Abstract
Objective
Although many adolescents use and abuse illicit drugs, few of those who could benefit from substance abuse treatment ever receive these services. The present study examines the prevalence of utilization of substance abuse treatment in national samples of adolescents over the past 22 years and identifies characteristics associated with receipt of these services.
Method
Monitoring the Future data on lifetime utilization of substance abuse treatment was available for 12th grade students who reported any lifetime illicit drug use from 1987 to 2008 (N = 25,537). After describing the prevalence of treatment utilization over this time period, logistic regression was used to examine potential predictors of treatment utilization.
Results
The overall prevalence of treatment utilization has remained relatively unchanged over the past 22 years. In multivariable models, adolescents reporting a greater frequency of lifetime use of marijuana or cocaine were more likely to receive substance abuse treatment. Additionally, substance abuse treatment utilization was more likely in those who received other mental health services.
Conclusion
Despite increased evidence for the effectiveness of substance abuse treatment, utilization of these services by adolescents has remained low and relatively stable over the past 22 years. Attempts to increase utilization of substance abuse treatment services would likely benefit from building on existing connections with mental health treatment.
Keywords: substance abuse, marijuana, treatment, cocaine, adolescents
1. Introduction
Lifetime illicit drug use is common among adolescents, with rates of substance use increasing as adolescents age (Johnston, O'Malley, Bachman, & Schulenberg, 2009; SAMHSA, 2009). Nearly half (48%) of 12th graders in the United States in 2010 report lifetime use of an illicit drug and 24% report current (defined as past 30 day) use of illicit drugs (Johnston et al., 2010). Although there has been a slight gradual decline in lifetime illicit drug use among high school seniors since a recent high point of 55% in 1999, the decline has leveled with some evidence of rates starting to increase again (Johnston et al., 2010). Overall, illicit drug use among the nation's youth continues to remain widespread and a source of concern (Johnston et al., 2009).
Despite the high prevalence of substance use, it is likely that the vast majority of adolescents who might benefit from substance abuse (SA) treatment never actually receive any form of specialty SA services (SAMHSA, 2009; Wu, Hoven, Tiet, & Wicks, 2002; Wu, 2003). In 2008, estimates indicate that, during the prior 12-months, SA treatment was received by only 9.9% of adolescents with an illicit drug use disorder and 5.9% of those with an alcohol use disorder (SAMHSA, 2009).
In order to identify potential gaps in care for illicit substance use, it is important to identify factors associated with the likelihood of receiving SA treatment among adolescents. After accounting for demographic differences, greater severity of alcohol or drug problems is consistently associated with an increased likelihood of receiving SA treatment (Wu et al., 2002; Wu, 2003).
To the best of our knowledge, all prior research examining illicit drug use and treatment utilization in adolescents in the United States has been based on data from a single large survey and has been limited to analyses of past 12-month SA treatment in those with diagnosable substance abuse or dependence (Wu et al., 2002; Wu, 2003). Because many adolescents who use illicit substances are at elevated risk for negative consequences, but may not yet have time to develop a diagnosable substance use disorder, prior research on SA treatment has missed many of those could benefit from SA treatment services. Also, over the past 20 years, the volume and quality of the evidence supporting the efficacy of SA treatment for adults and adolescents has increased dramatically (Miller & Wilbourne, 2002; Prendergast, Podus, Chang, & Urada, 2002). However, little attention has been given to potential changes in national rates of SA treatment utilization over time.
The present study examined the prevalence rates of SA treatment utilization across the past 22 years and considered the extent to which they may have changed. Additionally, we examined demographic and psychosocial predictors of receiving lifetime SA treatment. A clearer understanding of these characteristics could help refine future outreach and intervention efforts in adolescent substance users.
2. Methods
2.1. Sample
The data for the present study came from Monitoring the Future (MTF), an ongoing study that has annually surveyed a nationally representative sample of 12th grade students in the coterminous U.S. since 1975 (Johnston et al., 2009). The present study examines only 1987–2008 cohorts due to question availability. Variables of interest were included in one of the six questionnaire forms distributed randomly in each classroom in each school. Sampling and design procedures have been consistent across the years; detailed descriptions of MTF procedures are available elsewhere (Bachman, Johnston, O'Malley, & Schulenberg, 2006; http://www.monitoringthefuture.org). These analyses utilized data from 12th graders who were asked about use of treatment and were limited to those who reported lifetime use of any illicit drug (including marijuana, cocaine, heroin, other narcotics, LSD, tranquilizers, amphetamines, and/or barbiturates/sedatives without a prescription).
