SUMMARY
Aim
To perform a systematic review of the literature on the concurrent validity, predictive validity and responsiveness of radiographic metric measurement of femoro-acetabular joint space width (JSW) in hip osteoarthritis (OA).
Methods
Eligibility criteria: studies reporting any data on (1) JSW on X-rays in hip OA patients and (2) concurrent validity (correlations with clinical symptoms), predictive validity (correlations with future symptomatic state, joint space loss or joint replacement), and/or responsiveness (JSW change over time evaluated using the standardized response mean (SRM)). Search strategy: Medline PUBMED and Embase databases. Statistical analysis: Random-effects models were constructed to obtain pooled SRMs.
Results
Of 448 articles, 79 met the abstract inclusion criteria and were read for further screening. Of these, 15 reported measures of validity and 11 reported measures of responsiveness. Concurrent validity: Five studies suggested an association between JSW and symptoms in the general population. Two evaluated the correlations between JSW and symptoms in hip OA patients, with conflicting results. Five demonstrated that JSW is predictive of future hip joint replacement. Responsiveness was moderate (SRM = 0.66; 95% confidential interval (95%CI): 0.41, 0.91), but tended to be lower in randomized clinical trials than in cohort studies (0.35 vs 0.83), using an intention to treat rather than a completer analysis (0.30 vs 0.80), and using manual rather than computer-based measurement (0.47 vs 1.12).
Conclusion
There is evidence of a weak association between JSW and symptoms, of predictive validity for subsequent joint replacement, and of moderate responsiveness of metric measurement of JSW.
Keywords: Hip osteoarthritis, Joint space metric measurement, X-rays, Concurrent validity, Predictive validity, Responsiveness
Osteoarthritis (OA) is a major cause of disability worldwide. For many years, there has been a major interest among the scientific community, pharmaceutical companies, and regulatory agencies in the development of drugs that might influence the natural history of OA by preventing, retarding, or reversing cartilage breakdown. These disease-modifying OA drugs (DMOADs) need to be evaluated in trials using outcomes measures that reflect the natural history of OA. Radiographic variables, particularly metric measurement of minimal joint space width (JSW), are considered the most appropriate structural outcome measure1. However, the clinical relevance of this outcome remains doubtful, since there is a debate on whether an association with clinical symptoms exists. Moreover, the responsiveness is questionable since the progression of disease is frequently slow and variable from one patient to another.
Recently, international working groups were created under the auspices of the Food and Drug Administration (FDA) and the Osteoarthritis Research Society International (OARSI) in order to revisit and discuss the outcomes used in OA trials; one of these groups examined the assessment of structural change (ASC). The members of this group agreed that the first stage of their work was to assess the current knowledge on the properties of the instruments used to evaluate structural variables in OA. To assess a potential outcome measure, it is necessary to assess its psychometric properties, as defined by the Outcome Measures in Rheumatology Clinical Trials (OMERACT) filter2. The OMERACT filter checks that a potential outcome measure is truthful, reliable, and sensitive to change over time and between different severity stages. This report presents a systematic analysis of the literature performed on the concurrent validity, predictive validity and responsiveness of radiographic metric measurement of hip JSW in hip OA.
Methods
The draft strategy for the literature review was written in December 2008, sent to all members of the ASC working group, underwent iterative revision, and a final version of the protocol was approved in February 2009. The protocol is available and can be obtained from the corresponding author of the present article.
Eligibility criteria
Studies were eligible for analysis when reporting data on hip OA patients (regardless of the definition employed) and including
metric measurement of the hip joint JSW on X-rays, irrespective of the measurement technique (manually or computer-based method, evaluation of minimal, mean joint space, or joint area), the study design (cross-sectional or longitudinal), the presence of an intervention or not, or the presence of controls
concurrent validity of JSW (correlations with clinical symptoms, in particular pain and function) and/or predictive validity (correlation with future symptoms, joint space loss, or joint replacement), and/or responsiveness (JSW change over time) using either the reported standardized response mean (SRM) or where data allowing calculation of the SRM was available.
Search strategy
A systematic search of the literature was performed in March 2009 and updated in July 2009, using the Medline PUBMED and the Embase databases. The following search terms were used: ((Osteoarthritis[MeSH]) and (hip)) AND (X-ray OR radiography OR diagnostic imaging OR radiology OR disease progression) AND (joint space OR JSW OR disease progression). We limited the search to research conducted in humans and published in English, French, German or Spanish languages.
A quality control of the search terms was performed in January 2009: 30 relevant articles were selected at random from one investigator’s personal library. All were found to include the search terms. In addition, a manual search of the references of all screened full-text articles was performed. The abstracts of all potential relevant citations referenced were also screened.
