Abstract
Background
Little is known about treatment aims during the last 3 months of life.
Aim
To investigate important treatment aims in the last 3 months of patients’ lives in cases of non-sudden death.
Design and setting
Mortality follow-back study in the Netherlands.
Method
Data were collected retrospectively in 2009 within the representative Sentinel Network of GPs in the Netherlands. GPs completed a standardised registration form.
Results
Data for 279 patients were studied. Of these, 55% died of cancer and 45% of another disease. Treatment was aimed at palliation for 73% of the patients in months 2 and 3 before death, and for 95% of the patients in the last week of life. Seven per cent received treatment aimed at cure in the last week of life. In a minority of patients, cure/life prolongation and palliation were simultaneously important treatment aims. In the last week of life and in the 2–4 weeks before death, cure was more frequently reported as an important treatment aim in patients with a non-cancer disease than in patients with cancer. In the 2–4 weeks before death, palliation was an important treatment aim for a larger proportion of patients with cancer than patients with other diseases.
Conclusion
Registration by GPs show that, in the last weeks and days of life, cure was more frequently reported as an important treatment aim in patients with a non-cancer disease than in patients with cancer. For a small number of patients, palliation and cure/life prolongation were simultaneously important treatment aims.
Keywords: epidemiological studies, general practitioners, palliative care, terminal care, treatment
INTRODUCTION
The World Health Organization defines palliative care as:
‘An approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual’.1
Lynn and Adamson developed a model for palliative care that builds partially on this definition.2 According to this model, the palliative phase starts with the diagnosis of a disease that will probably lead to death. Initially, curative and life-prolonging treatments may be given alongside palliative treatments. According to this model, the emphasis on curative/life-prolonging treatments decreases gradually, shifting to an emphasis on palliation. However, few empirical data exist on the timing of this transition and the possible coexistence of treatment aims.
This study explores important treatment aims in the last 3 months of life for cancer patients versus non-cancer patients, and how these treatment aims may change as death approaches. To date, the main focus of attention of palliative care research has been on patients with cancer. However, there are indications that the disease symptoms often fluctuate in patients with non-cancer illnesses, such as end-stage chronic obstructive pulmonary disease (COPD) or heart failure, and the course of the disease is therefore difficult to predict.3-5 It can be expected that the shift towards palliative care in these patients may only take place shortly before death and that identifying a time point for transition to palliative care is more difficult for people with COPD, for instance.6 The course of the disease in patients with incurable cancer maybe relatively predictable, with a clearer demarcation between the curative and palliative stages.3,7
Little research has been done to test the assumption that palliative care may be started in an early stage, alongside curative or life-prolonging treatments. Van den Block et al found that the transition from cure to palliation often occurs at a late stage, and sometimes not at all.8 They also found substantially higher odds of palliative treatment goals for cancer patients in the last 3 months of life than for patients with another cause of death.8 However, in general, very limited research has been conducted into the differences between cancer and non-cancer patients, with regard to treatment aims at the end-of-life stage.9
How this fits in
Previous research in Belgium provided indications that a transition from cure to palliation often occurs late in the illness trajectory and sometimes not at all. The study presented shows that in the last 3 months of life there is an increase in treatments aimed at palliation, while there is a decrease in curative or life-prolonging treatments. In the last month, and also in the last week of life, cure is still an important treatment aim in some patients, although this is more often the case in patients with a non-cancer disease than in patients with cancer.
The following research questions will be addressed using registration data of Dutch GPs:8,10-12
What were important treatment aims for patients who died non-suddenly in (a) months 2 and 3 before death, (b) 2–4 weeks before death, and (c) the last week of life?
Was there a coexistence of important treatment aims; that is, were cure/life prolongation and palliation considered important at the same time?
Are there any differences between patients who died of cancer and patients with another non-sudden cause of death, regarding important treatment aims in the last 3 months before death?
METHOD
Study design and sample
Data were collected within the Dutch Sentinel Network of General Practices. In 2009, this consisted of 41 general practices (58 GPs), covering 0.8% of the 16 million patients in the Netherlands.13 This network is representative of all GPs with regard to age, sex, and population density.
