Abstract
Chronic low back pain (CLBP) is widespread among older adults (≥ 65 years) and is often treated inadequately. With a rapidly growing aging population, CLBP will increase and so will the demand for treatment. We believe that mind-body therapies can help to meet this demand. We present the methodology of a randomized, controlled clinical trial of 300 individuals with CLBP aged 65 years or older. The specific aims are, 1) to determine the effectiveness of a mindfulness meditation program in increasing function and reducing pain among older adults with CLBP, and 2) to evaluate the impact of mindfulness meditation on neuropsychological performance in older adults with CLBP. The intervention program is modeled on the Mindfulness-Based Stress Reduction Program (MBSR) and the control is adapted from the 10 Keys™ to Healthy Aging. We will measure self-reported and objectively measured physical function and include a variety of measures to assess pain intensity and pain interference and psychological function. Our primary hypothesis is that the MBSR program will be more effective than the 10 Keys ™ program in increasing function and decreasing pain. The proposed study represents the first large, well-controlled, comprehensive examination of the effects of a mind-body program on older adults with chronic pain.
Keywords: Low Back Pain, Older Adult, Mindfulness, Meditation, randomized clinical trial
1. Introduction
Among the 37 million older adults (≥ 65 years) alive today[1], it is estimated that up to 50% live with chronic pain [2]. More than 17 million of them have experienced at least one episode of low back pain during the past year [3], and it is the most frequently reported musculoskeletal problem [4]. Pain is associated with significant morbidity in the older adult, including decreased physical function, increased disability, decreased quality of life, poor sleep, and depression [5]. Despite its prevalence and associated morbidities, older adults suffer from inadequately treated pain. Conventional treatment options are not always feasible for the older adult. NSAIDs are limiting due to well-described gastrointestinal and nephrotoxic side-effects [6]. Opioids are associated with increased susceptibility to falls and fractures [7]. Millions of individuals suffer from compromised quality of life because of frequent pain episodes [3]. There is an urgent need for safe and effective therapies to relieve chronic pain in the older adult.
The multidimensional nature of pain lends itself to the multidimensional approach of mindbody medicine. Pain researchers have long recognized the complexity of a painful stimulus and have described not only a sensory component, but a cognitive and emotional element as well. Processing of a nociceptive stimulus involves sensory perception and motivational and affective responses. In turn, mind-body therapies are based on a comprehensive approach for the patient to address various dimensions of pain. Mind-body therapies like mindfulness meditation teach patients to work with the sensory, cognitive, and affective responses to pain. Because mind-body therapies do not involve medication, they offer a relatively safe treatment option for older adults who may have exhausted other forms of pain therapy. We describe the methodology of a randomized controlled trial of an 8-week mindfulness meditation program (Mindfulness-Based Stress Reduction [8] (MBSR) vs. an educational program (the 10 Keys™ to Healthy Aging [9]) in older adults with chronic low back pain (CLBP).
Kabat-Zinn, who introduced mindfulness meditation to the medical community, described mindfulness as “the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment by moment ” [10]. Previous research by Kabat-Zinn showed a significant reduction of pain among 90 patients with chronic pain conditions [11]. He published 4-year follow-up showing maintenance of pain improvement among 60–72% of 225 chronic pain patients [12]. 63 patients with rheumatoid arthritis were randomized to an MBSR program or a control program. Six-months after program completion, there was significant improvement in psychological distress and well-being [13]. Other studies have found that mindfulness meditation is associated with reduction in depression, anxiety, and stress [14–16]. Although these results are compelling, the studies present methodological problems as some lacked randomized controls, had small sample sizes, and included heterogeneous pain conditions and ages.
Because of the emphasis of mindfulness meditation on sharpening one’s attention to the present moment’s experience, researchers have been actively studying its effects on neuropsychological performance. One aspect of neuropsychological performance is attention. Mindfulness meditation has been found to improve attention among a healthy population who took the 8-week MBSR program as compared to a control group [17]. In addition to attention, executive function is also an important neuropsychological dimension and which can be tested with the Stroop task. This common test was used among healthy college students and those who were taught mindfulness meditation as compared to an active or passive control performed better on the Stroop [18]. Because of mindfulness meditation’s promising potential to affect neuropsychological performance, we will measure these two domains of neuropsychological performance (attention and executive function). Improving neuropsychological performance may be one of the mechanisms by which mindfulness meditation works.
