Abstract
OBJECTIVE:
To examine the agreement between three methods to calculate expected body weight (EBW) for adolescents with eating disorders: (1) BMI percentile, (2) McLaren, and (3) Moore methods.
METHODS:
The authors conducted a cross-sectional analysis of baseline information from adolescents seeking treatment of disordered eating at The University of Chicago. Adolescents (N = 373) aged 12 to 18 years (mean = 15.84, SD = 1.72), with anorexia nervosa (n = 130), bulimia nervosa (n = 59), or eating disorder not otherwise specified (n = 184). Concurrence between the BMI percentile, McLaren, and Moore methods was assessed for agreement above or below arbitrary cut points used in relation to hospitalization (75%), diagnosis (85%), and healthy weight (100%). Patterns of absolute discrepancies were examined by height, age, gender, and menstrual status. Limitations to some of these methods allowed comparison between all 3 methods in only 204 participants.
RESULTS:
Moderate agreement was seen between the 3 methods (κ values, 0.48–0.74), with pairwise total classification accuracy at each cut point ranging from 84% to 98%. The most discrepant calculations were observed among the tallest (>75th percentile) and shortest (<20th percentile) cases and older ages (>16 years). Many of the most discrepant cases fell above and below 85% EBW when comparing the BMI percentile and Moore methods, indicating disagreement on possible diagnosis of anorexia nervosa.
CONCLUSIONS:
These methods largely agree on percent EBW in terms of clinically significant cut points. However, the McLaren and Moore methods present with limitations, and a commonly agreed-upon method for EBW calculation such as the BMI percentile method is recommended for clinical and research purposes.
KEY WORDS: adolescence, body weight, eating disorders
What’s Known on This Subject:
Eating disorders are characterized by preoccupation with weight and shape, which is manifested by a refusal to maintain a normal weight. An exact determination of expected body weight (EBW) is critical for diagnosis and clinical management of these disorders.
What This Study Adds:
The McLaren and Moore methods present with several limitations when calculating EBW for adolescents with eating disorders. A commonly agreed upon method for EBW calculation such as the BMI percentile method is recommended for clinical and research purposes.
Eating disorders are characterized by disturbances in ingestive behavior and are usually accompanied by preoccupation with weight and shape.1 This preoccupation is often manifested by an inability to maintain a normal weight for age and height and is the primary diagnostic criterion for anorexia nervosa (AN). Determining the deviation from expected body weight (EBW) (often referred to as “ideal” body weight) is therefore important in the diagnosis of AN (<85% EBW) and the differential diagnosis of bulimia nervosa (>85% EBW) and eating disorder not otherwise specified (deviation from EBW less clearly demarcated).
In addition to diagnosis, EBW is used as an indicator of medical stability, as justification for hospitalization, to set appropriate target weights,2,3 and to track progress in treatment and assess recovery.4,5 Yet, there is no consensus on how best to calculate EBW for the pediatric and adolescent eating disorders population. Although absolute BMI (weight in kilograms/height in meters; see ref 2) has gained attention in both clinical and research settings, it is most commonly used to screen for obesity and is most applicable to the adult population.6,7 Moreover, BMI is based on height and weight only and does not account for unique phenomenon such as short stature or stunted linear growth due to malnutrition.8 Therefore, it is not an optimal method to reflect nutritional status, especially for adolescents. For pediatric and adolescent populations, age- and gender-adjusted BMI percentiles are more appropriate as weight and height normally increase until 20 years of age (Centers for Disease Control and Prevention [CDC] BMI-for-age growth charts; www.cdc.gov/growthcharts).9
Examination of an adolescent’s weight in relation to the 50th BMI percentile, also known as the BMI percentile method, or BMI method, is perhaps the most frequently used method to determine the weight criterion for an eating disorder diagnosis.10,11 In addition to the BMI method,9 other methods are used to calculate EBW; for example, the McLaren12 and Moore13 methods. The BMI, McLaren, and Moore methods are all pediatric specific and use the child or adolescent’s gender, age, and height to calculate EBW but do not take other measures of anthropometry (eg, body composition and body frame) into account. Researchers have demonstrated considerable agreement for EBW calculations across these 3 methods for healthy adolescents.14 However, such calculations are widely discrepant for older healthy adolescents at the lowest and highest percentiles.14
In studies of patients with eating disorders, authors rarely describe their method for calculating EBW. Therefore, the primary goal of the current study was to examine the agreement and/or discrepancy between the BMI, McLaren, and Moore methods when calculating EBW for adolescents with eating disorders. A secondary goal was to determine whether our findings would allow for clearer guidelines regarding the most appropriate method(s) to calculate EBW for the pediatric and adolescent eating disorders population.