GPs filled in a registration form after the death of each patient older than 1 year of age. In the Netherlands, in principle, all residents have a personal GP. The GP has a central role in the delivery of palliative care for people dying at home or in a home for older people. For this study, the following inclusion criteria were used:
the patient’s death was expected and non-sudden, as judged by the GP; and
in the final year before death, the patient resided either at home or in a home for older people.
Data of nursing-home residents were excluded because nursing-home physicians rather than GPs have the main responsibility for the end-of-life care of these patients in the Netherlands.14
Instrument
The instrument is a standardised 21-item registration form. This form was first tested for comprehensibility by GPs and consisted of multiple-choice and open-ended questions.
Important treatment aims were registered by asking: ‘How important were the following aspects of patient care: treatment aimed at cure?; treatment aimed at life prolongation?; and treatment aimed at palliation?’ GPs had to register these treatment aims retrospectively for the last week of life, the 2–4 weeks before death, and months 2 and 3 before death, using a 5-point Likert scale ranging from 1 (not at all important) to 5 (very important). Multiple responses (that is, treatment aims) were possible in each period.
Statistical analysis
The following approach was used to analyse the coexistence of important treatment aims: there is coexistence when the GP scored 4 or 5 for treatment aimed at palliation in combination with a score of 4 or 5 for treatments aimed at cure and/or life-prolongation. This analysis was done for each of the three different time periods.
To analyse differences between patients who died of cancer and patients with another cause of death, χ2 analysis’ was performed (SPSS, version 15.0). The scores on the item ‘How important were the following aspects of patient care?’ were dichotomised by combining the scores 1, 2, and 3, and by combining scores 4 and 5. Differences between the two groups of patients (cancer versus non-cancer) regarding treatment aims were tested for the three time periods distinguished.
RESULTS
Study population
The GPs reported 495 deaths in a 1-year period in 2009. Sixty-one per cent (n = 279) of the deaths were non-sudden. Results are based on data of 279 patients with a non-sudden death (Table 1).
Table 1.
Patient characteristics for non-sudden deaths (n = 279)
| Characteristic | Cancer, n = 153 | Non-cancer, n (%) = 126a | Total, n = 279 |
|---|---|---|---|
| Age at death, years | |||
| 1–64 | 43 (28.1) | 8 (6.3) | 51 (18.3) |
| 65–84 | 91 (59.5) | 49 (38.9) | 140 (50.2) |
| ≥85 | 19 (12.4) | 69 (54.8) | 88 (31.5) |
| Sex | |||
| Male | 71 (46.4) | 44 (34.9) | 115 (41.2) |
| Female | 82 (53.6) | 82 (65.1) | 164 (58.8) |
| Place of death | |||
| Home | 84 (54.9) | 38 (30.2) | 122 (43.7) |
| Care home | 14 (9.2) | 41 (32.5) | 55 (19.7) |
| Hospital | 28 (18.3) | 44 (34.9) | 72 (25.8) |
| Palliative care unit/hospice | 27 (17.6) | 3 (2.4) | 30 (10.8) |
Cardiovascular diseases (12.9%); respiratory diseases (7.9%); diseases of the nervous system(2.9%); stroke (3.9%), old age (11.8%); other (5.6%).
Eighty-two per cent of the patients were aged ≥65 years. More than half of the causes of death were malignancies; 63% of the patients died at home or in a care home, and 26% of the patients died in a hospital.
Important treatment aims
Important treatment aims in the three time periods studied are presented in Table 2.
Table 2.
