Abstract
BACKGROUND:
In the United States, drowning is the second leading cause of unintentional injury death in children aged 1 to 19 years, accounting for nearly 1100 deaths per year. Although a decline in overall fatal drowning deaths among children has been noted, national trends and disparities in pediatric drowning hospitalizations have not been reported.
METHODS:
To describe trends in pediatric drowning in the United States and provide national benchmarks for state and regional comparisons, we analyzed existing data (1993–2008) from the Nationwide Inpatient Sample, the largest, longitudinal, all-payer inpatient care database in the United States. Children aged 0 to 19 years were included. Annual rates of drowning-related hospitalizations were determined, stratified by age, gender, and outcome.
RESULTS:
From 1993 to 2008, the estimated annual incidence rate of pediatric hospitalizations associated with drowning declined 49% from 4.7 to 2.4 per 100 000 (P < .001). The rates declined for all age groups and for both males and females. The hospitalization rate for males remained consistently greater than for females at each point in time. Rates of fatal drowning hospitalization declined from 0.5 (95% confidence interval, 0.4–0.7) deaths per 100 000 in 1993–1994 to 0.3 (95% confidence interval, 0.2–0.4) in 2007–2008 (P < .01). No difference was observed in the mean hospital length of stay over time.
CONCLUSIONS:
Pediatric hospitalization rates for drowning have decreased over the past 16 years. Our study provides national estimates of pediatric drowning hospitalization that can be used as benchmarks to target and assess prevention strategies.
KEY WORDS: drowning, pediatric, hospitalization, incidence, trends
What’s Known On This Subject:
In the United States, drowning is the second leading cause of unintentional injury death among children (1–19), accounting for >1000 deaths per year. Total lifetime costs in 2000 were estimated to be $2.6 billion for children aged 0 to 14.
What This Study Adds:
National trends in pediatric drowning hospitalizations by age and gender have not been reported. This study provides benchmarks that can be used for state and regional comparisons and monitoring of injury prevention efforts.
In the United States, drowning is the second leading cause of unintentional injury death among children aged 1 to 19 years, accounting for >1000 deaths per year.1 In 2009, an estimated 5654 children aged 0 to 19 years sustained nonfatal drowning injuries, including an estimated 2000 children who were hospitalized for drowning-related injuries.1,2 For every pediatric drowning death, another 2 nonfatal drowning hospitalizations are documented.3 Nonfatal drowning may result in brain damage and long-term disability.3,4 Total lifetime costs associated with drowning were estimated to exceed $5.3 billion in 2000, including $2.6 billion for children aged 0 to 14 years.5 Although a decline in fatal drowning among children has been noted, national trends in pediatric drowning hospitalizations by age and gender have not been reported.
Drowning characteristics differ by age and gender.6 Young children (<4 years of age) have the highest mortality rate from drowning and are more likely to drown while bathing or falling into water. Older children are more likely to drown while swimming in open water.6,7 Males are 4 to 6 times more likely than females to experience a drowning injury, attributable to factors such as overestimation of swimming abilities and greater use of alcohol among adolescent males.8 Other risk factors for childhood drowning include lack of barriers and fencing around swimming pools, inadequate adult supervision, not wearing a personal floatation device, use of personal watercraft by children, and seizure disorders.7,9 Alcohol is involved in an estimated 30% to 50% of adolescent and adult drownings.10,11
In this study, we examined trends in child drowning hospitalization in the United States, including trends by age, gender, outcome, region, and mechanism. Assessing drowning hospitalizations is critical to understanding the most severe cases, because death certificate data often fail to capture the full extent of the problem, and drowning hospitalization cases capture cases with the greatest risk of long-term cognitive consequences. We also established national benchmarks for state and regional comparisons and discussed the implications of noted trends for injury prevention policy and practice.
