Abstract
Physical and verbal assaults by residents on care staff are not uncommon in long-term residential care facilities (LTCs). This research evaluated an Internet training designed to teach Nurse Aides (NAs) strategies to work with aggressive resident behaviors. Six LTCs were randomized in an immediate treatment (IT) and delayed treatment (DT) design, and NAs were recruited in each (IT: n = 58; DT; n = 45). The treatment involved two weekly visits to the on-line training. Hard copy assessments collected participant responses at baseline (T1), 8 weeks (T2), and at 16 weeks (T3). The DT group viewed the program after T2. HLM models show significant group differences at T2 in knowledge and the levels were maintained at T3. The number of aggressive incidents reported per day by the IT group were non-significant at T2, but decreased significantly from T1 to T3 with a very large effect size. The program was well received by users. These results suggest that the Internet training was an effective tool to reduce assaults in LTCs, and training effects may improve over time as NAs gain experience using the techniques.
Keywords: resident aggression, training, Internet, Nurse Aides, long term care, nursing homes
Introduction
Physical and verbal assaults against direct care workers in LTCs and hospital Emergency Departments (ED) occur frequently.1–4 Reportable injuries in the previous year, including scratches and cuts, bruises, and human bites were reported by more than half of CNAs in the National Nursing Assistant Survey,5 and by 35% in another study.6 Gates, Fitzwater, and Succop7 reported that 138 NAs incurred an average of 4.69 reportable assaults during 80 work hours, with a range of 0–67 assaults, and a study of 76 NAs at six LTCs reported a median of 26 aggressive incidents over a two-week period, and other research suggests that approximately 95% of incidents are probably undocumented.8
Whether or not an injury was sustained, after an assault NAs9 and ED workers2 experience increased anger, stress, job dissatisfaction, decreased feelings of safety, and fear of future assaults. In one study, diagnosable post traumatic stress disorder (PTSD) symptoms were found among 17% of ED health care workers after assaults, and 15% may have experienced suppressed functioning of their immune system.10 Some research indicates that after violent experiences, health care providers may avoid patients who might be violent,1, 11 which would necessarily lead to a decrease in quality of resident care in LTCs.
Staff training might help mitigate the impact of violence in LTCs, but NAs typically receive limited or no behavioral training to work with resident behaviors.5, 12–14 Instead, problematic resident behaviors are too often treated with psychotropic medications or restraint, while behavioral remedies are underutilized. 15–17 The limited research available on aggression management programs is focused on institutional settings, especially psychiatric units, with nurses identified as the population most at risk of violence.12, 18 In a meta analysis of 29 aggression management programs, which averaged 18 hours per year, Livingston et al.,12 reported that the aggression training programs lacked standardization, and may or may not reduce patient initiated violence, but they did appear to reduce use of restraint and coercive techniques by staff.
A grant from the National Institute on Aging provided funding to develop an Internet based training program to help NAs prevent or, if necessary, deal with aggressive resident behaviors. A prototype training of fundamental communication skills showed promising results,19 but follow-up assessments or training on how to react to violent behaviors was lacking. The research described here redesigned the prototype19 and added advanced skills training to help NAs deal with assaults including hits, grabs, and hair pulls. The Internet training was tested in LTCs, as reported here, and on-line with a sample recruited entirely on the Web.20
The program evaluation goals were to measure changes in: a) appropriate behavioral and communication techniques for working with residents who display aggressive behaviors, b) knowledge of how to react to aggressive behaviors, c) attitudes, self-efficacy, and empathy regarding aggressive resident behaviors, and d) frequency of assaults reported by NAs. Additionally we sought to measure user acceptance of the training.
Design and Methods
Research Design and Overview
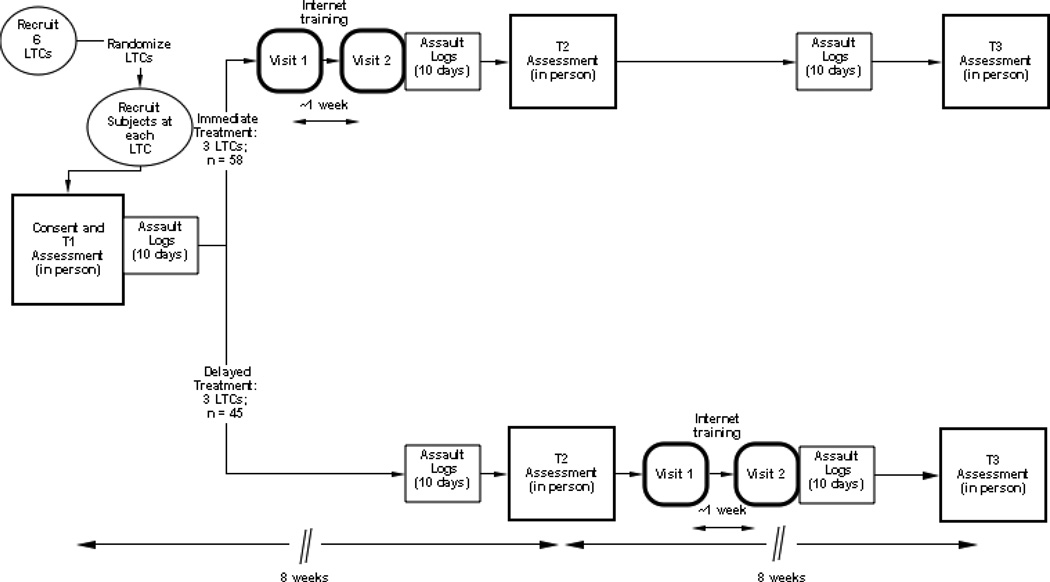
This research was conducted in six LTCs, randomized into immediate treatment (IT) and delayed-treatment (DT) conditions with LTC as the unit of randomization (see Figure 1). Six LTCs were recruited for the study in Cincinnati, Ohio. As described below, participants were recruited in each building. Participants met in groups to fill out a hard copy consent and assessment at baseline (T1). For the next 10 work days, all participants were asked to fill out Assault Logs (AL), which were brief records that detailed aggressive acts by residents. Participants in the IT Group then were asked to make two visits to view the intervention program, approximately one week apart. Immediately after the last program visit by the IT group, all participants were asked to again fill out the ALs on 10 work days. Approximately 4 weeks later, and 8 weeks after T1, all subjects met in groups to fill out a second hard copy assessment (T2). The DT group then visited the training program twice, one week apart, after which all subject filled out ALs on 10 work-days. Four weeks later, and approximately 16 weeks after T1, all subjects met in groups to complete a third assessment (T3).