Importance of treatment aims in three time periods: months 2 and 3 before death, the 2–4 weeks before death, and the lastweek of life (n = 279).
| Scores on Likert scale | Treatment aims, n (%) | ||
|---|---|---|---|
| Months 2 and 3 before death | Cure | Life prolongation | Palliation |
| 1 (not at all important) | 115 (54.2) | 90 (42.7) | 16 (7.3) |
| 2 | 26 (12.3) | 31 (14.7) | 11 (5.0) |
| 3 | 24 (11.3) | 38 (18.0) | 31 (14.2) |
| 4 | 21 (9.9) | 26 (12.3) | 40 (18.3) |
| 5 (very important) | 26 (12.3) | 26 (12.3) | 120 (55.0) |
| 2–4 weeks before death | |||
| 1 (not at all important) | 158 (70.2) | 123 (55.7) | 5 (2.2) |
| 2 | 23 (10.2) | 29 (13.1) | 7 (3.0) |
| 3 | 20 (8.9) | 29 (13.1) | 14 (6.1) |
| 4 | 14 (6.2) | 21 (9.5) | 45 (19.5) |
| 5 (very important) | 10 (4.4) | 19 (8.6) | 160 (69.3) |
| Last week of life | |||
| 1 (not at all important) | 200 (85.1) | 183 (78.2) | 8 (3.3) |
| 2 | 9 (3.8) | 15 (6.4) | 1 (0.4) |
| 3 | 9 (3.8) | 15 (6.4) | 4 (1.6) |
| 4 | 7 (3.0) | 11 (4.7) | 27 (11.0) |
| 5 (very important) | 10 (4.3) | 10 (4.3) | 206 (83.7) |
Palliation was an important treatment aim in 73% of the patients in months 2 and 3 before death, increasing to 89% in the 2–4 weeks before death, and 95% in the last week of life.
Life prolongation became less important as death neared. Life prolongation was an important treatment aim in 25% of the patients in months 2 and 3 before death, in 18% in the 2–4 weeks, and in 9% of patients in the last week before death.
In addition, GPs reported that treatments aimed at cure were important in 22% of the patients in months 2 and 3 before death, in 11 % in the 2–4 weeks before death, and in 7% in the last week of life.
Figures 1 and 2 show important treatment aims for patients who died of cancer and for patients with another cause of death. These figures are based on the data of GPs who responded with a score of 4 or 5 for the question ‘How important were the following aspects of patient care?’.
Figure 1.
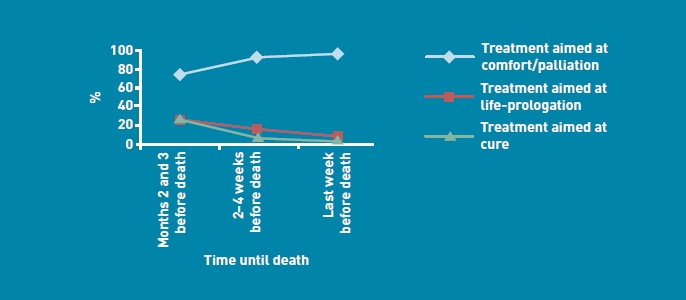
Important treatment aims for patients with cancer.
Figure 2.
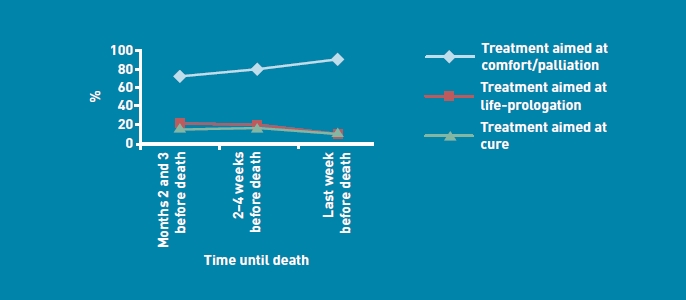
Important treatment aims for non-cancer patients.
In the last week of life, there was a significant difference between patients with cancer and other patients concerning treatment aimed at cure (cancer: n = 4, 3% versus non-cancer: n = 13, 13%, P = 0.005). Hence in the very last days of life, cure was more frequently an important treatment aim for patients with a non-cancer cause of death than for patients with cancer. Also in the 2–4 weeks before death, cure was more frequently an important treatment aim in patients with a non-cancer cause of death than in patients with cancer (cancer: n = 8, 6% versus non-cancer: n = 16, 17%, P = 0.01). However, there were no significant differences regarding treatments aimed at cure in months 2 and 3 before death.
