Abstract
OBJECTIVE
To determine the cost-effectiveness of medical and surgical management of early pregnancy loss
DESIGN
In the multi-center trial, 652 women with first-trimester pregnancy failure were randomized to medical or surgical management. Analyses of cost, effectiveness and incremental cost-effectiveness ratios and utilities were conducted.
SETTING
Analysis of data from a multi-center trial
PATEINTS
Secondary analysis of a multi-center trial
INTERVENTIONS
Cost effective analysis
MAIN OUTCOME
Cost and effectiveness of competing treatment strategies
RESULTS
Cost analysis of treatment demonstrates an increased cost of $336 for 13% increased efficacy of surgical management. This analysis was sensitive to the probability of extra office visit, cost of visit, and probability of success. When the surgical arm is divided into outpatient manual vacuum aspiration (MVA) versus inpatient electric vacuum aspiration (EVA), there is increased cost of $745 for EVA, but decreased cost of $202 for MVA, compared with medical management. In general, MVA was found to be more cost-effective than medical management. For treatment of incomplete or inevitable abortion, medical management was found to be less costly and more efficacious. Utilities studies demonstrated that a patient would need to prefer surgery 14% less than medication in order for its treatment efficacy to be outweighed by desire to avoid surgery.
CONCLUSION
Surgical or medical management of early pregnancy failure can be cost effective, depending on the circumstances. Surgery is cost effective and more efficacious when performed in an outpatient setting. For incomplete or inevitable abortion, medical management is cost effective and more efficacious.
INTRODUCTION
Early pregnancy failure is a common occurrence, affecting one-third of early pregnancies (1) and one-fourth of all women (2). Although the traditional treatment option for such pregnancies has been surgical evacuation of the uterus, medical treatment with misoprostol has been gaining popularity as a noninvasive alternative. Both surgical and nonsurgical treatments are currently acceptable in practice (3), but deciding what the best regimen to use in a given clinical scenario is not always clear.
A randomized clinical trial by Zhang demonstrated that misoprostol is an acceptable alternative to vacuum aspiration for the management of early pregnancy failure (4). The success rate of medical management was 84% compared to the 97% success of surgical management, but it is not known which approach is more cost effective. This large multi-center trial incorporated patients with three types of miscarriages (incomplete and inevitable, anembryonic, and fetal or embryonic demise) which were treated by two different surgical methods (manual vacuum aspiration and electric vacuum aspiration). We therefore performed a cost effective analysis of surgical versus medical therapy in the management of early pregnancy failure, looking at the varying surgical treatment options as well as the types of miscarriage in an effort to clarify which subgroups of patients would benefit from medical or surgical management.
MATERIALS AND METHODS
Trial background
The randomized trial was approved by the institutional review boards of the National Institute of Child Health and Human Development, Columbia University, the University of Miami, the University of Pennsylvania, the University of Pittsburgh, and Clinical Trials &Surveys Corp. Patients with anembryonic gestation, embryonic or fetal death, or incomplete or inevitable abortion were enrolled between March 2002 and March 2004 at the four participating institutions. Exclusion criteria included anemia (hemoglobin level below 9.5 g per deciliter), hemodynamic instability, a history of a clotting disorder or anticoagulant use (not including aspirin), allergy to prostaglandins or nonsteroidal anti-inflammatory drugs, and prior surgical or medical abortion that was either self-induced or induced by other physicians during the current pregnancy. Written informed consent was obtained by all subjects. Patients were randomized to medical or surgical management using a centralized, computer-automated telephone response system in a 3:1 ratio. Randomization was stratified according to the study site and the type of pregnancy failure (anembryonic gestation or fetal death vs. incomplete or inevitable spontaneous abortion) using randomly permuted blocks.
