Abstract
Individuals with elevated social anxiety appear especially vulnerable to cannabis-related problems, yet little is known about the antecedents of cannabis-related behaviors among this high-risk population. The present study used ecological momentary assessment (EMA) to examine the relations among social anxiety, cannabis craving, state anxiety, situational variables, and cannabis use in the natural environment during ad-lib cannabis use episodes. Participants were 49 current cannabis users. During the two-week EMA period, social anxiety significantly interacted with cannabis craving to predict cannabis use both cross-sectionally and prospectively. Specifically, individuals with higher social anxiety and craving were most likely to use cannabis. There was a significant social anxiety X state anxiety X others’ use interaction such that when others were using cannabis, those with elevations in both trait social anxiety and state anxiety were the most likely to use cannabis.
Keywords: social anxiety, state anxiety, cannabis, marijuana, craving, ecological momentary assessment
1. Introduction
People with social anxiety disorder (SAD) appear particularly vulnerable to cannabis use disorders (CUD). Compared to those without SAD, adolescents with SAD show nearly five times greater risk of developing adult cannabis dependence after controlling for other anxiety disorders, depression, and other relevant Axis I psychopathology (Buckner et al., 2008). When accounting for covariance among internalizing disorders, SAD emerges as the only internalizing disorder related to cannabis problems (Buckner, Mallott, Schmidt, & Taylor, 2006; Buckner et al., 2008). Further, studies using continuous measures of social anxiety also find a positive, significant relationship between social anxiety and cannabis-related problems (Buckner, Bonn-Miller, Zvolensky, & Schmidt, 2007; Buckner, Heimberg, Matthews, & Silgado, in press; Buckner, Heimberg, & Schmidt, 2011; Buckner & Schmidt, 2008; Marmorstein, White, Loeber, & Stouthamer-Loeber, 2010). The relationship between social anxiety and cannabis problems remains even after controlling for relevant variables such as other substance use, other types of anxiety, depression, and delinquency (Buckner, Bonn-Miller et al., 2007; Buckner & Schmidt, 2009; Buckner, Schmidt, Bobadilla, & Taylor, 2006; Marmorstein et al., 2010).
Despite the high rates of cannabis-related problems among those with elevated social anxiety, the nature of this relationship is poorly understood. Consistent with motivational models of substance use (e.g., Baker, Piper, McCarthy, Majeskie, & Fiore, 2004), it is assumed that people with elevated social anxiety use cannabis to reduce anxiety in social situations. Supporting this idea, using cannabis to manage social anxiety is related to greater cannabis use and use-related problems (Lee, Neighbors, Hendershot, & Grossbard, 2009). Cannabis users with elevated social anxiety report using cannabis to manage negative affect and to avoid social scrutiny (Buckner, Bonn-Miller et al., 2007). Further, using cannabis to manage negative affect mediated the relationship between social anxiety and cannabis-related problems in that study.
The majority of the extant research in this area is limited by the use of retrospective accounts of reasons for cannabis use. Three experimental studies offer a more controlled account of the relations between social anxiety and cannabis use. Consistent with retrospective reports, those with SAD (but not those without SAD) reported greater desire to use cannabis during (though not before or after) a social stressor (i.e., speech) task (Buckner, Silgado, & Schmidt, 2011). Among cannabis abstainers, those with SAD who received cannabidiol (CBD; an active component of cannabis) reported significantly less of an increase in state social anxiety during (but not before or after) a speech task compared to individuals with SAD who received placebo (although anxiety reported by those with SAD who received CBD was significantly greater than that reported by non-anxious controls) (Bergamaschi et al., 2011). CBD resulted in decreases in state anxiety following (though not during) a speech task in healthy volunteers (Zuardi, Cosme, Graeff, & Guimarães, 1993). Taken together, these studies suggest that individuals with higher trait social anxiety may be especially vulnerable to using cannabis during social situations rather than when alone in anticipation of the situation (to manage anticipatory anxiety or to enter the situation already intoxicated) or following the situation (to manage post-event processing, found to be related to distress among socially anxious indivduals; for review see Dannahy & Stopa, 2007).
One limitation to this body of work is that participants were never truly alone during these situations (as they were monitored by study staff) so it remains unclear whether socially anxious individuals are vulnerable to using cannabis when alone. A second limitation is that participants either did not use cannabis or did not choose when to receive CBD during these tasks. Thus, it remains unclear whether participants actually use cannabis during social situations and if so whether they do so to manage unpleasant negative affective states. This literature also is limited by the use of laboratory methods that may dramatically impact the ecological validity of the findings. Thus, further elucidation of the circumstances in which socially anxious individuals are vulnerable to using cannabis in more naturalistic settings could have important treatment and prevention implications.
The use of ecological momentary assessment (EMA) in prospective designs is one way to further elucidate the relations between social anxiety and cannabis use. EMA involves daily monitoring of target behaviors. Some of the key benefits of EMA include: (1) collection of data in real-world environments, thereby enhancing ecological validity; (2) minimization of retrospective recall bias by assessing relations between affective states and behaviors while participants experience the affect and/or engage in the targeted behavior; and (3) aggregation of observations over multiple assessments to facilitate within-subject assessments of behaviors across time and context (Shiffman, Stone, & Hufford, 2008).
