Abstract
Objective
The goal of this report is to describe the on going strategies, successes, challenges and solutions for recruitment in this multi-center, phase II chemoprevention trial targeting men at high risk for prostate cancer.
Methods
We developed and implemented a multi-center clinical trial in institutions with supportive infrastructure, lead by a recruitment team of experienced and committed physicians and clinical trial staff, implementing multi-media and community outreach strategies to meet recruitment goals. Screening logs were reviewed to identify trends as well as patient, protocol and infrastructure -related barriers impacting accrual and revisions to protocol implemented.
Results
Between January 2008 and February 2011 a total of 3547 individuals were prescreened with 94% (n=3092) determined to be ineligible based on diagnosis of cancer or benign biopsy results. Of these, 216 were considered eligible for further screening with 52% (n=113) declining to participate due to patient related factors and 14% (n=29) eliminated due to protocol-related criteria for exclusion. Ninety four (94) subjects consented to participate with 34% of these subjects (n=74) meeting all eligibility criteria to be randomized to receive study agent or placebo. Across all sites, 99% of the recruitment of subjects in this clinical trial is via physician recruitment and referral with less than 1% responding to other recruitment strategies.
Conclusion
A contemporary approach to subject recruitment and frequent evaluation is needed to assure responsiveness to emerging challenges to accrual and the evolving scientific literature. A focus on investing on improving systems for physician recruitment may be key to meeting recruitment target in chemoprevention trials.
Background
The American Cancer Society estimates that there will be 240,890 new cases of prostate cancer (CaP) in the United States (US) in 2011, and 33,720 men will die from this disease.[1] The initiation and progression of CaP may involve a complex array of both exogenous and endogenous factors.[2–5] Although it is clear that clinical CaP incidence and mortality vary greatly between populations, the frequency of latent CaP is evenly distributed among populations, suggesting that external factors such as diet, physical activity and other lifestyle factors are important in the transformation from latent into more aggressive, clinical cancer.[2–5] In addition, in most epithelial tissues, including the prostate, genetic progression and loss of cellular control functions are observed as the cell and tissue phenotype changes from normal to dysplasia (prostatic intraepithelial neoplasia or PIN), then to increasingly severe dysplasia (high grade PIN or HGPIN), superficial cancers and finally to invasive disease.[5] These features of prostate cancer, namely, high prevalence, long latency, significant mortality and morbidity, and the availability of intermediate predictive stages of progression, provide the most promise for evaluating agents for chemoprevention. Chemoprevention is the prevention of induction and inhibition of the development of preinvasive and invasive cancer and its progression or treatment of identifiable pre-cancers.[2] Several nutrients and nutrient derived agents have continued to demonstrate promise as potential chemopreventive agents in epidemiological, laboratory studies and pilot or early phase I–II studies. In spite of the unique opportunity for prevention as well as unavailability of alternative treatment strategies for this high risk group of men other than surveillance, chemoprevention trials for prostate cancer prevention have not been successful.