Surgical management typically consisted of manual vacuum aspiration (IPAS, Chapel Hill, NC) using local anesthesia or sedation at the discretion of the treatment team) in an outpatient setting at Columbia University and the University of Pittsburgh, and electric vacuum aspiration in an operating room at the University of Miami and the University of Pennsylvania (Synevac Vacuum Aspiration System 10 (Redwood, CA ) using sedation, spinal or general anesthesia at the discretion of the treatment team). The aspiration was performed by a study investigator or by a resident physician who was supervised by an investigator. All women were contacted by telephone on day 8 to inquire about any symptoms, medications, or emergency visits to the hospital after the treatment. Women returned for a follow-up visit on day 15 (range, day 13 to day 18). Medical management consisted of treatment with four 200-μg tablets (800 μg) of misoprostol (Cytotec, Searle) vaginally. These women returned on day 3, and if expulsion was not complete (a gestational sac was still visualized or the endometrial lining was greater than 30 mm on transvaginal ultrasonography), a second 800-μg dose of misoprostol was administered vaginally. On day 8 (range, day 6 to day 10), if the expulsion of products of conception was still not complete, vacuum aspiration was offered. The women returned for a follow-up visit on day 15. At each follow-up visit, transvaginal ultrasonography was performed, and the clinical investigator performed a physical examination, conducted an interview, and collected structured diary pages. In addition, at the day 15 visit, hemoglobin was measured and each woman completed a questionnaire assessing the acceptability of the treatment and the quality of life. A telephone interview was conducted on day 30 (range, day 25 to day 35) to determine whether any woman underwent additional treatment. Women with symptoms potentially related to the study treatment were followed until the symptoms resolved.
The study was designed as a non-inferiority trial given the assumption that medical treatment would not surpass surgical treatment. For medical treatment to be considered a reasonable alternative to surgery, it was decided that medical treatment should be effective 80% of the time, assuming a surgical success rate of 98%. Success was defined as complete uterine evacuation without the need for vacuum aspiration in the medical management group. Treatment failure was defined as the need for vacuum aspiration for the medical management group or a repeated aspiration in the surgical management group within 30 days after initial treatment. Full details of the trial have been published previously.(4)
Data analysis
The cost-effectiveness of medical management in comparison with surgical management was expressed in terms of incremental cost per effectiveness. We conducted a cost effectiveness analysis using decision analysis methodology. Models were constructed and analyzed using Data 3-0 for Windows. Patient characteristics, probabilities of outcome and side effects were taken from those in the randomized controlled trial. The costs that we evaluated included: misoprostol, vacuum aspiration, operating room and anesthesia for the electronic vacuum aspiration and manual vacuum aspiration, office visits, unscheduled visits, ultrasounds, surgery for treatment failure in both arms, and rehospitalizations. All costs were taken from University of Pennsylvania or Medicare cost reports (Supplemental Table 1). Incremental cost effectiveness ratios (based on a modified utility score where failure=0, medication success = 1, and surgical success = 0.95) were calculated for initial treatment and initial treatment with secondary surgery costs in case of failure. Cost, efficacy and incremental cost effectiveness ratios were then recalculated by surgical procedure and miscarriage type. The values of the following variables were varied as part of the sensitivity analyses: (i) cost of scheduled visits (ii) cost of rehospitalization, (iii) probability of rehospitalization, (iv) probability of an extra visit in the medication arm, and (v) likelihood of success in the medication arm without an extra visit. To examine the role of patient preference, a utility analysis was conducted. Cost effectiveness ratios are based on a modified utility score where unsuccessful treatment is defined as 0, medical therapy that successfully treated the miscarriage is defined as 1, and surgical success is defined as 0.95. Expectant management of a miscarriage was not a treatment arm in the parent randomized trial and thus was not assessed in this analysis.