We know of no studies using EMA to examine the affective and situational antecedents and correlates of cannabis use among socially anxious individuals. We recently found that concerns regarding the social consequences of anxiety symptoms (anxiety sensitivity [AS] social concerns) moderated the relation between cannabis craving and use (Buckner, Zvolensky et al., 2011). In that study, AS-social concerns was the only AS facet to have an interactive effect on cannabis use (i.e., fears of physical or mental/psychological consequences of anxiety did not interact with craving to predict use), suggesting that fears regarding social scrutiny may be especially important in cannabis use behaviors. Therefore, the present study aims to extend these findings by testing whether social anxiety more broadly interacted with cannabis craving and state anxiety to predict cannabis use using real-world data about ad-lib cannabis use episodes during a two-week EMA monitoring period. We also tested whether social anxiety would interact with situation type (alone vs social situation) to predict use. In light of data suggesting that social anxiety is related to conformity cannabis use motives (Buckner, Bonn-Miller et al., 2007), we also examined whether social anxiety would interact with others’ use to predict participant use.
We examined these relationships among undergraduates, a population ideally suited for studying the relationships between social anxiety and cannabis-related behaviors given that young adults broadly and college students specifically appear vulnerable to cannabis use and cannabis-related problems (Caldeira, Arria, O’Grady, Vincent, & Wish, 2008; Johnston, O’Malley, Bachman, & Schulenberg, 2007). In fact, the rate of cannabis use is increasing among college students but not same age, non-college peers (Substance Abuse and Mental Health Services Administration, 2010). Furthermore, the transition from high school to college is associated with increased social anxiety (Spokas & Heimberg, 2009) and elevated social anxiety and SAD are associated with cannabis-related problems in undergraduate samples (Buckner, Bonn-Miller et al., 2007; Buckner, Heimberg et al., in press; Buckner, Heimberg et al., 2011; Buckner, Mallott et al., 2006; Buckner & Schmidt, 2008, 2009; Buckner, Schmidt et al., 2006). The use of a non-clinical sample allows for the examination of these relationships among current users to provide insight into affective and situational variables that may play a role in maintaining cannabis use.
2. Method
2.1 Participants and Recruitment
Participants were recruited from October 2006-April 2008 based on responses to a mass screening assessing current (any past three months) cannabis use. Of the 3,200 undergraduates screened, 44.1% endorsed current cannabis use and were invited via email to participate. Of the 60 prospective participants that came to the laboratory and were assessed for eligibility, 3 were excluded because they denied lifetime cannabis use during the appointment, 3 were excluded due to non-availability of personal digital assistants (PDAs) at the time of their appointment, 1 was excluded due to loss of his PDA, and 4 were not compliant with EMA protocol (information regarding compliance provided below). The final sample was comprised of 49 (38.8% female) participants aged 18–22 years (M=19.14, SD = 1.02). Participants reported using cannabis an average of 5–6 times a week in the past three months with 40.1% reporting daily cannabis use and only 12.2% reporting less than weekly use.
Regarding prevalence of current DSM-IV diagnoses1, 63% met criteria for a current CUD (26.5% met criteria for cannabis abuse, 36.7% met criteria for cannabis dependence), 51.0% met for an alcohol use disorder (36.7% met for alcohol abuse), 6.1% had a non-cannabis illicit substance use disorder, and 2.0% had major depressive disorder. Regarding anxiety disorders, 20% had SAD, 2.0% had panic disorder, 6.1% had obsessive-compulsive disorder, and 2.0% had generalized anxiety disorder. Comorbidity was common with 51.0% meeting criteria for more than one disorder. The racial/ethnic composition of the sample was: 2.0% American Indian, 83.7% Caucasian, 2.0% Hispanic/Latino, 10.2% mixed, and 2.0% other.
2.2 EMA Assessments
EMA data were collected via PDAs that were manufactured by Palm® (Z22 Handheld). Data were collected using forms created with Satellite Forms 5.2 developed by Pumatech. EMA data collection included three types of EMA assessments (Wheeler & Reis, 1991). First, participants completed signal contingent assessments in which they completed assessments upon receipt of PDA signal. Participants were signaled six semi-random times throughout the day. The timing of the signal was determined randomly to be within +/− 17 min of each of six anchor times distributed evenly throughout the day (between 10:00 a.m. and midnight). Second, participants completed interval contingent assessments in which they completed assessments at the end of day (i.e., bedtime). Third, participants completed event contingent assessments in which they completed assessments each time they used cannabis. Assessments were automatically date and time stamped. Participants were presented with the same questions regardless of assessment type.
2.2.1 Craving
Participants were asked: “Please indicate how much you are craving cannabis by tapping the number which best corresponds to your urge to use cannabis RIGHT NOW.” The item was rated from 0 (No Urge) to 10 (Extreme Urge). This scale has been used in prior studies of cannabis craving (Buckner, Silgado et al., 2011) and was strongly correlated with the four factors of Marijuana Craving Questionnaire (MCQ; Heishman, Singleton, & Liguori, 2001): compulsivity (r = .51, p<.001), emotionality (r = .50, p<.001), expectancy (r = .65, p<.001), and purposefulness (r = .66, p<.001).
2.2.2 State Anxiety
State anxiety was assessed using a Subjective Units of Distress (SUDS; Wolpe, 1968) in which participants were asked to “Please indicate your current level of anxiety by circling the number that best corresponds with the way you are feeling RIGHT NOW” from 0 (Totally relaxed, on the verge of sleep) to 10 (The highest anxiety you have ever experienced). Similar SUDs ratings have been used in prior studies (e.g., Buckner, Silgado et al., 2011; Kocovski & Rector, 2008).
2.2.3 Situation Type and Others’ Cannabis Use
Participants were asked to choose whether they were in a “Social Situation (with other people)” or “Alone (not in a situation with other people)”. If Social Situation was selected, participants were asked if other people were using or about to use cannabis.
2.2.4 Self Cannabis Use
Participants were asked to indicate if they were about to use cannabis (yes or no).