Methods
Subjects
Subjects were 373 treatment-seeking adolescents, including research participants, evaluated at an outpatient eating disorders clinic from October 1998 through December 2009. The sample was composed of 342 (91.7%) females and 31 (8.3%) males, aged 12 to 18 years (mean = 15.84, SD = 1.72), who met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IVTR)1 criteria for AN (n = 130), bulimia nervosa (n = 59), or eating disorder not otherwise specified (n = 184). The majority were white (74.1%), and 13.2% were Hispanic, 7.6% black, 1.9% Asian/Pacific Islander, and 3.2% identified as “Other.” In addition to weight and height measures, participants provided demographic information and completed structured diagnostic interviews (ie, the Eating Disorder Examination15 and a set of paper-and-pencil questionnaires). For the purposes of this report, we only used weight, height, age, gender, menstrual status, ethnicity, and diagnosis. Written informed consent for patients aged 18 years or parental/guardian consent and adolescent assent for patients <18 years of age were obtained. The University of Chicago Institutional Review Board approved the research protocol.
EBW Calculations
EBW was calculated for each subject limited to three independent methods described in the following text: BMI,9 McLaren,12 and Moore13 methods.
In the BMI method, to calculate percent expected body weight (%EBW) for a given participant based on his or her height, age, and gender, the 50th percentile BMI for exact age and height at presentation on the CDC BMI-for-age percentiles chart4 was used (%EBW = BMI/50th percentile BMI for age and height × 100). A BMI at the 50th percentile would be the expected median in a group of normally developing adolescents, or EBW.
The McLaren method12 uses a growth chart based on height- and weight-for-age and for gender (eg, CDC). First, the participant’s height is plotted on the chart. A line is extended horizontally to the 50th percentile height-for-age of that participant. A second line is then extended vertically from the 50th percentile height-for-age to the corresponding 50th percentile weight. This 50th percentile weight is deemed the participant’s EBW.
The Moore method13 also uses a growth chart based on height- and weight-for-age and gender (eg, CDC), albeit in a slightly different way. The participant’s height-for-age percentile is determined, and the EBW is the weight that corresponds to that weight percentile (eg, a participant in the 30th percentile height-for-age and gender would have an EBW that corresponds to the 30th percentile weight-for-age and gender).
Of note, because of the asymptotic nature of the height curves as adolescents complete growth, the McLaren method cannot calculate EBW for girls >163 cm or for boys >176 cm. In addition, the Moore method cannot be used easily for children >97th or <3rd percentile for height or weight on the CDC growth charts, as these are the limits of what are pictured on the charts, and most practitioners do not readily access the raw CDC data for extremes of height and weight percentiles. As such, direct comparison between all 3 methods could only be made for 204 (55%) participants in our study.
Concurrence between the BMI, McLaren, and Moore methods was assessed primarily for agreement above or below EBW thresholds of 75% (hospitalization), 85% (AN diagnosis), and 100% (healthy goal weight). Patterns of absolute discrepancies were examined by height, age, gender, and menstrual status. Table 1 demonstrates the challenges around these 3 methods by calculating %EBW for a 14-year-old girl standing 165.1 cm (65 in.) tall.
TABLE 1.
Example Calculation For 14-Year-Old Girl Measuring 165.1 cm (65 in.) and 45.4 kg (100 lb)
| Method | Estimated EBW | Subject’s %EBW |
|---|---|---|
| BMI | 52.68 kg (116.15 lb) | 86.1 |
| Moore | 57.13 kg (125.95 lb) | 79.4 |
| McLaren | Incalculablea | Incalculablea |
Subject’s expected body weight and percent expected body weight could not be calculated using the McLaren method because she is taller than 163 cm.