Figure 1.
Research design for Internet training program evaluation.
The Intervention: Caring Skills: Dealing with Aggression
The Internet intervention, which has been described elsewhere,20 was developed with a National Institute on Aging grant. It consists of a series of courses, with extensive use of video for narration and behavior modeling demonstrations by paid actors, including right-way, wrong-way exemplars. NA models used positively oriented non-punitive redirection strategies designed to promote safety for both the NA and the resident. On-screen text, in the form of short titles, bulleted phrases, questions, and explanations, was written at 2nd– 6th grade reading level. Users moved between web pages by mouse-clicking “next” buttons, and answered text questions by clicking on radio buttons. Except for log-in, keyboarding was not required.
Visit 1 courses were designed to provide fundamental de-escalation skills with residents exhibiting aggressive behavior. Video vignettes (e.g., reacting to an agitated resident) were supplemented by narration and by supportive testimonials. The NA video models demonstrated fundamental techniques of an intervention strategy called the A.I.D.19, 21
Visit 2 offered advanced skills in four courses (About Hits, Hits With Fists or Arms, Hair Grabs, Wrist Grabs) that applied the A.I.D. principles to more extreme situations. The Visit 2 courses taught situation-specific advanced skills for dealing with hair grabs, attacks with fists, and wrist-grabs. Video modeling of key skills was performed by a psychiatric social worker who holds a black belt in Aikido.
Procedures
By agreement with the participating LTCs, all study activities were to be conducted on the employees’ own time (i.e., before or after work; on days off). Two computers were purchased by the research team and connected to the Internet in a private space reserved for the research. Each building provided additional meeting space to administer assessments.
After approval by an Institutional Review Board, a total of 11 local Research Assistants (RAs) and a Research Coordinator were hired to facilitate the research. Each completed the online NIH Human Subjects training course. They were directly supervised by co-authors EF and DG. RAs assisted with recruitment, assessment meetings and computer training visits, and they made reminder phone calls to participants the day before each research activities.
Recruitment
In each building, NAs were recruited from all shifts using flyers, payroll check inserts, announcements at staff meetings, and word of mouth advertising. RAs made multiple visits during shift changes to answer questions and encourage participation. An 800 telephone number to call was included on all recruiting materials, and NAs were also offered the opportunity to receive a call if they provided their phone number to an RA or a supervisor. Potential participants were all interviewed by telephone by the grant team’s coordinator to qualify for the study. Participants were required to be working at least 16 hours per week in one of the participating buildings. Once qualified, participants scheduled study activities (i.e., three assessments, two computer visits) at convenient times from among 4–6 available appointments. RAs made reminder phone calls the day before appointments. Participants who missed an appointment were contacted by telephone and rescheduled.
Approximately 335 NAs were employed across the six buildings when the research commenced. A total of 132 NAs were enrolled, and of those, 103 attended the first meeting to sign the informed consent and fill out the T1 assessment.
Assessments
Participants were offered a choice of times and dates to fill out assessments in supervised group settings in each of the six LTCs. RAs were available to provide assistance and answer questions, while providing privacy for the participants filling out the forms. The decision to conduct group meetings for assessments was made to assure that the participants would receive immediate help if they should experience difficulties reading or understanding the research instrument.
At their initial appointment, participants first signed an informed consent. The T1 assessment was identical for all participants. At T2, which was eight-weeks after T1, the assessment for the IT group contained additional items to measure viewer program acceptance. At T3, which was eight weeks after T2 and 16 weeks after T1, the DT group responded to the same additional items to measure viewer program acceptance.
At the T1 assessment meeting, participants also received instructions for use of ALs and a 10 day supply of cards. All participants were mailed packets of ALs thereafter (see Figure 1).
Internet program visits
After T1 assessments, IT Group participants were scheduled to use the Internet training program at two visits, one week apart. An RA provided computer orientation (e.g., login; mouse use; navigation instructions) and remained available if participants needed assistance. The two computers were in proximity, but they were positioned to minimize visual distraction to adjacent users. Headphones were provided to minimize sound distractions. At the end of their second computer program visit, users received a certificate of completion detailing subject matter and total viewing time. Users were encouraged to show the certificate to their supervisor for possible training credit. After T2 assessments, the DT Group used the Internet training program following procedures identical to those for the IT group. After T3, the Internet training was made available to all employees at all six LTCs for three months, with use supported by building supervisors.
Participants were paid by check after completing each assessment and computer visit, and in advance for ALs. They were paid $50 each for attending meetings to respond to T1 and T2, and $60 for T3 ($50 + $50 + $60 = $160).Participants were paid $20 at each visit to use the training program (2 × $20 = $40). AL participants were paid $25 in advance, at each time a AL card-packet was distributed (3 × $25 = $75).
Measures
The measurement instrument in this research was adapted from those developed used by Irvine et al.19, 20 which showed adequate reliability and validity. One section of the instrument used program specific items to measure changes in constructs associated with behavior change.22–24 Another section utilized video situational testing (VST)19, 25, 26 to probe NA knowledge and self efficacy to respond to simulated aggressive events. To minimize testing reactivity effects, the VSTs were presented only at T2 and T3. A third section assessed user acceptance of the website by sampling perceptions about the impact and value of the training program. At T2 (IT Group) and T3 (DT Group), participants also responded to items assessing their satisfaction with the training program and its functionality.
Self-efficacy
Eleven items assessed participant confidence to apply the concepts taught in the program (e.g., How confident are you in your ability to redirect a resident who is acting aggressively?). Response options were recorded on a 7-point Likert scale (1 = not at all confident, 7 = extremely confident). A mean composite score computed across the eleven items showed excellent internal reliability (α = .90) and test-retest reliability in the delayed treatment condition from T1 to T2 (r = .30).
Empathy
One item from the Personal Accomplishment scale27 was used to assess empathy and compassion. Participants were asked how much they agreed or disagreed with the following statement: “Even if a resident sometimes is verbally or physically aggressive towards me, I can easily understand how he/she feels about things.” Response options were on a 7-point Likert scale (1 = completely disagree, 7 = completely agree).
Attitudes
One item developed for the study asked about the participant’s attitude towards a resident’s aggressive behavior. Participants were asked how much they agreed or disagreed with the following statement “I believe that residents act aggressively because they have unmet needs.” Response options were on a 7-point Likert scale (1 = completely disagree, 7 = completely agree).