Methods
Our study used administrative discharge data from the 1993–2008 Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ), Rockville, Maryland. The NIS is created by AHRQ from the State Inpatient Databases provided by public and private statewide data organizations from participating states as part of a federal-state-private collaboration. The NIS is the largest, longitudinal, all-payer inpatient care database in the United States, with an average of 8 million hospitalizations from ∼1000 hospitals each year. The NIS approximates a 20% stratified random sample of all short-term US community hospitals. The sampling frame for the 2008 NIS includes State Inpatient Databases from ∼95% of all hospital discharges in the United States. Data were obtained from the HCUP Central Distributor, with approval from the institutional review board at the Johns Hopkins University. The NIS includes both patient level data such as demographics (eg, age, gender, race), admission type and source, up to 15 ICD-9-CM diagnostic and procedure codes, insurance status, total hospital charges, length of stay, discharge disposition, and hospital level information (eg, hospital ownership, number of beds, urban/rural, geographic region, and teaching status).
For this study, eligibility was limited to children who were ages 0 to 19 years at admission and who were hospitalized with a primary or secondary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code for drowning injury (994.1). Patients who died while hospitalized were included. The NIS contains no unique identifiers, so to reduce the effects of double counting multiple hospitalizations for the same drowning-related injury, the hospitalizations of patients who were discharged to another short-term care hospital were not included in the analysis (ie, only the terminal hospital admission was included).12 This assumes that these cases would likely be captured at the point of the definitive drowning care in the receiving hospital records.
Circumstances of drowning were determined based on the external cause of injury code (E-Code). We categorized circumstances of drowning injury into 5 groups: recreational swimming and diving (E910.2–910.3), in bathtubs (E910.4), other drowning activities (E910.0, E910.1, E910.8, E910.9), all other E-codes, and missing (E-code not available). Similarly, we determined intent of injury (ie, unintentional, intentional, undetermined) by using the available E-codes.
To generate national estimates of hospitalizations from the NIS, we used the appropriately scaled discharge weights provided by HCUP.13 With these weights, national estimates of hospitalization rates are rendered comparable across years, despite the varying number of states participating in each year of the HCUP project. All analyses were performed with the appropriate weighted stratified sample design, using the survey command (SVY) options within Stata 10.0/MP (College Station, TX). For the incidence rate calculations, we used US Census estimates for the national civilian population at midyears during this time interval.14 We present estimated crude hospitalization incidence rates by age, gender, and outcome. Because E-codes were missing for up to 55% of hospitalizations before 1997, we compared 2-year aggregate data for years 1998–1999 and 2007–2008 (where codes were missing for only ∼10% of hospitalizations) to evaluate changes in drowning mechanism and intent over time.
Results
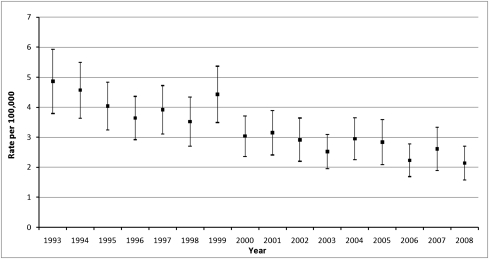
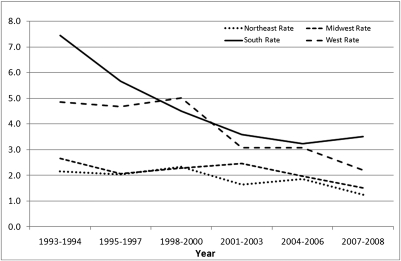
Pediatric hospitalizations for drowning declined 51% from an estimated 3623 in 1993 to 1781 in 2008. From 1993 to 2008, the estimated annual incidence rate of pediatric hospitalizations associated with drowning declined 57% from 4.9 to 2.1 per 100 000 (see Fig 1). The rates declined significantly for all ages and for both genders, although the rate for males remained greater at each point in time (see Table 1). In-hospital mortality declined 42% from an estimated 359 deaths in 1993 to 207 deaths in 2008. Fatal hospitalization rates declined by 40%, from 0.5 (95% confidence interval, 0.4–0.7) deaths per 100 000 in 1993–1994 to 0.3 (95% confidence interval, 0.2–0.4) in 2007–2008. Hospitalization rates decreased significantly across all geographic regions of the United States, with the greatest decline in drowning hospitalization rates occurring in the South, where the overall drowning rate fell from 7.5 hospitalizations per 100 000 in 1993–1994 to 3.5 per 100 000 in 2007–2008 (P < .001). Figure 2 illustrates the trends in pediatric drowning hospitalizations by region over the 16-year period. It is noteworthy that drowning hospitalization rates remain higher in the West and South than in the Northeast or Midwest, despite the declines of >50% in the West and South.