2.3 Procedure
The study was approved by the Florida State University’s (FSU) Institutional Review Board prior to data collection. Participants met individually with a trained clinical interviewer who obtained informed consent. Current DSM-IV diagnostic status was determined via clinical interview using the Anxiety Disorders Interview Schedule-IV-L (ADIS; DiNardo, Brown, & Barlow, 1994). The ADIS, a structured diagnostic interview, has been shown to be a reliable and valid measure of DSM-IV mood and anxiety disorders (T. A. Brown, DiNardo, Lehman, & Campbell, 2001). Interviews were conducted by trained graduate students under the supervision of the fourth author, a licensed clinical psychologist. Percent agreement between these clinical interviewers conducing ADIS interviews in our FSU laboratory during this time period for another study was found to be over 80% (Buckner & Schmidt, 2009).
Participants then completed a battery of self-report measures including the Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998), a measure of general social interaction fears. The SIAS demonstrates high levels of internal consistency and test-retest reliability across clinical, community, and student samples (Mattick & Clarke, 1998; Osman, Gutierrez, Barrios, Kopper, & Chiros, 1998). Individuals with SAD score higher than individuals with other anxiety disorders and non-anxious individuals on this measure (E. J. Brown et al., 1997). In the present sample, the SIAS demonstrated excellent internal consistency (α= .96). Depression was assessed using the Beck Depression Inventory-II (Beck, Steer, & Brown, 1996). Although the BDI is not indicative of the full clinical syndrome of depression, it has yielded adequate reliability estimates, and is a well-validated as a measure of depressive Symptomatology (Beck, Epstein, Brown, & Steer, 1988; Beck & Steer, 1987). The BDI demonstrated adequate reliability in the present sample (α = .93). State anxiety was measured with the State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). This scale has been found to demonstrate good internal consistency, test-retest reliability, and convergent validity with other measures of anxiety (STAI; Spielberger et al., 1983). The STAI-S demonstrated adequate reliability in the present sample (α = .87).
Participants were trained on the use of the PDA. The three types of EMA assessments were explained and participants were instructed not to complete assessments when it was inconvenient (e.g., while in class) or unsafe (e.g., while driving). In these instances, they were asked to respond to PDA signals within one hour if possible. Participants were also given a handout that included the date for their second appointment (described below) and printed instructions of how to use the PDA for their reference during the monitoring period.
During the 14-day monitoring period, participants were sent daily e-mails reminding them to complete the day’s assessments (including a reminder of all three assessment types). Participants’ second appointment occurred two weeks after their initial appointment to return the PDA. During the second appointment, they were debriefed, given research credit, and provided local cannabis treatment referrals.
2.4 Statistical Analysis
Hypotheses were evaluated using a series of generalized linear mixed-effects models with binary logistic response functions. All models included a random effect for subject and fixed effects for other predictors. Independent variables were centered by subtracting the grand mean from each individual score. Models included the main effects as well as the interaction term. The cross-sectional and prospective relationships of anxiety and cannabis craving to cannabis use were then evaluated in three separate ways. First at the daily level, mixed effects models were used to examine whether social anxiety (SIAS scores) interacted with cannabis craving or state anxiety (SUDS) to differentiate cannabis use days from non-use days. Because many of the participants completed assessments in the early morning hours (between midnight and 5:00AM), a new day was defined as beginning at 7:00AM. Data were aggregated by participant and day, thereby creating an average craving and SUDS rating for each participant on each day. Days were dummy coded (0=non-cannabis day, 1= cannabis use day). Next at the momentary level, generalized linear models with a logistic response function were used to evaluate whether SIAS scores interacted with craving or SUDS to predict use at a momentary level (i.e., whether SIAS scores X craving/SUDS at each assessment point predicted cannabis use at that assessment point). Then at the antecedent level, models comparable to those above evaluated whether SIAS scores interacted with craving or SUDS at one assessment point to predict cannabis use at the subsequent assessment. Specifically, SIAS scores X cannabis craving at one assessment point was used to predict cannabis use at the next assessment; and SIAS scores X SUDS at one assessment point was used to predict cannabis use at the next assessment. Pseudo R-squared values were calculated using error terms from the unrestricted and restricted models as described by Kreft and de Leeuw (1998).
As previously reported (Buckner, Crosby, Silgado, Wonderlich, & Schmidt, in press; Buckner, Zvolensky et al., 2011), participants completed a mean of 61% (SD=26%; range=2%–96% per participant) of random assessments and 64% (SD=19%; range=21%–93% per participant) of end of day assessments. In line with prior work (Hopper et al., 2006), we retained data from participants with at least 20% compliance rates. The final sample (N = 49) completed 4,069 signal contingent assessments (M=83.19, SD= 3.33 per participant), 518 interval contingent assessments (M=10.73, SD= 3.50 per participant), and 452 event contingent assessments (M=10.75, SD= 10.05 per participant). Participants recorded a total of 732 cannabis use entries (M=16.26, SD= 15.08 per participant), recorded using all three assessment types. Participants reported an average of 1.33 (SD=1.63) cannabis use episodes per day. Signal contingent assessments were completed on average 14.8 (SD=62.5) minutes after the signal occurred2. Cannabis craving ratings by date per participant ranged from 0–10 (M = 3.19, SD = 2.22) and SUDS ratings by date per participant ranged from 0–8.5 (M = 2.15, SD = 1.49).
3. Results
3.1 Baseline Variables’ Relationships with State Anxiety, Craving, and Cannabis Use during the Monitoring Period
Participants who reported daily cannabis use at baseline were significantly more likely to use cannabis during the monitoring period, β = 1.024, SE = .086, p < .001. They also reported higher craving during the monitoring period, β = 0.991, SE = .033, p < .001. Baseline state anxiety (STAI) was significantly related to SUDS during the monitoring period, β = .010, SE = .002, p < .001.