VST self-efficacy
A total of fourteen items were used to assess a participant’s level of confidence in their ability to successfully perform their NA duties if confronted with situations modeled in seven separate video vignettes (e.g., resident swings cane, which endangers nearby resident; agitated resident grabs another on a sofa). Response options were recorded on a 7-point Likert scale (1 = not at all confident, 7 = extremely confident). A mean composite score computed across the eleven items showed excellent reliability (α = .93) and good test-retest reliability in the IT group from T2 to T3 (r = .90).
VST knowledge
Using the same seven video situations, ten items assessed participant knowledge of recommended practices, and three items assessed knowledge of photos showing correct and incorrect ways to respond to physical aggression from a resident (i.e., how a NA might physically respond to having hair grabbed by a resident: 1 correct and 2 incorrect photos). The number of correct items was summed and divided by thirteen to indicate total percent of knowledge items correct. Good test-retest reliability in the IT group from T2 to T3 (r = .74),
Assault Logs
Study participants were asked to document physical or verbal assaults they experienced from residents. At each reporting period (see Figure 1), NAs were given packets of ALs with instructions and a sample filled-in AL. The ALs, adapted from Gates et al.,9 were 4”× 6” cards designed so NAs could quickly record assaults by checking boxes on the card or supplying short answers. AL entries included time incident occurred, resident’s gender and race/ethnicity, physical assault (i.e., use of an object, grab/pinch, hair pull, hit/slap, scratch/bite, kick, spit), and verbal assault (i.e., verbal threat, insult/sex talk), CNAs also recorded on the card each day the total hours they worked, number of residents cared for, and number of assaults that day. The NAs were asked to place their completed ALs in a locked box at the end of each shift. The assault data were inspected by one of the co-authors (EF), and then for analysis were converted to number of physical and verbal assaults experienced in an eight-hour workday.
User acceptance
Items to gauge user acceptance of the website were included on the T2 assessment for IT participants, and on the T3 assessment for the DT group. The items were adapted from instruments used in our previous Website evaluation research.20, 25, 26 Users were asked to agree or disagree with statements by responding on a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree). Eight Program Value items elicited responses regarding the program as a training tool (i.e., understandable, of interest, applicable, learned a lot, videos helpful, good use of time, easy to use, better compared to an inservice). Seven other Program Impact items were designed to measure the users’ perception of the program’s effect on them. The stem was, “If my employer made this training about how to manage aggressive resident behaviors available to all company employees…” Items mentioned included safety, job satisfaction, feeling cared about, positive feelings towards the company, commitment to the company, care for residents, and personal productivity. Two additional items asked users to rate the training program on a 7-point scale (1 = not at all; 7 = extremely positive) in terms of user satisfaction (“Overall, how satisfied were you with the training website?”) and recommend-ability (“How likely is it that you would recommend the training site to a co-worker?”).
Data Analysis
The three panel randomized group IT vs. DT design with crossover after the T2 assessment (Figure 1) allowed for evaluation of several effects: (a) between-subject evaluation of immediate program effects from T1 to T2 for the survey measures and ALs, and VST measures at T2 only, (b) within-subject IT maintenance of program effects from T1 to T3 for the survey measures, and ALs; VST measures from T2 to T3, and (c) within-subject DT replication of program effects from T2 to T3.
To account for the intra-correlation between nested units all models were conducted in a hierarchical linear model framework (HLM)28 with participants (level-1) nested within facility (level-2). A random intercept model with a mean centered level-1 covariate (i.e., the pre-intervention score) was used to assess outcomes that were measured prior to the intervention. Program effects that included VST outcomes assessed only post-intervention did not require a level-1 covariate and were thus modeled with a simple random intercept model. The models included study condition (coded 0 = delayed treatment and 1 = immediate treatment) as a level-2 predictor of the intercept. The level-2 coefficient associated with study condition represents the change of the immediate treatment group relative to the delayed treatment group and was used to test the hypothesis that the immediate treatment condition outperformed the delayed treatment condition. A simple random intercept model of change scores, defined as post-intervention minus pre-intervention scores, were used to assess the within-subject maintenance of effects for the immediate treatment group and replication of effects for the delayed treatment group. The intercept coefficient represents the amount of change over time in the study outcome and was used to test the hypothesis that the change was statistically greater than zero. Rates of missing data ranged from 0% – 21%, thus we used maximum likelihood estimates to impute missing data, as it produces more accurate and efficient parameter estimates than listwise deletion or last-observation-carried-forward.29 In addition to the statistical significance of each finding, the effect size, which is a measure of the strength of each finding, is also provided. A partial correlation coefficient, based on t values and degrees of freedom30 are provided as an estimate of the effect size. The following convention is used when interpreting the partial regression coefficient (pr): .14 is equal to a small effect, .36 a medium effect, and .51 a large effect.
Results
Baseline Equivalency and Attrition Analyses
Demographic characteristics (Table 1) and baseline assessments (Table 2) were compared across treatment condition to demonstrate group equivalency. No significant differences were found (p<.05) suggesting randomization produced initially equivalent groups. Of the 103 study participants 70 (69%) completed all three assessment surveys, 17 (17%) two surveys, and 15 (15%) one survey. Participants who completed all three surveys were compared to those who completed one or two surveys on study condition, demographic characteristics, and all T1 outcome measures. Attrition was not significantly related to any of the measures suggesting dropping out of the study did not bias results.
Table 1.
Demographic Characteristics by Study Condition
| Immediate Treatment (n=58) | Delayed Treatment (n=45) | |||
|---|---|---|---|---|
| N | % | N | % | |
| Sex (% female) | 45 | 77.6 | 44 | 97.8 |
| Age | ||||
| 18–20 years old | 29 | 50.0 | 26 | 57.8 |
| 21–35 years old | 9 | 15.5 | 8 | 17.8 |
| 36–45 years old | 7 | 12.1 | 5 | 11.1 |
| 46–55 years old | 2 | 3.4 | 6 | 13.3 |
| 55 or older | 1 | 1.7 | 0 | 0.0 |
| Did not respond | 10 | 17.2 | 0 | 0.0 |
| Race | ||||
| Black or African American | 35 | 60.3 | 24 | 53.3 |
| White or Caucasian | 11 | 19.0 | 20 | 44.4 |
| Mixed race /other | 2 | 3.4 | 0 | 0.0 |
| Did not respond | 10 | 17.2 | 1 | 2.2 |
| Annual household income | ||||
| Less than $20,000 | 17 | 29.3 | 6 | 13.3 |
| $20,000–$39,999 | 24 | 41.1 | 29 | 64.4 |
| $40,000–$59,999 | 6 | 10.3 | 6 | 13.3 |
| $60,000–$79,999 | 0 | 0.0 | 1 | 2.2 |
| More than $80,000 | 0 | 0.0 | 1 | 2.2 |
| Did not respond | 11 | 19.0 | 2 | 4.4 |
| Highest level of education | ||||
| Less than high school diploma | 4 | 6.9 | 1 | 2.2 |
| High school diploma or GED | 22 | 37.9 | 17 | 37.8 |
| Some college | 22 | 37.9 | 24 | 53.3 |
| College degree | 0 | 0.0 | 2 | 4.4 |
| Did not respond | 10 | 17.2 | 1 | 2.2 |
Table 2.