FIGURE 1.
Pediatric drowning hospitalizations by year, 1983–2008 (rates per 100 000 population, 95% confidence intervals).
TABLE 1.
National Trends in the Incidence of Pediatric Drowning Hospitalization by Fatality, Gender, and Age (Rates per 100 000 and 95% Confidence Intervals)
| 1993–1994 | 1995–1997 | 1998–2000 | 2001–2003 | 2004–2006 | 2007–2008 | |
|---|---|---|---|---|---|---|
| Overall | 4.7 (4.0–5.4) | 3.9 (3.4–4.3) | 3.7 (3.2–4.1) | 2.9 (2.5–3.3) | 2.7 (2.3–3.1) | 2.4 (1.9–2.8)a |
| Fatality | ||||||
| Nonfatal | 4.2 (3.6–4.9) | 3.4 (3.0–3.8) | 3.3 (2.9–3.7) | 2.6 (2.2–2.9) | 2.4 (2.0–2.7) | 2.1 (1.7–2.5)a |
| Fatal | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | 0.4 (0.3–0.4) | 0.3 (0.2–0.3) | 0.3 (0.2–0.4) | 0.3 (0.2–0.4)a |
| Gender | ||||||
| Male | 5.8 (4.9–6.7) | 5.0 (4.4–5.0) | 4.6 (4.0–5.2) | 3.6 (3.1–4.1) | 3.4 (2.9–3.9) | 2.9 (2.4–3.5)a |
| Female | 3.6 (3.0–4.2) | 2.7 (2.3–3.1) | 2.7 (2.3–3.1) | 2.1 91.8–2.4) | 1.9 (1.6–2.2) | 1.8 (1.4–2.2)a |
| Age, y | ||||||
| 0–4 | 12.7 (10.6–14.8) | 10.2 (8.8–11.6) | 9.3 (7.8–10.7) | 7.2 (6.1–8.3) | 6.8 (5.7–7.9) | 5.6 (4.4–6.8)a |
| 5–9 | 2.4 (1.9–2.9) | 2.6 (2.2–3.0) | 2.5 (2.1–2.8) | 2.2 (1.7–2.6) | 2.1 (1.7–2.5) | 1.8 (1.4–2.3)a |
| 10–14 | 1.8 (1.4–2.1) | 1.4 (1.1–1.7) | 1.8 (1.6–2.1) | 1.2 (1.0–1.4) | 1.1 (0.8–1.3) | 1.1 (0.8–1.4)a |
| 15–19 | 1.3 (1.0–1.6) | 1.2 (1.0–1.4) | 1.4 (1.2–1.6) | 1.1 (0.9–1.3) | 0.8 (0.7–1.0) | 0.9 (0.7–1.2)a |
Statistically significant difference between 1993–1994 and 2007–2008, P < .05.
FIGURE 2.
Pediatric drowning-related hospitalizations by region, 1993–2008 (rates per 100 000 population).
Table 2 presents national estimates of drowning hospitalization rates by circumstances (eg, swimming/diving, bathtub, etc), stratified by age. Because external cause of injury codes (E-codes) were frequently missing for drowning hospitalizations in the early years of the NIS (through 1997), we compared more recent data years (1998–1999 vs 2007–2008) in which E-codes were available for ∼90% of drowning hospitalizations. Overall, we observed a significant decline (40%) in bathtub-related drowning hospitalizations in children aged 0 to 4 years. Drowning hospitalizations due to swimming and diving decreased by nearly half in older children aged 10 to 14 years. Drowning hospitalizations due to other specified causes also decreased for most age groups. Table 3 provides details of changes in drowning circumstances by age and gender. We also examined intent of injury and found no significant trends for intentional drowning over this time period. Nearly 99% of pediatric drowning hospitalizations with a known, documented external cause of injury code were classified as unintentional in nature.
TABLE 2.