In addition, there were no significant differences between the percentages of patients with cancer and other patients, regarding treatments aimed at life prolongation in the three time periods.
In the 2–4 weeks before death, palliation was an important treatment aim in significantly more cancer patients compared with non-cancer patients (cancer: n = 128, 93% versus non-cancer: n = 77, 82%, P = 0.007). In the last week and in months 2 and 3 before death, there were no significant differences regarding treatments aimed at palliation.
Coexistence of important treatment aims
Table 3 shows that treatments aimed at palliation coexisted with life-prolonging/curative treatment aims for 17% of the patients in months 2 and 3 before death. This coexistence was observed for 13% of patients in the 2–4 weeks before death, and for 8% in the last week before death.
Table 3.
Coexistence of important treatment aims at three time periods, n (%)
| Important treatment aims | Palliation plus cure and/ or life prolongation are important aims (= coexistence) | No coexistence | Don’t know/ missing | Total |
|---|---|---|---|---|
| 2 and 3 months before death | 35 (17) | 176 (83) | 68 | 279 |
| 2–4 weeks before death | 30 (13) | 193 (87) | 56 | 279 |
| Lastweek before death | 18 (8) | 216 (92) | 45 | 279 |
DISCUSSION
Summary
In the last week of life, palliation was an important treatment aim in almost all patients with a non-sudden cause of death. In the 2–4 weeks before death and months 2 and 3 before death, palliation was an important treatment aim in 89% and 73% respectively of patients with a non-sudden cause of death.
Cure and life prolongation were more often important in the time periods that were relatively far away from death. However, in the last week of life cure was still an important treatment aim for 7% of patients. These patients mainly had a respiratory or cardiovascular disease. In these patients, death may be more difficult to predict than in patients with cancer.
Whether life prolongation/cure was an important treatment aim at the same time as palliation was also investigated. It was expected that coexistence of important treatment aims would be common. This expectation was derived from Lynn and Adamson’s model indicating that the palliative phase is a care continuum in which palliation interventions may be given simultaneously with curative or life-prolonging treatments. However, this expectation was not fully supported by the data: in months 2 and 3 before death, palliation and cure and/or life prolongation were simultaneously important treatment aims for only 17% of patients. This finding shows that one treatment aim often prevails over another at any given time.
In addition, differences in treatment aims between cancer patients and other patients were tested. As expected, in the last month of life cure was an important treatment aim for significantly more patients with a non-cancer cause of death than for patients with cancer. In addition, it was found that palliation was an important treatment aim in a larger number of cancer patients compared with other non-suddenly deceased patients in the 2–4 weeks before death. Recognition of approaching death is probably more difficult in non-cancer patients than in cancer patients, and it may therefore also be more difficult for GPs to discuss the prognosis and end-of-life issues with non-cancer patients.
Strengths and limitations
So far, most palliative care research has focused on the terminal stages of life.15-19 In addition, palliative care research on the last months of life of a diverse group of patients is scarce.20 This study, based on epidemiological data from a national representative network of general practices, is exceptional in this regard.
Another strength of the current study is the representativeness of the Sentinel Network for GPs in the Netherlands in terms of age and sex of the GP, and population density. Another strength is that the GPs participate in an existing sentinel network, which means that they were not just recruited for this palliative care study. This reduces the chance of bias in the findings.21
However, this study also has some limitations. Registrations of GPs were restricted to the last 3 months of life. Although this concerns a larger time span than in most other studies on palliative care, it would be interesting to explore whether treatments aimed at palliation may be also important in earlier phases before death.
Finally, a recall bias is possible due to the retrospective design. However, the authors expect that this bias will be small as the registration form was sent to the GP within 1 week of the patient’s death.