Recruiting participants who are at high risk for cancer continues to be costly and presents unique challenges globally.[6–7] The ability of research teams and institutions to recruit eligible subjects at high risk for cancer, who are willing to adhere to the study protocol in randomized clinical trials is an essential component of translational research[8] that may impact generalizability of reported results.[7] Several barriers and facilitators to recruitment in chemoprevention trials have been documented. These include subject, protocol and infrastructure related factors. With respect to subject-related factors, chemoprevention trials are targeted at high risk, healthy individuals who do not have any signs and symptoms of the disease[8] who are often unwilling to be randomized to placebo-control arms of the trial, especially if the trial involves immense burden to them, including compliance to agent and diet, frequent visits, completion of monitoring tools and most importantly if these studies include invasive procedures for biomarker evaluation such as biopsy, fine needle aspirations or bronchoscopy.[8] In addition, most of the agents under study are available in similar doses as over the counter (OTC) supplements or in “natural” forms that subjects have access to. This increased availability has encouraged subjects to opt out of participation in randomized clinical trials, where there is a chance of being assigned to a placebo arm.[9–10] Protocol-related factors include unrealistic exclusion and inclusion criteria such as use of other nutrient supplements and concomitant medications used for cardiac prophylaxis such as Aspirin or lipid lowering regimens, especially if these studies are targeted to otherwise healthy individuals. Institutional or infrastructure-related barriers include unavailability of culturally competent teams[7,9] with investigators not communicating with the community and target population who are stakeholders[12] as well as location and accessibility to research sites noted. While important for the protection of the privacy of human subjects, challenges have also emerged related to the use of community members and peers in subject recruitment as concerns related to the privacy of health information have been raised.[13–14]
Supportive marketing and public relations departments at sites that use community radio, newspaper and other published media advertisements, direct and indirect mailings, internet postings, development and distribution of decision aids[16] and print media exposure of clinical trials[15] utilizing culturally and literacy competent and experienced teams[7] have demonstrated success in attaining target recruitment numbers in other cancer prevention trials. The efforts of experienced and committed physician's investigators[17] who are key stakeholders have also been shown to be vital to the success of clinical trial recruitment. Research teams that pay meticulous attention to patient recruitment, retention, individualization of procedures with respect to multi-institutional sites[7] and frequent monitoring of subject screening, recruitment and randomization logs to inform revisions to procedures have been shown to significantly improve recruitment in clinical trials. In spite of the available literature on effective recruitment strategies, to date, few reports have identified the unique challenges and potential solutions to recruitment in chemoprevention trials using nutrient-derived agents for cancer prevention in otherwise healthy, high risk populations.
We are currently recruiting men diagnosed with High Grade Prostatic Intraepithelial Neoplasia (HGPIN) or Atypical Small Acinar Proliferation (ASAP) in a multi-center, phase II randomized, placebo-controlled chemoprevention trial of Polyphenon E to prevent progression to prostate cancer. As with most chemoprevention trials, we have experienced several challenges with accrual. Identification of challenges and solutions to recruitment barriers in chemoprevention trials may guide researchers in the future design of contemporary chemoprevention trials and additionally, to better select, focus and invest in strategies that are the most productive and efficient to recruit high risk populations. The goal of this paper is to describe the strategies, successes, challenges and potential solutions towards achieving target recruitment accrual in future chemoprevention trials.
Methods
Overview of current clinical trial
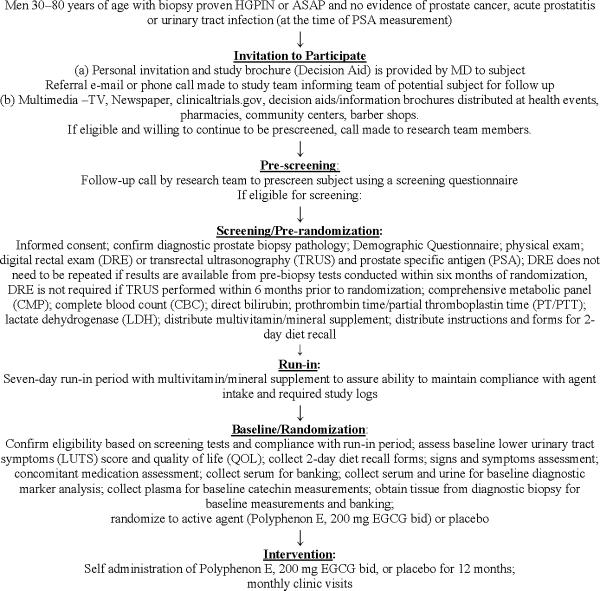
This 5-year project is a randomized double-blind placebo controlled phase II clinical trial examining the safety and efficacy of Polyphenon E at a dose of 200 mg EGCG bid administered for 12 months versus placebo on the occurrence of diagnosis in 240 men between ages 30 and 80 with a diagnosis of HGPIN or ASAP. Cohort participants are recruited from nine (9) research sites in the United States. In addition to disease progression as the ultimate outcome in this trial, we will also evaluate a selected combination of biochemical (PSA, steroid hormones), morphological (cytopathology, Ki-67) and genetic (apoptotic index) intermediate endpoint biomarkers relevant to prostate carcinogenesis. We have also included markers of safety, compliance, quality of life and exploratory studies examining the molecular targets of Polyphenon E. Prior to trial initiation, the Human Subjects Committees of each of the participating institutions approved all trial procedures. The randomization of study participants is stratified by diagnosis (HGPIN or ASAP) and geographical location of recruitment site. Figure.1 describes the overall trial design and data collection time points. All study participants receive twenty dollars for time and travel related to the monthly safety visits.