Descriptive Statistics for Study Outcomes
| Treatment (n=58) | Delayed Treatment (n=45) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Self-efficacy | 5.46 | 0.93 | 5.59 | 1.02 | 5.86 | 1.20 | 5.47 | 0.78 | 5.52 | 0.84 | 5.89 | 1.04 |
| Empathy | 5.19 | 1.38 | 5.43 | 1.27 | 5.74 | 1.02 | 5.31 | 1.29 | 5.20 | 1.27 | 5.96 | 0.88 |
| Attitudes | 4.57 | 1.70 | 5.44 | 1.61 | 5.86 | 1.10 | 4.93 | 1.59 | 5.02 | 1.79 | 5.98 | 1.16 |
| VST Self-efficacy | NA | NA | 5.40 | 1.14 | 5.45 | 1.37 | NA | NA | 4.92 | 1.00 | 5.42 | 1.30 |
| VST Knowledge | NA | NA | 0.54 | 0.24 | 0.56 | 0.26 | NA | NA | 0.38 | 0.19 | 0.59 | 0.25 |
| Incidents per day | 0.50 | 0.49 | 0.41 | 0.57 | 0.09 | 0.25 | 0.50 | 0.60 | 0.41 | 0.57 | 0.34 | 0.52 |
M = mean, SD = standard deviation, VST = video situation test, NA = not applicable.
Main Effects
The top panel of Table 3 shows the results of the immediate effects of the online program using T1–T2 comparisons. Results from the HLM models show significant and large group differences at T2 in VST knowledge, with the IT condition showing greater knowledge. No other significant T1–T2 effects were found, although, a trend level effect is found for VST self-efficacy (p = .086) that corresponds to a large effect size (pr = .74).
Table 3.
Results of Immediate (top panel), Maintenance (middle panel), and Replication of Study Effects (bottom panel).
| Immediate Effects (IT Group, T1–T2) | |||||
|---|---|---|---|---|---|
| Coefficient | SE | t-value | p-value | pr | |
| Self-efficacy | 0.07 | 0.13 | 0.44 | .683 | .21 |
| Empathy | 0.23 | 0.30 | 0.77 | .484 | .36 |
| Attitudes | 0.52 | 0.34 | 1.52 | .202 | .61 |
| VST Self-efficacy | 0.47 | 0.22 | 2.23 | .086 | .74 |
| VST Knowledge | 0.16 | 0.04 | 3.58 | .036 | .87 |
| Incidents per day | −0.01 | 0.13 | −0.02 | .984 | .01 |
| Maintenance Effects (IT Group, T1–T3) | |||||
| Coefficient | SE | t-value | p-value | pr | |
| Self-efficacy | 0.39 | 0.15 | 2.58 | .084 | .88 |
| Empathy | 0.55 | 0.20 | 2.82 | .099 | .89 |
| Attitudes | 1.22 | 0.35 | 3.47 | .188 | .92 |
| VST Self-efficacy (T2–T3) | 0.05 | 0.10 | 0.51 | .662 | .34 |
| VST Knowledge (T2–T3) | 0.02 | 0.04 | 0.48 | .677 | .32 |
| Incidents per day | −0.41 | 0.09 | −4.83 | .044 | .96 |
| Replication Study, (DT Group, T2–T3) | |||||
| Coefficient | SE | t-value | p-value | pr | |
| Self-efficacy | 0.37 | 0.13 | 2.87 | .105 | .90 |
| Empathy | 0.76 | 0.21 | 3.66 | .193 | .93 |
| Attitudes | 0.96 | 0.24 | 4.02 | .164 | .94 |
| VST Self-efficacy | 0.50 | 0.23 | 2.17 | .121 | .84 |
| VST Knowledge | 0.21 | 0.03 | 6.17 | <.001 | .97 |
| Incidents per day | −0.07 | 0.08 | −0.79 | .513 | .49 |
Notes. Degrees of freedom were 4 for the immediate study effects, 2 for tests of maintenance effects, and 2 for tests of replication effects.
SE = standard error,
pr = partial regression coefficient, an estimate of effect size; .14 = small, .36 = medium, large = .51. 28
The middle panel of Table 3 shows the results for the maintenance of effects analyses (T2–T3) for the IT condition. The intercept coefficient from the VST knowledge model (0.02) indicates the IT condition stayed approximately the same from T2 to T3 lending support to the maintenance of knowledge gained. There was a significant decrease from T2 to T3 in the number of assaults reported per day, with a very large effect size of .96.
The bottom panel of Table 3 shows the results for the replication of study effects on the DT group. VST knowledge increased significantly from T2 to T3 with a large effect size. The 21% increase is of similar magnitude to the 16% difference between the IT-DT groups measured at T2. No other significant replication effects were found.
Program Usage and Dose Response
Most participants made a special trip each time to visit the training program, usually on a day off, while some made the visits before or after their shift. A total of 13 participants (14%) had difficulty using the computer mouse and needed initial assistance. Most of those expressed apprehension at using the computer.
At Visit 1, most IT participants (n=50, 86%) viewed both courses, and the remainder (n=8, 14%) did not see either course. The average amount of time spent at Visit 1 was 46.2 minutes (SD=22.1). At Visit 2, most IT participants (n=48, 83%) viewed all four courses, 1 (2%) viewed one course, and 9 (16%) did not view any course. The average amount of time spent at Visit 2 was 26.8 minutes (SD=13.6). The average amount of time spent on the program, across Visit 1 and 2 was 73.1 minutes (SD = 34.7 minutes).