RESULTS
In the trial, of the 491 women assigned to receive misoprostol, 71% had complete expulsion by day 3 and 84% by day 8. Overall, treatment failed in 16% of this group. In the surgical arm, 3% had treatment failure and required a repeat aspiration. The average initial treatment costs per patient for medical and surgical therapy are $415 and $873 respectively, yielding an incremental increase in cost of $459 (110% increase) for surgical therapy. Initial efficacy was 13% better for VA (84% vs. 97%) resulting in a cost effectiveness ratio of $3526 per successful treatment. When the cost of a VA for initial treatment failure was factored (cost of initial treatment and cost of treating those that failed initial therapy, the costs of medical and surgical therapy are $563.4 and $899.4 respectively, yielding an incremental increase in cost of $335 (56.9% increase) for surgical therapy. The cost effectiveness ratio is $2707 per successful treatment (Table 1). Cost for assumptions as to type of surgical procedure (EVA versus MVA) are presented in Table 2. In the surgical arm, 57% were treated with manual vacuum aspiration in an outpatient setting and 43% with electronic vacuum aspiration in an operating room. Sensitivity analysis demonstrates that surgical treatment would be more effective and less expensive if all surgical procedures were performed as outpatients using manual vacuum extraction.
Table 1.
Cost, Efficacy and Incremental Cost Effectiveness Ratios (ICER) for Surgical versus Medical Treatment, by Surgery Type
| Strategy | Cost (USD) | Incremental Cost | Efficacy | Incremental Efficacy | ICER |
|---|---|---|---|---|---|
| All surgery | |||||
| Medication | $563.4 | - | 0.844 | - | |
| Surgery | $899.4 | $335.9 | 0.968 | 0.124 | $2,707 |
|
| |||||
| EVA alone | |||||
| Medication | $563.4 | - | 0.844 | - | |
| Surgery | $1,308.8 | $745.4 | 0.977 | 0.134 | $5,580 |
|
| |||||
| MVA alone | |||||
| Surgery | $361.0 | - | 0.955 | - | |
| Medication | $563.4 | $202.4 | 0.844 | −0.112 | Dominated |
Table 2.
Cost, Efficacy and Incremental Cost Effectiveness Ratios for Surgical versus Medical Treatment, by Miscarriage Type
| Strategy | Cost (USD) | Incremental Cost | Efficacy | Incremental Efficacy | ICER |
|---|---|---|---|---|---|
| Fetal demise group | |||||
| Medication | $511.9 | - | 0.878 | - | |
| Surgery | $957.8 | $445.9 | 0.979 | 0.101 | $4,415 |
|
| |||||
| Anembryonic gestation | |||||
| Medication | $617.6 | - | 0.807 | - | |
| Surgery | $842.1 | $224.4 | 0.962 | $875 | $1,445 |
|
| |||||
| Incomplete gestation | |||||
| Medication | $523.1 | - | 0.933 | - | |
| Surgery | $718.8 | $195.7 | 0.876 | −0.0582 | Dominated |
Table 2 shows the results of examining the three types of failed pregnancies separately. Embryonic or fetal death was diagnosed in 58%, and we found that surgery was still more costly per unit efficacy, with an ICER of $4,415. Anembryonic gestation comprised 36% of patients in the original study, and women with an anembryonic gestation had a lower rate of success in the medical arm than the other groups, and this was reflected in the lower ICER of $1445 for this group. In the incomplete or inevitable abortion group, which comprised 6% of the initial study population, medical treatment was more efficacious than surgery, and given its increased efficacy and decreased cost, the ICER was dominated.
We then performed sensitivity analysis, examining the incremental cost per unit efficacy over feasible ranges for multiple variables. One way sensitivity analysis demonstrates that the incremental cost per efficacy is not responsive to the cost of a scheduled visit (over the range of $50 to $200), the cost of rehospitalization (over the range of USD$2000–6000), or probability of rehospitalization (over the range of 0–0.2) However, if the probability of having an extra visit on the medication arm rises above 0.815, surgery is less expensive (Graph 1). Two-way sensitivity analysis examining the likelihood of success in the medical arm without a second visit and the cost of a scheduled visit demonstrates that surgery can be favorable (both less costly and more efficacious) only as medical treatment becomes less efficacious and the cost of scheduled visits are higher (Graph 2).
Graph 1.
