Abstract
Objectives
Postoperative complications induced by hydrogen peroxide (H2O2) are described in the neurosurgical literature and mainly involve oxygen venous emboli, postoperative pneumocephalus; some of them even fatal. However, recently there are more and more published case reports for significant cardiac dysrhythmia related to the use of this chemical agent during routine neurosurgical interventions.
Design
Retrospective, two-centre study.
Setting
Retrospective review of clinical/radiological documentation (including preoperative medical history, operation report and intraoperative anesthesiology data charts).
Participants
Patients scheduled for cranial neurosurgical interventions.
Main outcome measures
Intraoperative occurrence of trigeminocardiac reflex (TCR), according the earlier defined by our group criteria, or other severe cardiovascular complications related to the intraoperative use of H2O2.
Results
Five cases were included in the study fulfilling the strict inclusion/exclusion criteria. Two of the cases were recognized as intraoperative TCR, in the other three cases the cardiovascular effects were possibly due to TCR in one, mechanical stimulation of vital centre in anterior hypothalamus, brainstem, or either mechanical or thermal action of H2O2.
Conclusions
According to this two-centre study, we can give, for the first time, evidence that cardiovascular complications according to the intraoperative use of H2O2 in neurosurgery are not rare with an incidence of 3%. Special reference is given to the occurrence of the TCR in this context.
Introduction
Hydrogen peroxide (H2O2) is a liquid commonly used in neurosurgical practice to disinfect the surgical field and to achieve hemostasis.1 Its action is due to the large quantity of reactive oxygen species (ROS) liberated during its contact with the (neural) tissues and the exotermic chemical reaction.1,2 However, its use is not always without adverse effects – mainly venous embolism1–3 and postoperative pneumocephalus, some of them even fatal.3 Recently however, there are an increasing number of publications that warn for significant cardiac dysrhythmias related to the intraoperative use of H2O2.1,4 The exact cause remains unknown, nevertheless some possible mechanisms such as trigemino-cardiac reflex (TCR) initiation by chemical stimulation of trigeminal afferents4 or possible stimulation of the cardiovascular centres in the brainstem or anterior hypothalamus1,5,6 are discussed.
Herewith we present a case series of dysrhythmias related to the use of H2O2, summarize the published data and describe the possible underlying mechanisms. Special reference is given to the possible occurrence of TCR.
Material and Methods
Consecutive patient's clinical documentation regarding preoperative medical history, operation report and intraoperative anaesthesiology data charts of all cranial neurosurgical operation were retrospectively evaluated from two institutions – Tokuda Hospital, Sofia, Bulgaria (year 2010) and All India Institute of Medical Sciences, New Delhi, India (years 2006–2010).
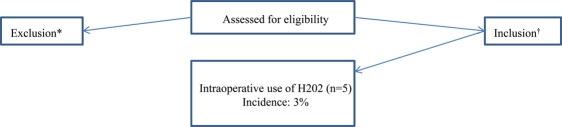
The inclusion criteria were the intraoperative occurrence of cardiovascular complications, including TCR according the earlier defined criteria by our group,7 and the intraoperative use of H2O2 during microsurgical cranial operation (Figure 1). The latter was defined that the H2O2 has to be in contact with the dura mater (epidural/subdural space). Exclusion criteria were a known history of autonomic nervous system dysfunction or no contact of H2O2 with dura mater surface (epidural/subdural space).
Figure 1.
Flow diagram depicting the study design. *H2O2 in contact with the dura mater (epidural/subdural space) (for details see Methods); †no contact of H2O2 with dura mater surface (epidural/subdural space); known autonomic dysfunction (for details see Methods). H2O2 = hydrogen peroxide
Definition of the trigeminocardiac reflex
According to strict and generally accepted criteria, the occurrence of the TCR is considered if there is seen a decrease 20% or more decrease in heart rate (HR) and mean arterial blood pressure (MABP) as response to a stimulus.7 Cessation of stimulus must have resulted in a spontaneous increase in the (HR) and the MABP to normal levels.7,8
Intraoperative monitoring
Routine monitoring during surgery included electrocardiography, heart rate and pulse oxymetry. All hemodynamic parameters were monitored continuously and recorded throughout the surgical procedure.
Ethical approval
As it was a real retrospective study, an ethical approval was not needed. However both institutions' ethical committees were informed about the study and its design.
Role of funding and sponsorship source
The authors declare not to have received any funding or sponsorship.
