SYNOPSIS
Objectives
A typology of local public health systems was recently introduced, and a large degree of structural transformation over time was discovered in the systems analyzed. We present a qualitative exploration of the factors that determine variation and change in the seven structural configurations that comprise the local public health delivery system typology.
Methods
We applied a 10-item semistructured telephone interview protocol to representatives from the local health agency in two randomly selected systems from each configuration—one that had maintained configuration over time and one that had changed configuration over time. We assessed the interviews for patterns of variation between the configurations.
Results
Four key determinants of structural change emerged: availability of financial resources, interorganizational relationships, public health agency organization, and political relationships. Systems that had changed were more likely to experience strengthened partnerships between public health agencies and other community organizations and enjoy support from policy makers, while stable systems were more likely to be characterized by strong partnerships between public health agencies and other governmental bodies and less supportive relationships with policy makers.
Conclusions
This research provides information regarding the determinants of system change, and may help public health leaders to better prepare for the impacts of change in the areas discussed. It may also help those who are seeking to implement change to determine the contextual factors that need to be in place before change can happen, or how best to implement change in the face of contextual factors that are beyond their control.
The Council on Linkages Between Academia and Public Health Practice publication “Public Health Systems Research: Summary of Research Needs” and the public health systems research agenda in “Public Health Systems Research: Setting a National Agenda” both cite the need for comparative analysis of different types of public health systems.1,2 This need is complicated by the wide variation in structural characteristics of public health delivery systems; it often serves to blur the similarities among systems and makes comparative research on public health structure, process, and outcomes difficult. A key aspect of conducting comparative analysis is the development of meaningful, uniform categories for comparison. Creating meaningful categories allows researchers to differentiate among systems, and enables them to identify variations in key characteristics or domains that may be related to differences in other variables (e.g., public health department and system performance, or community health status).
System typologies have already been developed and used to conduct comparative analysis research in fields similar to public health, most notably health care.3,4 Typologies also have been developed in public health. For example, Halverson et al. developed a three-type model of the structure of public health agency-managed care collaborations.5 All of these typologies define key characteristics of health systems to differentiate among them.
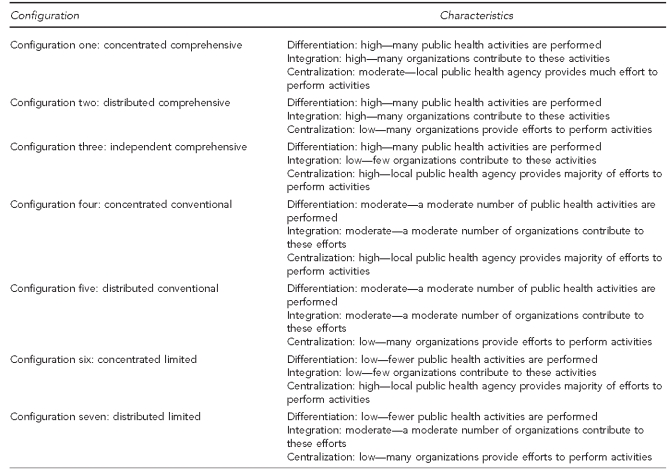
Mays et al. have introduced a typology of local public health delivery systems that distinguishes systems based on three structural characteristics: (1) differentiation, defined by range of services provided; (2) centralization, defined by the distribution of control over and responsibility for the system; and (3) integration, defined by the distribution of service provisions between the public health agency and other members in the system.6 Using these characteristics, seven distinct system clusters, or configurations, were identified through hierarchical analysis of longitudinal data from a national sample of local public health systems. Data for each system examined were collected twice—in 1998 and in 2006. Figure 1 lists these configurations, along with their varying levels of differentiation, centralization, and integration.
Figure 1.
Seven configurations of public health systems developed by Mays et al.a and their associated characteristics
aMays GP, Scutchfield FD, Bhandari MW, Smith SA. Understanding the organization of public health delivery systems: an empirical typology. Milbank Q 2010;88:81-111.
Mays et al. identified differences among the configurations in the characteristics described previously, but they did not examine why these differences existed or why some systems migrate from one configuration to another over time. This topic was of particular interest given that the analysis found a large degree of structural transformation over time. This finding led to a qualitative study, described in this article, to uncover the forces that precipitated and shaped this change. This article presents a qualitative exploration of factors that determine variation and change in the seven structural configurations that comprise the local public health delivery system typology.