Screening and extraction
All abstracts were read by one reviewer (JFM). Full-text articles were obtained if likely to be relevant or where relevance could not be determined from the abstract.
Criteria for exclusion were: studies reporting results on OA joints other than hip, or combined results on hip and other joint OA which did not present hip results separately, no radiographic evaluation or radiographic data not reported, radiographic assessment not evaluated by metric measurement of JSW (thus excluding studies in which joint space was evaluated using an atlas), secondary OA, and case reports. Reviews, editorials, comments, and systematic literature reviews were not included.
A full-text review of the articles was performed by one reviewer (DCML) using a predetermined data abstraction form approved by the ASC group. The data extracted included the year of publication, name of the first author, study design, X-ray acquisition and measurement technique, evaluated population or patients, demographics, baseline and when available follow-up clinical status (pain, function), baseline and when available follow-up JSW metric measurement, change in JSW (mean and standard deviation), SRM, cross-sectional and longitudinal relationship between JSW metric measurement and clinical status, relationship between JSW and further joint space loss and/or total joint replacement.
After data extraction, a second reviewer (JFM) read all the articles to ensure quality control of data extraction.
Statistical analysis
Responsiveness was assessed by the SRM, defined as the mean change in minimum JSW divided by the standard deviation of change. Articles reporting the SRM or its components were included in the analysis. For randomized clinical trials (RCTs), only the placebo arm was entered to ensure a measure of the natural history of disease progression. Pooled estimates of the SRM were performed using random-effects models. We calculated the overall pooled SRM along with the pooled SRM by study design (cohort vs RCT), analysis type (intention to treat (ITT) vs completers), and measurement method (computer vs manual).
Results
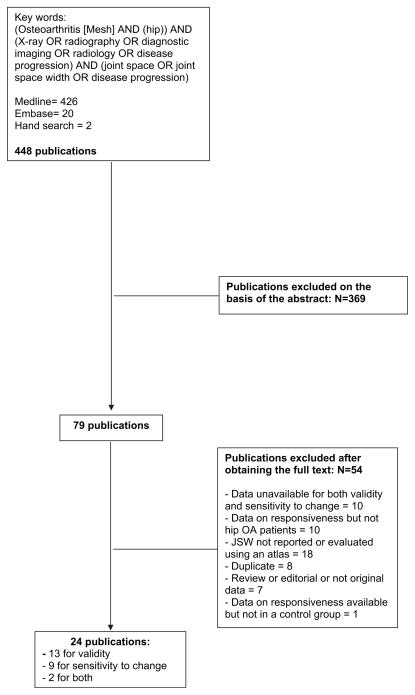
We identified 448 articles. Seventy-nine (18%) articles met the initial inclusion criteria and were read for further screening. Of these, 15 (19%) articles reported validity results and 11 (14%) articles reported responsiveness results (Fig. 1).
Fig. 1.
Flow-chart of the screening process for articles included in the systematic review.
Concurrent validity
Cross-sectional relationship between JSW and symptoms
Five studies evaluated the correlation between JSW and symptoms in the general population (Table I). In a population-based study (3595 participants), the presence of hip pain, of moderate and severe disability and, to a lesser extent, stiffness, were associated with minimal JSW3. In another population-based study (3208 participants), a minimal JSW ≤ 2 mm was significantly associated with self-reported pain in or around the hip joint during the previous 12 months4. In 735 participants from the Johnston County Osteoarthritis Project, who had JSW measured at the first follow-up, categorized minimal JSW was not related to pain, but a minimal JSW < 2.5 mm was associated with functional impairment5. In a sample of 195 patients presenting with new episodes of pain, there was a negative correlation between JSW and duration of hip pain6. In a sample of 220 patients consulting for hip pain, pain duration ≥ 3 months was associated with a minimal JSW ≤ 2.5 mm7. In 759 men aged 60–75 years, the prevalence of hip pain was associated with a reduced minimal JSW8.
Table I.