Baseline SIAS scores were related to greater SUDS during the monitoring period, β = .022, SE = .010, p = .036. SIAS scores were unrelated to cannabis use frequency, β = −.003, SE = .003, p = .250, and cannabis craving, β = −.004, SE = .017, p = .805, during the monitoring period. Baseline depression was unrelated to SUDS, β = .019, SE = .021, p = .373, cannabis use, β = .005, SE = .005, p = .312, and cannabis craving, β = .022, SE = .035, p = .520. Gender was related to SUDS, β = .817, SE = .319, p = .014, but was unrelated to cannabis use, β = .106, SE = .085, p = .215, and cannabis craving, β = .740, SE = .539, p = .176, during the monitoring period.
3.2 Social Anxiety X Cannabis Craving in the Prediction of Cannabis Use3
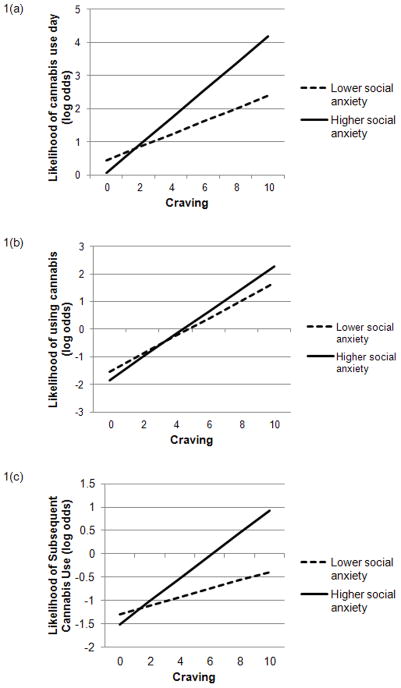
We next examined whether SIAS scores moderated the relations between cannabis craving and use to determine whether those with greater craving and greater trait social anxiety would be the most likely to use cannabis. The first two analyses examined the cross-sectional relations between the SIAS scores X craving interaction and cannabis use. First, we examined whether the SIAS scores X mean craving interaction predicted cannabis use days versus non-use days. This interaction was significant, β = 0.007, SE = .001, p < .001, pseudo R2 = .088. Effect size estimates suggest that the main effects accounted for 8.1% of the variance in cannabis use day status (pseudo R2 = .081) with the interaction accounting for an additional 0.6%. As evidenced in Figure 1a, elevations in both SIAS scores and state cannabis craving were associated with greater likelihood of a cannabis use day. To further clarify the nature of the interaction, tests of simple slopes were conducted (see Aiken & West, 1991; Holmbeck, 2002). The simple slopes were significant for both high social anxiety (β = 0.42, p < .001) and low social anxiety (β = 0.19, p < .001), suggesting that greater craving was related to greater odds of experiencing a cannabis use day for those with high and low social anxiety.
Figure 1.
Trait social anxiety X cannabis craving predicting cannabis use at the daily (1a), momentary (1b), and antecedent (1c) levels.
Second, the momentary relations between the SIAS scores X mean craving interaction and cannabis use were examined. The SIAS scores X craving interaction was significant, β = 0.003, SE = .001, p = .018, pseudo R2 = .307. The main effects accounted for 30.4% of the variance in cannabis use day status with the interaction accounting for an additional 0.3%. Inspection of the graph (Figure 1b), suggesting that individuals with higher SIAS scores and higher craving were the most likely to use cannabis. The simple slopes were significant for both high social anxiety (β = 0.41, p < .001) and low social anxiety (β = 0.32, p < .001).
At the antecedent level, the SIAS scores X craving interaction significantly predicted subsequent cannabis use, β = 0.005, SE = .001, p < .001, pseudo R2 = .106. The main effects accounted for 8.9% of the variance in subsequent cannabis use with the interaction accounting for an additional 1.7%. Inspection of the graph (Figure 1c) suggests that individuals with higher SIAS scores and elevated craving were the most likely to subsequently use cannabis. The simple slopes were significant for both high social anxiety (β = 0.23, p < .001) and low social anxiety (β = 0.09, p < .001).
3.3 Social anxiety X State Anxiety in the Prediction of Cannabis Use3, 4
We next examined whether social anxiety moderated the relations between SUDS and cannabis use to determine whether those with greater state anxiety and greater trait social anxiety would be the most likely to use cannabis. The cross-sectional relations between SIAS scores, SUDS, and cannabis use were examined in two ways. First, at the daily level, the SIAS scores X SUDS interaction significantly predicted cannabis use versus not-use days, β = 0.003, SE = .001, p = .023, pseudo R2 = .009. Effect size estimates suggest that the main effects accounted for the majority of the variance in cannabis use day status (pseudo R2 = .008). As evidenced in Figure 2, the odds of participant cannabis use on a particular day were greatest among those with lower SIAS scores and lower daily SUDS ratings. Only the simple slope for low social anxiety was significant (β = −0.11, p = .002), suggesting that greater state anxiety was related to lower odds of participants with lower social anxiety experiencing a cannabis use day. The simple slope for high social anxiety was not significant (β = −0.01, p = .574).
Figure 2.
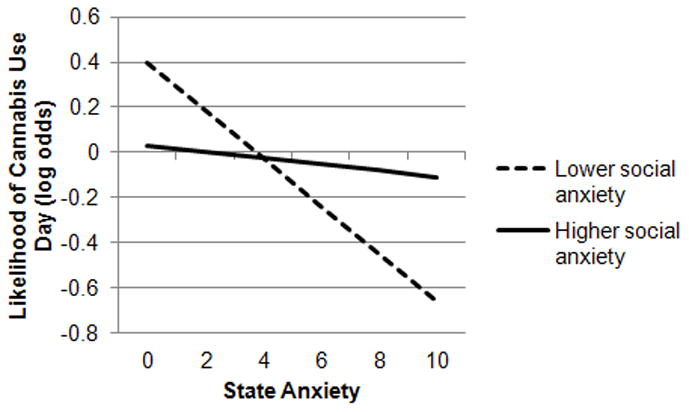
Trait social anxiety X state anxiety predicting cannabis use at the daily level.