Statistical Analysis
Statistical analyses were completed in R version 2.10. Using categories as described earlier (above/below cut points for hospitalization, diagnosis of AN, or a healthy goal weight), total classification accuracy and unweighted and quadratically weighted κ values were calculated for pairwise comparisons of the 3 methods for EBW calculation. Although both types of κ statistics reflect overall measures of concordance, quadratically weighted κ values give more penalty to the larger discrepancies (eg, a subject in the <75% EBW category using one method and >100% EBW category using another) compared with the unweighted κ values. Total classification accuracy was further calculated for the 3-way comparison. In addition, the actual values of %EBW (as opposed to the categories mentioned earlier) were plotted as pairwise comparisons of the 3 methods. Linear models were fit for each of these comparisons, and intraclass correlations were calculated. Finally, these pairwise differences were evaluated across levels of the following covariates: age, gender, height percentile, and menstrual status.
Results
Agreement
Table 2 presents the pairwise and 3-way agreement of each of these methods by the 3 predetermined cut points. Looking first at pairwise agreement, all 3 possible pairs perform moderately well at each threshold, with total classification agreement ranging from 84.2% to 97.5%. The BMI and Moore methods tended to have the lowest classification agreement (84.2%–87.7%), followed by the BMI and McLaren methods (87.7%–96.1%) and then the Moore and McLaren methods (90.2%–97.5%). Agreement tended to perform best on the lower extreme cut points; that is, better agreement was seen when predicting whether adolescents were above or below 75% EBW (87.7%–97.5%) compared with that for the 85% EBW cut point (84.2%–95.1%) and the 100% EBW cut point (85.8%–90.2%). κ values indicate moderate-to-good agreement overall, with the unweighted κ values ranging from 0.49 to 0.74 and quadratically weighted κ values ranging from 0.72 to 0.89. The superiority of the quadratically weighted κ values to the unweighted κ values indicates that when disagreement occurs, it most often occurs one cell over (eg, one measure indicates <75% EBW whereas another indicates 75% to 85% EBW).
TABLE 2.
Total Classification Agreement and Overall κ-Value Estimates for Pairwise and 3-Way Comparisons
| Agreement 75% EBW | Agreement 85% EBW | Agreement 100% EBW | Agreement, κ | |||||
|---|---|---|---|---|---|---|---|---|
| Comparison | Na | % | Na | % | Na | % | Unweighted | Quadratic Weights |
| BMI–Moore comparison | 0.487 | 0.721 | ||||||
| Agreement | 327 | 87.7 | 314 | 84.2 | 320 | 85.8 | ||
| Disagreement | 46 | 12.3 | 59 | 15.8 | 53 | 14.2 | ||
| BMI–McLaren comparison | 0.592 | 0.824 | ||||||
| Agreement | 196 | 96.1 | 180 | 88.2 | 179 | 87.7 | ||
| Disagreement | 8 | 3.9 | 24 | 11.8 | 25 | 12.3 | ||
| Moore–McLaren comparison | 0.737 | 0.888 | ||||||
| Agreement | 199 | 97.5 | 194 | 95.1 | 184 | 90.2 | ||
| Disagreement | 5 | 2.5 | 10 | 4.9 | 20 | 9.8 | ||
| 3-Way comparison | NC | NC | ||||||
| 3-Way agreement | 192 | 51.5 | 175 | 46.9 | 174 | 46.6 | ||
| Disagreement (all methods measurable) | 12 | 3.2 | 29 | 7.8 | 30 | 8.0 | ||
| Disagreement (McLaren unmeasured) | 35 | 9.4 | 35 | 9.4 | 38 | 10.2 | ||
| Moore/BMI agreement, McLaren unmeasured | 134 | 35.9 | 134 | 35.9 | 131 | 35.1 | ||
When comparing BMI with Moore, N = 373. When comparing BMI with McLaren or Moore with McLaren, the McLaren method is unable to be calculated for several cases and thus the N = 204. NC, not calculable.
Three-way agreement patterns indicate that about half of the time, all 3 measures agree on classification above or below 75% EBW (51.5%), 85% EBW (46.9%), and 100% EBW (46.6%). In about one-third of cases (35.1%–35.9%), the Moore and BMI methods agree on the classification, whereas the McLaren cannot be calculated (ie, a form of disagreement). The remaining cases represent measured disagreement.