Figure 1.
Phase II Clinical Study of Polyphenon E in Men with HGPIN or ASAP
Proactive Recruitment Strategies
Infrastructure
We invited 3 sites, other than the primary site (Moffitt Cancer Center) from large institutions in urban cities like Chicago and Philadelphia and 1 large VA Medical Center in Tampa, Florida with established clinical trials infrastructure and Genito-urinary oncology programs, anticipating our challenge to recruit this subset of men with HGPIN, as well as the need for a relatively large pool of patients to successfully recruit subjects from an economically and racially representative population. Special teams were established for administration, recruitment, intervention and retention, biomarkers and data safety monitoring to work closely and provide efficient, standardized and centralized services for successful implementation of this proposal.
Characteristics of site Principal Investigators (PIs) and other healthcare providers
We selected PIs from these sites who had significant experience and commitment to recruiting subjects in chemoprevention and other clinical trials. The physicians were also involved from the start in the planning and implementation process of the clinical trial. At each of these sites, we also encouraged the PIs to work closely with community physicians, oncologists and to include primary care physicians and urologists as secondary source to recruit subjects.
Conservative estimation of target recruitment from available sample
It was estimated that on an average, 15% of all men biopsied at each site would be diagnosed with HGPIN annually. Although a history of actual annual number of men diagnosed with HGPIN was obtained for each site, we anticipating realistically and conservatively that only 50% of eligible subjects will meet all criteria for inclusion to be randomized to this clinical trial.
Recruitment and Retention Team
We also formed a Recruitment/Intervention & Retention Team that participated in the initial design of the recruitment procedures (Figure 1). Members of the Recruitment/Intervention & Retention Team included the site PIs and clinical coordinators led by the PI at the MCC research base. This team's role is to ensure implementation of all established procedures consistently for recruitment, intervention and retention of trial subjects. The team participated in developing the methods for recruitment and retention and has scheduled bi-monthly teleconferences to discuss challenges and solutions, successful strategies and revises procedures for recruitment and retention, based on specific needs at each site. A monthly screening and recruitment log is completed at each site and submitted to the PI at the MCC research base. Specific data from screening logs includes number of biopsies reviewed (pre-screening), potentially eligible subjects, number definitively determined ineligible, number of subjects randomized, and specific reasons why eligible subjects were not recruited. In addition, a comprehensive review of screening logs, current recruitment strategies, the recruitment and retention team's meeting minutes and other communications is completed each quarter by the PI to categorize issues as patient or protocol -related and evaluate other barriers impacting recruitment of subjects in this phase II clinical trial. Barriers are categorized as (a) patient (b) protocol or (c) infrastructure-related. Based on data obtained from the recruitment logs and meeting minutes, protocol, patient and infrastructure-related issues are identified and modifications to the protocol to improve recruitment are implemented, without compromising the original goals of the research trial.
Multi-media advertisements and Marketing of study
Upon receipt of approval from Institutional Review Boards, with the assistance of the Institutional public relations and marketing teams, an initial national and local media campaign was initiated using TV, newspaper, print and web-based communications of the clinical trial. A decision aid brochure was developed to describe the trial rationale, eligibility criteria, benefits and risks, responsibility of subjects and a contact number, to be distributed at Men's Health events, community medical clinic sites, churches, community organizations, pharmacies and barber shops. The trial was also listed in the clinical trials.gov website of the National Institute of Health.