METHODS
The public health systems examined in this study were members of the 236 public health systems, all serving populations of at least 100,000 people, that were analyzed to create the Mays et al. typology.6 The systems were located in all but four states in the U.S. (Massachusetts, Maine, Rhode Island, and Wyoming). Each of the 236 systems was classified according to the seven configurations of the typology and then further stratified based on whether or not the system migrated from one configuration to another between 1998 and 2006. Two systems from each configuration were randomly selected for in-depth qualitative analysis: (1) a system that had remained stable from 1998 to 2006 and (2) a dynamic system that had changed to another configuration between the two time periods. Including both stable and dynamic systems of each configuration allowed this study to examine the forces that influence variation and change in system structure. The systems were grouped for analysis based upon their configuration in the 1998 survey. Because configurations four and six did not contain any stable systems, two additional dynamic systems were randomly selected.
The authors designed a 10-item semistructured telephone interview protocol to explore factors hypothesized to influence variation and change in public health system structure. Questions were primarily open-ended but were supplemented with probing sub-questions that addressed specific areas of change or stability in each system, as identified by the system representative's responses to the 20-question National Longitudinal Study of Public Health Systems (NLSPHS) surveys in 1998 and 2006. Evidence suggested that changes in areas such as the State Children's Health Insurance Program (SCHIP), Medicaid, and the managed care environment, as well as the renewed emphasis on preparedness after the events of 9/11, likely influenced migration between configurations. For example, 63% of the respondents to the National Association of County and City Health Officials' 2005 Profile of Local Health Departments reported stronger relationships with other state, local, or federal agencies as a result of efforts to improve preparedness.7 Thus, these topics were integrated into questions that asked about three interrelated types of factors hypothesized to influence stability and change in public health system structure: economic factors (financial resources), institutional factors (relationships among organizations), and political factors (relationships with policy decision makers).
The questionnaire was pilot-tested on directors from three health departments and revised based on their feedback to enhance instrument clarity and reliability. Telephone interviews were then conducted with the directors or their designee of the 14 health departments in the systems selected for analysis. Interviews were recorded, transcribed by a medical transcriptionist, and checked for accuracy against the original recordings; any mistakes were noted and corrected. Data from the corrected transcripts were then coded according to identified themes and assessed for patterns of variation between clusters by three project staff.
RESULTS
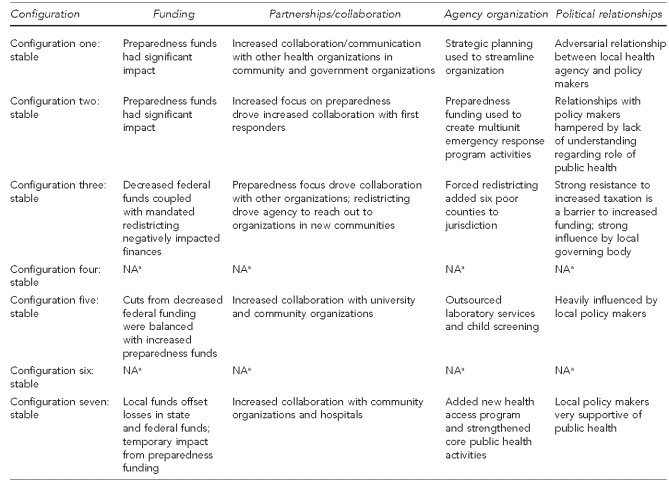
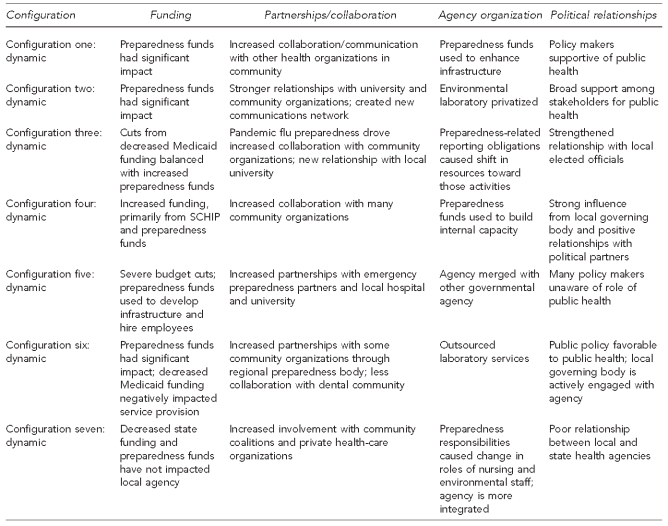
Four key determinants of structural variation and change in local public health delivery systems related to the topics contained in the survey emerged: availability of financial resources, interorganizational relationships, public health agency organization, and political relationships. The nature and intensity of these factors varied widely across the seven system configurations. Figures 2 and 3 summarize how each of these factors varied across the seven configurations.