Results
Five cases were included in the study (Table 1). Cases 1 and 2 are related to patients diagnosed and operated on for traumatic intracranial lesions. The other cases – 3, 4 and 5 – were described during skull base interventions and dysrhythmia and were recorded in similar conditions – local application of H2O2 at the end of the procedure in order to secure hemostasis. The incidence of intraoperative use of H2O2 and the occurrence of cardiovascular complications was 3% in this retrospective study.
Table 1.
Description of the cases presented with dysrhythmia related to the use of H2O2
| Case | Age (years)/Gender | Preoperative medications | Type of surgery | Requiring intervention | Possible cause |
|---|---|---|---|---|---|
| 1 | 60/M | Yes – beta blockers | Acute subdural hematoma removal – fronto temporo parietal craniotomy | No | TCR – chemical stimulation to trigeminal afferents |
| 2 | 67/M | No | Chronic subdural hematoma removal – fronto temporo parietal cranitomy | No | TCR – chemical stimulation to trigeminal afferents |
| 3 | 16/F | No | Pituitary adenoma – pterional craniotomy– | No | TCR Anterior hypothalamus stimulation |
| Exothermic reaction of H2O2 | |||||
| 4 | 15/M | No | Craniopharyngeoma – right frontal craniotomy | No | Mechanical stimulation of anterior hypothalamus |
| Exothermic reaction of H2O2 | |||||
| 5 | 12/M | No | Posterior fossa surgery for cerebellar tumor – Midline suboccipital craniectomy | No | Mechanical stimulation of vital centres Thermal irritation from the exothermic reaction from H2O2 |
TCR = trigemino-cardiac reflex, H2O2 = hydrogen peroxide
Regarding potential risk factors for the occurrence of the TCR – only patient 1 was receiving as preoperative medication beta blocker (Metoprolol 50 mg).4 In cases 3, 4 and 5 the H2O2 irrigation was associated with bradycardia only, but not significant hypotension during craniotomy surgery and posterior cranial fossa intervention. After careful analysis, the dysrhythmia in case 5 were related to possible stimulation of the cardiovascular centres in the brainstem. Another possible mechanism was considered to be associated to the exothermic reaction of H2O2 dissociation to affect the brainstem vital centres. Similar possibilities were given in the other cases1,5,6 with mechanical and chemical stimulation of the anterior hypothalamus related with bradycardiac phenomena during craniotomy for cranipharyngioma and pituitary surgery, all occurring during the H2O2 irrigation at the end of the procedure with the aim of securing hemostasis. A true possibility for TRC, however, was only recorded in case 3, where the phenomenon was associated with the possible action of H2O2 over the maxillary and ophthalmic divisions of the trigeminal nerve in the lateral wall of cavernous sinus during H2O2 irrigation of surgical wound.
Illustrative case report of Case 1
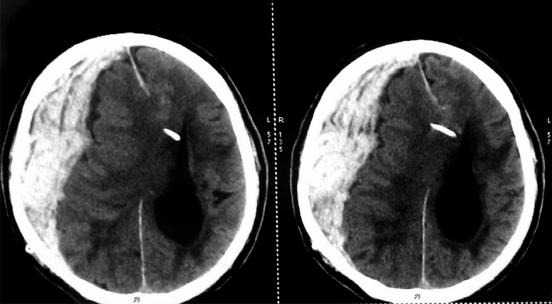
A 60-year-old Caucasian man diagnosed with normal pressure hydrocephalus (NPH) and treated via ventriculo-peritoneal shunting earlier, presented with gradually decreased consciousness progressing to coma after a fall in his bathroom. An emergent CT scan was performed and he was diagnosed with large subdural haematoma with significant midline shift (Figure 2). After clinical discussion, the patient was scheduled for an emergent craniotomy with removal blood cloth and decompression.
Figure 2.
Preoperative CT scans demonstrating a large subdural haematoma with a significant midline shift
The anaesthetic technique was standard for neurosurgical intervention.4
The patient was operated on approximately 3 hours after the accident. After realization of large fronto-temporal parietal approach (trauma flap) and opening the dura mater, several blood clots were removed. Several ruptured bridging veins were coagulated. During the whole procedure the patient was haemodynamically stable. When the whole haematoma was removed, the haematoma cavity was irrigated with 3% diluted H2O2 and gauze with this solution was administered in the cavity aiming to achieve haemostasis. At the time we did this manoeuvre there occurred the TCR and the patient's blood pressure dropped from 110/80 mmHg to 75/50 mmHg and his pulse dropped from 95 bpm to 75 bpm. The surgeon was immediately informed and the gauze soaked with H2O2 was removed. The cavity was irrigated with normal saline. Following this, the MABP and HR returned to normal and no more concomitant drops in both parameters were recorded. No further use of H2O2 was allowed. Until the end of the procedure the patient remained haemodynamically stable and there was no change in the end tidal carbon dioxide volume. Therefore the possibility of air embolism was excluded.