In regards to the momentary level associations, the SIAS scores X SUDS interaction was not significant, β = −0.001, SE = .001, p = .390, pseudo R2 = .024.
The temporal relations between SIAS, SUDS, and cannabis use were examined using cross-lagged analyses testing whether SIAS scores interacted with SUDS at one assessment point to predict cannabis use at the subsequent assessment. This SIAS scores X SUDS interaction was not significant, β = 0.001, SE = .002, p = .441, pseudo R2 = .006.
3.4 Situation Type and Peer Influence3
To examine whether individuals with elevated SIAS scores were especially likely to use cannabis in social situations (e.g., to cope in the social situation) or alone (e.g., as an avoidance strategy), we tested whether SIAS scores interacted with situation type (social situation vs. alone) to predict use. This interaction was significant, β = 0.017, SE = .007, p = .013, pseudo R2 = .324. The main effects accounted for 31.6% of the variance in cannabis use with the interaction accounting for an additional 0.8%. As evidenced in Figure 3, the odds of participant cannabis use were greatest among those with higher SIAS scores who were in social situations. The simple slopes were significant for both high social anxiety (β = 1.76, p < .001) and low social anxiety (β = 1.25, p < .001).
Figure 3.
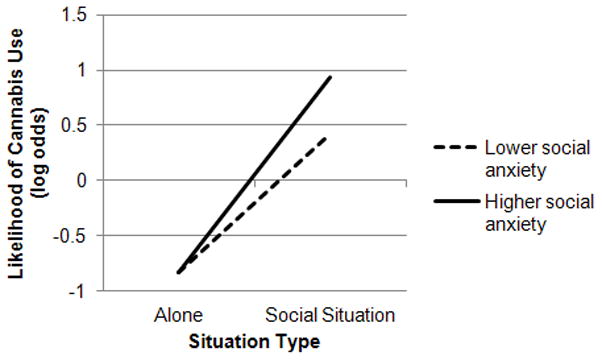
Trait social anxiety X situation type predicting cannabis use at the momentary level.
Next, we tested whether others’ cannabis use interacted with SIAS scores to predict cannabis use. This interaction was not significant, β = −0.024, SE = .014, p = .082, pseudo R2 = .830. However, it may be only under situations of heightened state anxiety that others’ use interacts with SIAS scores to predict use. This SIAS scores X SUDS X others’ use interaction was significant, β = −0.025, SE = .007, p = .001, pseudo R2 = .723. When others were using, the SIAS scores X SUDS interaction was significant, β = 0.02, SE = .007, p = .010, pseudo R2 = .025. As evidenced in Figure 4a, when others were using cannabis, the odds of participant cannabis use were greatest among those with higher SIAS scores and higher SUDS. Only the simple slope for high social anxiety was significant (β = 0.33, p = .015), suggesting that greater state anxiety is related to greater odds of cannabis use day among those with higher social anxiety when others are using cannabis. The simple slope for low social anxiety was not significant (β = −0.20, p = .139).
Figure 4.
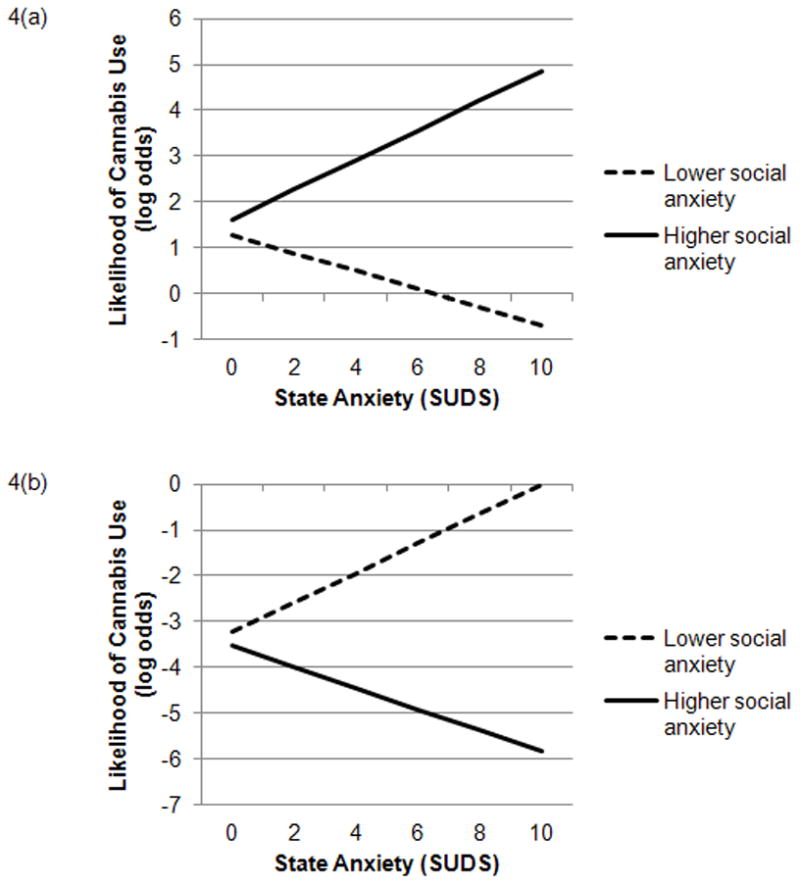
Trait social anxiety X state anxiety predicting cannabis use at the momentary level in situations in which (4a) others are using cannabis and (4b) other are not using cannabis.