Comparison with existing literature
Until a few years ago, researchers often used the terms ‘palliative’ and ‘terminal’ synonymously, and also made a fairly strict separation between the curative and palliative phases. In accordance with the model of Lynn and Adamson, the palliative phase is currently considered as a care continuum that starts with the diagnosis of a life-threatening illness.2,22 Van den Block et al found that a transition from cure to palliation often occurs late in the dying process and sometimes not at all.8 Starting late with palliative care may be due to late recognition of the approaching death, which may be a problem particularly in patients with chronic diseases other than cancer.
Fitzsimons et al pointed to the necessity of embracing the palliative care approach at an earlier stage, to address the needs of patients with life-threatening chronic illness.20 Furthermore, Murray et al concluded that end-of-life care for patients with cardiac failure or other non-malignant diseases should be proactive and designed to meet specific needs.7 In addition, Pinnock et al pointed to the necessity of careful assessment of possible supportive and palliative care needs along people’s lifetime journey with COPD.6 However, the findings of the present study show that for almost all patients in the Netherlands (95%) where death is non-sudden, palliation was an important treatment aim in the last week of their life, although 7% still received treatment aimed at cure in this last week.
The finding that the vast majority of the subgroup of patients with a non-cancer cause of death received treatments aimed at palliation in the last phase of life indicates that, currently, Dutch GPs are also alert to the palliative care needs of non-cancer patients.
Implications for research and practice
Investigation of treatment aims in earlier phases of illness would be interesting. This corresponds with the idea in today’s palliative care policy and research that the palliative phase may already start with the diagnosis of a life-threatening disease. Future research could also consider whether supporting the patient had been an important treatment aim. The concept of ‘supportive care’ has gained in usage, for instance for people with chronic diseases and temporary decompensations or intercurrent illnesses. It would be interesting to explore whether supportive care is frequently given in the very last period of life, and whether supportive care is often combined with treatments aimed at cure, life prolongation, or palliation.
In addition, it would be interesting to conduct a prospective longitudinal study, in which the GP perspective as well as the perspectives of relatives and patients on the treatments and the treatment aims could be explored. Furthermore, it would be relevant to focus on differences between patients with various types of cancer, as well as between various groups of patients with specific chronic diseases.
Acknowledgments
We wish to acknowledge all participating GPs for providing the registration data for this study. In addition, thanks are due to Marianne Heshusius of the Netherlands Institute for Health Services Research for supervising the data-collection process.
Funding
This work was supported by the Netherlands Organisation for Health Research and Development (ZonMw; grant number 11510010).
Ethical approval
According to Dutch law, no approval of a medical ethics committee is needed for post-mortem anonymous data. The anonymity of the patients and GPs was strictly preserved throughout the data-entry and analysis process.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.World Health Organization. WHO definition of palliative care. http://www.who.int/cancer/palliative/definition/en/ (accessed 17 Oct 2011)
- 2.Lynn J, Adamson DM. Living well at the end of life. Adapting health care to serious chronic illness in old age. RAND health white paper WP-137. Santa Monica: RAND; 2003. [Google Scholar]
- 3.Costantini M, Beccaro M, Higginson IJ. Cancer trajectories at the end of life: is there an effect of age and gender? BMC Cancer. 2008;8:127. doi: 10.1186/1471-2407-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Formiga F, Chivite D, Ortega C, et al. End-of-life preferences in elderly patients admitted for heart failure. Q J Med. 2004;97(12):803–808. doi: 10.1093/qjmed/hch135. [DOI] [PubMed] [Google Scholar]