2.2. Measures
Respondents were asked: “Have you ever attended a treatment program for alcohol or drug abuse where you stayed overnight?” and “Have you ever received any other kind of professional counseling, treatment, or therapy because of your use of alcohol or drugs?” Responses were combined to create an indicator of any lifetime SA treatment (recoded as no/yes).
The present analyses included gender and an indicator of race/ethnicity (Caucasian, African American, Hispanic, or Other race). Parents' education was coded as the highest level of either the mother's or father's education (recoded as high school or less vs. some college or more.) The participant's school was coded as located in the South, North Central, West or Northeast as well as in an urban, suburban or rural location.
School factors that were examined included self-reported high school grades (“A” = 9 to “D” = 1), and number of days school was skipped in the past four weeks (“none” = 1 to “four or more days” = 5). Respondents reported their weekly average number of nights out for fun and recreation (“Less than one” = 1 to “six to seven” = 6).
Measures of frequency of lifetime use of the three most common substances of abuse in the MTF (Johnston et al., 2009) - alcohol, marijuana and cocaine - were each coded on a 7-point scale ranging from “0 occasions” to “40 or more”.
Respondents were asked how many times (if any) in the past 12 months s/he had seen a doctor or other professional for a routine physical check-up or for some physical illness or symptom. The response options were “None” = 1 to “10+ times” = 6. Responses to these two questions were combined to create an indicator of any visit to a professional for medical treatment (recoded as no/yes). Respondents were also asked how many times (if any) in the past 12 months s/he had seen a doctor or other professional for some emotional or psychological problem or symptom (recoded no/yes).
2.3. Data Analysis
We first describe the prevalence of use of SA treatment from 1987-2008 among lifetime illicit drug users. Logistic regression was used with year and year-squared as covariates to examine possible linear and quadratic effects of time on the odds of SA treatment utilization. Next, we estimated the bivariate associations between participant characteristics and treatment utilization. Finally, a multivariate logistic regression analysis examined the impact of the adolescent characteristics on odds of SA treatment services, controlling all other variables. The analyses were performed in SAS® v9.2 accounting for the complex multistage sampling design, and the data were weighted to adjust for differential selection probabilities; an alpha of p < 0.01 was chosen due to the large sample size.
3. Results
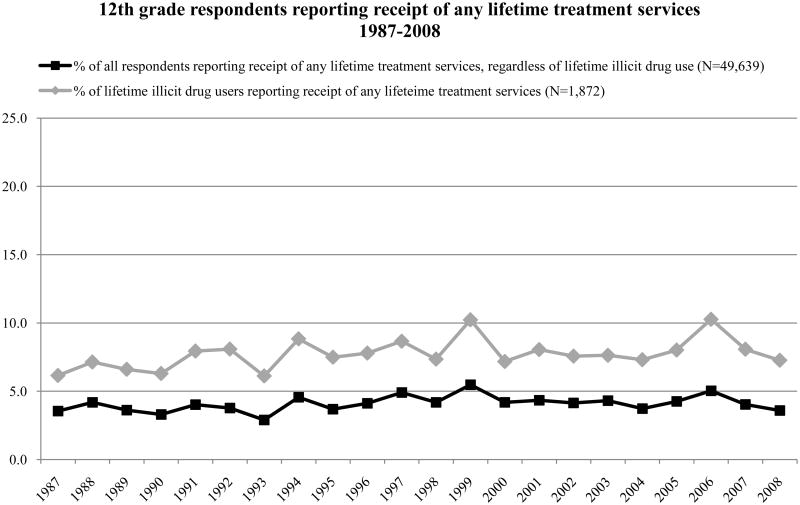
Of the 57,711 initial respondents, 25,537 reported use of an illicit substance in their lifetime and were the basis for the remaining analyses. From 1987 to 2008 the prevalence of lifetime SA service utilization among high school seniors who reported lifetime use of an illicit substance ranged from 6.1% to 10.3% (Figure 1). No linear or quadratic effects were found for time. Across all years, 2.0% of participants reported any lifetime SA residential treatment and 6.9% reported any other lifetime SA treatment. In bivariate analyses, all adolescent characteristics, with the exception of past 12-month physical health medical visits, were associated with likelihood of receiving SA treatment (Table 1). Receipt of SA treatment was more common in males, Caucasian students (relative to Black and Hispanic students), those with higher parent education, those from North Central (relative to the North East) and rural areas (vs. suburban or urban), and those with lower grades, who skipped more days of school, and who spent more evenings out with friends. Adolescents with higher lifetime frequencies of alcohol, marijuana, and cocaine use, as well as those with a mental health visit in the past year, were more likely to have received SA treatment.