When others were not using cannabis, the SIAS scores X SUDS interaction was also significant, β = −0.018, SE = .009, p = .044, pseudo R2 = .021. However, as evidenced in Figure 4b, when others were not using, the odds of participant cannabis use were lowest among those with higher SIAS scores and higher SUDS. The simple slopes were not significant for either high (β = −0.24, p = .236) or low (β = 0.33, p = .078) social anxiety.
4. Discussion
The present study is the first known EMA study examining the relations of social anxiety with situational and affective correlates and antecedents of cannabis use. The current study extends prior work finding social anxiety to be related to cannabis-related problems (e.g., Agosti, Nunes, & Levin, 2002; Buckner, Bonn-Miller et al., 2007; Buckner, Heimberg et al., 2011; Buckner, Mallott et al., 2006; Buckner & Schmidt, 2008; Marmorstein et al., 2010) by identifying that socially anxious individuals appear especially likely to use cannabis when experiencing elevations in cannabis craving. Further, although situations involving others using cannabis place all users at risk for cannabis use, socially anxious users appear especially vulnerable to using when others are using cannabis, particularly during periods of elevated state anxiety. Notably, these significant moderational effects were above and beyond the variance accounted for by the main effects. Given that our sample was comprised of relatively heavy cannabis users, these moderational analyses, despite accounting for small degree of incremental variance, could be clinically meaningful (Abelson, 1985).
It is noteworthy that social anxiety interacted with cannabis craving to predict cannabis use in all three of our tests of these relations, providing strong support for the importance of craving in cannabis use among those with higher social anxiety. This finding is especially noteworthy as it suggests that socially anxious individuals may not use substances such as cannabis only in response to elevations in state social anxiety but in response to other types of distress (in this case, unpleasant craving symptoms). It may be that individuals with social anxiety are especially vulnerable to using cannabis in response to craving as a result of a lower ability to tolerate the distress associated with craving. Social anxiety has been found to be related to lower distress tolerance (Bacon & Ham, 2010) and lower distress tolerance is related to coping motivated cannabis use (Zvolensky et al., 2009) and cannabis use-related problems (Buckner, Keough, & Schmidt, 2007). Future work testing the role of distress tolerance in the relations between social anxiety, craving, and cannabis use will be an important next step.
Unexpectedly, trait social anxiety did not interact with state anxiety to predict cannabis use. In fact, the odds of cannabis use on a particular day were lowest among those with higher trait social anxiety and higher daily state anxiety ratings. One possible interpretation of this finding is that socially anxious individuals experienced less overall state anxiety on days they use cannabis. However, this finding is contrary to laboratory studies finding that socially anxious participants do not experience less state anxiety than less socially anxious participants after consuming CBD (Bergamaschi et al., 2011). Further, the lack of significant SIAS X SUDS interactions at the momentary or antecedent levels suggests that socially anxious users may not be using cannabis to directly manage state anxiety. Alternatively, these unexpected findings could be an artifact of our reliance on SUDS ratings, which assessed state anxiety broadly rather than examining state social anxiety specifically. It may be that during periods of some types of state anxiety (e.g., worry about an exam), participants were less likely to use cannabis. Future work teasing apart state social anxiety from state anxiety more broadly will be an important next step in this line of work.
We attempted to address this limitation by examining whether trait social anxiety interacted with state anxiety in social situations. Trait social anxiety did interact with state anxiety when others were using cannabis. This finding suggests that perhaps trait social anxiety is not related to using cannabis in response to state anxiety broadly (as evidenced by the lack of significant social anxiety X state anxiety interactions at the momentary and antecedent levels). Rather, socially anxious individuals may only be vulnerable to using cannabis to manage increases in state social anxiety (i.e., anxiety experienced during a social event for fear of scrutiny).
The finding that socially anxious individuals were especially vulnerable to using cannabis during periods of elevated state anxiety when others were also using has important implications for the treatment of co-occurring SAD and CUD. Therapists may consider incorporating out-of-session exposure exercises that encourage patients to engage in social interactions with cannabis-abstaining individuals. Although cognitive-behavioral therapy (CBT) for substance use disorders encourages patients to avoid high-risk use situations (e.g., situations in which others are using), socially anxious individuals may especially benefit from sessions designed to encourage them to spend time with people who do not use cannabis as they appear the least likely to use cannabis during periods of elevated state anxiety when others are not using.
Interestingly, social anxiety interacted with situation type such that socially anxious individuals in social situations were especially vulnerable to cannabis use. This finding seems counter to work finding that social avoidance was more strongly related to problematic cannabis use than anxiety in social situations (Buckner, Heimberg et al., 2011). However, it may be that greater social avoidance is related to more use-related problems because use is more likely to occur in social situations. Thus, more socially avoidant users may have less experience managing their use than their less avoidant peers, which may lead to problems such as using more than intended, driving while intoxicated, etc.