Concurrent validity: correlations between symptoms and hip joint space metric measurement (JSW) in the general population and in patients with hip pain
| First author (reference) | Design | Number of subjects/patients | Mean age: yrs (SD) and % males | Type of JSW | Results |
|---|---|---|---|---|---|
| Reijman3 | Community-based cohort, cross-sectional | 3595 subjects aged ≥55 years | 66.0 ± 6.9 years, 41.8% | Minimal JSW 7.5% participants with minimal JSW ≤ 2.5 mm, 3.0% with minimal JSW ≤ 2.0 mm, 1.4% with minimal JSW ≤ 1.5 mm | Hip pain associated with minimal JSW ≤ 2.5 mm (OR = 2.4, 95%CI = 1.7–3.4), ≤2.0 mm (OR = 4.5, 95%CI = 2.9–7.0) and ≤1.5 mm (OR = 6.6, 95%CI = 3.6–12.2) Moderate disability associated with minimal JSW ≤2.5 mm (OR = 2.7, 95%CI = 2.0–3.7), ≤2.0 mm (OR = 3.7, 95%CI = 2.4–5.9) and ≤1.5 mm (OR = 5.3, 95%CI = 2.9–9.8) Severe disability associated with minimal JSW ≤ 2.5 mm (OR = 3.0, 95%CI = 2.0–4.4), ≤2.0 mm (OR = 4.1, 95%CI = 2.5–7.0) and ≤1.5 mm (OR = 6.1, 95%CI = 3.1–12.1) |
| Jacobsen4 | Community-based, cross-sectional | 3208 | Men: 62.5 (NA) Women: 65.0 (NA), 37.8% | Minimal JSW, 6.0% men and 5.7% women with minimal JSW ≤ 2.0 mm | MJSW ≥ 2 mm significantly associated to self-reported hip pain (OR = 3.5, 95%CI = 2.1–5.7 in men; 1.7, 95%CI = 1.1–2.5 in females), groin pain (OR = 2.3, 95%CI = 1.3–4.1 in men; 2.0, 95%CI = 1.3–3.2 in females), and thigh pain (OR = 1.9, 95%CI = 1.1–3.3 in men; 1.5, 95%CI = 1.0–2.3 in females) during the previous 12 months |
| Gossec5 | Subjects from a community-based cohort, cross-sectional | 735 | 67.2 (9.5), 34.3% | Categorical minimal JSW | JSW not related to pain, JSW < 2.5 mm associated with functional impairment, categorized in quartiles (OR = 1.67, 95%CI = 1.0–2.78 compared to JSW > 3 mm) |
| Birell6 | Cross-sectional, patients with new episode of hip pain in primary care | 195 | Median age = 63, 33.3% | Dichotomized minimal JSW, cut off: ≤2.5 mm or 1.5 mm | Pain duration associated with JSW Pain duration < 3 months, 28% with JSW ≤ 2.5 and 7% with JSW ≤ 1.5 mm; Pain duration = 3–12 months, 25% with JSW ≤ 2.5 and 13% with JSW ≤ 1.5 mm; Pain duration > 12 months, 43% with JSW ≤ 2.5 mm and 26% with JSW ≤ 1.5 mm, P = 0.02 |
| Bierma-Zienstra7 | Descriptive, cross-sectional | 220 | 66 (9.6), 27% | Dichotomized minimal JSW, ≤ 2.5 mm and ≤ 1.5 mm | JSW ≤ 2.5 mm correlated with pain duration ≥ 3 months (OR = 2.34, 95%CI = 1.26–4.32) and with morning stiffness (OR = 2.0, 95% CI = 1.15–3.62) JSW ≤ 1.5 mm correlated with morning stiffness (OR = 2.6, 95%CI = 1.12–6.06) |
| Croft8 | Cross-sectional, men who underwent intravenous urogram | 759 | Age between 60 and 75 years | Minimal JSW | Pain in 20.4% of hips, 28.3% of hips with JSW ≤ 2.5 mm, and in 56% of hips with JSW ≤ 1.5 mm |
OR: Odds Ratio.
95%CI: 95% Confidential Interval.
mm: millimetre.
There were very few data on the relationship between JSW and symptoms in hip OA patients (Table II). In a sample of 41 hip OA patients, the functional impairment correlated with minimal and sum JSW, in the operated and the contralateral hips9. Beside the participants from the Johnston County Osteoarthritis Project, Ref. 5 also provided data from patients included in a 3-year RCT. The baseline clinical parameters explained only 0.4% of the variability of the baseline minimal JSW (P = 0.44).10 In the same sample, categorical JSW was not related to pain nor functional impairment5.
Table II.