Figure 1.
•The Monitoring the Future study is an ongoing annual survey of the behaviors, attitudes and values of American secondary school students. Since 1975, the study has collected confidential surveys administered in classrooms by trained interviewers for nationally representative samples of 12th grade students in the coterminous United States. Procedures have remained consistent over the years; for further study details see http://www.monitoringthefuture.org.
Table 1.
Characteristics associated with receipt of substance abuse treatment among adolescents reporting illicit drug use.
| Respondent Characteristics | Percentage receiving treatment | Bivariate Odds Ratio (99% CI) | Multivariate Odds Ratio (99% CI) |
|---|---|---|---|
| Gender | |||
| Female (ref.) | 6.77 | ||
| Male | 8.36 | 1.26 (1.08 – 1.46)* | 1.05 (0.87 – 1.27) |
| Parents' Education | |||
| ≤ high school (ref.) | 6.67 | ||
| At least some college | 8.04 | 1.22 (1.03 – 1.45)* | 1.09 (0.86 – 1.37) |
| Race/Ethnicity | |||
| Caucasian(ref.) | 8.31 | ||
| African American | 3.15 | 0.36 (0.24 – 0.53)* | 0.71 (0.43 – 1.18) |
| Hispanic | 5.98 | 0.70 (0.53 – 0.93)* | 0.69 (0.47 – 1.02)* |
| Other Race | 6.98 | 0.83 (0.61 – 1.11) | 0.97 (0.66 – 1.41) |
| Region | |||
| North East (ref.) | 6.61 | ||
| South | 6.67 | 1.01 (0.80 – 1.27) | 1.13 (0.83 – 1.54) |
| North Central | 9.51 | 1.49 (1.19 – 1.86)* | 1.63 (1.20 – 2.22)* |
| West | 7.94 | 1.22 (0.95– 1.56) | 1.32 (0.95 – 1.82) |
| Urbanicity | |||
| Rural (ref.) | 8.82 | ||
| Suburban | 7.34 | 0.82 (0.68 – 0.99)* | 0.74 (0.57 – 0.96)* |
| Urban | 7.25 | 0.81 (0.66 – 0.99)* | 0.65 (0.49 – 0.87)* |
| Grades | |||
| D=1 to A=9 | 7.50 | 0.90 (0.87 – 0.94)* | 0.96 (0.92 – 1.02) |
| # of days skipped school in past month | |||
| none=1 to 5=four+ days | 7.56 | 1.19 (1.13 – 1.25)* | 0.98 (0.92 – 1.05) |
| Weekly evenings out | |||
| less than one=1 to six to seven=6 | 7.41 | 1.22 (1.14 – 1.29)* | 1.04 (0.97 – 1.12) |
| Number of occasions of lifetime alcohol use | |||
| none=1 to 7=40+ | 7.64 | 1.66 (1.52 – 1.82)* | 1.27 (1.15 – 1.41)* |
| Number of occasions of lifetime marijuana use | |||
| none=1 to 7=40+ | 7.58 | 1.53 (1.46 – 1.61)* | 1.30 (1.22 – 1.38)* |
| Number of occasions of lifetime cocaine use | |||
| none=1 to 7=40+ | 7.51 | 1.57 (1.51 – 1.63)* | 1.35 (1.27 – 1.43)* |
| Past 12-month visit to a doctor/other professional for emotional or psychological problems or symptoms | |||
| No | 6.16 | ||
| Yes | 18.12 | 3.37 (2.74 – 4.14)* | 3.14 (2.43 – 4.05)* |
| Past 12-month visit to a doctor/other professional for check-up or illness or injury | |||
| No | 7.15 | ||
| Yes | 7.41 | 1.04 (0.87 – 1.24) | 0.97 (0.78 – 1.20) |
p < .01
Notes:
- Ns for the bivariate models ranged from 19,715-24,322.