Figure 2.
Major themes emerging from an analysis of qualitative data obtained from interviews with 236 local health departments that were stable in each public health system configuration: U.S., 1998–2006
aNone of the 236 systems examined by Mays et al. remained stable in these configurations from 1998–2006. See: Mays GP, Scutchfield FD, Bhandari MW, Smith SA. Understanding the organization of public health delivery systems: an empirical typology. Milbank Q 2010;88:81-111.
NA = not available
Figure 3.
Major themes emerging from an analysis of qualitative data obtained from interviews with 236 local health departments that were dynamic in each public health system configuration: U.S., 1998–2006
SCHIP = State Children's Health Insurance Program
Configuration one: concentrated comprehensive systems
Increased preparedness funding drove changes in both the stable and dynamic systems analyzed. However, while both respondents reported using funds to hire staff, the local health agency in the dynamic system also used preparedness funds to facilitate organizational change through enhancing departmental infrastructure, particularly communications capacity. Both systems experienced increased collaboration with other community organizations; the stable system also experienced increased involvement of government organizations. Organizational change inside the agency representing the stable system was internally focused and driven by a strategic planning process, while change in the agency in the dynamic system was the previously discussed change from external preparedness funding. The stable system was characterized by an adversarial relationship between the local health agency and policy makers, primarily due to a lack of understanding by policy makers of the role of public health, while the dynamic system enjoyed a political climate that was supportive of public health.
Configuration two: distributed comprehensive systems
Preparedness funding again drove change in both systems and was used to strengthen relationships among different units within the local health agency in both systems. However, the agency in the stable system also used preparedness funds to involve personnel from multiple units in activities in a newly developed emergency response program. While both systems enjoyed increased collaboration with system partners, the stable system experienced increased partnerships with first responders driven by an emphasis on preparedness. In contrast, the dynamic system was characterized by strengthened relationships between the agency and other community organizations, as well as a university and a newly created communications network. Organizational change in the stable department was internal and focused on strengthening infrastructure through integrating personnel from multiple units in activities in a newly developed emergency response program. In contrast, the dynamic department reported -outsourcing laboratory services. The stable system experienced difficult relationships with policy makers, who displayed a lack of understanding of the role of public health, while the dynamic system enjoyed broad support among stakeholders for public health activities.
Configuration three: independent comprehensive systems
Reduced federal funds, particularly Medicaid funds, adversely affected both systems in configuration three. Preparedness funds stimulated increased collaboration between the local health agency and other community organizations in both systems; the agency in the dynamic system also used preparedness funds to offset staffing cuts. State-mandated redistricting in the stable system increased the local health agency's service area; as a result, the system was characterized by new relationships with community organizations in areas absorbed by redistricting. The systems differed significantly in their political climate: the stable system was characterized by resistance of citizens to increased taxation being a barrier to increased funding and a strong influence by the local governing body, while the dynamic system enjoyed a strengthened relationship with elected officials.
Configuration four: concentrated conventional systems
In the dynamic configuration, the four departments reported increases in state and federal funding, primarily in the forms of expanded SCHIP coverage, and an increase in preparedness funding. The system experienced increased collaboration among the local agency and a large city health department within its boundaries, managed care organizations, nonprofits, and schools. Preparedness funds were used by the agency to cross-train existing personnel and increase communications and data analysis capacity. The system enjoyed positive relationships with political partners and strong influence from the local governing body.
Configuration five: distributed conventional systems
Both configuration five systems were influenced by preparedness funding, and both agencies used preparedness funds to hire staff. The dynamic agency also used preparedness funds to develop departmental infrastructure. The stable system enjoyed strong ties between the agency and community partners, while the dynamic system was characterized by increased partnerships with preparedness partners and a local hospital. The stable department reported outsourcing of laboratory services and child screening, and the dynamic department reported being merged with another governmental agency. The stable system was characterized by a heavy influence of local policy makers. In contrast, the transitional system experienced a general ambivalence or lack of knowledge of policy makers regarding public health.