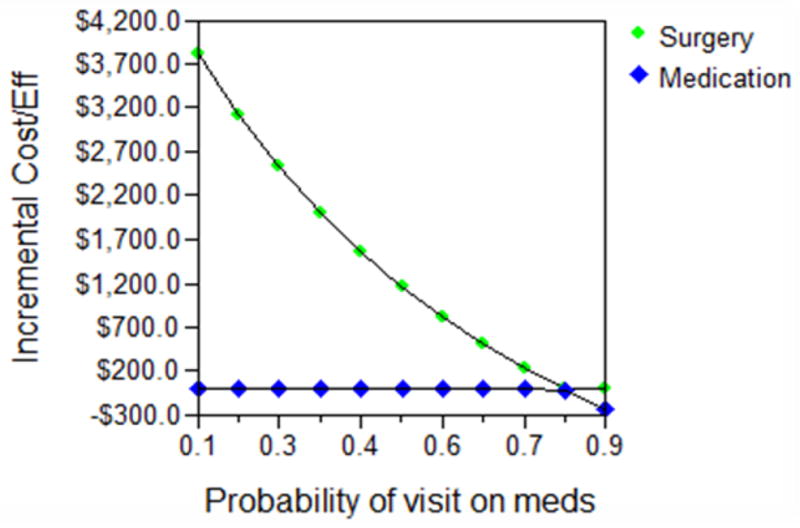
One-way sensitivity analysis
Graph 2.
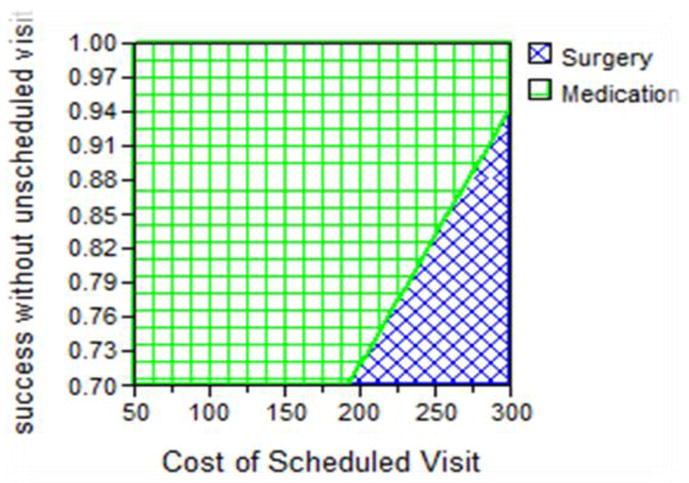
Two-way sensitivity analysis
One way of taking patient preference into account in the cost effectiveness of a medical procedure is to use a utility analysis. The latter demonstrates that medication becomes more effective and less costly if surgery is preferred 14% less then medication (ICER is dominated at 0.86 on a scale of 0 – 1).
DISCUSSION
This study demonstrates that overall, medical therapy is a cost-effective treatment of early pregnancy loss. However, there are situations when surgical management is both more effective and less costly than medical management. Surgery can become more efficacious and less costly if a) surgical treatment is done in an outpatient setting (without general anesthesia), b) the probability of medically treated women needing extra visits is high or c) the cost of outpatient visit is high and success of medical management is low. Conversely, medical management becomes both less costly and more efficacious in the case of incomplete or inevitable abortions as well as when a patient’s desire to avoid surgery is high.
Evaluating the type of surgical procedure, manual vacuum aspiration and electric vacuum aspiration, separately shows a distinction in terms of cost which then translates into its cost efficacy. MVA, given that it is an outpatient procedure which does not require an operating room, has clear savings in terms of cost and time over EVA, with no appreciable change in efficacy (5, 6). Office-based surgical management of early pregnancy failure not only offers cost savings over operating room management, but with similar patient satisfaction without increased complication rates (7). Data from our own randomized trial indicate that although pain severity scores were better in the EVA group, the MVA group had better physical and emotional role functioning scores and fewer patients undergoing MVA missed work or required help at home (8). In another model with estimated outcomes from the literature, MVA was also found to be a more cost-effective strategy than medical management (9). Our present study confirms the conclusions that MVA is more cost-effective than medical management, but has the advantages of using estimated patient cost and efficacy from a randomized trial in the United States. Currently, MVA is not universally available in outpatient settings treating women with early pregnancy failure, but this study provides further evidence that it would be a manner of increasing efficacy of miscarriage treatment over medical management without needing to sacrifice time and money associated with sending a patient to the operating room.