- N for the multivariate logistic model was 16,908 after deleting cases with missing data.
- The final model included dummy variables for each year of the study as control variables. Coefficients are not presented here in order to increase the readability of the table.
- We ran additional analyses. One model excluded the indicator of past 12-month medical visit for emotional/psychological issues; the other included an indicator of lifetime poly-substance use (i.e., use of ≥ 2 illicit substances). The results of these supplementary analyses were similar to those described in Table 1.
Many of these relationships were no longer significant in the multivariate model; however, several factors remained significantly associated with lifetime SA treatment. Adolescents in the North Central region had 1.66 (95%CI: 1.31 – 2.11) greater adjusted odds of treatment receipt than the North East. Relative to those in rural areas, adolescents in suburban (0.75, 95%CI: 0.61 – 0.91) and urban (0.66, 95%CI: 0.53 – 0.82) areas were less likely to receive treatment. The adjusted odds of receiving treatment significantly increased for each one-step increase in self-reported count of lifetime use occasions (on a seven-point scale) of alcohol (OR=1.26, 95%CI: 1.17 – 1.36), marijuana (OR=1.30, 95%CI: 1.24 – 1.36) and cocaine (OR=1.33, 95%CI: 1.27 – 1.40). Adjusted odds of SA treatment increased over three fold (3.09, 95%CI: 2.55 – 3.75) for adolescents who reported past-12 month mental health treatment compared to those who did not.
4. Discussion
Despite growing evidence for the effectiveness of SA treatment (Miller & Wilbourne, 2002; Prendergast et al., 2002) and increased calls to improve access to SA treatment for all individuals in need (APA, 2002; Greenfield, 2005), rates of lifetime utilization of SA treatment in adolescent substance users are low and have remained relatively stable over the past 22 years (ranging from 6% to 10%, with no systematic time trend). Given that 48% of recent American 12th graders report using an illicit drug during their lifetime (Johnston et al., 2010), a clear disparity exists between the potential need for treatment and utilization of SA treatment services.
Greater frequency of lifetime occasions of use of alcohol, marijuana and cocaine was related to a higher likelihood of receiving SA treatment among these national samples of 12th graders who have used an illicit drug at least once. This is consistent with prior research (Wu et al., 2002; Wu, 2003) and, on one hand, appropriate in that treatment should be provided to those with the most extensive substance-related problems. On the other hand, these findings also highlight the fact that many adolescents with lower severity of substance use may be missed within the current treatment system. Given that prior substance use is a strong predictor of future substance-related problems in adolescents (Fuller, 2001; Lynskey, Heath, Bucholz, Slutske, Madden, Nelson et al., 2003; Merline et al., 2004; Miller, Gold, Belkin, & Klahr, 1989; Wagner & Anthony, 2007), intervening early in these individuals could help to reduce a number of subsequent adverse outcomes.
Consistent with prior research (Wu, 2006), SA treatment utilization was more common in those adolescents who already had contact with the mental health treatment system (note that contact for physical health treatment was unrelated). This could reflect the fact that co-occurring psychopathology helped to bring these individuals to the attention of mental health providers who recommended referral to SA treatment. Mental health treatment providers may be well-positioned to facilitate appropriate follow-through on referrals to SA treatment. These findings highlight the importance of establishing strong links between existing mental health and SA treatment services. The fact that rural adolescents were more likely to receive SA treatment than suburban or urban adolescents (significant in multivariate models) suggests particular geographic strengths and gaps in SA treatment availability and warrants further attention.
This study has several limitations. The primary outcome was based on two broad questions, so the extent and type of treatment utilization is unknown. The study intentionally utilized an inclusive definition of illicit drug use and this likely lead to a lower estimated prevalence of service utilization than would have been observed in samples restricted to only those with severe substance use. Unmeasured fluctuations in population factors (e.g., positive perceptions of SA treatment) may have influenced the results. Given our focus on 12th graders, high school drop outs are excluded, suggesting limits on the generalizability of the results.