At Visit 1, most DT participants (n=39, 87%) viewed both courses, and the remainder (n=6, 13%) did not see either course. The average amount of time spent at Visit 1 was 45.8 minutes (SD=18.9). At Visit 2, most DT participants (n=37, 82%) viewed all four courses, 1 (2%) viewed three courses, and 7 (16%) did not view any course. The average amount of time spent at Visit 2 was 27.3 minutes (SD=12.6). The average amount of time spent on the program, across Visit 1 and 2 was 73.2 minutes (SD = 30.7 minutes). The IT and DT participants did not statistically differ (at p<.05) on the amount of time using the program.
To assess dose response, change scores (defined as the posttest measure minus the pretest measure) from the survey measures and VST self-efficacy and knowledge scores at T2 for the IT group and T3 for the DT group were correlated with total time of program use. Effect sizes in the small to medium range were found between time of program usage and improvement in self-efficacy (r = .18, p = .064) and attitudes (r = .17, p = .089). Time spent using the program was also correlated with the post intervention scores for VST knowledge (r = .31, p = .002); a medium effect size. Taken together results suggest treatment participants who invested more time using the program showed modest increases in study outcomes compared to participants who used the program less.
User acceptance
A mean score of 4.47 (SD = 0.45), computed across the eight Program Value items (Table 4), indicated that participants agreed to a high degree that the program was a valuable training tool. A mean Program Impact score of 4.16 (SD = 0.58) across the seven impact items indicated the participants agreed or strongly agreed that the program would have a positive effect on them. Responses averaged 6.1 (SD = 0.8) to the user satisfaction items, and 6.3 (SD = 0.9) for the would-recommend item, suggesting high user acceptance.
Table 4.
Program acceptance scores: Usability, and Impact
| Strongly disagree |
Disagree | Neither agree nor disagree |
Agree | Strongly agree |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | M | SD | |
| Program Usability | ||||||||||||
| Everything is easy to understand. | 1 | 2.2 | 3 | 6.5 | 3 | 6.5 | 22 | 47.8 | 17 | 37.0 | 4.11 | 0.95 |
| The training program has much that is of interest to me. | 0 | 0.0 | 0 | 0.0 | 1 | 2.2 | 25 | 55.6 | 19 | 42.2 | 4.40 | 0.54 |
| I can apply the training content to my job. | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 19 | 41.3 | 27 | 58.7 | 4.59 | 0.50 |
| I learned a lot from the training. | 0 | 0.0 | 0 | 0.0 | 2 | 4.3 | 15 | 32.6 | 29 | 63.0 | 4.59 | 0.58 |
| The video scenes in the training helped me learn. | 0 | 0.0 | 0 | 0.0 | 2 | 4.3 | 21 | 45.7 | 23 | 50.0 | 4.46 | 0.59 |
| Using the training website was a good use of my time. | 0 | 0.0 | 0 | 0.0 | 2 | 4.3 | 18 | 40.0 | 25 | 55.6 | 4.51 | 0.59 |
| The training website was easy to use. | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 15 | 32.6 | 31 | 67.4 | 4.67 | 0.47 |
| Compared to an in-service on a similar topic, I learn more using a training website like this. | 0 | 0.0 | 1 | 2.2 | 5 | 11.1 | 13 | 28.9 | 26 | 57.8 | 4.42 | 0.78 |
| Impact | ||||||||||||
| “If my employer made this training about how to manage aggressive resident behaviors available to all company employees …” | ||||||||||||
| I would feel safer on the job. | 0 | 0.0 | 0 | 0.0 | 4 | 8.7 | 27 | 58.7 | 15 | 32.6 | 4.24 | 0.60 |
| I would feel more satisfied with my job. | 0 | 0.0 | 0 | 0.0 | 4 | 8.7 | 28 | 60.9 | 14 | 30.4 | 4.22 | 0.59 |
| I would feel like my company cares about me. | 1 | 2.2 | 0 | 0.0 | 6 | 13.0 | 24 | 52.2 | 15 | 32.6 | 4.13 | 0.81 |
| I would feel more positive about my company. | 1 | 2.2 | 0 | 0.0 | 7 | 15.6 | 21 | 46.7 | 16 | 35.6 | 4.13 | 0.84 |
| I would feel a greater commitment to my company. | 1 | 2.2 | 0 | 0.0 | 12 | 26.1 | 19 | 41.3 | 14 | 30.4 | 3.98 | 0.88 |
| I would be able to provide better care for the residents. | 0 | 0.0 | 1 | 2.2 | 4 | 8.7 | 26 | 56.5 | 15 | 32.6 | 4.20 | 0.69 |
| I would be more productive at my job. | 0 | 0.0 | 0 | 0.0 | 7 | 15.2 | 21 | 45.7 | 18 | 39.1 | 4.24 | 0.71 |
M = mean, SD = standard deviation.
Discussion
The results from this randomized Internet trial in LTC settings suggest that the Internet training had a positive and meaningful impact on the NAs. Knowledge significantly increased for the IT group, with effects maintained 16 weeks after the T1 assessment. While not significant, IT group scores for self efficacy, empathy, and attitude improved from T2 to T3 (Table 2), with very large effect sizes (Table 3). DT group scores for self efficacy, empathy, and attitudes, while also not significant at T3, showed improvement from T2 with very large effect sizes, and mean values at T3 were comparable to those of the IT group at T3 (Table 2). Further, dose response analysis suggests a modest causal relationship between program viewing time and improved scores. These results provide strong support for previous studies which have shown the effectiveness of Internet training programs for NAs.19–21, 31–34 They extend understanding about maintainence effect from Internet training ,which previously were only reported by one study,20 and that was for only 8 weeks.
The incidence of assaults diminished significantly for the IT group at T3 (i.e., 16 weeks after T1; 13 weeks after training), with a very large effect size, and the DT group showed non-significant improvement with a medium effect size at T3 (i.e., 6 weeks after training; Table 3). We believe that this type of behavioral evidence is important to support the other outcomes. Too often in our view, researchers mistakenly equate changes in knowledge and psycho-social measures with changes in behavior or skills, but without supportive behavioral results. This research supports the efficacy of the training program to decrease the incidence of assaults, which has only been reported previously in a LTC by a pilot study.35 The significant decrease in assaults from T2–T3 suggests that with time and experience using the training techniques, the NAs continued to benefit from the training. Our results seem to suggest that the training helped the NAs to prevent residents from becoming aggressive. By responding effectively and appropriately to aggressive behavior, the NAs may have prevented situations from escalating into truly assaultive incidents. In sum, by providing behavioral data, the research reported here supports previous research20 of the benefits of an Internet training specifically to address aggressive behaviors, and we extend to 16 weeks the period to which Internet training effects may be shown.