Pediatric Drowning Hospitalizations by Circumstances and Age (Rates per 100 000, 95% Confidence Interval)
| 1998–1999 | 2007–2008 | |
|---|---|---|
| Swimming/diving (E910.2-3) | ||
| Overall | 0.5 (0.5–0.6) | 0.4 (0.3–0.5)* |
| 0–4 y | 0.6 (0.4–0.7) | 0.5 (0.3–0.6) |
| 5–9 y | 0.6 (0.5–0.8) | 0.4 (0.3–0.6) |
| 10–14 y | 0.6 (0.4–0.8) | 0.3 (0.2–0.4)* |
| 15–19 y | 0.4 (0.3–0.5) | 0.3 (0.2–0.4) |
| Bathtub (E910.4) | ||
| Overall | 0.4 (0.3–0.5) | 0.3 (0.2–0.3)* |
| 0–4 y | 1.4 (1.1–1.8) | 0.8 (0.6–1.0)* |
| 5–9 y | —a | —a |
| 10–14 y | —a | —a |
| 15–19 y | —a | —a |
| Other Drowning (E910.0,1,8,9) | ||
| Overall | 2.4 (1.9–2.9) | 1.4 (1.0–1.7)* |
| 0–4 y | 6.6 (5.2–8.1) | 3.6 (2.8–4.5)* |
| 5–9 y | 1.6 (1.2–2.0) | 1.3 (0.9–1.6) |
| 10–14 y | 0.9 (0.7–1.2) | 0.5 (0.3–0.7)* |
| 15–19 y | 0.6 (0.5–0.8) | 0.3 (0.2–0.4)* |
| Other E-code (not E910) | ||
| Overall | 0.2 (0.1–0.2) | 0.1 (0.1–0.1) |
| 0–4 y | 0.4 (0.2–0.6) | 0.2 (0.1–0.3) |
| 5–9 y | —a | —a |
| 10–14 y | 0.1 (0.1–0.2) | 0.1 (0.0–0.1) |
| 15–19 y | 0.1 (0.0–0.2) | 0.1 (0.0–0.2) |
| Missing E-code | ||
| Overall | 0.5 (0.3–0.6) | 0.2 (0.3–0.3)* |
| 0–4 y | 1.1 (0.8–1.4) | 1.0 (0.5–1.5) |
| 5–9 y | 0.3 (0.1–0.4) | 0.3 (0.1–0.5) |
| 10–14 y | 0.3 (0.1–0.4) | 0.1 (0.0–0.2) |
| 15–19 y | 0.3 (0.2–0.4) | 0.1 (0.0–0.1)* |
Rates unstable (<0.1/100 000).
*P < .05
TABLE 3.
Pediatric Drowning Hospitalizations by Circumstances, Age, and Gender (Rates per 100 000, 95% Confidence Interval)
| 1998–1999 | 2007–2008 | |
|---|---|---|
| Swimming/diving | ||
| Male | 0.8 (0.6–0.9) | 0.6 (0.4–0.7) |
| 0–4 y | 0.8 (0.5–1.1) | 0.6 (0.3–0.8) |
| 5–9 y | 0.8 (0.6–1.1) | 0.7 (0.4–1.0) |
| 10–14 y | 0.8 (0.5–1.0) | 0.4 (0.2–0.6)* |
| 15–19 y | 0.7 (0.4–0.9) | 0.6 (0.4–0.8) |
| Female | 0.3 (0.2–0.4) | 0.2 (0.2–0.3) |
| 0–4 y | 0.4 (0.2–0.5) | 0.4 (0.2–0.5) |
| 5–9 y | 0.4 (0.2–0.6) | 0.3 (0.1–0.4) |
| 10–14 y | 0.5 (0.2–0.7) | 0.3 (0.1–0.4) |
| 15–19 y | 0.1 (0.0–0.2) | 0.1 (0.0–0.2) |
| Bathtub | ||
| Male | 0.4 (0.3–0.5) | 0.2 (0.2–0.3) |
| 0–4 y | 1.3 (0.9–1.8) | 0.9 (0.6–1.1)* |
| 5–9 y | —a | 0.1 (0.0–0.2) |
| 10–14 y | 0.1 (0.0–0.3) | —a |
| 15–19 y | —a | —a |
| Female | 0.4 (0.3–0.5) | 0.3 (0.2–0.3)* |
| 0–4 y | 1.5 (1.1–2.0) | 0.8 (0.5–1.1)* |
| 5–9 y | —a | —a |
| 10–14 y | —a | —a |
| 15–19 y | —a | —a |
| Other Drowning (E910) | ||