Results
The trial was initially set up in 4 large centers with senior investigators who were the primary surgeons conducting biopsies for the diagnosis of prostate cancer, HGPIN or ASAP at these sites. Although the number of potential subjects prescreened at each site met the recruitment target as proposed during the first year of recruitment, the number of men diagnosed with HGPIN has been significantly reduced to 3% of total number of subjects biopsied compared to 15% as originally estimated. However, 11% of subjects screened were diagnosed with HGPIN and/or suspicious ASAP, resulting in physician recommendation of a repeat biopsy. Based on these lower than anticipated number of potentially eligible men in year 1, we invited and recruited an additional 5 experienced PIs (Feist-Weiller Cancer Center, Shreveport, LA, Overton Brooks VA, Shreveport, LA; Center for Cancer Care-Watson Clinic, Lakeland, Florida, University of Florida, Jacksonville, Florida and VA Minneapolis, Minnesota) to participate in this trial, setting realistic recruitment goals at each site and increasing the number of sites from the original 4 to 9 sites. In addition, with a significantly increased number of diagnosis of ASAP compared to HGPIN, we consulted with the trial biostatistician and pathologists at the sites and amended the protocol to include men with ASAP in the trial, with the goal of increasing accrual by allowing inclusion of this group. The statistical section was modified and random assignment adjusted to account for this variability in the subject population, without compromising the power.
Although a timeline of 6 months was planned for trial initiation, there was a significant delay in the protocol approval process by the Scientific Review Committees and the Institutional Review Boards (IRB) and the Investigational New Drug Approvals from Food and Drug Administration (FDA) prior to drug shipment to each site. Average time taken for protocol approval by Institutional Scientific review, IRB and FDA was 12–14 months. Additionally, a change in ownership of pharmaceutical company requiring several modifications of protocol and resubmission to IRB and FDA for subsequent approval of amendments by each of the institutional IRBs. Institutionally, faculty, including PI and staff turnover or faculty sabbatical at collaborating sites was significant with 3/4 primary sites requiring re-activation of the clinical trial and training of new PI and staff.
Table 1 presents characteristics of the total number of subjects pre-screened and those ultimately included or excluded from the screening process leading to randomization. Since initiating recruitment in January 2008 through February 2011 a total of 3547 individuals undergoing prostate biopsies were prescreened for eligibility to participate in this clinical trial. The anticipated participant pool dropped significantly from prior estimates with 91% (n=3119) of this group of prescreened subjects determined to be ineligible for further screening based on diagnosis of prostate cancer, ASAP or benign prostate. Among the 9% yield from prescreening, final eligibility could not be determined on 112 individuals due to pending tests (repeat biopsy within 3 months or other diagnostics). These subjects continue to be monitored by the recruitment teams to determine future eligibility. From the prescreening process, 216 men were eligible for screening and invited to participate in the study. Table 2 displays the number of subjects eligible for screening and classifies the patient and protocol related barriers that impacted the total number ultimately screened. Of the 216 men eligible for screening, 52% (n=113) declined to participate due to patient related factors (such as time and travel required, chance of getting a placebo, resistance to future biopsies, and financial concerns) with 58 men declining without providing a specific reason. Of the total eligible for screening, 94 subjects signed consent to begin the process. From this group of subjects, 74 men completed the screening and run-in phase successfully and were randomized to receive study agent or placebo. Among the 20 subjects not randomized after signing consent, 15 were ineligible due to abnormal screening labs and 5 withdrew consent for other unspecified reasons. Thus among subjects found potentially eligible at initial pre-screening, 34% were randomized in this clinical trial.
Table 1.
Characteristics of subjects pre-screened for eligibility based on protocol inclusion/exclusion criteria
| Prescreening | Number(N) | Percentage (%) |
|---|---|---|
| Total pre-screened | 3547 | |
| Prostate cancer diagnosis | 1596 | 45 |
| Benign diagnosis | 1164 | 33 |
| ASAP(prior to being added to protocol in year 3) | 109 | 3 |
| Other Cancers | 29 | 0.8 |
| Other illness/Recent abnormal labs prior to screening | 75 | 2 |
| Concomitant medications | 37 | 1 |
| History of GI bleeds | 10 | 0.3 |
| Age >80 years | 48 | 1.4 |
| PSA > 10 | 18 | 0.5 |
| Ineligible/Unknown | 133 | 3.8 |
| parameters | ||
| Biopsy Pending | 112 | 3.2 |
|
| ||
| Total number eligible for screening visit | 216 | 6.1 |
Table 2.