We also found that the type of miscarriage affected the incremental cost-efficacy ratio. Stratifying the type of miscarriage into embryonic or fetal death, anembryonic gestation and incomplete or inevitable abortion, medical therapy in the incomplete or inevitable abortion group is both less costly and more effective with a dominated ICER. The failure rates for the three miscarriage types in the study were 19% for anembryonic gestation, 12% for embryonic or fetal demise and 7% for incomplete or inevitable abortion. Pooled data of medical versus surgical treatment of incomplete miscarriage shows that surgical management had 1.5 times the chance of success over medical management (10). However, the regimens as well as efficacy of medical management for treating incomplete abortion in these studies varied greatly, from 13% success with a single dose of 400μg of misoprostol orally (11) to 95% success with 200μg of misoprostol four times daily (orally) after 200μg of misoprostol intravaginally for 5 days (12). Other studies comparing incomplete to missed abortions found lower failure rates for the incomplete abortion group (0–7.1%) than for the missed abortions (13.3–23.1%) with varying misoprostol regimens (13–15). The results presented here demonstrate that for treatment of the incomplete or inevitable miscarriage subtype, not only is medical management more efficacious than for the other miscarriage subtypes, but when cost is factored in, medical management becomes both more efficacious and less costly than surgical management. While costs form one intuitions were used in the study, unless the relative cost of procedures and medication are dramatically different at other institutions, these findings should be valid externally.
Women’s preferences and experiences with medical treatment vary, and are difficult to quantitate. However, an individual woman’s choice should be taken into account when there are safe efficacious alternatives. This study supports the notion that if a person’s desire for one intervention is high over another (for instance, medical versus surgery) it can affect an incremental cost-effectiveness ratio. In the current analysis, women would need to prefer surgical management 14% less than medical management for medical therapy to become relatively more efficacious and less costly. Quality of life questionnaires from the current study indicated that although misoprostol treatment was associated with greater pain and lower acceptability of treatment-related symptoms, treatment acceptability and quality of life were similar for both medical and surgical treatment (4). Other investigation into the acceptability of misoprostol for the treatment of miscarriage suggest that the majority of women would recommend and choose their type of treatment again, but the percentage of women who reported high acceptability of medical who recommend it significantly decreased if the procedure was unsuccessful (16–18). One study reported that women preferred misoprostol treatment over surgical evacuation as long as the success rate with medical therapy exceeds 65%, stating the desire to avoid surgery or for a more natural process most commonly (17).
Other studies have demonstrated an economic advantage of medical management over the traditional surgical management (19–21), but direct comparisons are limited due to varied management strategies, definitions of outcome measures and assignment of cost. The estimates in the analysis in You et al. were based on pooled data from the literature (20), and those from Petrou et al and Graziosi et al were from a study of women in southern England and the Netherlands, respectively (19, 21). In the British study, the primary endpoint was complete evacuation, and women with incomplete miscarriage were excluded. The medical therapy was 800μg misoprostol vaginally, repeated in 24 hours if needed, whereas the surgical management consisted of all suction curettages with general anesthesia. (21) In the Dutch study, the primary effectiveness outcome was cost per gynecologic infection prevented. Women in the surgical arm all received surgical suction curettage with general anesthesia and those in the medical arm were admitted to the hospital (22). Moreover in this study, treatment varied by miscarriage type; those with incomplete miscarriages were treated with 800μg misoprostol whereas missed abortions were treated with a combination of mifepristone and misoprostol (22). Our data using a United States based population, confirm some these previous findings while demonstrating that medical management with misoprostol was more cost-effective compared to surgically-based therapy (comprised of manual vacuum aspiration and electric vacuum aspiration) as a whole, but further demonstrate a cost-savings if only MVA is performed. Of note, rare but serious adverse events such as intrauterine adhesions were not factored into this analysis as no such cases were noted in our large clinical trial. This study did not evaluate the cost effectiveness of expectant management.