Concurrent validity: cross-sectional and longitudinal correlations between symptoms and JSW metric measurement in hip OA patients
| Reference | Design | Number of patients | Age, years, mean (SD) and % males | Type of JSW | Results |
|---|---|---|---|---|---|
| Amaro9 | Descriptive, cross-sectional Hip OA patients prior to joint replacement | 41 | 68.4 (9.4), 41% | JSW continuous: minimal and sum (lateral + superior + axial) JSW | Lequesne’s index correlated with minimal JSW, r = −0.57, P < 0.05 for operated hip and r = −0.70, P < 0.05 for non-operated hip Lequesne’s index correlated with sum JSW, r = −0.63, P < 0.05 for operated hip and r = −0.71, P < 0.05 for non-operated hip |
| Dougados10 | RCT, cross-sectional and 1-year follow-up | 458 | 63.0 (7.0), 40.4% | JSW continuous: dichotomized change in minimal JSW (≥0.6 mm or not) | Baseline clinical parameters explained only 0.4% of the variability of the baseline JSW (P = 0.44) Baseline Lequesne’s index > 10 related to 12 months changes in JSW ≤ 0.6 mm (OR = 2.66, 95%CI = 1.46–4.83, P < 0.0001) |
| Gossec5 | Same RCT as above, cross-sectional | 507 | 63.0 (7.0), 40.4% | Categorical minimal JSW, cut-offs of 1.5, 2.5, and 3.0 mm | JSW not related to pain or functional impairment |
| Lane11 | Cohort of women with fractures, aged over 65 years 8-year follow-up |
745 | 71.8 (5.2), 0% | Change in minimal JSW, continuous and dichotomized (> or ≤0.5 mm) | Mean decrease in JSW = 0.5 ± 0.63 and 0.35 ± 0.55 mm in hips with and without baseline pain, respectively (P = 0.034) Decrease ≥ 0.5 mm: 53.7% and 30.7% of hips with and without baseline pain, respectively OR = 1.9, 95%CI = 1.4–2.6, P < 0.001) |
OR: Odds Ratio.
95%CI: 95% Confidential Interval.
mm: millimetre.
Longitudinal relationship between JSW and symptoms (Table II)
We did not find any studies that evaluated the relationship between change in symptoms and change in JSW. Two studies evaluated the relationship between baseline symptoms and subsequent joint space loss. In 458 patients included in a 3-year RCT, baseline Lequesne’s index > 10 was an independent predictor of subsequent 1-year change in minimal JSW ≥ 0.6 mm10. In a study of 745 women aged over 65 with radiographic hip OA (936 hips), the joint space loss during follow-up was increased in subjects with baseline hip pain11.
Predictive validity
Prediction of future joint space loss (Table III)
Table III.
Predictive validity: correlations between JSW metric measurement and future joint space loss in hip OA patients
| Reference | Design and follow-up | Number of patients | Age, years, mean (SD) and % males | Type of JSW | Results |
|---|---|---|---|---|---|
| Conrozier12 | Retrospective study from a case registry of patients who had undergone THR for OA, mean radiological follow-up of 81.2 ± 59.9 months | 61 patients, 69 hips | Men: 62.0 (10.4) Women: 61.8 (10.4), 44.2% |
JSW continuous: mean JSW | The mean JSW at entry was not related to further annual joint space loss |
| Dougados10 | 3-year RCT | 458 | 63 (7), 40.4% | JSW continuous | Baseline JSW < 2.0 mm was an independent predictor of a further 0–1 year radiological progression, defined as a 1-year JSW loss of at least 0.6 mm (OR = 2.11, 95% CI = 1.30–3.44) |
OR: Odds Ratio.
95%CI: 95% Confidential Interval.
mm: millimetre.
In a retrospective study of 69 patients with hip OA who had undergone total hip replacement (THR), the mean of mean JSW at entry was not related to subsequent annual joint space loss (mean follow-up = 81.2 ± 59.9 months)12. In 458 patients included in a 3-year RCT, a baseline minimal JSW < 2.0 mm was an independent predictor of 12 month radiological progression10.
Prediction of future joint space loss or future joint replacement
In a prospective cohort (mean follow-up = 6.6 ± 0.5 years), a baseline minimal JSW ≤ 2.5 mm was a predictor of a joint space loss ≥ 1.0 mm or a THR on a multivariate analysis performed on all included subjects, but was not on an analysis restricted to the 411 patients with hip pain at baseline13.
Prediction of total hip joint replacement (Table IV)
Table IV.