Characteristics of subjects eligible for screening based on protocol and patient-related factors
| Screening | Number(N) | Percentage(%) |
|---|---|---|
| Total screened | 216 | |
| Protocol-related | ||
| Abnormal labs at screening (LFTs,other) | 10 | |
| PSA >10 | 3 | |
| Participation in another trial | 9 | |
| Withdrew consent | 5 | |
| After consent, subject found ineligible | 2 | |
| Total not screened due to protocol-related factors | 29 | 14 |
| Subject-related | ||
| Language barrier | 3 | |
| Travel | 12 | |
| Time commitment | 14 | |
| Participation in a randomized trial (did not want to get the placebo) | 7 | |
| Did not want to change current regimen | 13 | |
| Did not want to have additional biopsies | 5 | |
| Financial concern | 1 | |
| Unknown reason | 58 | |
| Total not screened due to patient-related factors | 113 | 52 |
| Total number of subjects consented for screening | 74 | 34 |
Table 3 presents the characteristics of subjects randomized to the clinical trial. 73.3% of subjects in the study were white, non-Hispanic men with 18.7% of the men from African American non-Hispanic ethnicity. Over 70% of the men were between ages 50–70 and diagnosed with HGPIN. Over 60% of the men had some years of college education. Over 60% recruited had a history of smoking and a family history of cancer, while 20% reported a family history of prostate cancer.
Table 3.
Demographic characteristics of subjects randomized to clinical trial.
| Variables | Number (n) | Percentage (%) |
|---|---|---|
| Race/Ethnicity | ||
| Black/AA (non-Hispanic) | 14 | 18.7 |
| White(non-Hispanic) | 55 | 73.3 |
| White (Hispanic) | 6 | 8 |
|
| ||
| Age | ||
| 30–40 | 0 | 0 |
| 41–50 | 4 | 5.3 |
| 51–60 | 26 | 34.7 |
| 61–70 | 30 | 40.0 |
| 71–80 | 15 | 20.0 |
|
| ||
| Education | ||
| 6th–11th grade | 5 | 6.7 |
| GED | 4 | 5.3 |
| High school graduate | 11 | 14.7 |
| Vocational school | 3 | 4.0 |
| Some college | 23 | 30.7 |
| Graduated college | 12 | 16.0 |
| Post graduate/professional | 17 | 22.7 |
|
| ||
| Diagnosis | ||
| HGPIN | 56 | 74.7 |
| ASAP | 9 | 12.0 |
| HGPIN/ASAP | 10 | 13.3 |
|
| ||
| Cancer History | ||
| Family history of other cancers | ||
| Yes | 45 | 60.0 |
| No | 30 | 40.0 |
|
| ||
| Prostate Cancer History | ||
| Family history of prostate cancer | ||
| Yes | 15 | 20.0 |
| No | 60 | 80.0 |
|
| ||
| History of Smoking | ||
| Yes | 46 | 61.3 |
| No | 29 | 38.7 |
In examining the effectiveness of various strategies for recruitment, we observed findings contrary to what prior research has shown. Although we marketed the protocol using TV, newspaper advertisements and other print and web-based media in addition to developing decision aids with distribution at community health centers and events, the number of subjects recruited using these marketing strategies was less than 1%. Similarly, marketing of the protocol to community urologists, internists and oncologists, using brochures yielded less than 1% subjects. No subjects were recruited advertising in pharmacies and barber shops using brochures or posters. Across all sites, 99% of the subjects recruited and randomized were recruited by the lead, committed physicians who presented the trial to potential subjects, with less than 1% of those participating recruited using other methods.
Discussion
In spite of a fair number of studies in the research literature discussing barriers and facilitators of recruiting men and women in clinical trials (cancer treatment and cancer prevention trials), few have focused on recruitment of men and women in chemoprevention trials in high risk populations. The largest prospective chemoprevention trial of healthy men (SELECT),[6] utilized two recruitment strategies to solicit subjects and found that a direct mail recruitment strategy was relatively more successful in recruiting participants to this trial with a reported yield of 2–3%[6]. Compared to these recruitment strategies in healthy community participants, we observed a relatively greater percentage in this chemoprevention trial targeting men at high risk for CaP with a yield of 6%. Additionally, of the 2.16% subjects qualifying during initial screening in the SELECT trial, only 15.1% ultimately recruited to the clinical trial,[6] compared to 34% of eligible subjects recruited in this chemoprevention trial. Other cancer prevention studies report over 70%,[7–8,15,23] recruitment rates using news radio and internet (11.8%), print and flyers (10.%). Unlike our previously reported chemoprevention trials[9–10], where we were able to recruit and randomize over 80% of eligible subjects utilizing primarily media outreach to recruit subjects, only 34% of eligible subjects were randomized in this clinical trial.