The incidence of resident aggression at baseline, as indicated by assault logs in this research, is similar to that reported in the literature. Incidents in this research of .50 incidents/day per NA (Table 2), calculate to 2.5/5-day work-week. Gates et al.7 reported an incidence of 4.69 reportable assaults during 80 work hours, amounting to roughly 2.35/5-day work-week. Snyder et al.8 reported a median of 26 incidents in 2 weeks, or 2.6/5-day work-week, but suggested that 95% of incidents were unreported. Thus, this study is consistent with other research in documenting the high rate of aggressive/assaultive behavior that is present in the LTC work environment.
Training acceptance, as show by mean Program Value and Program Impact scores, were 4.47 and 4.42 respectively on a scale of five, which is quite high. A national sample of NAs, who were not paid for using the same Internet training program, gave it similarly high value and impact scores of 4.5 and 4.2 respectively.20 Thus, the NAs from the research reported here, some of whom were initially inexperienced with computers, rated the Website about the same as a national population of NAs who were presumably more experienced computer users. While these are speculative self-report measures, they indicate solid user approval of the Web training program.
While the results of this research are positive, the findings from the online study,20 which used the same measures, found stronger effects across a wider array of measures. In that study, significant effects in self efficacy and attitudes were maintained for eight weeks, with empathy showing a positive trend (p=.07). VST scores for self efficacy and knowledge were significant with moderate and very large effect sizes respectively. Several factors might help explain the difference between the online study20 and that reported here. We speculate that the research reported here might have shown more statistically significant effects had the sample size been larger. Using the LTCs as the unit of randomization and analysis reduced the statistical power of the analysis. The fact that the NAs in this research usually made a special trip to their LTC to participate in research activities might also have been a factor, and the effect of gathering in groups to fill in assessments cannot be determined. Different exposure to the intervention program might also have been influential. Program visits by the IT group in this research totaled 73 minutes (SD = 34.7 minutes), with 14% and 16% failing to visit the training program at Visit 1 and 2 respectively. In contrast, in the online study,20 where participants were not paid for program visits, total Visit 1–2 time averaged 97 minutes (SD = 46.9 minutes), all subjects viewed at least one of the two Visit 1 courses, and only 10% failed to view any of the Visit 2 courses. All of these issues, plus demographic differences in the NA populations might have played a factor. Compared to the online study, the NAs in this research were significantly (p<.05) younger, ethnically diverse, had lower annual incomes, and less education. At baseline, they had significantly higher levels of self-efficacy, and lower levels of VST knowledge at baseline compared to the online sample.
Limitations of the research include the measurement of assaults, and limited duration of follow-up interval (i.e., 16 weeks) to evaluate maintenance of program effects. Given the decrease in assaults over time, perhaps more than 16 weeks may be needed to fully realize the training effects on the incidence of assaults, and even more time would be needed to determine if the levels were maintained. Also, the ALs were self-report measures and the definition of an assault may vary by individuals, so our findings should be viewed with caution pending further research. Additionally, single items were used to measure empathy and attitudes, suggesting the need for further research of these constructs with LTC staff.
This on-site study and our earlier the online study20 are early efforts to document maintenance effects of Web-based training, but more research on longer-term impact, supported by in vivo observations, is clearly needed. Whether these results would generalize to all employees if the Internet training were integrated into the training regime at each LTC is also unclear. Also unknown is whether the same results would be achieved in other regions, and with a different cultural mix of NAs. Finally, we are aware of no research into how to integrate most effectively an Internet based training curriculum into a LTCs training regime.
Limitations notwithstanding, this research provides support to studies demonstrating the benefits of Internet training for NAs,19–21, 25, 31–34 and provides new evidence for maintenance of training effects. This research, supported by the online study,20 provides evidence of the beneficial effects of training to help NAs react to resident behaviors which might escalate into assaults. The functionality of the program was satisfactory, and more importantly, users valued it to the extent that they viewed their employer more favorably, and they felt it made them more productive and better caregivers.
If Internet training is to be integrated into an LTC environment, a model that is different from the traditional in-service training will need to be embraced.20 The automation associated with internet programming is appealing because it is less trainer-intensive to implement, and trainee viewing time and comprehension are easily monitored by supervisors. Individuals potentially can be pulled briefly from caregiving duties without the need to arrange for group inservice meetings, which thus simultaneously removes a sizeable number of NAs from care giving duties. Web training also offers the potential for brief retraining or refresher courses for individuals, which are not otherwise readily available within an in-service-based training model. In addition, Web training offers opportunity for orientation of new employees to normalize expectations of employee behavior at the LTC. Valuable group discussions are also practical. We believe that discussions are likely to be even more effective after the users has been exposed to the content and can talk about how to best apply the knowledge. Using a projector connected to the Internet program, a trainer could review key points and engage a group discussion, or an on-line discussion might be facilitated in a college setting. For instance, a hair-grab scene from the training program might be displayed, and a discussion might cover how to avoid the situation, or to protect the worker without endangering the resident. And discussion might include an employer’s policies on calling for help, and how to report assaults. The trainer might also lead a brief practice session on specific techniques demonstrated in the video modeling scenes (e.g., escaping from a resident hair grab or arm-hold; when to call for help).
Admittedly, transition to technology-based training will take time for some LTC settings. Few online NA training programs are yet available, and few LTCs are architecturally designed to accommodate computerized training. Movement in this direction, however, seems inevitable, with some signs that it is already happening. Golden Living Inc., a national chain of LTCs and assisted living facilities already uses touch screens in hallways for NAs to record caregiving activities and resident behaviors on MDS 3.036 data templates (ABI, personal observation). In a pilot study reported elsewhere, an LTC purchased two computers, connected to the Internet via the cable TV provider, and conducted an Internet dementia training for all non-caregiving staff.37 While the adoption of new training technology may be slowed by space limitations, cost constraints, and reluctance to change existing policies or training models, we think that the benefits will outweigh these barriers. Since use of computers is becoming more commonplace in schools, we believe that delays in adopting the technology are more likely to be due to organizational resistance and infrastructure, rather than to the learners.