Configuration six: concentrated limited systems
The dynamic system in configuration six that we analyzed had shifted to configuration three in 2006. The system experienced decreased Medicaid funding, resulting in decreased service provision, particularly to children, and a shift of vulnerable populations to managed care organizations. Preparedness funding drove the creation of new preparedness programs. The system experienced increased partnerships with some community organizations as the result of the development of a regional preparedness body, but less collaboration with others, such as the dental community. Agency organizational changes included the outsourcing of laboratory services. The system was characterized by public policies that were favorable toward public health and a local governing body that was actively engaged in public health activities.
Configuration seven: distributed limited systems
Both configuration seven systems experienced decreased state funds; however, the agency in the stable system used local funds to offset losses at the state and federal level. Federal preparedness funds had little impact on either system, with the stable agency reporting that the loss of preparedness funds had caused a reduction in preparedness personnel, and the dynamic agency reporting that preparedness funds had not trickled down to the department from the state health agency. Both systems developed strong relationships with community and health-care organizations, as well as a strengthened departmental infrastructure. The stable system enjoyed local policy makers who were very supportive of the health agency. In contrast, the dynamic system was characterized by poor relationships between the local and state health agencies.
DISCUSSION
Local public health systems varied widely in the economic, institutional, and political forces that shaped their structure during the study period. The patterns of variation observed in these determinants suggest sharp distinctions in the experiences of stable systems vs. dynamic systems. Dynamic systems were more likely to enjoy strong support from stakeholders, in particular policy makers. This finding stands in sharp contrast to the stable systems, which were more likely to be characterized by adversarial relationships between public health agencies and policy makers. The result, however, is no surprise: to reorganize and restructure, it is imperative to have the support of those who are major political stakeholders. To attempt to make change without the support and encouragement of the political arm of the community would not seem to be a wise course of action.
In addition, dynamic systems were more likely to report increased levels of collaboration with other community organizations between the 1998 and 2006 surveys. Stable systems, in contrast, were more likely to report increased collaboration with other governmental organizations, including first responders and schools. This collaboration was motivated, to a large degree, by increased preparedness funding. The strong reported influence of preparedness funding on partnerships is potentially troubling in light of the relatively transient nature of such funding. In the absence of funding, it may be difficult or impossible to sustain these relationships. It would be interesting to examine the extent to which these two types of partnerships—one with governmental agencies focused on preparedness and the other with other community organizations focused on assessment, support, and technical services—were the most lasting relationships, and the extent to which either lasted beyond the loss of major preparedness funding support.
Preparedness funding also profoundly influenced the nature and character of organizational change in the systems examined. Public health agencies in dynamic systems were more likely to report more externally related organizational change, including outsourcing functions (e.g., the laboratory) or developing relationship capacity specifically related to the preparedness function. In contrast, agencies in stable systems looked internally and focused on structural changes that were not totally related to preparedness funding. They used the funding to make modifications to their current way of doing business rather than seeking new ways to structure or organize their activities. Once again, this difference is potentially troubling given the relatively short-term nature of much preparedness funding. The organizational structure brought about by preparedness funding may not be sustainable in the absence of that funding.
Given the wide and varied diversity of conditions under which public health systems operate, it may be impossible to label one typology, or group of typologies, as being superior to or more desirable than others. However, given this diversity, as well as their reported superior performance, highly differentiated systems may often be preferable to those showing less differentiation.6 If this is the case, then it is also possible to identify certain drivers of desirable vs. undesirable change.
While all the systems analyzed reported being strongly influenced by changes in funding, in particular state and federal funds, the departments migrating from typologies characterized by the highest levels of differentiation to those of lower differentiation seemed to function in a reactive fashion to funding changes; that is, much reported change was focused externally. These departments tended to focus on strengthening outside partnerships rather than improving departmental infrastructure. While strengthening partnerships and engaging more stakeholders may be viewed in a positive light, it may also indicate a sort of mission creep. These departments, instead of strengthening core operations, may have abandoned many services that were traditionally offered to focus on services that are supported or mandated by funding changes. In contrast, departments in systems that maintained high levels of differentiation, or migrated to high levels of differentiation, seemed to be able to react to these changing conditions while developing or maintaining a focus on internal improvements (e.g., streamlining infrastructure). Perhaps the impact of funding changes was mitigated, to some extent, by engaging a large number of system partners to provide services that were supported or mandated by funding changes.