In examining the effectiveness of strategies for recruitment, we observed that although we marketed the protocol using TV, newspaper, internet and other print media, all shown to be effective in prior research by our group and others, the number of subjects recruited using these marketing strategies was less than 1%. Of those men responding to mass media strategies in this trial, most did not meet the initial eligibility criteria noted in the marketing event and therefore required a great deal of recruiter time to address calls without any subjects recruited for screening. Similarly, marketing of the protocol to community urologists and internists using brochures yielded no subjects for screening. Although, the community doctors were assured that subjects will be returned to their practice for all surveillance procedures few subjects were recruited from this source. Similarly, there were no subjects recruited by advertising in pharmacies and barber shops using posters containing trial information or decision aid brochures. These findings are unique and should inform future researchers to carefully consider the use of techniques that will be the most effective.
Considering the significant cost associated with these various strategies we decided to focus our efforts on those shown to be most effective. 99% of the subjects randomized were recruited by the lead, committed PI at each participating institution who presented the trial as a treatment option to potential subjects on the day when the biopsy diagnosis was given to the patient. Although previous studies have reported the significant on enrollment impact of individual physicians of patients into clinical trials[24–25] we observed a significant impact, with the majority of subjects recruited using this strategy, higher than most reported studies. We attribute the success of this recruitment strategy to several factors: (a) committed and experienced physicians; (b) participation of physicians in the design of this clinical trial; (c) patient's high level of trust in their physician; (d) timing of presentation of the trial as an option, post biopsy, and; (e) absence of treatment options for men at high risk for prostate cancer other than surveillance. Additionally, these recruitment rates were accomplished by the MD without any clinical trial alert system or an electronic medical system[17,25] to assist the physicians with this process at each of these sites, emphasizing the commitment and the feasibility of physicians to recruit high risk subjects in chemoprevention trials. Further research is recommended to more clearly elucidate approaches critical for successful physician involvement.
This trial presents unique challenges unlike few previously reported clinical trials, in that it is targeted to healthy men and uses a nutrient derived agent to prevent progression of this high risk stage to prostate cancer. Although scientifically meritorious, the trial design also presents other challenges in that it uses a systematic agent development model, with strict criteria for pre-screening, screening, run-in phase prior to randomization, criteria for inclusion and exclusion, frequent visits for objective adherence, safety monitoring, and invasive monitoring of intermediate endpoint biomarkers and with the substantial duration of intervention of one year.
Thus far our experience has been unique and may be useful to inform future chemoprevention trials in high risk populations. Barriers at multiple levels have been identified including those of the patient, protocol and infrastructure. We have attempted to respond to these barriers without compromising the original goals of the trial. The following strategies are highlighted as those most successful in addressing patient and protocol related barriers and boosting accrual since initiation of the trial (1) Scheduling distance visits and email/fax communication for monthly lab work and allowing for monitoring of pill count and diaries via email and facsimile communication, to reduce the hardship associated with monthly time and travel to research sites (2) Modifying inclusion criteria to allow for the use of nutritional supplements other than those containing the agent being studied; (3) Accommodating subject schedules by allowing for flexible timing of follow up visits by adjusting and changing coordinator work hours as needed; (4) Modifying inclusion criteria to include men with ASAP thereby increasing the sample pool without compromising the statistical power; (5) Allowing subjects to have study related care at referring physician's office when desired; (6) Providing templates for regulatory applications to reduce time to submission and subsequent approval; (7) Closely monitoring outreach and advertising activities to determine which are most effective; (8) Providing training/retraining to sites with PI and/or staff turnover. Though challenges at the level of infrastructure have some common themes, by far they vary from site to site and are less easily addressed on at the protocol level. In order to fully address and find solutions, more in-depth exploration, perhaps at the varying types of sites (specialty center, academic hospital, Veteran's Affairs Medical Center) is recommended. Though these issues faced by our study team may not be inherent and therefore generalizable to all clinical trials we believe that they may be more common in cancer prevention as well as investigator initiated trials. The distinct advantage is that different from pharmacy initiated trials, investigator initiated trials have the advantage of closely monitoring for barriers as well as the ability to more quickly modify as able to improve recruitment. For any study team conducting investigator initiated, chemoprevention trials, these challenges should be anticipated and recruitment targets planned accordingly in future clinical trial designs.