Predictive validity: correlation between hip joint space metric measurement (JSW) and future THR
| Reference | Design and follow-up | Number of subjects/patients | Age, years, mean (SD) and % males | Type of JSW | Results |
|---|---|---|---|---|---|
| Reijman3 | Community-based cohort, mean follow-up = 6.6 ± 0.5 years | 3561 | 67.1 (7.98) | Mean JSW | Baseline JSW ≤ 2.5 mm predicts future THR OR right hip = 18.6, 95%CI = 10.7–32.3 OR left hip = 22.6, 95%CI = 11.8–43.0 |
| Birrell14 | Cohort of patients with a new episode of hip pain recruited by GPs, median duration follow-up = 36 months | 195 | 63 (11), 32% | Minimal JSW | JSW predictive of future THR In a 0–6 composite score for prediction of THR, the weight of JSW is 2 (joint space > 2.5 = 0, JSW 1.5–2.5 = 1, joint space < 1.5 = 2) |
| Lievense15 | Patients aged >50 years with hip pain, followed-up for a mean 2.7 ± 0.25 years then 5.8 ± 0.3 years | 193 (mean follow-up 2.7 years) and 163 subjects (mean follow-up = 5.8 years) | 65.6 (9.6), 26.9% | Minimal JSW | Baseline JSW < 2.5 mm predictor of future THR on univariate (OR for future 3 years THR = 6.6, P < 0.01; OR for future 6 years THR = 7.1, P < 0.01), but not on multivariate analysis |
| Dougados16 | 3-year RCT | 506 | Minimal JSW: 1-year change in JSW categorized in four grades (no change, worsening < 25%, worsening between 25% and 50%, worsening > 50%) | Baseline JSW < 2 mm associated with a THR during the 3 following years (relative risk = 1.85, 95%CI = 1.18–2.90) First year change in JSW associated with THR during the 2 following years, relative risk of being operated = 2.89; P < 0.01 (grade 1 vs 2); 2.09, P = 0.07 (grade 2 vs 3); and 5.3, P < 0.0001 (grade 3 vs 4) |
|
| Maillefert17 | 3-year RCT + 2 years of additional follow-up after end of the trial | 422 (first analysis) and 384 (second analysis) | 63.0 (6.8), 41.7% (first analysis) and 43.7% (second analysis) | Minimal JSW | A 1-year decrease in JSW ≥ 0.2 mm or 15% predicted THR during the next 4 years (sensibility and specificity of 75% and 68%; 74% and 78%, respectively) Similar results for 0–2 years changes in JSW |
OR: Odds Ratio.
95%CI: 95% Confidential Interval.
mm: millimetre.
A relationship between baseline JSW and later hip replacement was observed in five studies (two of them evaluating the same sample). In a population-based study, a minimal JSW ≤ 2.5 mm was associated with subsequent THR (mean follow-up = 6.6 ± 0.5 years)3. In a cohort of 195 patients with a new episode of hip pain, the baseline minimal JSW was predictive of being put on a waiting list for joint replacement (median duration follow-up = 36 months)14. In a cohort of 224 subjects aged > 50 years with hip pain followed-up for a mean 2.7 ± 0.25 years then 5.8 ± 0.3 years, a baseline joint space < 2.5 mm was predictive of future joint replacement on unadjusted analysis15. In 506 patients included in a 3-year RCT, a baseline minimal JSW < 2 mm and the first year change in minimal JSW were associated with THR during the 2-year follow-up16. Patients included in the same RCT were followed-up for an additional 2 years. A decrease of minimal JSW of at least 0.2 mm during the first year predicted joint replacement during the 4 following years and a decrease of minimal JSW of at least 0.4 mm during the first two years predicted joint replacement during the 3 following years17.
Responsiveness
Data on minimal JSW were extracted from 11 articles (seven cohorts, four RCTs)11,12,18–26. Structural assessment analysis was performed as an ITT analysis in three RCTs, and as a completer analysis in the last RCT and in the cohorts. The assessment of minimal JSW was performed using a manual technique in four studies, and a computer-based technique in seven. The mean sample size was 164. Results are shown in Table V. The overall SRM was 0.66 (95% confidential interval (95%CI) = 0.41–0.91). The responsiveness tended to be higher in cohorts (SRM = 0.83; 95%CI: 0.49, 1.16) than in RCTs (SRM = 0.35; 95%CI: 0.12, 0.57). Responsiveness was also higher in analyses of completers (SRM = 0.80; 95%CI: 0.50, 1.10) compared to ITT analyses (SRM = 0.30; 95%CI: 0.06, 0.55). Responsiveness varied by method of measurement, with greater responsiveness seen in studies using computer-based measurement (SRM = 1.12; 95%CI: 0.64, 1.59) compared to manual measurement (SRM = 0.47; 95%CI: 0.31, 0.62).
Table V.
Summary of hip responsiveness from radiographs using random-effects pooling of the SRM of the minimum JSW
| Analysis | Number of studies | Mean sample size | SRM | 95% Confidence Interval |
|---|---|---|---|---|
| Overall | 11 | 164 | 0.66 | 0.41, 0.91 |
| Study design | ||||
| RCT | 4 | 111 | 0.35 | 0.12, 0.57 |
| Cohort | 7 | 194 | 0.83 | 0.49, 1.16 |
| Analysis | ||||
| Completers | 8 | 176 | 0.80 | 0.50, 1.10 |
| ITT | 3 | 132 | 0.30 | 0.06, 0.55 |
| Measurement technique | ||||
| Computer | 4 | 40 | 1.12 | 0.64, 1.59 |
| Manual | 7 | 234 | 0.47 | 0.31, 0.62 |
The data on mean JSW and joint space area were too sparse to allow any pooled analysis. Some studies suggested responsiveness to be comparable to that observed for minimal JSW12,18,20,27.