4.1 Limitations and Future Directions
Several limitations specific to the present investigation warrant discussion. First, only 10 participants met DSM-IV criteria for current SAD, limiting our ability to examine whether observed relations generalize to people with SAD. Second, we only examined one type of negative affect (state anxiety) during the monitoring period and future work will benefit from examining whether other types of negative affect (e.g., sadness, anger) interact with trait social anxiety to predict cannabis use. Third, we did not examine cannabis-related problems during the EMA period and future work is necessary to determine under what circumstances socially anxious users are vulnerable to use-related problems. Fourth, we did not examine use of other substances during the monitoring period. Given the high rate of alcohol use disorders in this sample combined with data suggesting that social anxiety is related to using alcohol to cope in social situations (Buckner & Heimberg, 2010), future EMA work could benefit from examining whether socially anxious individuals use other substances to cope with elevated anxiety. Fifth, we examined social interaction anxiety as our primary measure of trait social anxiety and future work could benefit from examining whether other types of social anxiety (e.g., performance fears, fear of positive evaluation) are similarly related to craving, state anxiety, and cannabis use. Sixth, future work could benefit from collection of more detailed information regarding the nature of the relationships the participant had with peers (e.g., close friends, acquaintances, strangers) as well as specifications regarding the types of social situations in which participants were involved. Seventh, data collected during the monitoring period were collected using single item assessments that may have been completed while participants were under the influence of cannabis. However, our data suggest that these assessments may have nevertheless been valid given that participants who identified as daily users at baseline reported more marijuana use and craving during the monitoring period and baseline state anxiety was correlated with state anxiety ratings during the monitoring period. Nevertheless, future work using a multi-method, multi-informant method may provide additional information about the validity of these reports. Eigth, we emailed participants daily to remind them to complete the assessments and this strategy resulted in compliance rates that were somewhat higher than those reported in other EMA studies of non-treatment samples of substance users which, although obtaining comparable compliance estimates, assessed compliance only on days the recording device was used by the participant (Hopper et al., 2006). However, our participants were not given a “practice period”, a practice common in EMA research (Shiffman et al., 2002; Smyth et al., 2007) that may have resulted in even greater compliance.
4.2 Conclusions
Despite these limitations, the present findings provide important insight into cannabis use behaviors among individuals with elevated trait social anxiety, a group that appears especially vulnerable to experiencing cannabis-related problems (e.g., Buckner, Bonn-Miller et al., 2007; Buckner, Heimberg et al., in press; Buckner, Heimberg et al., 2011; Buckner, Mallott et al., 2006; Buckner & Schmidt, 2008; Marmorstein et al., 2010) and CUD (Agosti et al., 2002; Buckner et al., 2008; Stinson, Ruan, Pickering, & Grant, 2006). Findings highlight the important roles of craving, state social anxiety, and peer cannabis use play in maintaining cannabis use among socially anxious cannabis users. These data suggest that socially anxious individuals may use cannabis not only to manage increases in state anxiety (especially in social situations when others are using cannabis) but to manage unpleasant symptoms of cannabis craving. Given the high rates of co-occurring social anxiety and cannabis-related problems, it is our hope that this study will serve as a first step in continued EMA studies aimed at understanding factors that maintain cannabis use and use-related problems among this high-risk population.
Research Highlights.
During the two-week EMA period, social anxiety significantly interacted with cannabis craving to predict cannabis use both cross-sectionally and prospectively.
Individuals with higher social anxiety and higher craving were the most likely to use cannabis.
Social anxiety significantly interacted with situation type such that socially anxious individuals in social situations were especially likely to use cannabis.
There was a significant social anxiety X state anxiety X others’ use interaction such that when others were using, those with elevations in both social anxiety and state anxiety were the most likely to use cannabis.
Acknowledgments
This research was supported in part by a National Institute on Drug Abuse (NIDA) grant F31 DA021457 awarded to Julia D. Buckner.
Data were collected in the Anxiety and Behavioral Health Laboratory at Florida State University.
Footnotes
Percentages add up to greater than 100% due to comorbidity.
A similar pattern of findings was obtained when analyses were conducted excluding all signal contingent data that was not compliant with study instructions (i.e., completed more than 60 minutes after signal prompt).
A similar pattern was obtained when AS-social concerns were included as a covariate in all analyses.
A similar pattern was obtained when sex was included as a covariate in all analyses concerning state anxiety scores.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Julia D. Buckner, Louisiana State University.
Ross D. Crosby, University of North Dakota School of Medicine & Health Sciences and the Neuropsychiatric Research Institute
Stephen A. Wonderlich, University of North Dakota School of Medicine & Health Sciences and the Neuropsychiatric Research Institute
Norman B. Schmidt, Florida State University
References
- Abelson RP. A variance explanation paradox: When a little is a lot. Psychological Bulletin. 1985;97:129–133. doi: 10.1037/0033-2909.97.1.129. [DOI] [Google Scholar]
- Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse. 2002;28:643–652. doi: 10.1081/ADA-120015873. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Bacon AK, Ham LS. Attention to social threat as a vulnerability to the development of comorbid social anxiety disorder and alcohol use disorders: An avoidance-coping cognitive model. Addictive Behaviors. 2010 doi: 10.1016/j.addbeh.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295x.111.1.33. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal Of Consulting And Clinical Psychology. 1988;56:893–897. doi: 10.1037/0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the BDI-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bergamaschi MM, Queiroz RHC, Chagas MHN, de Oliveira DCG, De Martinis BS, Kapczinski F, Quevedo J, Roesler R, Schröder N, Nardi AE, Martín-Santos R, Hallak JEC, Zuardi AW, Crippa JAS. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naïve social phobia patients. Neuropsychopharmacology. 2011;36:1219–1226. doi: 10.1038/npp.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EJ, Turovsky J, Heimberg RG, Juster HR, Brown TA, Barlow DH. Validation of the Social Interaction Anxiety Scale and the Social Phobia Scale across anxiety disorders. Psychological Assessment. 1997;9:21–27. doi: 10.1037/1040-3590.9.1.21. [DOI] [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, Schmidt NB. Marijuana use motives and social anxiety among marijuana-using young adults. Addictive Behaviors. 2007;32:2238–2252. doi: 10.1016/j.addbeh.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Crosby RD, Silgado J, Wonderlich SA, Schmidt NB. Immediate antecedents of marijuana use: An analysis from ecological momentary assessment. Journal of Behavior Therapy and Experimental Psychiatry. doi: 10.1016/j.jbtep.2011.09.010. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG. Drinking behaviors in social situations account for alcohol-related problems among socially anxious individuals. Psychology of Addictive Behaviors. 2010;24:640–648. doi: 10.1037/a0020968. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Matthews RA, Silgado J. Marijuana-related problems and social anxiety: The role of marijuana behaviors in social situations. Psychology of Addictive Behaviors. doi: 10.1037/a0025822. (in press) [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Schmidt NB. Social anxiety and marijuana-related problems: The role of social avoidance. Addictive Behaviors. 2011;36:129–132. doi: 10.1016/j.addbeh.2010.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32:1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Mallott MA, Schmidt NB, Taylor J. Peer influence and gender differences in problematic cannabis use among individuals with social anxiety. Journal of Anxiety Disorders. 2006;20:1087–1102. doi: 10.1016/j.janxdis.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Marijuana effect expectancies: Relations to social anxiety and marijuana use problems. Addictive Behaviors. 2008;33:1477–1483. doi: 10.1016/j.addbeh.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. A randomized pilot study of motivation enhancement therapy to increase utilization of cognitive-behavioral therapy for social anxiety. Behaviour Research and Therapy. 2009;47:710–715. doi: 10.1016/j.brat.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Social anxiety disorder and marijuana use problems: The mediating role of marijuana effect expectancies. Depression and Anxiety. 2009;26:864–870. doi: 10.1002/da.20567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Bobadilla L, Taylor J. Social anxiety and problematic cannabis use: Evaluating the moderating role of stress reactivity and perceived coping. Behaviour Research and Therapy. 2006;44:1007–1015. doi: 10.1016/j.brat.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Silgado J, Schmidt NB. Marijuana craving during a public speaking challenge: Understanding marijuana use vulnerability among women and those with social anxiety disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2011;42:104–110. doi: 10.1016/j.jbtep.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Smits J, Norton PJ, Crosby RD, Wonderlich SA, Schmidt NB. Anxiety sensitivity and marijuana use: An analysis from ecological momentary assessment. Depression and Anxiety. 2011;28:420–426. doi: 10.1002/da.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, Arria AM, O’Grady KE, Vincent KB, Wish ED. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addictive Behaviors. 2008;33:397–411. doi: 10.1016/j.addbeh.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannahy L, Stopa L. Post-event processing in social anxiety. Behaviour Research and Therapy. 2007;45:1207–1219. doi: 10.1016/j.brat.2006.08.017. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Heishman SJ, Singleton EG, Liguori A. Marijuana Craving Questionnaire: Development and initial validation of a self-report instrument. Addiction. 2001;96:1023–1034. doi: 10.1046/j.1360-0443.2001.967102312.x. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Su Z, Looby AR, Ryan ET, Penetar DM, Palmer CM, Lukas SE. Incidence and patterns of polydrug use and craving for ecstasy in regular ecstasy users: an ecological momentary assessment study. Drug and Alcohol Dependence. 2006;85:221–235. doi: 10.1016/j.drugalcdep.2006.04.012. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. College Students & Adults Ages 19–45. II. Bethesda, MD: National Institutes of Health & U.S. Department of Health and Human Services; 2007. Monitoring the Future National Survey Results on Drug Use 1975–2007. [Google Scholar]
- Kocovski NL, Rector NA. Post-event processing in social anxiety disorder: Idiosyncratic priming in the course of CBT. Cognitive Therapy and Research. 2008;32:23–36. doi: 10.1007/s10608-007-9152-z. [DOI] [Google Scholar]
- Kreft I, de Leeuw J. Introducing Multilevel Modeling. London: Sage Publications Ltd; 1998. [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs. 2009;70:279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. Journal of Abnormal Child Psychology. 2010;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/S0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Osman A, Gutierrez PM, Barrios FX, Kopper BA, Chiros CE. The Social Phobia and Social Interaction Anxiety Scales: Evaluation of psychometric properties. Journal of Psychopathology and Behavioral Assessment. 1998;20:249–264. doi: 10.1023/a:1023067302227. [DOI] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Hickcox M, Gnys M. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal of Abnormal Psychology. 2002;111:531–545. doi: 10.1037/0021-843X.111.4.531. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y) Pal Alto, CA: Mind Garden; 1983. [Google Scholar]
- Spokas M, Heimberg RG. Overprotective parenting, social anxiety, and external locus of control: Cross-sectional and longitudinal relationships. Cognitive Therapy and Research. 2009;33:543–551. doi: 10.1007/s10608-008-9227-5. [DOI] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: Prevalence, correlates and co-morbidity. Psychological Medicine. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Summary of National Findings. I. Office of Applied Studies; Rockville, MD: 2010. Results from the 2009 National Survey on Drug Use and Health. NSDUH Series H-38A, HHS Publication No. SMA 10-4586Findings. [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. doi: 10.1111/1467-6494.ep9110141804. [DOI] [Google Scholar]
- Wolpe J. Psychotherapy by reciprocal inhibition. Integrative Psychological and Behavioral Science. 1968;3:234–240. doi: 10.1007/BF03000093. [DOI] [PubMed] [Google Scholar]
- Zuardi AW, Cosme RA, Graeff FG, Guimarães FS. Effects of ipsapirone and cannabidiol on human experimental anxiety. Journal of Psychopharmacology. 1993;7:82–88. doi: 10.1177/026988119300700112. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Marshall EC, Johnson K, Hogan J, Bernstein A, Bonn-Miller MO. Relations between anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations to coping and conformity marijuana use motives among young adult marijuana users. Experimental and Clinical Psychopharmacology. 2009;17:31–42. doi: 10.1037/a0014961. [DOI] [PMC free article] [PubMed] [Google Scholar]