Conclusion
Unlike other clinical trials, chemoprevention trials using nutrient-derived substances present unique challenges to recruitment. Although mass media and community outreach efforts to recruit participation in clinical trials have demonstrated success in epidemiological studies and treatment trials, we have not experienced the same result. Targeting and directing efforts to support committed physicians who are primary directors of surveillance in this high risk population may be most cost-effective and offers the most promise for successful recruitment in chemoprevention trials. Additionally, clinical trial recruitment may be significantly enhanced by establishing and utilizing a Clinical Trial Alert system. We also recommend that institutions focus on investing their efforts on improving systems for physician clinical trial recruitment over other methods as this may be key to meeting recruitment target in chemoprevention and other clinical trials. A contemporary approach with frequent evaluation, flexibility to revise and remove barriers and continuous implementation of novel solutions to facilitate recruitment and remove barriers is needed to assure responsiveness to the emerging challenges of accrual in the evolving scientific literature.
Acknowledgement
The research study was funded by the National Institute of Health - National Cancer Institute R01 CA12060-01A1.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimers: None
References
- [1]. [accessed 9/26/11]; http://www.cancer.org/Cancer/ProstateCancer/DetailedGuide/prostate-cancer-key-statistics,
- [2].Kelloff GJ, Lieberman R, Steele VE, et al. Chemoprevention of prostate cancer: Concepts and strategies. Eur Urol. 1999;35:342. doi: 10.1159/000019906. [DOI] [PubMed] [Google Scholar]
- [3].Bostwick DG, Burke HB, Djakiew D, et al. Human prostate cancer risk factors. Cancer. 2004;101:2371. doi: 10.1002/cncr.20408. [DOI] [PubMed] [Google Scholar]
- [4].Mohamed MA, Greif PA, Diamond J, et al. Epigenetic events, remodelling enzymes and their relationship to chromatin organization in prostatic intraepithelial neoplasia and prostatic adenocarcinoma. BJU Int. 2007;99:908. doi: 10.1111/j.1464-410X.2006.06704.x. [DOI] [PubMed] [Google Scholar]
- [5].Bostwick DG, Qian J. High-grade prostatic intraepithelial neoplasia. Mod Pathol. 2004;17:360. doi: 10.1038/modpathol.3800053. [DOI] [PubMed] [Google Scholar]
- [6].Chlebowski RT, Menon R, Chaisanguanthum RM, Jackson DM. Prospective evaluation of two recruitment strategies for a randomized controlled cancer prevention trial. Clin Trials. 2010;7(6):744–8. doi: 10.1177/1740774510383886. [DOI] [PubMed] [Google Scholar]
- [7].Menon U, Gentry-Maharaj A, Ryan A, et al. Recruitment to multicentre trails – lessons from UKCTOCS: descriptive study. BMJ. 2008;337:12079. doi: 10.1136/bmj.a2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kye SH, Tashkin DP, Roth MD, et al. Recuritment strategies for a lung cancer chemoprevention trial involving ex-smokers. Contemp Clin Trials. 2009;30(5):464–72. doi: 10.1016/j.cct.2009.05.004. [DOI] [PubMed] [Google Scholar]
- [9].Kumar NB, Besterman-Dahan K, Kang L, Pow-Sang J, Xu P, Allen K, Riccardi D, Krischer J. Results of a Randomized Clinical Trial of the Action of Several Doses of Lycopene in Localized Prostate Cancer: Administration Prior to Radical Prostatectomy. Clinical Medicine: Urology. 2008 Apr 16;1:1–14. doi: 10.4137/cmu.s718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kumar NB, Krischer JP, Allen K, Riccardi D, Besterman-Dahan K, Salup R, Kang L, Xu P, Pow-Sang J. A Phase II Randomized, Placebo-Controlled Clinical Trial of Purified Isoflavones in Modulating Steroid Hormones in men diagnosed with Prostate Cancer. Nutr Cancer. 2007;59(2):163–8. doi: 10.1080/01635580701432678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Baquet CR, Henderson K, Commiskey P, Morrow JN. Clinical trials: the art of enrollment. Semin Oncol Nurs. 2008 Nov;24(4):262–9. doi: 10.1016/j.soncn.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Maslin-Prothero S. The role of the multidisciplinary team in recruiting to cancer clinical trials. Eur J Cancer Care. 2006;15(2):146–54. doi: 10.1111/j.1365-2354.2005.00625.x. [DOI] [PubMed] [Google Scholar]