2. Study objectives and hypotheses
The primary objective of Aging Successfully with Pain is to determine the effectiveness of a mind-body program in increasing function and reducing pain among older adults with chronic low back pain as compared to a health education program. The mind-body program is modeled after the 8-week MBSR program and the health education program, on the 10 Keys™ to Healthy Aging. Our primary hypothesis is that the MBSR program will be more effective than the 10 Keys ™ program in increasing function and decreasing pain. Our secondary aim is to evaluate the impact of mindfulness meditation on neuropsychological performance in older adults with chronic low back pain. There is evidence that in community dwelling older adult patients with heterogeneous persistent non-malignant pain disorders, pain severity is associated with diminished executive function [19]. In older adults with CLBP decrements in multiple domains of neuropsychological performance has been described by researchers as compared with pain-free age-matched controls, specifically immediate and delayed memory, language, executive function, and manual dexterity [20]. An unexpected finding in this study was that the association between pain severity and physical performance was no longer significant when analyses controlled for neuropsychological performance, suggesting neuropsychological performance mediated the relationship between pain severity and physical performance. Therefore, even with more severe pain, if neuropsychological performance was high, there was not an effect on physical function. Improved neuropsychological performance as a result of mindfulness meditation may, therefore, mediate any effects observed on physical function and pain. We will assess neuropsychological performance through an innovative software program named the Computer-Based Assessment of Mild Cognitive Impairment (CAMCI), a brief, standardized, and comprehensive computer-based assessment of mental status [21–22]. It evaluates several domains of neuropsychological performance, including attention and executive function. Our secondary hypothesis is that mindfulness meditation will be associated with significant improvement in neuropsychological performance as compared to participants in the health education program.
3. Materials and methods
3.1 Overview
This experimental study is designed as a randomized, education-controlled clinical trial of a mindfulness based stress reduction program for older adults with CLBP. We plan to recruit 300 participants with CLBP aged 65 years and older. We have modified the MBSR program to specifically target individuals with chronic pain. The control group will receive the 10 Keys™ to Healthy Aging developed at the University of Pittsburgh Center for Healthy Aging. This is a successful community-based health education program that teaches older adults about topics relevant to their health. Because of the important health topics taught, it will provide a valuable program to participants. Pain information is not a component of the 10 Keys™ program, and we purposefully did not add this information to avoid contamination of the control group since back pain programs have been shown to be of benefit to patients with CLBP [23].
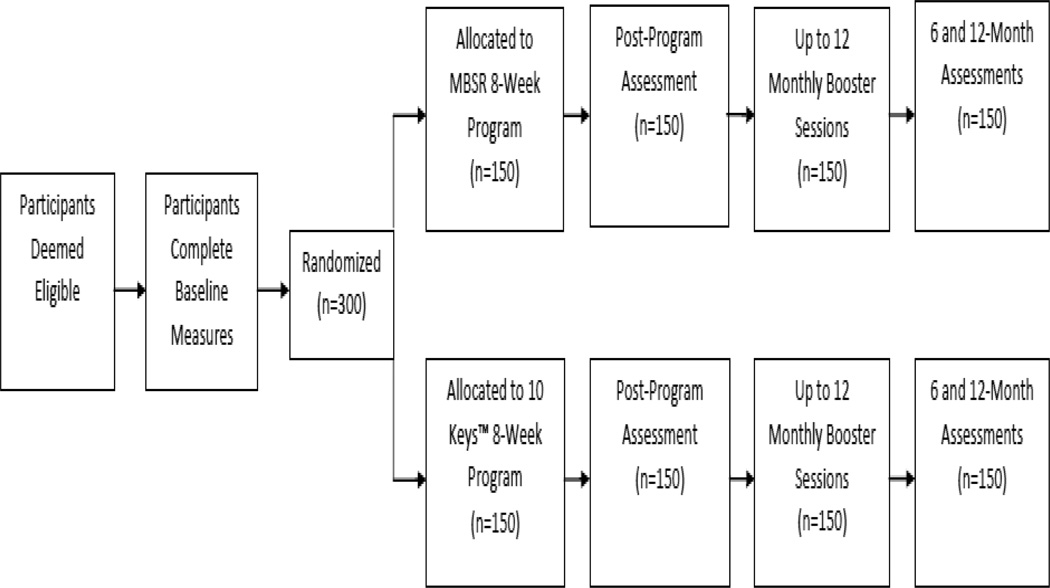
We will offer monthly “booster” classes at the completion of both programs for up to 12 months. We will measure self-reported and objectively measured physical function with tests validated in an older population. We view pain as multidimensional; therefore, to adequately capture the impact of the mind-body program on pain we will include a variety of measures to assess not only pain intensity but psychological function and neuropsychological performance. Focus groups will be conducted on a subset of participants to collect in-depth personal descriptions of using mindfulness meditation for improving function and reducing pain. See Figure 1.
Fig. 1.
Aging Successfully with Pain study design
The trial addresses several limitations in previous clinical trials on mindfulness meditation for chronic pain, including addressing CLBP only instead of a variety of chronic pain conditions, including a rigorous control condition, and large sample size. There are other unique aspects to the trial such as examining the effects of a mind-body program on physical function and the multidimensional aspects of pain in older adults with CLBP, and describing how pain, a common late life problem, may be correlated with cognitive ability as measured through neuropsychological performance.