Research indicates that NAs want training to deal with abusive residents,38 and that perceptions of adequate training can improve job satisfaction,38, 39 which in turn has been linked to job commitment and retention.2, 8, 40–42 Consistent provision of appropriate training is an important element of the culture change movement43, 44 to improve care giving, and to decrease violence towards staff.8, 12, 18 LTCs that adopt culture change models benefit by experiencing reduced worker turnover, higher occupancy rates, and improved competitiveness in the market place.45, 46
If only for training NAs to deal safely and respectfully with aggressive resident behaviors, the need is clear,1–8 but well researched effective training models have not been forthcoming.12 Both residents and caregiving staff will benefit from more effective staff training.
Acknowledgements
This research was funded by a grant from the National Institute on Aging (R44AG024675). This project required the efforts of a multidisciplinary team. Bess Day led on evaluation logistics. Program development involved Gretchen Boutin, Carol Dennis, Vicky Gelatt, Elizabeth Greene, Rob Hudson, Beth Machamer, James Madson, Dave Merwin, Nick Martini, Percy Perez-Pinedo, Diana Robson, Jeremy Russell, Tammy Salyer, Ellen Seigel, Marni Stamm, and Jay Thompson. John Booker, CNA, Jeff Beatty, Evelyn Fitzwater, DSN, Donna Gates, EdD, Christine Osterberg, RN, Joanne Rader, RN, Pat Sheehan, Lisa Stratton, Robin Wagner, PhD, and Lucy Willis, PhD. consulted on behavioral issues and presentation integrity. Peter Sternberg LCSW was the Akido expert and video trainer for advanced behavioral responses to resident aggression. Jeff Gau conducted the statistical analyses. Dennis Ary, Evelyn Fitzwater, and Donna Gates and Ann Glang made helpful comments on earlier versions of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
REFERENCES
- 1.Gates DM, Fitzwater E, Meyer U. Violence against caregivers in nursing homes. Expected, tolerated, and accepted. [Accessed Apr.];J Gerontol Nurs. 1999 25(4):12–22. doi: 10.3928/0098-9134-19990401-05. http://www.slackjournals.com/jgn. [DOI] [PubMed] [Google Scholar]
- 2.Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emerg Med. 2006 Oct;31(3):331–337. doi: 10.1016/j.jemermed.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Zeller A, Hahn S, Needham I, Kok G, Dassen T, Halfens RJ. Aggressive behavior of nursing home residents toward caregivers: a systematic literature review. Geriatr Nurs. 2009 May–Jun;30(3):174–187. doi: 10.1016/j.gerinurse.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Shaw MM. Aggression toward staff by nursing home residents: findings from a grounded theory study. J Gerontol Nurs. 2004;30(10):43–54. doi: 10.3928/0098-9134-20041001-11. http://www.slackjournals.com/jgn. [DOI] [PubMed] [Google Scholar]
- 5.Squillace MR, Remsburg RE, Harris-Kojetin LD, Bercovitz A, Rosenoff E, Han B. The National Nursing Assistant Survey: improving the evidence base for policy initiatives to strengthen the certified nursing assistant workforce. Gerontologist. 2009 Apr;49(2):185–197. doi: 10.1093/geront/gnp024. [DOI] [PubMed] [Google Scholar]
- 6.Tak S, Sweeney MH, Alterman T, Baron S, Calvert GM. Workplace assaults on nursing assistants in US nursing homes: A multilevel analysis. Am J Public Health. 2010;100:1938–1945. doi: 10.2105/AJPH.2009.185421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gates D, Fitzwater E, Succop P. Relationships of stressors, strain, and anger to caregiver assaults. Issues Ment Health Nurs. 2003 Dec;24(8):775–793. [PubMed] [Google Scholar]
- 8.Snyder LA, Chen PY, Vacha-Haase T. The underreporting gap in aggressive incidents from geriatric patients against certified nursing assistants. Violence Vict. 2007;22(3):367–379. doi: 10.1891/088667007780842784. [DOI] [PubMed] [Google Scholar]
- 9.Gates DM, Fitzwater E, Deets C. Testing the reliability and validity of the assault log and violence prevention checklist. Journal of Gerontological Nursing. 2003;29:18–23. http://www.slackjournals.com/jgn. [Google Scholar]
- 10.Gates DM, Gillespie GL, Succop P. Violence against nurses and its impact on stress and productivity. [Accessed Mar–Apr];Nurs Econ. 2011 29(2):59–66. quiz 67. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=21667672. [PubMed] [Google Scholar]
- 11.Gillespie GL, Gates DM, Miller M, Howard PK. Violence against healthcare workers in a pediatric emergency department. Advanced Emergency Nursing Journal. 2010;32(1):68–82. [Google Scholar]
- 12.Livingston JD, Verdun-Jones S, Brink J, Lussier P, Nicholls T. A narrative review of the effectiveness of aggression management training programs for psychiatric hospital staff. J Forensic Nurs. 2010 Spring;6(1):15–28. doi: 10.1111/j.1939-3938.2009.01061.x. [DOI] [PubMed] [Google Scholar]
- 13.Molinari VA, Merritt SS, Mills WL, et al. Serious mental illness in Florida nursing homes: need for training. Gerontol Geriatr Educ. 2008;29(1):66–83. doi: 10.1080/02701960802074321. [DOI] [PubMed] [Google Scholar]
- 14.Glaister JA, Blair C. Improved education and training for nursing assistants: keys to promoting the mental health of nursing home residents. Issues Ment Health Nurs. 2008 Aug;29(8):863–872. doi: 10.1080/01612840802182912. [DOI] [PubMed] [Google Scholar]
- 15.Brooker D. Person-Centred Dementia Care: Making Services Better. London: Jessica Kingsley Publishers; 2007. [DOI] [PubMed] [Google Scholar]
- 16.Donat DC, McKeegan C. Employing behavioral methods to improve the context of care in a public psychiatric hospital: some applications to health care management. Psychiatr Rehabil J. 2003 Fall;27(2):177–181. doi: 10.2975/27.2003.178.181. [DOI] [PubMed] [Google Scholar]
- 17.Kolanowski A, Fick D, Frazer C, Penrod J. It's about time: use of nonpharmacological interventions in the nursing home. J Nurs Scholarsh. 2010 Jun;42(2):214–222. doi: 10.1111/j.1547-5069.2010.01338.x. [DOI] [PubMed] [Google Scholar]
- 18.Farrell G, Cubit K. Nurses under threat: a comparison of content of 28 aggression management programs. Int J Ment Health Nurs. 2005 Mar;14(1):44–53. doi: 10.1111/j.1440-0979.2005.00354.x. [DOI] [PubMed] [Google Scholar]