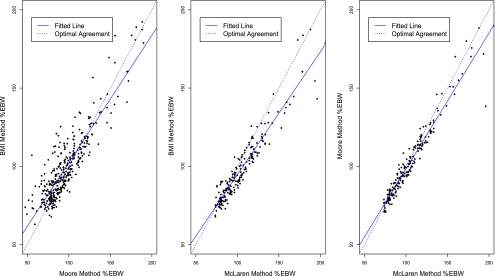
Figure 1 plots the pairwise comparisons of the 3 methods continuously. Although the individual comparisons cluster near the line of optimal agreement, significant noise and discrepancies can be seen, especially when comparing the BMI and Moore methods. Intraclass correlation for the BMI and Moore methods was 0.88 (95% confidence interval [95% CI], 0.85–0.90), for the BMI and McLaren methods was 0.90 (95% CI, 0.87–0.92), and for the Moore and McLaren methods was 0.96 (95% CI, 0.95–0.97).
FIGURE 1.
Pairwise comparisons of the 3 methods to calculate %EBW at the continuous level. Intraclass correlations associated with these 3 graphs were 0.879, 0.902, and 0.960, respectively.
Most Discrepant Cases
Although agreement at the categorical level was relatively high, some adolescents had extremely different calculations of %EBW for the various methods, with the biggest discrepancy being nearly 60% EBW. Table 3 presents the five most discrepant cases for each pairwise comparison. Most of these discrepancies will be clinically relevant for eating disorder assessment. For instance, one adolescent was measured as 143.2% with the BMI method and 196.0% in the McLaren method. As both are above 85% EBW, they would not distinguish AN from other eating disorders. Others crossed boundaries between characterizing the adolescent as severely underweight versus above their ideal weight. For instance, one adolescent was measured as 107.1% EBW with the BMI method and 55.4% EBW with the Moore method. Generally, these severely discrepant calculations occurred in females and older ages (primarily 16–18 years). The 5 most discrepant cases between the BMI and Moore methods tended to be tall, whereas the discrepant cases in the other comparisons ranged in height.
TABLE 3.
Characteristics of the 5 Most Discrepant Pairwise Disagreements
| Comparison | Discrepancy of Interesta | BMI | Weight (kg) | Height (cm) | Age (mo) | Gender | %EBW BMI | %EBW Moore | %EBW McLaren |
|---|---|---|---|---|---|---|---|---|---|
| BMI–Moore | |||||||||
| 51.7 | 22 | 71.6 | 180.3 | 195 | F | 107.1 | 55.4 | NC | |
| 35.9 | 25.7 | 80.1 | 176.5 | 216 | F | 120.9 | 85 | NC | |
| 35.2 | 25.4 | 78 | 175.3 | 188 | F | 125.3 | 90.1 | NC | |
| 32.2 | 24.7 | 75.7 | 175.3 | 197 | F | 119.5 | 87.3 | NC | |
| 30.5 | 23.2 | 71.2 | 175.3 | 196 | F | 112.6 | 82.1 | NC | |
| BMI–McLaren | |||||||||
| 52.8b | 29.9 | 41.3 | 117.5 | 204 | F | 143.2 | 138.4 | 196 | |
| 49.9c | 34.3 | 59.9 | 132.1 | 220 | F | 160.6 | 171.2 | 210.5 | |
| 38.9d | 31.3 | 53.1 | 130.2 | 188 | F | 154.5 | 171.8 | 193.4 | |
| 28.4 | 23.3 | 33.2 | 119.4 | 156 | F | 124.5 | 150.9 | 152.9 | |
| 27.1e | 37.9 | 93.9 | 157.5 | 213 | F | 178.8 | 189.9 | 205.9 | |
| Moore–McLaren | |||||||||
| 57.6b | 29.9 | 41.3 | 117.5 | 204 | F | 143.2 | 138.4 | 196 | |
| 39.3c | 34.3 | 59.9 | 132.1 | 220 | F | 160.6 | 171.2 | 210.5 | |
| 21.6d | 31.3 | 53.1 | 130.2 | 188 | F | 154.5 | 171.8 | 193.4 | |
| 16e | 37.9 | 93.9 | 157.5 | 213 | F | 178.8 | 189.9 | 205.9 | |
| 12.3 | 29.3 | 72.6 | 157.5 | 217 | F | 137.5 | 146.1 | 158.4 |
Discrepancy measured as the absolute difference between the 2 reference methods of calculating %EBW. b–eIndicates the same case appearing under multiple pairwise discrepancies. NC, not calculable.