The protocol for this study was approved by the University of Pittsburgh Institutional Review Board.
3.2 Inclusion and Exclusion Criteria
Participants are selected if they meet all inclusion criteria including: age ≥ 65, intact cognition (Mini-Mental State Exam (MMSE) ≥24), CLBP defined as moderate pain on the Pain Thermometer ( It has 6 choices on a vertical "thermometer" ranging from "no pain at all" to "the pain is almost unbearable") [24], pain must occur daily or almost every day for at least the previous three months, participants must exhibit functional limitations due to low back pain defined as a score of at least 11 on the Roland and Morris Disability Questionnaire, speak English, and have access to a telephone.
Participants are excluded if they do not meet the above inclusion criteria, have participated in a mindfulness meditation program before since we want to capture the effects of learning meditation for the first time on outcomes, have an underlying illness such as malignancy, infection, unexplained fever, significant involuntary weight loss (≥ 10 pounds), or recent trauma, are non-ambulatory, have significant visual or hearing impairment (affecting the ability to hear the workshop instructor complete assessments such as the Computer-Based Assessment of Mild Cognitive Impairment, as well as monthly telephone assessments), have other pain that is more severe than their back pain, have acute or terminal illness, and moderate to severe depression (Geriatric Depression Questionnaire score ≥ 21).
3.3 Recruitment
A variety of recruitment strategies are used to enroll participants for this study. The majority of participants are contacted primarily through direct mail, which includes letters and mailed brochures. Addresses are obtained in the following ways: through several established University of Pittsburgh registries, and direct purchase of addresses through a direct mail business. The latter has the capability of providing customized mailing lists (e.g., age and location).
Additionally, print ads are placed in local news, religious, and community-based publications, many of which are aimed at local senior citizen populations. Flyers are also posted throughout area hospitals and clinics.
3.4 Screening
Once telephone contact is established, verbal consent is obtained and screening questionnaires are administered. Screening for this study takes place in two phases. The first phase begins over the telephone using a structured questionnaire administered by a trained research assistant. If during the phone screening phase a participant meets inclusion criteria, he or she is then invited to undergo informed consent and complete phase two of screening.
The second phase of screening takes place in-person after individuals have signed informed consent in accordance with the University of Pittsburgh Institutional Review Board guidelines. A qualified staff member administers the MMSE, Roland and Morris Disability Questionnaire and the Geriatric Depression Questionnaire to confirm eligibility. Participants also undergo a physical exam to identify underlying conditions that require medical attention and would prevent participation.
3.5. Randomization
After successful screening, written informed consent, physical exam, and baseline measures have been completed, all eligible research participants entering this study are randomized into one of two groups, 1) MBSR program (intervention) or, 2) 10 Keys™ to Healthy Aging (control). Randomization assignment was performed by a systems analyst using statistical software with a random-number generator to create a list of group assignments before study recruitment began and was created based on the specific number of expected eligible participants and divided equally between the intervention and control group. Study staff and the PI do not have access to this list. Once an eligible participant has been screened, the Project Manager submits a request to the electronic data entry system to randomize the eligible participant. The program locates the first unassigned record in the randomization list and assigns the participant to the group designated in that record. Once a participant is randomized, the Project Manager calls the participant to alert them of their randomization status and their workshop start date. A letter confirming this information is then sent to the participant’s mailing address. Randomization balance (age, race, ethnicity, education, income) is checked quarterly by the lead biostatistician (CGM).
3.6. Study Interventions: MBSR Program
Frequency and setting: Participants will be seen in a group format once a week for 90 minutes for 8-weeks. Group size will be 10–12 participants per class. We found this to be the optimal class size in our pilot work because the group was small enough to encourage individual participation, but not too large that participants were afraid to speak up. The intervention is modeled on the Mindfulness-Based Stress Reduction program which has been taught as a psycho-educational intervention in a group-based format since the late 1970’s. The group-based format has advantages over individual instruction as it is more efficient to teach in a group setting rather than individually and participants benefit from sharing each other’s experiences learning mindfulness meditation and applying mindfulness to daily life. The sessions will be led by an experienced MBSR teacher who has undergone teacher training in at least two intensive (≥ 100 hours) teacher training programs conducted by the University of Massachusetts Medical School Center for Mindfulness.
Program Principles
Four methods of mindfulness meditation will be taught. These techniques take regular activities like sitting, walking, and lying down and transform them into a meditation through directed breathing and mindful awareness of thoughts and sensations [8].