Discussion
The present study focused on metric measurement of JSW since it is currently the most frequently used method evaluating structural changes on X-rays in clinical trials21,22,25,26 and has been demonstrated to be more responsive than other methods, such as the Kellgren and Lawrence or the OARSI grading systems5. The main limitation is the heterogeneity of the included studies in their design, inclusion and exclusion criteria, sample size, outcomes.
The results suggest that, in the general population as well as in the subjects with hip pain, there is an association between minimal JSW and the presence of hip symptoms. Surprisingly, the relationship between JSW and symptoms has rarely been evaluated in hip OA patients. In this review, the results of cross-sectional correlations were too sparse and heterogeneous to allow any conclusion, while longitudinal studies suggested that baseline joint symptoms are moderately correlated to subsequent joint space loss.
Several factors must be taken into account when interpreting these results. First, joint pain is influenced by numerous factors, including patient-related factors. A recent study showed that the relationship between pain and joint space (non-metric measurement) is increased when the patients are their own controls, at least for the knee28. It would be interesting to conduct such a study, using JSW metric measurement, in hip OA patients. Second, OA is symptomatically a disease with fluctuating symptoms, which makes it difficult to interpret the correlations between structural data and symptomatic data obtained at only one point in time. Again, additional studies evaluating the relationship between JSW and symptoms obtained at several points of time would be of interest. Third, most studies did not adjust for analgesic and non-steroidal anti-inflammatory drug consumption when evaluating the association between JSW and symptoms. This might alter the associations, at least with respect to pain.
Taken together, the results of this analysis suggest that there is some evidence of a weak association between JSW and symptoms in hip OA. However, additional studies are needed to clarify the association.
Results on predictive validity suggest that absolute levels of JSW might be predictive of later joint space loss, though these data are heterogeneous; there is more data to suggest that loss of JSW is predictive of subsequent THR. One can question the relevance of joint replacement as an end-point to evaluate the validity of JSW. While arthroplasty is usually performed in patients with advanced symptomatic and structural disease, surgeons have reported that they are weakly or moderately influenced by X-rays when deciding whether joint replacement is indicated or not29,30. It has also been shown that in clinical practice, JSW is a major predictive factor of the decision to perform hip replacement31. Thus, JSW and joint replacement might not be truly independent. However, the reasons why JSW influences the surgeons’ decision remain unclear. If these reasons are differential diagnosis (some surgeons might consider that pain and functional impairment are certainly due to OA in patients with severe joint space narrowing, but might be due, at least in part, to another disease in those with mild joint space narrowing), optional treatments (the surgeons might consider that an additional or complementary medical treatment is less likely to be efficient in patients with severe joint narrowing), and/or disease’s potential evolution (surgeons might consider that a spontaneous clinical improvement is less likely to be observed in patients with severe joint loss), joint replacement might be considered as a valid outcome.
The present results suggest good evidence for a moderate responsiveness of JSW in hip OA. It must be pointed out however that the responsiveness tended to be lower in RCTs than in cohort studies, and lower using an ITT rather than a completer analysis (which might explain the higher responsiveness in cohort studies). Potential DMOADs are evaluated using RCTs and an ITT analysis, so the responsiveness of JSW in such studies should be considered as mild, rather than moderate.
Acknowledgments
Acknowledgements to the other members of the OARSI/FDA ASC group: B Dardzinski, D Dreher, J Duryea, F Eckstein, D Felson, G Gold, A Guermazi, MP Hellio Le Graverand-Gastineau, J Huckle, D Hunter, H Keen, S Kingsbury, J Kraines, G Lester, R Maciewicz, S Mazzuca, E Morris, T Mosher, JP Pelletier, H Potter, MA Preston, J Randle, L Rovati, E Schneider, B Story, S Totterman, W Tsuji and M Wahba.
Footnotes
Author contributions
Delphine Chu Miow Lin: conception and design, data extraction and analysis, redaction of the manuscript.
William Reichmann: conception and design, statistical analysis, data analysis, redaction of the manuscript.
Laure Gossec: conception and design, data extraction, redaction of the manuscript.
Elena Losina: conception and design, statistical analysis, data analysis, redaction of the manuscript.
Philip Conaghan: conception and design, data analysis, redaction of the manuscript.
Jean Francis Maillefert: conception and design, data extraction and analysis, redaction of the manuscript.
Conflict of interest
The authors do not have any conflict of interest to declare.
Declaration of funding and role of funding source
The OARSI FDA OA Initiative received financial support from the following professional organization: American College of Rheumatology.
Additionally the OARSI FDA OA Initiative received financial support from the following companies: Amgen, ArthroLab, Astra-Zeneca, Bayer Healthcare, Chondrometrics, CombinatoRx, Cypress BioScience, DePuy Mitek, Expanscience, 4QImaging, Genevrier/IBSA, Genzyme, King (Alpharma), Merck, Merck Serono, NicOx, Pfizer, Rottapharm, Smith & Nephew and Wyeth.