| Male | 3.0 (2.4–3.6) | 1.7 (1.3–2.1)* |
| 0–4 y | 8.1 (6.2–10.0) | 4.0 (2.9–5.0)* |
| 5–9 y | 2.1 (1.6–2.6) | 1.2 (0.9–1.6)* |
| 10–14 y | 1.2 (0.8–1.5) | 0.9 (0.5–1.2) |
| 15–19 y | 1.0 (0.7–1.2 | 0.6 (0.3–0.8)* |
| Female | 1.8 (1.4–2.2) | 1.0 (0.8–1.3)* |
| 0–4 y | 5.1 (4.0–6.3) | 2.7 (2.0–3.5)* |
| 5–9 y | 1.2 (0.8–1.5) | 0.9 (0.6–1.3) |
| 10–14 y | 0.7 (0.5–1.0) | 0.3 (0.1–0.4)* |
| 15–19 y | 0.3 (0.2–0.5) | 0.1 (0.0–0.2)* |
| Other E-code (not E910) | ||
| Male | 0.2 (0.1–0.3) | 0.1 (0.1–0.2) |
| 0–4 y | 0.5 (0.2–0.8) | 0.3 (0.1–0.5) |
| 5–9 y | 0.1 (0.0–0.2) | —a |
| 10–14 y | 0.2 (0.1–0.4) | 0.1 (0.0–0.1) |
| 15–19 y | 0.1 (0.0–0.2) | 0.2 (0.1–0.3) |
| Female | 0.1 (0.1–0.2) | 0.1 (0.0–0.1) |
| 0–4 y | 0.3 (0.1–0.5) | 0.1 (0.0–0.2)* |
| 5–9 y | —a | —a |
| 10–14 y | —a | —a |
| 15–19 y | 0.1 (0.0–0.2) | —a |
Rates unstable (<0.1/100 000).
*P < .05.
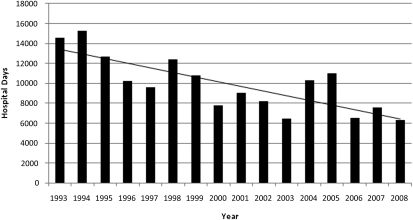
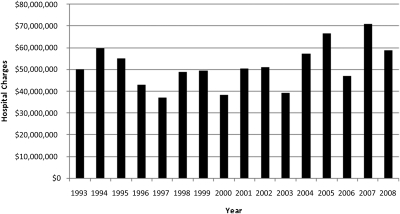
Figure 3 illustrates the total estimated hospital days for pediatric drowning by year. Total annual hospital days declined from an estimated 14 570 days in 1993 to ∼6295 days in 2008. No trend in mean hospital length of stay was observed over the 16-year period. Figure 4 provides estimates of total hospital charges by year. Interestingly, over this period, the decline in drowning hospitalizations appears to have partially offset the increase in mean charges due to health care cost inflation. As a result, total hospital charges for pediatric drowning are similar in recent years to the early 1990s.
FIGURE 3.
Estimated total hospital days for pediatric drowning, 1993–2008 (ages 0–19 years, United States).
FIGURE 4.
Total hospital charges for pediatric drowning, 1993–2008 (ages 0–19 years, United States).
Discussion
Consistent with decreases in pediatric drowning mortality, we observed a significant decline in the rate of pediatric drowning hospitalizations, primarily because of decreases in the South and West. This is an important finding that provides some evidence of a true decrease in drowning incidents, rather than a possible shift from fatal out-of-hospital drowning to nonfatal in-hospital cases. Compared with the Northeast and Midwest, children remain more likely to be hospitalized for drowning in the West and South, although the gap has closed considerably in recent years.