The methods used are: 1) the body scan, where in a lying position, the participant is guided to place their attention non-judgmentally on each area of the body from the toes to the top of the head and directing the breath to each region in turn, 2) sitting practice, which is focused attention on breathing while sitting on a chair, 3) walking meditation, which is mindful slow walking with focused attention on body sensation and or breathing, and 4) mindful stretching: participants are taught to purposefully direct their awareness to physical sensation while doing simple stretching exercises while seated. In the original MBSR program the mindful movement component is yoga and in our modified program it is stretching. We did this change explicitly, taking into account that yoga may not be feasible for some older adults.
During the first week participants will be introduced to the principles and practice of mindfulness meditation. The homework requirement of daily meditation (six of seven days/week) lasting 50 minutes (45 minutes of meditation, 5 minutes to complete a log) will be reviewed. Support materials of CD recording, daily log and reading materials will be handed out. The CD contains recordings of guided meditations for the body scan, sitting meditation, and mindful stretching.
During the second and following weeks the sessions will include a general discussion of the participants’ experience with the meditation method, including problem-solving regarding obstacles to the meditation practice. Theoretical material related to meditation, relaxation, pain and the mind-body connection will be presented at this time. About 30 minutes will be spent at each session in these discussions. Table 1 presents a summary of each week’s class.
Table 1.
The 8-week Mindfulness Based Stress Reduction program
Week 1
|
Week 2
|
Week 3
|
Week 4
|
Week 5
|
Week 6
|
Week 7
|
Week 8
|
Booster sessions
We expect that it will take more time than 8-weeks for participants to develop familiarity and proficiency with mindfulness meditation, as the program in and of itself is only an introduction to meditation. Research studies support this, showing an effect 6–12 months after completion of the program [13, 25]. Therefore, to encourage proficiency with the meditation method, we will conduct booster sessions for all participants who have completed the 8-week program. Sessions will occur monthly for 12 months (12 sessions) and will last for one hour. Each session will be structured around 30–40 minutes of mindfulness meditation and 20–30 minutes of discussion around the themes brought up during the 8-week program.
3.7. The 10 Keys™ program
A convincing comparison group is essential for participant recruitment and retention and necessary to control for key components of the mind-body program. Therefore, the comparison group will control for time, group size, attention, homework, and facilitator time. We are basing the 8-week health education program on a successful aging curriculum known as the 10 Keys™ to Healthy Aging. Because this intervention teaches important health topics that are relevant to the older adult, it will provide a valuable program to participants.
We have edited the program to eight topics, so that we could conduct 8-classess to parallel the mind-body program. Each key provides important risk/benefit information related to the topic, and homework assignments that ask participants to apply what they have learned in class. The curriculum also informs older adults about risk factors for diseases, such as hypertension, diabetes, and hyperlipidemia, and preventive strategies for improving health, including maintaining social contact, cancer screening, immunizations and social participation. The program is taught by a health-educator. The two keys that were removed were Combat Depression and Be Physically Active since these could potentially impact outcomes of physical function and pain. Table 2 presents the topics that are discussed.
Table 2.
10 Keys™ to Healthy Aging: 8-week program
| Key #1: Lower Systolic Blood Pressure |
| Key #2: Stop Smoking |
| Key #3: Participate in Cancer Screening |
| Key #4: Get Immunized Regularly |
| Key #5: Blood Glucose |
| Key #6: Lower LDL Cholesterol |
| Key #7: Maintain Healthy Bones, Joints & Muscles |
| Key #8: Maintain Social Contact |
Booster sessions
To ensure the control group receives an equal amount of attention and social support, we will also offer monthly booster classes to all participants who have completed the 8-week program. They will meet, like the intervention group, monthly for 12 months (12 sessions), for one hour. The classes will be based on the topics presented in the 10 Keys™ to Healthy Aging, or a topic requested by participants.
3.8. Adherence and retention
Interventions to promote adherence and retention
Adherence-promoting strategies for the intervention group for home meditation includes the log, audio recording and instructional materials. Group sessions will stress the importance of home practice and group participation, and discussion will include problem-solving around barriers to the meditation practice. The control group will be reminded of the importance of group participation and how to implement what they have learned during each class for their own health.
Participants are given the following material incentives to remain in the study: they are reimbursed $50 for each of the four in-person assessments, $75 if they participate in the focus group, they receive parking vouchers when they drive for the classes or the assessments, and receive an extra $40 to reimburse for gasoline. Transportation by a cab or car/van service for those participants who cannot drive is provided.
Attendance will be taken at each session, and when a participants misses class (and the instructor was not notified that the participant would miss a class), a follow-up phone call by the instructor will occur to determine the reason for missing the class, review any materials that were relevant to the class with the participant, and encourage continued participation
Treatment fidelity and credibility
Adherence to each of the protocols (delivery, receipt and enactment of the MBSR and 10 Keys™ program) will be assessed using a standardized checklist by the Project Manager or PI. Additionally, two of the Co-Investigators (CMG, NG) with expertise in the MBSR program and 10 Keys™ program respectively, met with both program instructors prior to the delivery of the program to answer questions and finalize the programs. They also meet as needed (up to monthly) to review the sessions and answer any questions. Sessions are audio recorded; ten percent of the sessions will be chosen at random and feedback provided to the program teachers by the PI.