Discussion
According to the best of our knowledge, there are only five case reports (including the present case) in the literature describing the occurrence of dysrhythmias resulting by the irrigation of surgical field with H2O2 during neurosurgical operations.1,4–6 Two of these cases are clearly associated with the TCR, in the other three it may be suspected. We are the first to summarize and discuss all these cases in the light of potential cardiovascular hazards.
Strengths and weaknesses of the study
Of course, the present series is a relatively small case series, moreover collected in a retrospective manner. To draw any relevant conclusions, we need a consistency and strength of the association, the presence of a type of stimulus–incidence relationship and a biological plausibility.7 All these three principal requirements are given in these case series. Based on the fact that our study is a two-centre study and we could find a clear cause–effect relationship, as it is required by our initial definition of the TCR,7 our findings are therefore accurate and clinical useful.
Strengths and weaknesses in relations to other studies
The research about TCR has traditionally been based on case reports or small case studies,9 so that the current research goes in line with that phenomenon. The two-centre study character of the present work underlines the importance and especially the reproducibility of the new finding. It opens the door for two- or even multicentre studies examining the TCR, which would give further insight into this reflex. However, H2O2 is not always used in the same reproducible concentration in neurosurgery so that there is some weakness to our previous publications about the intraoperative occurrence of the TCR. Nevertheless the H2O2 as an important risk factor for intraoperative occurrence of TCR is clearly shown in the current study.
Possible mechanisms
We have already discussed elsewhere in detail of the possible underlying mechanism of action of H2O2 in TCR initiation.4 However, it is known that H2O2 produces oxygen and volume expansion on contact with organic tissue which is related with significant exothermic reaction and the release of ROS.1,5,6 Even in small quantities, H2O2 could initiate peripheral cardiovascular reflexes,10,11 an effect mediated by the ROS. In (neuro)surgical settings, however, the used concentration of H2O2 is generally much higher (3%) compared to the laboratory experimental micromolar concentrations. In the first two case reports we consider that liberated oxygen species from the H2O2 exerted a substantial concomitant chemical stimulation on a large dural surface innervated by all three branches of the trigeminal nerve which might be the cause of central TCR initiation. Other, already known risk factors for the intraoperative occurrence of the TCR, like lighter plane of anaesthesia or drugs such as sufentanil, afentanil and calcium channel blockers could be excluded in these cases. It has already been shown in experimental and clinical situations that TCR could be initiated, independently of the kind of stimulation or of trigeminal nerve branches involved,12,13 with a constant incidence from 8–18%.12–14 Even so we have currently no exact incidence of the TCR initiation by intraoperative use of H2O2 (around 3% in the present series), it could be assumed that it is lower,12 giving rise to our previous hypothesis that more than one risk factor has to be present for initiating the TCR.
In this study, we would especially shed light that except from TCR, other mechanisms for cardiac dysrhythmia should also be taken in mind when using H2O2 near vital brain centres responsible for the control of the cardiovascular system, namely hypothalamus and the brainstem.1,4,5 For cases 3 and 4 this could have possibly been due to stimulation of the anterior hypothalamus. It is likely that H2O2 irrigation may have generated an intense parasympathetic activity leading to bradycardia by mechanical stimulation. Since H2O2 produces an exothermic reaction on contact with organic tissues, the possibility of raised temperature in the area of hypothalamus cannot be ruled out – a mechanism which may have been responsible for the dysrhythmia14 in case 5.