The strengths of this study include the use of a large, multicenter randomized trial, with data on varying types of miscarriages and both available surgical interventions for treatment of early pregnancy failure. Patients were randomized to vaginal misoprostol or surgical management and thus expectant management or other types of medical management (such as mifepristone or alternative regimens of misoprostol), or the effect of patient choice could not be evaluated in this study. Further, although our utilities studies demonstrate a point at which patient preference would affect the cost-effectiveness ratio, we do not have the data necessary to determine how this utility can be translated back to inform clinical practice. Finally, generalizability of this study is limited to a United States population given the differences in health care systems and cost throughout the world, and even within the United States, MVA is not universally available for use in outpatient settings.
In conclusion, this study demonstrates that although surgery is the more efficacious and more costly treatment of first trimester pregnancy failure, this is not always the case. If surgical treatment is done in an outpatient setting without incurring the additional operation room and anesthesia costs, surgical treatment with manual vacuum aspiration is less costly as well as more efficacious than medical management. Finally, there are certain situations when medical management should be considered over surgical management, such as when a patient desires to avoid surgery or has an incomplete or inevitable abortion.
Supplementary Material
Acknowledgments
This project has been funded by the National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services under Contract Numbers: N01-HD-1-3321 through 3325 with additional support from R01-HD036455 (KB), K24HD060687 (KB) and T32-HD007440 (MR).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mary Rausch, North Shore University Hospital, Manhasset, NY.
Scott Lorch, The Children’s Hospital of Philadelphia, Philadelphia, PA.
Karine Chung, University of Southern California. Los Angeles, CA.
Margaret Frederick, Clinical Trials & Surveys Corp., Owings Mills, MD.
Jun Zhang, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD.
Kurt Barnhart, University of Pennsylvania Medical Center, Philadelphia, PA.
References
- 1.Wilcox AJ, Weinberg CR, O’Connor JF, Baird DD, Schlatterer JP, Canfield RE, et al. Incidence of early loss of pregnancy. N Engl J Med. 1988;319(4):189–94. doi: 10.1056/NEJM198807283190401. [DOI] [PubMed] [Google Scholar]
- 2.Warburton D, Fraser FC. Spontaneous Abortion Risks in Man: Data from Reproductive Histories Collected in a Medical Genetics Unit. Am J Hum Genet. 1964;16:1–25. [PMC free article] [PubMed] [Google Scholar]
- 3.Chen BA, Creinin MD. Medical management of early pregnancy failure: efficacy. Semin Reprod Med. 2008;26(5):411–22. doi: 10.1055/s-0028-1087107. [DOI] [PubMed] [Google Scholar]
- 4.Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761–9. doi: 10.1056/NEJMoa044064. [DOI] [PubMed] [Google Scholar]
- 5.Blumenthal PD, Remsburg RE. A time and cost analysis of the management of incomplete abortion with manual vacuum aspiration. Int J Gynaecol Obstet. 1994;45(3):261–7. doi: 10.1016/0020-7292(94)90252-6. [DOI] [PubMed] [Google Scholar]
- 6.Koontz SL, Molina de Perez O, Leon K, Foster-Rosales A. Treating incomplete abortion in El Salvador: cost savings with manual vacuum aspiration. Contraception. 2003;68(5):345–51. doi: 10.1016/s0010-7824(03)00162-8. [DOI] [PubMed] [Google Scholar]
- 7.Dalton VK, Harris L, Weisman CS, Guire K, Castleman L, Lebovic D. Patient preferences, satisfaction, and resource use in office evacuation of early pregnancy failure. Obstet Gynecol. 2006;108(1):103–10. doi: 10.1097/01.AOG.0000223206.64144.68. [DOI] [PubMed] [Google Scholar]