3.9. Outcome measures
Outcome measures were chosen to reflect our primary aim of determining the impact of the mind-body program on physical function and pain and our secondary outcome of evaluating the impact of mindfulness meditation on neuropsychological performance. Outcome measures were also chosen because of their demonstrated feasibility, reliability, and validity in older adults with chronic pain. All 300 participants will receive identical pre- and post-treatment assessments. Data will be collected and interviewer-administered by a trained research assistant who is blinded to group assignment. We will use a paperless data management system.
Measures of physical function
Physical function will be assessed using self-reported measures, as well as performance-based measures because of the different strengths of these two approaches. The Roland and Morris Disability Questionnaire (RMDQ) [24] will be our primary outcome measure. It contains 24 questions related specifically to functional limitations as a result of low back pain such as “I change position frequently to try and get my back comfortable” or “Because of my back, I use a hand rail to get upstairs.” A score of 0 means there is no disability due to the back, and a score of 24 means there is severe disability. Normative data have been published for older adults with chronic pain to aid in the interpretation of the RMDQ scores. Mean scores for older adults were around 12 [26]. The RMDQ has been shown to be reliable and valid in community dwelling older adults with CLBP [27]. Internal consistency ranges from 0.87–0.95 [28–29]. Short Physical Performance Battery (SPPB) [30–32] tests lower extremity function by measuring standing balance, gait speed and timed chair rise, tasks that are commonly encountered by older adults. It has been subjected to rigorous psychometric evaluation in numerous populations of older adults. It predicts both risk of disability as well as mortality [31]. The maximum score is 12 and higher scores indicate better function.
Measures of Pain
Numeric Pain Rating Scale (NRS) [33] The 0–20 NRS is a preferred pain measure among older adults and has been found to be sensitive to changes in pain sensation in this population [34–35]. Higher scores indicate worse pain. McGill Pain Questionnaire-Short Form (MPQ-SF) [36] is a widely used, validated and reliable generic pain measure that has been used in an older population. Pain is measured in three domains: sensory, affective and total descriptors. There are 15 questions and higher scores indicate worse pain. Chronic Pain Acceptance Questionnaire [37–38]. It is a 20-item scale that measures acceptance of pain which has been shown to correlate with reports of lower pain intensity and less physical disability. Higher scores indicate greater chronic pain acceptance. Life control, affective distress, pain intensity, and pain interference with daily activities will be measured with the first section of the Multidimensional Pain Inventory [39]. The scale has 8-items and higher scores indicate worse pain.
Measures of Neuropsychological Performance
We will use the Computer-Based Assessment of Mild Cognitive Impairment (CAMCI) [21–22]. The CAMCI collects data in a standardized fashion and resembles a simple screening test that is user-friendly to the older adult. The CAMCI is presented on a tablet PC with touch screen response and takes approximately 30 minutes to complete. It includes an assessment across various cognitive domains including attention, learning, memory, speed, and executive function.
Measures of the Executive Function Domain
Part 2 of the Tracking Test, for this test the computer displays a series of numbers and months in circles and participants are asked to connect the circles on the screen alternating between months forward, January through December, and numbers in reverse order, 12 to 1. The test is scored for number correct and time taken to completion. We chose this test as our primary outcome measure for Specific Aim 2 because it is a measure of executive function.
Go/no go task, where participants are asked to tap the screen twice if they hear one beep and once if they hear two beeps. The rules are then changed and they are asked to tap twice if they hear one beep and do nothing if they hear two beeps. Scores range from 0 to 10 with lower scores indicating poorer executive function.
Reverse digit span, participants hear a series of numbers and are then asked to tap numbers on a display on the bottom of the computer screen in the reverse order. The longest series with at least one correct is the obtained score.
ATM transaction, where participants are shown an ATM-type screen and asked to make a transfer of funds from saving to checking. Number of correct transactions and time are recorded.
Measures of the Attention Domain
Part 1 of the Tracking Test, for this test the computer displays numbers 1 through 22 in circles and the participant is asked to connect the string of 22 numbers in ascending order by taping on the screen. The score is number correct out of 22 and the time taken to completion.
Star task, where respondents are instructed to respond to an infrequently occurring stimulus. Scores are number correct out of 16 targets and median reaction time for correct and incorrect responses.
Digit forward span, participants hear a series of numbers, one per second, and after presentation are asked to tap the numbers in the same order on a number display (1 through 9) presented on the bottom of the computer screen. The longest series with at least one correct is the obtained score.