- 5.Habraken JM, Pols J, Bindels PJ, Willems DL. The silence of patients with end-stage COPD: a qualitative study. Br J Gen Pract. 2008;58(557):844–849. doi: 10.3399/bjgp08X376186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinnock H, Kendall M, Murray SA, et al. Living and dying with severe chronic obstructive pulmonary disease: multi-perspective longitudinal qualitative study. BMJ. 2011;342:d142. doi: 10.1136/bmj.d142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray SA, Boyd K, Kendall M, et al. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ. 2002;325(7370):929. doi: 10.1136/bmj.325.7370.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van den Block L, Deschepper R, Bossuyt N, et al. Care for patients in the last months of life: the Belgian Sentinel Network Monitoring End-of-Life Care study. Arch Intern Med. 2008;168(16):1747–1754. doi: 10.1001/archinte.168.16.1747. [DOI] [PubMed] [Google Scholar]
- 9.O’Leary N, Murphy NF, O’Loughlin C, et al. A comparative study of the palliative care needs of heart failure and cancer patients. Eur J Heart Fail. 2009;11(4):406–412. doi: 10.1093/eurjhf/hfp007. [DOI] [PubMed] [Google Scholar]
- 10.Abarshi E, Onwuteaka-Philipsen B, Donker G, et al. General practitioner awareness of preferred place of death and correlates of dying in a preferred place: a nationwide mortality follow-back study in the Netherlands. J Pain Symptom Manage. 2009;38(4):568–577. doi: 10.1016/j.jpainsymman.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Abarshi E, Echteld M, Van den BLock, et al. Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliat Med. 2010;24(2):166–174. doi: 10.1177/0269216309351381. [DOI] [PubMed] [Google Scholar]
- 12.Abarshi E, Echteld MA, Van den BLock, et al. The oldest old and GP end-of-life care in the Dutch community: a nationwide study. Age Ageing. 2010;39(6):716–722. doi: 10.1093/ageing/afq097. [DOI] [PubMed] [Google Scholar]
- 13.Donker GA. Continuous morbidity registration at Dutch Sentinel General Practice Network 2009. Utrecht: NIVEL; 2009. [Google Scholar]
- 14.Hoek JF, Ribbe MW, Hertogh CM, van der Vleuten CP. The role of the specialist physician in nursing homes: the Netherlands’ experience. Int J Geriatr Psychiatry. 2003;18(3):244–249. doi: 10.1002/gps.816. [DOI] [PubMed] [Google Scholar]
- 15.Borgsteede SD, Deliens L, Francke AL, et al. Defining the patient population: one of the problems for palliative care research. Palliat Med. 2006;20(2):63–68. doi: 10.1191/0269216306pm1112oa. [DOI] [PubMed] [Google Scholar]
- 16.Borgsteede SD, Graafland-Riedstra C, Deliens L, et al. Good end-of-life care according to patients and their GPs. Br J Gen Pract. 2006;56(522):20–26. [PMC free article] [PubMed] [Google Scholar]
- 17.Borgsteede SD, Deliens L, Van der Wal G, et al. Interdisciplinary cooperation of GPs in palliative care at home: a nationwide survey in The Netherlands. Scand J Prim Health Care. 2007;25(4):226–231. doi: 10.1080/02813430701706501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borgsteede SD, Deliens L, Beentjes B, et al. Symptoms in patients receiving palliative care: a study on patient-physician encounters in general practice. Palliat Med. 2007;21(5):417–423. doi: 10.1177/0269216307079821. [DOI] [PubMed] [Google Scholar]
- 19.Borgsteede SD, Deliens L, Graafland-Riedstra C, et al. Communication about euthanasia in general practice: opinions and experiences of patients and their general practitioners. Patient Educ Couns. 2007;66(2):156–161. doi: 10.1016/j.pec.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Fitzsimons D, Mullan D, Wilson JS, et al. The challenge of patients’ unmet palliative care needs in the final stages of chronic illness. Palliat Med. 2007;21(4):313–322. doi: 10.1177/0269216307077711. [DOI] [PubMed] [Google Scholar]
- 21.Fischer S, Miccinesi G, Hornung R, et al. Responders and non-responders in a study on medical end-of-life decisions in Denmark, the Netherlands, Sweden and Switzerland. Soz Praventivmed. 2006;51(1):24–33. doi: 10.1007/s00038-005-0004-x. [DOI] [PubMed] [Google Scholar]
- 22.Radbruch L, Payne S. White paper on standards and norms for hospice and palliative care in Europe: part 1. Recommendations from the European Association for Palliative Care. Eur J Palliat Care. 2009;16(6):278–289. [Google Scholar]