Because of the extensive missing data on external cause of injury in the early years of HCUP, we limited our assessment of the trends in drowning circumstances to 1998–2008. By limiting our analyses to later years, we also avoid potential confounding that may have occurred because of changes in hospital admitting practices in response to managed care and cost containment pressures that occurred in the early to mid-1990s. Between 1998–1999 and 2007–2008, we observed a significant change in drowning hospitalization rates for selected ages and mechanisms. Reductions in bathtub drowning hospitalizations among the youngest children may reflect a response to targeted injury prevention efforts that have been aimed at parents and caregivers of young children, encouraging increased vigilance in supervision. In addition, a focus on the drowning risks associated with infant bathtub seats may also have contributed to the observed reduction.15 Hospitalizations due to “other” drowning circumstances also decreased for most age groups. However, the lack of detail in the external cause of injury codes within the ICD-9-CM severely limits our ability to monitor and track progress by specific drowning circumstances. The transition of hospital discharge data collection systems to ICD-10-CM may improve drowning surveillance because of the expanded detail in coding.16
Previous studies have concluded that medical care for severe submersion episodes contributes minimally to improvements in survival.17–19 Interestingly, we did observe a decrease in the rate of in-hospital deaths over the 14-year period, although the in-hospital case fatality did not change significantly. Although improvements in treatment might be having an impact on survival, it is not clear from these data what level of neurologic functioning survivors may have. An alternate explanation is that better decision-making in the prehospital period may be resulting in more pronouncement of death in the field for unsurvivable cases. Others have speculated that where children swim may be shifting from natural bodies of water to more supervised settings, such as pools and beaches with lifeguards. In such settings, individuals (lifeguards and/or bystanders) with training in cardiopulmonary resuscitation (CPR) may allow for immediate resuscitation at the site of a drowning incident, and this could have a positive impact on in-hospital survival.10 However, these hospital discharge data do not include any information on prehospital CPR or the time between submersion and initial resuscitation. Although trauma registries may be more likely to capture this additional information, trauma registries vary in their inclusion of drowning cases. Therefore, a separate surveillance approach for drowning may be needed.
Over the time period of our study, important public and private efforts to reduce the risk of drowning in children have been promoted, such as installation of four-sided pool fencing, the use of personal floatation devices, and the encouragement to swim in supervised areas. Swimming lessons have generally been endorsed for the protection of children aged 5 and older by a variety of public health authorities. Recent evidence also suggests that participation in formal swimming lessons is associated with an 88% reduction in the risk of drowning in children aged 1 to 4 years.3,20 All of these interventions offer the potential to further reduce drowning hospitalizations in children. However, better surveillance capacity is needed to capture the relevant risk and protective factors associated with childhood drowning. Detailed information on the circumstances of drowning (eg, type of swimming location, time of day, supervision, time to CPR, etc) would assist in both monitoring prevention practices as well as in identifying areas for targeted intervention. Similarly, postacute outcomes data are needed to assess the quality of life for pediatric drowning.
Several limitations are worth noting. First, we relied on the ICD-9-CM diagnosis codes to identify drowning, and thus misclassification of drowning cases is a possibility. Also, a significant proportion of pediatric drowning cases were indeterminate with regard to external cause because of nonspecific or missing codes. Last, the NIS does not include functional impairment or cognitive measures at discharge. As such, outcomes are limited to in-hospital survival only.
Conclusions
Although pediatric hospitalization rates for drowning have decreased over the past 14 years, drowning remains a significant public health problem. Hospitalization rates remain higher in the West and South. One possible explanation is that children in the West and South tend to have more exposure to drowning because of warmer climates and readily available recreational swimming opportunities. However, differences in prehospital response, time to resuscitation, and prehospital medical control protocols for pediatric drowning may also affect the proportion of children who make it to the hospital for treatment. We did observe some improvement in hospital survival for pediatric drowning, although we were not able to assess the cognitive level or functional outcome of survivors.
Given the extraordinary lifetime costs for children experiencing near-drowning, future efforts should continue to focus on translating effective drowning prevention strategies into public health practice. Policy and educational interventions aimed at increasing the use of personal floatation devices, reducing the inappropriate use of personal watercraft, increasing the availability of water supervision, assuring pool fencing, and increasing participation by children in formal swimming lessons offer the potential to reduce drowning hospitalizations further in the coming years. Our study provides national estimates of pediatric drowning hospitalizations that can be used as benchmarks to inform drowning prevention efforts and to help target interventions to high-risk areas. Given the significant burden of drowning in both real and human costs, additional monitoring of pediatric drowning is needed.
Acknowledgments
Dr Bowman and this study received support from Cooperative Agreement 5R49CE001507 from the Centers for Disease Control and Prevention. Dr Aitken received support from the National Institutes of Health/National Center for Research Resources Clinical and Translational Research grant UL1RR029884 (Arkansas Translational Research Institute, University of Arkansas for Medical Sciences).