Measures of Mindfulness
Mindfulness, which is key to the meditation method, remains unexplored in an older population. We will explore this with the Mindful Attention Awareness Scale (MAAS) [40–41]. It measures attention and awareness of present moment experience in daily life. There is a 15-item and 5-item version. The shorter version will be used for the monthly assessments. Higher scores indicate more mindfulness.
Treatment expectancy and credibility
This will be collected to assess if participants perceived the two programs to be of equal face validity. Questions will include participants’ rating of their level of confidence with the treatment, whether they would recommend the treatment to a friend, perceived expertness of the treating clinicians, and expectation of positive treatment outcomes. Participants will also be asked to evaluate their global impression of change at the conclusion of the 8-week program, and at 6 and 12 months follow-up [42].
Monthly evaluation of treatment outcome
To examine the process of change, brief monthly telephone evaluations of important domains (function, pain, mindfulness, health system encounters, medication change, other therapies for pain such as medications, injections, or complementary therapy like chiropractic, acupuncture or yoga) will be conducted for all participants.
3.10. Data Analysis
All analyses for treatment group comparisons will use the original treatment assignment as randomized for each participant (intent-to-treat). To test whether the negative impact of pain on function can be reduced from mindfulness meditation, we will compare average function immediately following completion of the 8-week s time point using a mixed effects model with a fixed effect for intervention group and a random class effect (approximately 16 classes, 8 intervention and 8 control) controlling for baseline function. We are proposing to control for classes as a random effect because we hypothesize that responses immediately following each 8-week program will be correlated for participants that are in the same class. Although we anticipate this correlation among participant responses to be small, we feel it is appropriate to control for this relatedness so that we do not falsely conclude the intervention program is more effective than the control program. The analysis for secondary functional outcomes (SPPB) will follow the same approach as that described for the Roland and Morris. We will also test the immediate intervention effects on measures of pain (NRS< MPQ-SF), psychological function, and neuropsychological function using the same methodology. Each analysis will be conducted at α=0.05 since these measures are secondary to function as measured by the RMDQ.
We will test long term effects of our intervention on function, pain, and psychological function using data immediate post-treatment, 6-months post-treatment, and 12-months post-treatment. Linear mixed models will be used controlling for baseline function. Participant and class will be treated as random effects to control for the correlation among repeated measurements on the same person and correlation among measurements of participants in the same class. We will test for a difference in the change in outcome over time using an interaction term between treatment group and time (immediate post-treatment, 6- and 12-months). We will conduct analyses in an exploratory fashion to check for consistency in intervention effects across potentially moderating variables. Variables to be considered are age, sex, race/ethnicity, education, and IQ.
Improving neuropsychological performance may be one of the mechanisms by which mindfulness meditation works. We will explore these possibilities in our analysis by determining whether baseline attention and executive function predicts outcome in physical function and pain relief, as well as whether change in attention and executive function predicts the same. We propose a mediation analysis as we hypothesize that the effect of mindfulness meditation on physical function is partially mediated by cognitive function. We will use single-mediator and multiple mediator methods incorporating product of coefficients as described by MacKinnon, Fairchild, and Fritz to test for mediation [43]. We will estimate the mediated effect by taking the product of the following coefficients: 1) the coefficient for the intervention effect on executive function, 2) the coefficient for executive function in a model testing the intervention effect on physical function controlling for executive function. This estimate will provide the reduction in the program effect on physical function when adjusted for neuropsychological function. The confidence interval for the mediated effect will be calculated using bootstrap methods. If zero is not contained in the interval, then we would conclude significant mediation exists [44]. We will test for a multiple-mediator model using executive function and attention.
Treatment expectancy
We will directly evaluate participant’s beliefs about the control program and compare them to participants in the intervention program by collecting treatment credibility and expectancy ratings. We do not anticipate any lasting therapeutic effects of the control program on the outcome measures. We do anticipate, however, that placebo and other non-specific effects that commonly result from participation in a group and in research studies will be seen in our participants [45], and that comparison of the control group with the intervention group will help to determine the magnitude of these effects. We will compare baseline measures between non-responders and responders so that future mind-body interventions can be targeted to those most likely to benefit from them.