Discrepancy by Covariates
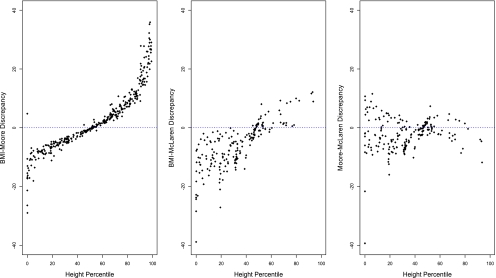
Pairwise discrepancies (eg, BMI method estimate minus Moore method estimate) were compared across the range of height percentiles (Fig 2), age (Fig 3), gender (Fig 4), and menstrual status (Fig 5).
FIGURE 2.
Pairwise discrepancy according to height percentile.
FIGURE 3.
Pairwise discrepancy according to age.
FIGURE 4.
Pairwise discrepancy according to gender.
FIGURE 5.
Pairwise discrepancy according to menstruation status. PA, primary amenorrhea; SA, secondary amenorrhea; oligo, oligomenorrhea; BC, birth control.
Regarding height percentiles, a near-cubic relationship between height percentile and the BMI–Moore discrepancy was seen, with the Moore method yielding much larger estimates for %EBW at lower height percentiles (eg, <20th percentile) and the BMI method giving larger estimates at the higher height percentiles (eg, >75th percentile). In comparing both the BMI and Moore methods against the McLaren method, the discrepancies were most pronounced for lower height percentiles.
In terms of age, the BMI and Moore methods have consistent disagreement across this age range (12–18 years old). When comparing the BMI and Moore methods against the McLaren method, the discrepancies increase with age. The Moore method tends to estimate higher values of %EBW among older ages compared with both other methods, particularly above age 16 years.
With respect to gender, the McLaren method provides larger estimates of %EBW than either the Moore or BMI methods for girls, but this bias was less for boys. There seems to be more variability for girls than for boys, which could be a function of the fact that our sample was mostly girls. In terms of menstrual status, for those on birth control and/or with regular menses, the McLaren method provides larger estimates of %EBW than either the Moore or BMI methods, but this finding could be confounded by age.
Discussion
The primary objective was to test 3 methods used to calculate EBW for adolescents with eating disorders: BMI, McLaren, and Moore. Specifically, we were interested in the extent to which these methods brought about agreement or disagreement on cut points for hospitalization (75% EBW), diagnosis (85% EBW), and healthy weight (100% EBW). Our secondary goal was to determine whether our findings would allow for clearer guidelines regarding the determination of EBW for this patient population.
Overall, there was moderate agreement between the 3 methods, with pairwise total classification accuracy at each cut point ranging from 84% to 98%. The 3 methods largely agree on %EBW in terms of clinically significant cut points with the exception of the discrepant calculations for a relatively small number of cases (2.5% -15.8%). Correlations were lowest for BMI and Moore (0.88) and highest for Moore and McLaren (0.96). The most discrepant calculations were observed among the taller patients (>75th percentile), shorter patients (<20th percentile), and those >16 years of age. Many of these most discrepant cases, when comparing the BMI and Moore methods, fell above and below 85% EBW. For instance, this discrepancy not only indicated disagreement on the weight criterion for possible diagnosis of AN, but also the same individual (see Table 3, first case) would warrant hospitalization given the Moore method (ie, 55% EBW) while simultaneously being considered close to normal weight given the BMI method (ie, 107% EBW). The evidence for agreement was not as striking for gender and menstrual status as it was for height and age. The McLaren method presented with the most significant limitation in that it cannot be used for boys >176 cm or girls >163 cm (median height for girls aged ≥14 years), which limited our original sample by >40%. In addition, the Moore method is challenging at extremes of height and weight. Therefore, our study demonstrates, even prior to the analyses, the importance of the BMI method as a methodology that can apply to children and adolescents at all ages, heights, and weights.