- 8.Edwards S, Tureck R, Fredrick M, Huang X, Zhang J, Barnhart K. Patient acceptability of manual versus electric vacuum aspiration for early pregnancy loss. J Womens Health. 2007;16(10):1429–36. doi: 10.1089/jwh.2007.0362. [DOI] [PubMed] [Google Scholar]
- 9.Rocconi RP, Chiang S, Richter HE, Straughn JM., Jr Management strategies for abnormal early pregnancy: a cost-effectiveness analysis. J Reprod Med. 2005;50(7):486–90. [PubMed] [Google Scholar]
- 10.Sotiriadis A, Makrydimas G, Papatheodorou S, Ioannidis JP. Expectant, medical, or surgical management of first-trimester miscarriage: a meta-analysis. Obstet Gynecol. 2005;105(5 Pt 1):1104–13. doi: 10.1097/01.AOG.0000158857.44046.a4. [DOI] [PubMed] [Google Scholar]
- 11.de Jonge ET, Makin JD, Manefeldt E, De Wet GH, Pattinson RC. Randomised clinical trial of medical evacuation and surgical curettage for incomplete miscarriage. BMJ. 1995;311(7006):662. doi: 10.1136/bmj.311.7006.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sahin HG, Sahin HA, Kocer M. Randomized outpatient clinical trial of medical evacuation and surgical curettage in incomplete miscarriage. Eur J Contracept Reprod Health Care. 2001;6(3):141–4. [PubMed] [Google Scholar]
- 13.Bagratee JS, Khullar V, Regan L, Moodley J, Kagoro H. A randomized controlled trial comparing medical and expectant management of first trimester miscarriage. Hum Reprod. 2004;19(2):266–71. doi: 10.1093/humrep/deh049. [DOI] [PubMed] [Google Scholar]
- 14.Demetroulis C, Saridogan E, Kunde D, Naftalin AA. A prospective randomized control trial comparing medical and surgical treatment for early pregnancy failure. Hum Reprod. 2001;16(2):365–9. doi: 10.1093/humrep/16.2.365. [DOI] [PubMed] [Google Scholar]
- 15.Ngai SW, Chan YM, Tang OS, Ho PC. Vaginal misoprostol as medical treatment for first trimester spontaneous miscarriage. Hum Reprod. 2001;16(7):1493–6. doi: 10.1093/humrep/16.7.1493. [DOI] [PubMed] [Google Scholar]
- 16.Harwood B, Nansel T. Quality of life and acceptability of medical versus surgical management of early pregnancy failure. BJOG. 2008;115(4):501–8. doi: 10.1111/j.1471-0528.2007.01632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graziosi GC, Bruinse HW, Reuwer PJ, Mol BW. Women’s preferences for misoprostol in case of early pregnancy failure. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):184–6. doi: 10.1016/j.ejogrb.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Graziosi GC, Bruinse HW, Reuwer PJ, van Kessel PH, Westerweel PE, Mol BW. Misoprostol versus curettage in women with early pregnancy failure: impact on women’s health-related quality of life. A randomized controlled trial. Hum Reprod. 2005;20(8):2340–7. doi: 10.1093/humrep/dei019. [DOI] [PubMed] [Google Scholar]
- 19.Petrou S, Trinder J, Brocklehurst P, Smith L. Economic evaluation of alternative management methods of first-trimester miscarriage based on results from the MIST trial. BJOG. 2006;113(8):879–89. doi: 10.1111/j.1471-0528.2006.00998.x. [DOI] [PubMed] [Google Scholar]
- 20.You JH, Chung TK. Expectant, medical or surgical treatment for spontaneous abortion in first trimester of pregnancy: a cost analysis. Hum Reprod. 2005;20(10):2873–8. doi: 10.1093/humrep/dei163. [DOI] [PubMed] [Google Scholar]
- 21.Graziosi GC, van der Steeg JW, Reuwer PH, Drogtrop AP, Bruinse HW, Mol BW. Economic evaluation of misoprostol in the treatment of early pregnancy failure compared to curettage after an expectant management. Hum Reprod. 2005;20(4):1067–71. doi: 10.1093/humrep/deh709. [DOI] [PubMed] [Google Scholar]
- 22.Trinder J, Brocklehurst P, Porter R, Read M, Vyas S, Smith L. Management of miscarriage: expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial) BMJ. 2006;332(7552):1235–40. doi: 10.1136/bmj.38828.593125.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