Power analysis and justification of sample size
We propose to recruit a total of 300 participants (150 per intervention arm) to allow approximately 120 participants per intervention arm available for a complete case analysis (we anticipate 20% attrition at the assessment immediately following the 8 week program sessions based on our pilot work [46–47]). In trials such as ours that are randomized at the individual level but the intervention is delivered in the group setting, there is an anticipated correlation among the outcomes of individuals within the same groups. This violates the assumption of independence used in most statistical methods. A common measure of this correlation is the intraclass correlation coefficient (ρ). Importantly, if we ignore this correlation coefficient we risk being underpowered to detect a meaningful effect [48]. We have no preliminary data to estimate the intraclass correlation for participants within the same group so we have used estimates that have been cited in the literature for human studies. Power analysis was conducted in NCSS/PASS [49] using the cluster randomization algorithm for a two-sample t-test assuming 12–15 class cohort groups per intervention arm and 10 individuals per class. With α=0.05 using a two-sample t-test for clustered randomized trials, adjusted for correlation within groups (ρ=0.01–0.02; for human studies) [50], we have 80–90% power to detect a 2.5 point difference in the Roland and Morris Disability Questionnaire using an average standard deviation of 5.9 from our pilot work (effect size 2.5/5.9=0.42). This sample size is large enough to counter the valid criticism that mind-body studies are underpowered to assess their effects. We will also be able to capture other small effects that would be missed with a smaller sample size.
4. Discussion
Unlike a medication trial with a placebo drug, research participants in group behavioral interventions cannot be blinded to their group assignment. Thus, not only may participants’ expectations influence outcomes, but also the attention and support of the facilitator, as well as the other group participants. To minimize expectancy effects we will present both programs as health education programs that may or may not have an impact on the participant’s back pain. Additionally, we will ask treatment expectancy questions to both groups to evaluate and control for it in data analysis. Although the personality and experience of the facilitators cannot be controlled for, we have specifically recruited expert educators who are enthusiastic about their interventions.
Potential participants may be specifically interested in meditation, as its purported effects on pain and quality of life are frequently reported in popular media. To avoid disappointment in randomization assignment we will describe each program in enough detail during the consent process so that participants can decline to participate if they are not interested.
Program adherence is critical to the success of the study. To encourage this as well as completion of homework assignments (daily meditation for the MBSR group or weekly assignments related to the 10 Keys™), group sessions will stress the importance of homework and group participation.
In conclusion, our trial is the first large, rigorously designed, randomized controlled trial of a mind-body intervention for older adults with chronic low back pain. This population has been largely ignored in mind-body pain research. Chronic low back pain is common among older adults and frequently undertreated. Mind-body therapies have the potential to fill the need for safe treatment of pain in the older adult since they have few side-effects. Mindfulness meditation is particularly well-suited to the older adult both in theory and practice because it addresses the multidimensional nature of pain and its consequences and at the same time is a safe and gentle method that can be taught regardless of age. Despite this promising potential, large, randomized controlled studies have not been done in the older adult with chronic pain to evaluate its effectiveness. If proven effective, this type of intervention could be broadly implemented as an adjunct method to increase function and decrease pain in this population.
Acknowledgements
This work was supported by a grant from the National Institute on Aging r01 AG034078-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Number of older Americans. [Accessed July 19, 2011]; [online] http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2008_Documents/Population.aspx.
- 2.Gibson SJ. IASP global year against pain in older persons: highlighting the current status and future perspectives in geriatric pain. Expert Review of Neurotherapeutics. 2007;7:627–635. doi: 10.1586/14737175.7.6.627. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis & Rheumatism. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Bressler HB, Keyes WJ, Rochon PA, et al. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–1819. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Scudds RJ, Mc DRJ. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain. 1998;75:229–235. doi: 10.1016/s0304-3959(97)00224-8. [DOI] [PubMed] [Google Scholar]
- 6.Walt R, Katschinski B, Logan R, et al. Rising frequency of ulcer perforation in elderly people in the United Kingdom. Lancet. 1986;1:489–492. doi: 10.1016/s0140-6736(86)92940-5. [DOI] [PubMed] [Google Scholar]
- 7.Shorr RI, Griffin MR, Daugherty JR, et al. Opioid analgesics and the risk of hip fracture in the elderly: codeine and propoxyphene. Journal of Gerontology. 1992;47:M111–M115. doi: 10.1093/geronj/47.4.m111. [DOI] [PubMed] [Google Scholar]
- 8.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delacorte; 1990. [Google Scholar]
- 9.Newman AB, Bayles CM, Milas CN, et al. The 10 keys to healthy aging: Findings from an innovative prevention program in the community. Journal of Aging and Health. 2010;22:547–566. doi: 10.1177/0898264310363772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- 11.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J, Lipworth L, Burney R, et al. Four-Year Follow-Up of a Meditation-Based Program for the Self-Regulation of Chronic Pain: Treatment Outcomes and Compliance. The Clinical Journal of Pain. 1986;2:159–173. [Google Scholar]