These discrepant calculations underscore the implications when using one method rather than another for the assessment of adolescents with eating disorders who are outside the norm for height or >16 years of age. This consideration is especially important for research endeavors when study inclusion is contingent upon a diagnosis that is arrived at via EBW calculations. For example, it is fair to say that for very tall adolescents, the BMI method will calculate higher %EBW than the Moore method. If clinicians are uncertain about the diagnosis of AN, they should consider the trade-offs of making a false-positive versus a false-negative diagnosis when choosing one method over another. However, in the interest of advancing a shared language among clinicians and researchers, we suggest that the BMI method be used as it may pose the fewest obstacles (ease of calculation) or exceptions (height and age). We acknowledge that in some instances clinical decision-making will be complex and require a more flexible approach. However, a uniform adherence to 1 method to calculate EBW will strengthen clinical and research practice.
Some limitations and strengths to our study should be considered. We did not know a priori that the shortcomings for the McLaren and Moore methods would result in these methods not being feasible for EBW calculations in a subset of our sample. However, only upon attempting comparisons of these methods did we learn that >40% of our sample could not be compared in this way. To date, it has not been well established that eating disorder patients would present this many outliers, nor has such a finding been presented in an empirical manner. Thus, our study shows that there is little utility for the McLaren method in an adolescent eating disorder sample. A limitation of all 3 methods involves the inability to account for stunted growth in pediatric subjects with eating disorders (ie, height stunting will affect calculation of EBW and will underestimate it in all likelihood). It is for practitioners to take this limitation into consideration when growth stunting is suspected clinically, based on genetic potential as evidenced by parental height, or on prior growth records showing a clear slowing of linear growth. As a result, clinicians should anticipate perhaps having to aim for higher treatment goal weights or adjusting EBW once linear growth returns to normal. Second, it is crucial to acknowledge that the cut points studied here, although commonly used in clinical practice, are arbitrary and should not be seen as absolute indicators of illness or health. For example, hospitalization is not indicated only when weight is below 75% EBW, and the DSM-IVTR cut point of 85% EBW was initially intended as an example but is often mistakenly reified into a concrete cut point. The DSM-5 Eating Disorder Workgroup specifically noted that for clinical purposes, it would be undesirable to settle on a “specific numerical standard” for weight for AN.16 Finally, we considered 3 methods for EBW calculation, whereas others still in use (see, eg, refs 17 and 18) were not included in this comparison.
Conclusions
This study represents a first step to examine the level of agreement and/or disagreement between the BMI, McLaren, and Moore methods, and future research should investigate their performance; that is, can these methods be delineated on whether one is more predictive of known biological measures of low weight, such as blood pressure or body temperature. Our findings warrant some closing considerations. First, clinicians should refrain from talking about “ideal” weight or expressing this target with unrealistic accuracy (eg, 2 decimal points). It is more informative to use the terms “average” or “median,” as has been suggested by others,19 or “expected” as we indicate here, when referring to reference weight. Second, it is imperative that the research and clinical communities attempt a common language by stating their method for EBW calculation and standardizing units of measurement (eg, kilograms rather than pounds). Based on this study, we would recommend the BMI method when assessing the pediatric and adolescent eating disorders population. Third, the use of an electronic medical record that includes BMI charts as part of pediatric software packages should be encouraged.20 Removing the barrier of calculating BMI by hand is time and cost efficient in pediatric practice. Finally, and in reference to a recent report from the American Academy of Pediatrics,21 pediatricians are at the forefront in terms of diagnosing eating disorders and should therefore routinely calculate and plot patients’ weight, height, and BMI on appropriate age and gender charts. Pediatricians should pay close attention to deviations from an individual child’s growth curve (ie, falling off personal trajectory) as such personalized growth curves provide considerable support in the determination of healthy target and potentially improve early identification of eating disorders.
Acknowledgment
This study was supported by grant NRSA T32 MH 082761 from the National Institutes of Health.
Glossary
- AN
anorexia nervosa
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- DSM-IVTR
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision
- EBW
expected body weight
- %EBW
percent expected body weight
Footnotes
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting of the article or revising it critically for important intellectual content; and final approval of the version to be published.