While individuals from pharmaceutical, biotechnology and device companies actively participated in on-going working group discussions, due to the conflict of interest policy enacted by OARSI, these individuals were not allowed to vote on the final recommendations made by OARSI to the FDA.
References
- 1.FDA. Clinical Development Programs for Drugs, Devices and Biological Products Intended for the Treatment of OA. FDA; 1999. [Google Scholar]
- 2.Boers M, Brooks P, Strand CV, Tugwell P. The OMERACT filter for outcome measures in rheumatology. J Rheumatol. 1998;25:198–9. [PubMed] [Google Scholar]
- 3.Reijman M, Hazes JM, Pols HA, Bernsen RM, Koes BW, Bierma-Zeinstra SM. Validity and reliability of three definitions of hip osteoarthritis: cross sectional and longitudinal approach. Ann Rheum Dis. 2004;63:1427–33. doi: 10.1136/ard.2003.016477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. The relationship of hip joint space to self reported hip pain. A survey of 4. 151 subjects of the Copenhagen city heart study: the osteoarthritis substudy. Osteoarthritis Cartilage. 2004;12:692–7. doi: 10.1016/j.joca.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Gossec L, Jordan JM, Lam MA, Fang FF, Renner JB, Davis A, et al. Comparative evaluation of 3 semi-quantitative radiographic grading techniques for hip osteoarthritis in terms of validity and reproducibility in 1404 radiographs: report of the OARSI-OMERACT task force. Osteoarthritis Cartilage. 2009;17:182–7. doi: 10.1016/j.joca.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane GL, Silman A. Radiographic change is common in new presenters in primary care with hip pain. PCR Hip Study Group. Rheumatology. 2000;39:772–5. doi: 10.1093/rheumatology/39.7.772. [DOI] [PubMed] [Google Scholar]
- 7.Bierma-Zeinstra SMA, Oster JD, Bernsen RMD, Verhaar JAN, Ginai AZ, Bohnen AM. Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care. J Rheumatol. 2002;29:1713–8. [PubMed] [Google Scholar]
- 8.Croft P, Cooper C, Wickham C, Coggen D. Defining osteoarthritis of the hip for epidemiologic studies. Am J Epidemiol. 1990;132:514–22. doi: 10.1093/oxfordjournals.aje.a115687. [DOI] [PubMed] [Google Scholar]
- 9.Amaro A, Amado F, Duarte JA, Appell HJ. Gluteus medius muscle atrophy is related to contralateral and ipsilateral hip joint osteoarthritis. Int J Sports Med. 2007;28:1035–9. doi: 10.1055/s-2007-965078. [DOI] [PubMed] [Google Scholar]
- 10.Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, et al. Radiological progression of hip osteoarthritis: definition, risk factors and correlations with clinical status. Ann Rheum Dis. 1996;55:356–62. doi: 10.1136/ard.55.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lane NE, Nevitt MC, Hochberg MC, Hung YY, Palermo L. Progression of radiographic hip osteoarthritis over eight years in a community sample of elderly white women. Arthritis Rheum. 2004;50:1477–86. doi: 10.1002/art.20213. [DOI] [PubMed] [Google Scholar]
- 12.Conrozier T, Jousseaume CA, Mathieu P, Tron AM, Caton J, Bejui J, et al. Quantitative measurement of joint space narrowing progression in hip osteoarthritis: a longitudinal retrospective study of patients treated by total hip arthroplasty. Br J Rheumatol. 1998;37:961–8. doi: 10.1093/rheumatology/37.9.961. [DOI] [PubMed] [Google Scholar]
- 13.Reijman M, Hazes JM, Pols HA, Bernsen RM, Koes BW, Bierma-Zeinstra SM. Role of radiography in predicting progression of osteoarthritis of the hip: prospective cohort study. BMJ. 2005;330:1183. doi: 10.1136/bmj.38442.457488.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Birrell F, Afzal C, Nahit E, Lunt M, Macfarlane GJ, Cooper C, et al. Predictors of hip joint replacement in new attenders in primary care with hip pain. Br J Gen Pract. 2003;53:26–30. [PMC free article] [PubMed] [Google Scholar]
- 15.Lievense AM, Koes BW, Verhaar JA, Bohnen AM, Bierma-Zeinstra SM. Prognosis of hip pain in general practice: a prospective followup study. Arthritis Rheum. 2007;57:1368–74. doi: 10.1002/art.23094. [DOI] [PubMed] [Google Scholar]
- 16.Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, et al. Requirement for total hip arthroplasty: an outcome measure of hip osteoarthritis? J Rheumatol. 1999;26:855–61. [PubMed] [Google Scholar]