- 13.Pradhan EK, Baumgarten M, Langenberg P, et al. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis & Rheumatism. 2007;57:1134–1142. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- 14.Teasdale JD, Segal ZV, Williams JM, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting & Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 15.Speca M, Carlson LE, Goodey E, et al. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine. 2000;62:613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Carlson LE, Ursuliak Z, Goodey E, et al. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Supportive Care in Cancer. 2001;9:112–123. doi: 10.1007/s005200000206. [DOI] [PubMed] [Google Scholar]
- 17.Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cognitive, Affective & Behavioral Neuroscience. 2007;7:109–119. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- 18.Wenk-Sormaz H. Meditation Can Reduce Habitual Responding. Advances in Mind-Body Medicine. 2005 Fall-Winter;Vol 21(3–4):33–49. 2005. [PubMed] [Google Scholar]
- 19.Karp JF, Reynolds CF, Butters MA, et al. The Relationship Between Pain and Mental Flexibility in Older Adult Pain Clinic Patients. Pain Medicine. 2006;7:444–452. doi: 10.1111/j.1526-4637.2006.00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merrill SS, Seeman TE, Kasl SV, et al. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–M26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 21.Saxton J, Morrow L, Baumann S, et al. Presentation to the international Neuropsychological Society. St. Louis: 2005. The Computer-Based Assessment of Mild Cognitive Impairment (CAMCI) [Google Scholar]
- 22.Morrow L, Saxton J, Snitz E, et al. Use of computer-based assessment of mild cognitive impairment in primary care physician offices. Presentation to the 15th annual meeting of the Society for Prevention Research; Washington, DC. 2007. [Google Scholar]
- 23.Heymans MW, van Tulder MW, Esmail R, et al. Cochrane Database of Systematic Reviews. 2004. Back schools for non-specific low-back pain. Art. No: CD000261. [DOI] [PubMed] [Google Scholar]
- 24.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting & Clinical Psychology. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- 26.Nicholas MK, Asghari A, Blyth FM. What do the numbers mean? Normative data in chronic pain measures. Pain. 2008;134:158–173. doi: 10.1016/j.pain.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 27.Weiner D, Pieper C, McConnell E, et al. Pain measurement in elders with chronic low back pain: traditional and alternative approaches. Pain. 1996;67:461–467. doi: 10.1016/0304-3959(96)03150-8. [DOI] [PubMed] [Google Scholar]
- 28.Turner JA, Fulton-Kehoe D, Franklin G, et al. Comparison of the Roland-Morris Disability Questionnaire and generic health status measures: a population-based study of workers' compensation back injury claimants. Spine. 2003;28:1061–1067. doi: 10.1097/01.BRS.0000062007.95197.08. discussion 1067. [DOI] [PubMed] [Google Scholar]
- 29.Stratford PW, Binkley JM. A comparison study of the back pain functional scale and Roland Morris Questionnaire. North American Orthopaedic Rehabilitation Research Network. J Rheumatol. 2000;27:1928–1936. [PubMed] [Google Scholar]
- 30.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 31.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 32.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–661. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herr KA, Spratt K, Mobily PR, et al. Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clinical Journal of Pain. 2004;20:207–219. doi: 10.1097/00002508-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Herr K, Mobily P, Richardson G. Use of experimental pain to compare psychometric properties and usability of pain scales in the adult and older adult populations. Paper presented at: Annual Meeting of the American Society for Pain Management in Nursing; Orlando, FL. 1998. [Google Scholar]
- 35.Chibnall JT, Tait RC. Pain assessment in cognitively impaired and unimpaired older adults: a comparison of four scales. Pain. 2001;92:173–186. doi: 10.1016/s0304-3959(00)00485-1. [DOI] [PubMed] [Google Scholar]
- 36.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 37.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107:159–166. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 38.McCracken LM, Eccleston C. Coping or acceptance: what to do about chronic pain? Pain. 2003;105:197–204. doi: 10.1016/s0304-3959(03)00202-1. [DOI] [PubMed] [Google Scholar]
- 39.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 40.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality & Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 41.Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. Journal of Psychosomatic Research. 2005;58:29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 42.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy & Experimental Psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 43.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 45.Price DD, Milling LS, Kirsch I, et al. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147–156. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- 46.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134:310–319. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morone NE, Rollman BL, Moore CG, et al. A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain Medicine. 2009;10:1395–1407. doi: 10.1111/j.1526-4637.2009.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pals SL, Murray DM, Alfano CM, et al. Individually randomized group treatment trials: a critical appraisal of frequently used design and analytic approaches. American Journal of Public Health. 2008;98:1418–1424. doi: 10.2105/AJPH.2007.127027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hintze J. NCSS, PASS, and GESS. Kaysville, UT: NCSS; 2007. [Google Scholar]
- 50.Killip S, Mahfoud Z, Pearce K. What Is an Intracluster Correlation Coefficient? Crucial Concepts for Primary Care Researchers. Ann Fam Med. 2004;2:204–208. doi: 10.1370/afm.141. [DOI] [PMC free article] [PubMed] [Google Scholar]