This study is the first of which we are aware to present long-term trends in lifetime SA service utilization in adolescents. The prevalence of SA treatment utilization has remained low and relatively stable over the past 22 years. Clearly, many at-risk adolescents continue to fail to receive SA treatment. Although those with more severe use are more likely to receive services, it is likely that the gap between the need for services and receipt of this care is greatest in those with less than obvious problems with substance use. Because these individuals are at clear elevated risk for future adverse outcomes relative to those without any substance use, outreach efforts should include a focus on these individuals.
Research Highlights.
Rates of lifetime utilization of substance abuse treatment in adolescent substance users are low and have remained relatively stable over the past 22 years (ranging from 6% to 10%).
Greater frequency of lifetime occasions of use of alcohol, marijuana and cocaine was related to a higher likelihood of receiving substance abuse treatment.
Substance abuse treatment utilization was more common in those adolescents who already had contact with the mental health treatment system.
Acknowledgments
Role of Funding Sources: Data collection for this study was funded by support from the National Institute on Drug Abuse (R01 DA 01411). The content here is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
Footnotes
Contributors: Drs. Ilgen and Schulenberg designed the study and wrote the protocol. Dr. Ilgen and Ms. Czyz conducted literature searches and provided summaries of previous research studies. Ms. Kloska conducted the statistical analysis. Dr. Ilgen wrote the first draft and Ms. Kloska and Drs. Schulenberg, Johnston and O'Malley significantly shaped the revision of the manuscript. All of the authors contributed to, and have approved, the final manuscript.
Conflict of Interest: All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. American Psychiatric Association Position Statement on Inclusion of substance related disorders as psychiatric disorders in any program designed to assure access and quality of care for persons with mental illness. APA Operations Manual, 200913 2002 [Google Scholar]
- Bachman JG, Johnston LD, O'Malley PM, Schulenberg JE. The Monitoring the Future project after thirty-two years: Design and procedures (Monitoring the Future Occasional Paper No 64) Institute for Social Research; Ann Arbor, MI: 2006. [Google Scholar]
- Fuller CM. Factors Associated with Adolescent Initiation of Injection Drug Use. Public Health Reports Hyattsville. 2001;116:136–145. doi: 10.1093/phr/116.S1.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF. Alcohol & Drug Abuse: Is Parity for the Treatment of Substance Use A: Disorders Really Sensible? Psychiatric Services. 2005;56:153–155. doi: 10.1176/appi.ps.56.2.153. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975-2008 volume I: Secondary school students 2009 [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Marijuana use is rising; ecstasy use is beginning to rise; and alcohol use is declining among U S teens. University of Michigan News Service; Ann Arbor, MI: Dec 14, 2010. [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, Statham DJ, Martin NG. Escalation of Drug Use in Early-Onset Cannabis Users vs. Co-twin Controls. JAMA. 2003;289:427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- Merline AC, O'Malley PM, Schulenberg JE, Bachman JG, Johnston LD. Substance use among adults 35 years of age: Prevalence, adulthood predictors, and impact of adolescent substance use. American Journal of Public Health. 2004;94:96–102. doi: 10.2105/ajph.94.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller N, Gold M, Belkin B, Klahr A. The diagnosis of alcohol and cannabis dependence in cocaine dependents and alcohol dependence in their families. Addiction. 1989;84:1491–1498. doi: 10.1111/j.1360-0443.1989.tb03931.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Prendergast ML, Podus D, Chang E, Urada D. The effectiveness of drug abuse treatment: a meta-analysis of comparison group studies. Drug and Alcohol Dependence. 2002;67:53–72. doi: 10.1016/s0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- SAMHSA. Results from the 2008 National Survey on Drug use and Health: national Findings. (NSDUH Series H-36).Office of Applied Studies. 2009 HHS Publication No. SMA 09-4434. [Google Scholar]
- Wagner FA, Anthony JC. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug and Alcohol Dependence. 2007;86:191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Wu P, Hoven C, Tiet Q, P K, Wicks J. Factors associated with adolescent utilization of alcohol treatment services. American Journal of Drug and Alcohol Abuse. 2002;28:353–369. doi: 10.1081/ada-120002978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Fuller CJ. Factors associated with adolescents receiving drug treatment: findings from the National Household Survey on Drug Abuse. Journal of Behavioral Health Services & Research. 2003;30:190–201. doi: 10.1007/BF02289807. [DOI] [PMC free article] [PubMed] [Google Scholar]