- [13].Whittle J, Fletcher KE, Morzinski J, et al. Ethical challenges in a randomized controlled trial of peer education among veterans service organizations. J Empir Res Hum Res Ethics. 2010;5(4):43–51. doi: 10.1525/jer.2010.5.4.43. [DOI] [PubMed] [Google Scholar]
- [14].Simon C, Mosavel M. Community members as recruiters of human subjects: ethical considerations. Am J Bioeth. 2010;10(3):3–11. doi: 10.1080/15265160903585578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].McIntosh S, Ossip-Klein DJ, Spada J, Burton K. Recruitment strategies and success in a multi-county smoking cessation study. Nicotine Tob Res. 2000;2(3):281–4. doi: 10.1080/14622200050147556. [DOI] [PubMed] [Google Scholar]
- [16].Evans DG, Harvie M, Bundred N, Howell A. Update of breast cancer prevention and screening trials. J Med Genet. 2010;47(12):853–5. doi: 10.1136/jmg.2010.082768. [DOI] [PubMed] [Google Scholar]
- [17].Embi PJ, Jain A, Harris CM. Physicians' perceptions of an electronic health record-based clinical trial alert approach to subject recruitment: a survey. BMC Med Inform Decis Mak. 2008;8:13. doi: 10.1186/1472-6947-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Iczkowski KA. Current prostate biopsy interpretation: criteria for cancer, atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, and use of immunostains. Arch Pathol Lab Med. 2006;130:835. doi: 10.5858/2006-130-835-CPBICF. [DOI] [PubMed] [Google Scholar]
- [19].Epstein JI, Herawi M. Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications for patient care. J Urol. 2006;175:820. doi: 10.1016/S0022-5347(05)00337-X. [DOI] [PubMed] [Google Scholar]
- [20].Schoenfield L, Jones JS, Zippe CD, et al. The incidence of high-grade prostatic intraepithelial neoplasia and atypical glands suspicious for carcinoma on first-time saturation needle biopsy, and the subsequent risk of cancer. BJU Int. 2007;99:770. doi: 10.1111/j.1464-410X.2006.06728.x. [DOI] [PubMed] [Google Scholar]
- [21].Allam CK, Bostwick DG, Hayes JA, et al. Interobserver variability in the diagnosis of high- grade prostatic intraepithelial neoplasia and adenocarcinoma. Mod Pathol. 2996;9:742. [PubMed] [Google Scholar]
- [22].Kim HL, Yang XJ. Prevalence of high-grade prostatic intraepithelial neoplasia and its relationship to serum prostate specific antigen. Int Braz J Urol. 2002;28:413. [PubMed] [Google Scholar]
- [23].Gren L, Broski K, Childes J, et al. Recruitment methods employed in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Clin Trails. 2009;6(1):52–9. doi: 10.1177/1740774508100974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Mannel RS, Walker JL, Gould N, et al. Impact of individual physicians on enrollment of patients into clinical trials. Am J Clin Oncol. 2003;26(2):171–3. doi: 10.1097/00000421-200304000-00014. [DOI] [PubMed] [Google Scholar]
- [25].Heinemann S, Thüring S, Wedeken S, Schäfer T, Scheidt-Nave C, Ketterer M, Himmel W. A clinical trial alert tool to recruit large patient samples and assess selection bias in general practice research. BMC Med Res Methodol. 2011 Feb 15;11(1):16. doi: 10.1186/1471-2288-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]