- 19.Irvine AB, Bourgeois M, Billow M, Seeley JR. Internet training for nurse aides to prevent resident aggression. Journal of the American Medical Director's Association. 2007 Oct;8(8):519–526. doi: 10.1016/j.jamda.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Irvine AB, Billow M, Gates D, Fitzwater E, Seeley JR, Bourgeois M. Internet Training to Respond to Aggressive Resident Behaviors. The Gerontologist. doi: 10.1093/geront/gnr069. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irvine AB, Billow MB, Bourgeois M, Seeley JR. Mental illness training for long term care staff. Journal of the American Medical Director's Association. doi: 10.1016/j.jamda.2011.01.015. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bandura A. Principles of Behavior Modification. New York: Holt, Rinehart and Winston; 1969. [Google Scholar]
- 23.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 24.Fishbein M. The role of theory in HIV prevention. AIDS Care. 2000;12(3):273–278. doi: 10.1080/09540120050042918. [DOI] [PubMed] [Google Scholar]
- 25.Irvine AB, Ary DV, Bourgeois MS. An interactive multimedia program to train professional caregivers. Journal of Applied Gerontology. 2003;22(2):269–288. [Google Scholar]
- 26.Irvine AB, Philips L, Duncan S, Seeley J, Wyant R, Moore RW. A web program that improves sedentary employee exercise behavior. Am J Health Promotion. 2011;25(3):199–206. doi: 10.4278/ajhp.04121736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ray E, Miller K. Social support, home/work stress, and burnout: Who can help? Journal of Applied Behavioral Science. 1994;30(3):357–373. [Google Scholar]
- 28.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage Publications Inc; 2002. [Google Scholar]
- 29.Schafer J, Graham J. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 30.Rosenthal R, Rubin DB. r equivalent: A simple effect size indicator. Psychol Methods. 2003 Dec;8(4):492–496. doi: 10.1037/1082-989X.8.4.492. [DOI] [PubMed] [Google Scholar]
- 31.Hobday JV, Savik K, Smith S, Gaugler JE. Feasibility of Internet training for care staff of residents with dementia: the CARES program. J Gerontol Nurs. 2010 Apr;36(4):13–21. doi: 10.3928/00989134-20100302-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacDonald C, Stodel E, Casimiro L. Online dementia care training for healthcare teams in continuing and long-term care homes: A viable solution for improving quality of care and quality of life for residents. International Journal on E-Learning. 2006;5(3):27. http://www.aace.org/pubs/ijel/. [Google Scholar]
- 33.Rosen J, Mulsant BH, Kollar M, Kastango KB, Mazumdar S, Fox D. Mental health training for nursing home staff using computer-based interactive video: a 6-month randomized trial. Journal of the American Medical Directors Association. 2002;3(5):291–296. doi: 10.1097/01.JAM.0000027201.90817.21. [DOI] [PubMed] [Google Scholar]
- 34.Breen A, Swartz L, Flisher AJ, et al. Experience of mental disorder in the context of basic service reforms: the impact on caregiving environments in South Africa. Int J Environ Health Res. 2007 Oct;17(5):327–334. doi: 10.1080/09603120701628388. [DOI] [PubMed] [Google Scholar]
- 35.Fitzwater E, Gates D. Testing an intervention to reduce assaults on nursing assistants in nursing homes: A pilot study. Geriatric Nursing. 2002;23(1):18–23. doi: 10.1067/mgn.2002.122800. [DOI] [PubMed] [Google Scholar]
- 36.Pate T, editor. Long-Term Care Facility Resident Assessment Instrument User’s Manual Version 3.0. Baltimore, MD: Centers for Medicare & Medicaid Services; 2010. [Google Scholar]
- 37.Irvine AB, Beatty JA, Seeley JR. Non-Direct Care Staff Training to Work with Residents with Dementia. Health Care Management Review. 2011 manuscript submitted. [Google Scholar]
- 38.Sengupta M, Harris-Kojetin LD, Ejaz FK. A national overview of the training received by certified nursing assistants working in U.S. nursing homes. Gerontol Geriatr Educ. 2010;31(3):201–219. doi: 10.1080/02701960.2010.503122. [DOI] [PubMed] [Google Scholar]
- 39.Noelker LS, Ejaz FK, Menne HL, Bagaka's JG. Factors affecting frontline workers' satisfaction with supervision. J Aging Health. 2009 Feb;21(1):85–101. doi: 10.1177/0898264308328641. [DOI] [PubMed] [Google Scholar]
- 40.Institute of Medicine. [Accessed April 28, 2010];Retooling for an Aging America: Building the Health Care Workforce. 2008 http://www.nap.edu/catalog/12089.html. [PubMed]
- 41.Yeatts DE, Cready C, Swan J, Shen Y. The perception of "training availability" among certified nurse aides: relationship to CNA performance, turnover, attitudes, burnout, and empowerment. Gerontol Geriatr Educ. 2010;31(2):115–132. doi: 10.1080/02701961003795722. [DOI] [PubMed] [Google Scholar]
- 42.Rosen J, Stiehl EM, Mittal V, Leana CR. Stayers, leavers, and switchers among certified nursing assistants in nursing homes: A longitudinal investigation of turnover intent, staff retention, and turnover. The Gerontologist. 2011 doi: 10.1093/geront/gnr025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Noland M. Successful ageing: Keeping the “person” in person-centered care. British Journal of Nursing. 2001;10(7):450–454. doi: 10.12968/bjon.2001.10.7.5330. http://www.britishjournalofnursing.com/. [DOI] [PubMed] [Google Scholar]
- 44.McCormack B. Person-centredness in gerontological nursing: an overview of the literature. J Clin Nurs. 2004 Mar;13(3a):31–38. doi: 10.1111/j.1365-2702.2004.00924.x. [DOI] [PubMed] [Google Scholar]
- 45.Crandall LG, White DL, Schuldheis S, Talerico KA. Initiating person-centered care practices in long-term care facilities. [Accessed Nov.];J Gerontol Nurs. 2007 33(11):47–56. doi: 10.3928/00989134-20071101-08. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18019118. [DOI] [PubMed] [Google Scholar]
- 46.Doty M, Koren M, Sturla E. [Accessed September 26, 2011];Culture Change in Nursing Homes: How Far Have We Come? Findings From The Commonwealth Fund 2007 National Survey of Nursing Homes. 2008 http://www.commonwealthfund.org/Publications/Fund-Reports/2008/May/Culture-Change-in-Nursing-Homes--How-Far-Have-We-Come--Findings-From-The-Commonwealth-Fund-2007-Nati.aspx.