Given the dynamic nature of much state and federal funding, departments and systems that are highly dependent upon these funds may become less differentiated and more reactive. They may have a harder time maintaining stability and improving internal operations. It is difficult to make lasting improvements to departmental infrastructure when funds used to improve infrastructure are temporary. Highly differentiated systems that wish to maintain their levels of differentiation, or systems seeking to increase their differentiation, may wish to develop strategies to mitigate the impact of short-term increases/decreases in funding. However, while shifting to a more differentiated system may be the most desirable solution to funding-related problems, the relative financial stability associated with the configuration seven systems suggests that another potential solution to the problem of transient funding faced by other departments may be to ensure that an adequate base of local funds exists to dampen the effects of funding changes at the state and federal level.
Limitations
This research did have some limitations. For one, some of the departments interviewed had experienced changes in leadership between the two NLSPHS surveys, and different individuals completed the surveys. Second, some of the changes identified and examined by the authors may have been due to differences in respondent perception rather than organizational change. Third, many of the questions in the interview instrument were open-ended. Thus, it was possible for the interviewers, to some extent, to impact the breadth and depth of the examination of the data and influence the results through a sort of researcher bias. Fourth, this research may not be generalizable to many health departments, particularly those serving small communities, because the departments chosen for the NLSPHS all served populations of at least 100,000 people. Furthermore, the number of departments interviewed was also quite small.
Many of these limitations could be addressed through exploring whether these results apply to a larger number of departments, perhaps by developing a questionnaire based on these results and determining if the phenomenon uncovered exist in other departments. It would also be informative to examine departments serving smaller communities, and determine the degree to which the experiences of these departments mirrored those serving larger populations.
CONCLUSIONS
The results of this qualitative research provide additional insight into the results of the empirical analysis conducted by Mays et al. However, the results also raise additional questions and confirm some anecdotal concerns regarding the organization and function of health departments, particularly related to funding. Our results, particularly as they relate to the impact of preparedness funds, suggest that funding drives many health departments' activities. It is imperative to closely monitor the impact of the medical care funding changes, especially those driven by the Affordable Care Act,8 on the nature of public health departments and their capacity to provide a range of population-based services. They could cause profound changes to the organization and activities of local health departments.
This research uncovered valuable information about the drivers of organizational stability and change in the departments examined. The results of this research provide public health leaders and researchers with information regarding the impact of changes in these contextual factors on departments, and may help public health leaders to better prepare for the impacts of change in the areas discussed. It may also help public health leaders who are seeking to implement organizational change determine the contextual factors that need to be in place before change can happen, or how best to implement change in the face of contextual factors that are beyond their control.
REFERENCES
- 1.Council on Linkages Between Academia and Public Health Practice. Public health systems research: summary of research needs. 2005. [cited 2011 Oct 6]. Available from: URL: http://www.phf.org/link/phsr/phsragendas.pdf.
- 2.Lenaway D, Halverson P, Sotnikov S, Tilson H, Corso L, Millington W. Public health systems research: setting a national agenda. Am J Public Health. 2006;96:410–3. doi: 10.2105/AJPH.2004.046037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wendt C, Frisina L, Rothgang H. Healthcare system types: a conceptual framework for comparison. Soc Policy Admin. 2009;43:70–90. [Google Scholar]
- 4.Mitchell SM, Shortell SM. The governance and management of effective community health partnerships: a typology for research, policy, and practice. Milbank Q. 2000;78:241–89. 151. doi: 10.1111/1468-0009.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halverson PK, Mays GP, Kaluzny AD, Richards TB. Not-so-strange bedfellows: models of interaction between managed care plans and public health agencies. Milbank Q. 1997;75:113–38. doi: 10.1111/1468-0009.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mays GP, Scutchfield FD, Bhandari MW, Smith SA. Understanding the organization of public health delivery systems: an empirical typology. Milbank Q. 2010;88:81–111. doi: 10.1111/j.1468-0009.2010.00590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leep CJ. 2005 national profile of local health departments. Washington: National Association of County and City Health Officials; 2006. [DOI] [PubMed] [Google Scholar]
- 8. Public Law 111-148 to be codified as amended in various sections of title 42 of the U.S.C. and the Internal Revenue Code, 26 U.S.C.