Unanswered questions and future research
Further (patho)physiological details, like effect of concentration of H2O2 on the intraoperative occurrence of the TCR and the incidence of the TCR in relation to a cumulating risk factors, should explored in animal model research and later in prospective studies.15
Conclusion
Hydrogen peroxide was considered as a safe agent until recently, except some rare case of pulmonary embolism. With an incidence of 3% in the present study for cardiovascular complications, the intraoperative use of H2O2 has to be considered in a new light. Regarding to our present work, the utilization of H2O2 during intracranial interventions, especially near vital brain centres (hypothalamus and brainstem) and trigeminaly innervated intracranial structures (dura mater and large cerebral vessels) should be regarded with caution because of the possible risks for cardiovascular complications. Prompt communication with the surgeon and a greater vigilance is necessary during the period of H2O2 irrigation. Cardiac dysrhythmias should be kept in mind and added to the already known possible complications (venous embolism and postoperative pneumocephalus) related to the intraoperative use of H2O2.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
BS
Contributorship
TS and BS wrote the article, and interpreted and analysed the data; TS and HP collected the data; SK, CK and TS performed the operation and the patient's treatment and provided substantial information regarding the patient's case; NH, HP and LL provided some specific and general ideas that initiated the work and helped to finish the work; NS made substantial corrections to the manuscript; all authors read and approved the final manuscript
Acknowledgements
None
Reviewer
Shahab Khan
References
- 1.Prabhakar H, Rath GP, Dash HH Bradycardia following hydrogen peroxide irrigation during posterior fossa surgery. Anaesthesia 2006;61:914 [DOI] [PubMed] [Google Scholar]
- 2.Prabhakar H, Rath GP Venous oxygen embolism with use of hydrogen peroxide during craniotomy in the supine position. J Clin Neurosci 2008;15:1072 [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman GA, Lipow KI Pneumocephalus with neurological deficit from hydrogenperoxide irrigation. Case illustration. J Neurosurg 2004;100:1122 [DOI] [PubMed] [Google Scholar]
- 4.Spiriev T, Tzekov C, Kondoff S, Laleva L, Sandu N, Arasho B, Schaller B Trigemino-cardiac reflex during chronic subdural haematoma removal: report of chemical initiation of dural sensitation. J R Soc Med Sh Rep 2011;2:27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prabhakar H, Pal Singh G, Bindra A, Ali Z Dysrhythmias resulting from surgical manipulations of pituitary tumour and hydrogen peroxide irrigation of surgical wound. Indian J Anaesth 2010;54:352–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prabhakar H, Bithal PK, Pandia MP, Gupta MM, Rath GP Bradycardia due to hydrogen peroxide irrigation during craniotomy for craniopharyngioma. J Clin Neurosci 2007;14:488–90 [DOI] [PubMed] [Google Scholar]
- 7.Schaller B, Probst R, Strebel S, Gratzl O Trigeminocardiac reflex during surgery in the cerebellopontine angle. J Neurosurg 1999;90:215–20 [DOI] [PubMed] [Google Scholar]
- 8.Schaller B Trigeminocardiac reflex. A clinical phenomenon or a new physiological entity? J Neurol 2004;251:658–65 [DOI] [PubMed] [Google Scholar]
- 9.Sandu N, Sadr-Eshkevari P, Schaller B Usefulness of case reports to improve medical knowledge regarding trigemino-cardiac reflex in skull base surgery. J Med Case Reports 2011;15:149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang HS, Stahl GL, Longhurst JC Cardiac-cardiovascular reflexes induced by hydrogen peroxide in cats. Am J Physiol 1995;268:H2114–24 [DOI] [PubMed] [Google Scholar]
- 11.Soukhova GK, Ahmed M, Fletcher EC, Yu J Hydrogen peroxide in the lung parenchyma stimulates vagally mediated phrenic activity. Chest 1999;116:1365–820 [DOI] [PubMed] [Google Scholar]
- 12.Schaller B, Cornelius JF, Prabhakar H, et al. Trigemino-Cardiac Reflex Examination Group (TCREG). The trigemino-cardiac reflex: An update of the current knowledge. J Neurosurg Anesthesiol 2009;21:187–95 [DOI] [PubMed] [Google Scholar]
- 13.Schaller BJ, Filis A, Buchfelder M Trigemino-cardiac reflex in humans initiated by peripheral stimulation during neurosurgical skull-base operations. Its first description. Acta Neurochir (Wien) 2008;150:715–17 [DOI] [PubMed] [Google Scholar]
- 14.Kumada M, Dampney RA, Reis DJ The trigeminal depressor response: A novel vasodepressor response originating from the trigeminal system. Brain Res 1977;119:305–26 [DOI] [PubMed] [Google Scholar]
- 15.Sandu N, Cornelius J, Filis A, et al. Cerebral hemodynamic changes during the trigeminocardiac reflex: description of a new animal model protocol. ScientificWorld Jounral 2010;10:1416–23 [DOI] [PMC free article] [PubMed] [Google Scholar]