Glossary
- AHRQ
Agency for Healthcare Research and Quality
- CPR
cardiopulmonary resuscitation
- E-code
External Cause of Injury
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- NIS
Nationwide Inpatient Sample
Footnotes
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
References
- 1.Web-based Inquiry Statistic Query and Reporting System. Atlanta, GA: National Center for Injury Prevention and Control; 2009. Available at: www.cdc.gov/injury/wisqars/. Accessed August 14, 2011
- 2.National Statistics on Children. HCUPnet, Kids’ Inpatient Database 2009. Rockville, MD: Agency for Healthcare Research and Quality. Available at: http://hcupnet.ahrq.gov. Accessed August 14, 2011
- 3.American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention . Prevention of drowning. Pediatrics. 2010;126(1):178–18520498166 [Google Scholar]
- 4.American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention . Prevention of drowning in infants, children, and adolescents. Pediatrics. 2003;112(2):437–439 [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein EA, Corso PS, Miller TR, et al. The Incidence and Economic Burden of Injuries in the United States. New York, NY: Oxford University Press; 2006 [Google Scholar]
- 6.Quan L, Cummings P. Characteristics of drowning by different age groups. Inj Prev. 2003;9(2):163–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brenner RA, Trumble AC, Smith GS, Kessler EP, Overpeck MD. Where children drown, United States, 1995. Pediatrics. 2001;108(1):85–89 [DOI] [PubMed] [Google Scholar]
- 8.Doll LS, Haas EN. Handbook of Injury and Violence Prevention. New York, NY: Springer; 2007 [Google Scholar]
- 9.Centers for Disease Control and Prevention. Water-Related Injuries: Fact Sheet. 2009. Atlanta, GA: Centers for Disease Control and Prevention. Available at: www.cdc.gov/homeandrecreationalsafety/water-safety/waterinjuries-factsheet.html. Accessed August 17, 2011 [Google Scholar]
- 10.Brenner RA. Prevention of drowning in infants, children, and adolescents. Pediatrics. 2003;112(2):440–445 [DOI] [PubMed] [Google Scholar]
- 11.Dietz PE, Baker SP. Drowning: epidemiology and prevention. Am J Public Health. 1974;64(4):303–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westfall JM, McGloin J. Impact of double counting and transfer bias on estimated rates and outcomes of acute myocardial infarction. Med Care. 2001;39(5):459–468 [DOI] [PubMed] [Google Scholar]
- 13.Barrett M, Coffey R, Levit K, Nagamine M. Population Denominator Data for Use with the HCUP Databases. Rockville, MD: Agency for Healthcare Research and Quality; 2006. Report No. 2006-06
- 14.Intercensal population estimates. US Census Bureau 2008. Available at: www.census.gov/popest/data/datasets.html. Accessed August 20, 2011
- 15.Rauchschwalbe R, Brenner RA, Smith GS. The role of bathtub seats and rings in infant drowning deaths. Pediatrics. 1997;100(4). Available at: www.pediatrics.org/cgi/content/full/100/4/e1 [DOI] [PubMed] [Google Scholar]
- 16.Watzlaf VJ, Garvin JH, Moeini S, Anania-Firouzan P. The effectiveness of ICD-10-CM in capturing public health diseases. Perspect Health Inf Manag. 2007;4:6. [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings P, Quan L. Trends in unintentional drowning: the role of alcohol and medical care. JAMA. 1999;281(23):2198–2202 [DOI] [PubMed] [Google Scholar]
- 18.Graf WD, Quan L, Cummings P. Outcome of children after near drowning. Pediatrics. 1998;101(1 pt 1):160–161 [DOI] [PubMed] [Google Scholar]
- 19.Kyriacou DN, Arcinue EL, Peek C, Kraus JF. Effect of immediate resuscitation on children with submersion injury. Pediatrics. 1994;94(2 pt 1):137–142 [PubMed] [Google Scholar]
- 20.Brenner RA, Taneja GS, Haynie DL, et al. Association between swimming lessons and drowning in childhood: a case-control study. Arch Pediatr Adolesc Med. 2009;163(3):203–210 [DOI] [PMC free article] [PubMed] [Google Scholar]