FINANCIAL DISCLOSURE: Dr Le Grange receives royalties from Guilford Press and honoraria from the Training Institute for Child and Adolescent Eating Disorders, LLC. The other authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
References
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Revised 4th ed. Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- 2.Golden NH, Katzman DK, Kreipe RE, et al. Society for Adolescent Medicine . Eating disorders in adolescents: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33(6):496–503 [DOI] [PubMed] [Google Scholar]
- 3.Golden NH, Jacobson MS, Sterling WM, Hertz S. Treatment goal weight in adolescents with anorexia nervosa: use of BMI percentiles. Int J Eat Disord. 2008;41(4):301–306 [DOI] [PubMed] [Google Scholar]
- 4.Rome ES, Ammerman S, Rosen DS, et al. Children and adolescents with eating disorders: the state of the art. Pediatrics. 2003;111(1):e98–e108 [DOI] [PubMed] [Google Scholar]
- 5.Couturier J, Lock J. What is remission in adolescent anorexia nervosa? A review of various conceptualizations and quantitative analysis. Int J Eat Disord. 2006;39(3):175–183 [DOI] [PubMed] [Google Scholar]
- 6.Hebebrand J, Wehmeier PM, Remschmidt H. Weight criteria for diagnosis of anorexia nervosa. Am J Psychiatry. 2000;157(6):1024. [DOI] [PubMed] [Google Scholar]
- 7.Yager J, Powers PS. Clinical Manual of Eating Disorders, 1st ed. Washington, DC: American Psychiatric Publishing; 2007:462 [Google Scholar]
- 8.Lantzouni E, Frank GR, Golden NH, Shenker RI. Reversibility of growth stunting in early onset anorexia nervosa: a prospective study. J Adolesc Health. 2002;31(2):162–165 [DOI] [PubMed] [Google Scholar]
- 9.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000; (314):1–27 [PubMed] [Google Scholar]
- 10.Hebebrand J, Himmelmann GW, Heseker H, Schafer H, Remschmidt H. Use of percentiles for the body mass index in anorexia nervosa: diagnostic, epidemiological, and therapeutic considerations. Int J Eat Disord. 1996;19(4):359–369 [DOI] [PubMed] [Google Scholar]
- 11.Hebebrand J, Casper R, Treasure JL, Schweiger U. The need to revise the diagnostic criteria for anorexia nervosa. J Neural Transm. 2004;111(7):827–840 [DOI] [PubMed] [Google Scholar]
- 12.McLaren DS, Read WWC. Classification of nutritional status in early childhood. Lancet. 1972;2(7769):146–148 [DOI] [PubMed] [Google Scholar]
- 13.Moore DJ, Durie PR, Forstner GG, Pencharz PB. The assessment of nutritional status in children. Nutr Res. 1985;5:797–799 [Google Scholar]
- 14.Phillips S, Edlbeck A, Kirby M, Goday P. Ideal body weight in children. Nutr Clin Pract. 2007;22(2):240–245 [DOI] [PubMed] [Google Scholar]
- 15.Fairburn CG, Cooper Z. The eating disorders examination. In: Fairburn CG, Wilson GT, eds. Binge Eating: Nature, Assessment, and Treatment, 12th ed. New York, NY: Guilford Press; 1993:317–360 [Google Scholar]
- 16.American Psychiatric Association. DSM-5 development. Available at: www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=24. Accessed October 20, 2011
- 17.Hamill PV, Drizd TA, Johnson CL, Reed RB, Roche AF, Moore WM. Physical growth: National Center for Health Statistics percentiles. Am J Clin Nutr. 1979;32(3):607–629 [DOI] [PubMed] [Google Scholar]
- 18.Hamwi GJ. Therapy: changing dietary concepts. In: Danowski TS, ed. Diabetes Mellitus: Diagnosis and Treatment. Vol. 1 New York, NY: American Diabetes Association; 1964:73–78 [Google Scholar]
- 19.Peebles R, Hardy KK, Wilson JL, Lock JD. Are diagnostic criteria for eating disorders markers of medical severity? Pediatrics. 2010;125(5):e1193–e1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bordowitz R, Morland K, Reich D. The use of an electronic medical record to improve documentation and treatment of obesity. Fam Med. 2007;39(4):274–279 [PubMed] [Google Scholar]
- 21.Rosen DS, American Academy of Pediatrics Committee on Adolescence . Identification and management of eating disorders in children and adolescents. Pediatrics. 2010;126(6):1240–1253 [DOI] [PubMed] [Google Scholar]