 1971–2004. JAMA. 2006;295:2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 30.Tae-Seale T, Chandler C. Rural Healthy People 2010: A companion document to Healthy People 2010. College Station, TX: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Center; 2003. Nutrition and overweight concerns in rural areas: A literature review; pp. 115–130. [Google Scholar]
- 31.Fitzgibbons M, Hayman L, Haire-Joshu D. Childhood obesity: Can policy changes affect this epidemic? [Accessed October 9, 2007];Society for Behavioral Medicine policy brief. 2006 :1–4. http://www.sbm.org/policy/childhood_obesity.asp.