- 17.Maillefert JF, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, et al. Relevant change in radiological progression in patients with hip osteoarthritis. I. Determination using predictive validity for total hip arthroplasty. Rheumatology. 2002;41:142–7. doi: 10.1093/rheumatology/41.2.142. [DOI] [PubMed] [Google Scholar]
- 18.Chevalier X, Conrozier T, Gehrmann M, Claudepierre P, Mathieu P, Unger S, et al. Tissue inhibitor of metalloprotease-1 (TIMP-1) serum level may predict progression of hip osteoarthritis. Osteoarthritis Cartilage. 2001;9:300–7. doi: 10.1053/joca.2000.0389. [DOI] [PubMed] [Google Scholar]
- 19.Conrozier T, Saxne T, Shan Sei Fan C, Mathieu P, Tron AM, Heinegard D, et al. Serum concentration of cartilage oligomeric matrix protein and bone sialoprotein in hip osteoarthritis: a one year prospective study. Ann Rheum Dis. 1998;57:527–32. doi: 10.1136/ard.57.9.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dougados M, Villers C, Amor B. Sensitivity to change of various roentgenological severity scoring systems for osteoarthritis of the hip. Rev Rhum. 1995;62:169–73. [PubMed] [Google Scholar]
- 21.Dougados M, Nguyen M, Berdah L, Mazieres B, Vignon E, Lequesne M. Evaluation of the structure-modifying effects of diacerein in hip osteoarthritis. Arthritis Rheum. 2001;44:2539–47. doi: 10.1002/1529-0131(200111)44:11<2539::aid-art434>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 22.Lequesne M, Maheu E, Cadet C, Dreiser RL. Structural effect of avocado/soybean unsaponifiables on joint space loss in osteoarthritis of the hip. Arthritis Care Res. 2002;47:50–8. doi: 10.1002/art1.10239. [DOI] [PubMed] [Google Scholar]
- 23.Maheu E, Cadet C, Marty M, Dougados M, Ghabri S, Kerloch I, et al. Reproducibility and sensitivity to change of various methods to measure joint space width in osteoarthritis of the hip: a double reading of three different radiographic views taken with a three-year interval. Arthritis Res Ther. 2005;7:R1375–85. doi: 10.1186/ar1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papacoulas CD, Ward RJ, Tonkin CJ, Buckland-Wright C. Cancellous bone changes in hip osteoarthritis: a short-term longitudinal study using fractal signature analysis. Osteoarthritis Cartilage. 2005;13:998–1003. doi: 10.1016/j.joca.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Pavelka K, Gatterova J, Gollerova V, Urbanova Z, Sedlackova M, Altman RD. A 5-year randomized controlled, double-blind study of glycosaminoglycan polysulphuric acid complex (Rumalon®) as a structure modifying therapy in osteoarthritis of the hip and knee. Osteoarthritis Cartilage. 2000;8:335–42. doi: 10.1053/joca.1999.0307. [DOI] [PubMed] [Google Scholar]
- 26.Rozendaal RM, Koes BW, van Osch GJVM, Uitterlinden EJ, Garling EH, Willemsen SP, et al. Effect of glucosamine sulfate on hip osteoarthritis. Ann Intern Med. 2008;148:268–77. doi: 10.7326/0003-4819-148-4-200802190-00005. [DOI] [PubMed] [Google Scholar]
- 27.Maillefert JF, Sharp JT, Aho LS, Dougados M. Comparison of a computer-based method and the classical manual method for radiographic joint space width assessment in hip osteoarthritis. J Rheumatol. 2002;29:2592–6. [PubMed] [Google Scholar]
- 28.Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ. 2009;339:b2844. doi: 10.1136/bmj.b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mancuso CA, Ranawat CS, Esdaile JM, Johanson NA, Charlson ME. Indications for total hip and total knee arthroplasties. Results of orthopaedic surveys. J Arthroplasty. 1996;11:34–46. doi: 10.1016/s0883-5403(96)80159-8. [DOI] [PubMed] [Google Scholar]
- 30.Dreinhöfer KE, Dieppe P, Stürmer T, Gröber-Grätz D, Flören M, Günther KP, et al. Indication for total hip replacement: comparison of assessments of orthopaedic surgeons and referring physicians. Ann Rheum Dis. 2006;65:1346–50. doi: 10.1136/ard.2005.047811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maillefert JF, Roy C, Cadet C, Nizard R, Cohen P, Ravaud P. Factors influencing surgeons’ decisions in the indication for total joint replacement in hip osteoarthritis in real life. Arthritis Care Res. 2008;59:255–62. doi: 10.1002/art.23331. [DOI] [PubMed] [Google Scholar]