Abstract
Blue dyes such as Patent Blue V (PBV) have been used in medical procedures for decades, and in the United Kingdom they are routinely utilised in sentinel lymph node biopsy (SLNB) for staging the axilla in early breast cancer. However, it has long been recognised that such dyes are associated with anaphylaxis. It has recently been estimated in a prospective study that allergy to PBV occurs with a frequency of 0.9%. Since repeated SLNB (and therefore further exposure to PBV) is increasingly being advocated for the small proportion of patients who develop a local (in-breast) recurrence, and because anaphylaxis can be life-threatening, it is important that those individuals that are allergic to PBV are recognised on their first medical exposure. The measurement of serum mast-cell tryptase (MCT) and skin prick test (SPT) are used in the investigation of suspected anaphylaxis because positive results are supportive of type-1 mediated hypersensitivity. Here we report the clinical features, MCT results and SPT results that pertain to a series of four patients referred to our drug allergy clinic with suspected anaphylaxis following SLNB. We recommend that all patients that show clinical evidence of allergy following exposure to PBV are referred to a specialist drug allergy service for further evaluation to investigate the cause.
Keywords: Anaphylaxis, Tryptase, Skin prick test, Blue dye, Lymph-node biopsy
INTRODUCTION
Blue dyes, such as Patent Blue V (PBV), have been used in medical procedures worldwide for decades. In the UK, National Institute of Clinical Excellence guidelines recommend that sentinel lymph node biopsy (SLNB) is the preferred method for staging the axilla in early breast cancer and this should be performed using the combined localization technique of blue dye and radioactive tracer [1]. Reports of the association of blue dyes with anaphylaxis date since 1960s [2, 3]. The frequency of allergic reactions to PBV was recently reported as 0.9% in the 7,917 UK patients enrolled in NEW START and ALMANAC (ALMANAC was a multicentre randomised study that compared axillary lymphatic mapping against nodal axillary clearance and NEW START was a UK-wide sentinel node biopsy training programme) [4]. This figure is similar to the frequency estimates in older, smaller studies [5-8].
Allergy to PBV has been attributed to type-I hypersensitivity because the reactions occur in the right time frame, subjects with an appropriate clinical history show a positive result on skin testing and the presence of a specific IgE to PBV has been demonstrated in a patient with a relevant history [5, 8-10]. It has been proposed that PBV acts as a hapten that binds to an unidentified carrier protein [11]. Since these reactions can arise on the first medical exposure, it is thought that sensitisation occurs as a result of exposure to blue dyes used in food, textiles and cosmetics [9, 10, 12].
In the course of general anaesthesia there are many potential causes for bronchospasm, hypotension, angioedema and urticaria, which may be allergic or non-allergic. Recognising allergic reactions caused by PBV can be particularly difficult because there is frequently not a clear temporal association between administering the drug and the onset of symptoms [13]. The Association of Anaesthetists of Great Britain and Ireland (AAGBI) guidelines state that anaphylaxis arising during anaesthesia should be managed with 50 µg intravenous (IV) boluses of adrenaline given as quickly as possible and appropriate volumes of 0.9% saline or Ringer's solution used to maintain blood pressure [14]. It is recommended that once the patient has been stabilised 10 mg of IV chlorpheniramine and 200 mg of IV hydrocortisone are administered. If blood pressure cannot be maintained on an adrenaline infusion an alternative vasopressor such as metaraminol is considered, depending on the experience of the anaesthetist. Blood samples should be taken for mast cell tryptase (MCT) as close to the event as practical, at 1-2 h and at baseline (24 h or more after the event). If anaphylaxis during anaesthesia is suspected, it is the anaesthetist's responsibility to refer the patient to an allergy centre for investigation.
Anaphylactic reactions may be allergic (mediated by an immune mechanism) or non-allergic (previously called anaphylactoid). If the reaction is caused by type-1 hypersensitivity (i.e. it is IgE mediated), skin prick test (SPT) can be used to identify the causal drug. Recently a diagnostic protocol for investigating suspected allergic reactions to PBV by skin testing has been proposed [15]. Detecting a rise in serum MCT is helpful because it is indicative of mast cell degranulation and supports a diagnosis of drug allergy. Here we report the clinical features, MCT results and SPT results that pertain to a series of four patients referred to our drug allergy clinic (DAC) with suspected anaphylaxis following SLNB.
CASE REPORTS
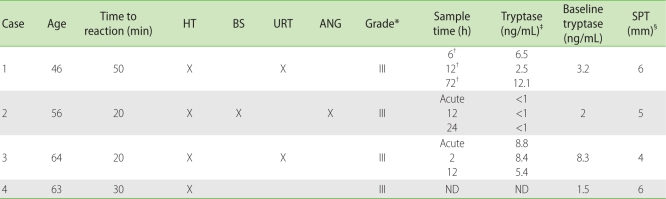
The patients were identified during an anaesthetic audit of critical incidents after they showed clinical evidence of immediate hypersensitivity during SLNB, from which they had all made a full recovery (Table 1). In accordance with the AAGBI guidelines the patients were referred for drug-allergy testing [14]. None had a known history of prior medical exposure to PBV. In the drug-allergy clinic SPT were performed in duplicate using a panel consisting of a positive control (histamine chloride, 10 mg/mL), a negative control (normal saline) and appropriate dilutions of all the other drugs to which they had been exposed (in each case hypnotics, muscle relaxants and opioids). PBV was used at vial concentration (25 mg/mL), which has previously been shown to be non-irritating [5, 13, 14]. A SPT result that was at least 3 mm greater than the negative control was considered positive. None of the patients showed any evidence of dermatographism with the negative control.
Table 1.
Clinical characteristics and clinical features of allergic reactions to PBV in all four patients and their tryptase and SPT results
PBV, Patent Blue V; SPT, skin prick test; HT, hypotension; BS, bronchospasm; URT, urticaria; ANG, angioedema; ND, not done. *Reactions were graded from I to IV using the criteria described by Barthelmes et al. [4]: grade I (urticaria, blue hives, pruritis or generalised rash); grade II (transient hypotension, bronchospasm or laryngospasm); grade III (severe hypotension requiring vasopressor support and/or change/abandoning of planned procedure and/or high dependency unit/intensive therapy unit admission); grade IV (cardiorespiratory arrest and/or death). †Timing of samples uncertain - 3 samples were received by the laboratory and the following results were recorded: day 1 (6 h post reaction), 6.5 µg/L; day 2 (18 h post reaction), 2.5 µg/L; day 4 (72 h post reaction), 12.1 µg/L. It is suspected there was a mix up in labelling the samples. ‡Serum MCT was measured by fluorescent immunoassay (Immunocap, Phadia, normal range 2-14 ng/mL). Levels above 14 ng/mL or increased by a factor of three or more from baseline were considered increased. §A SPT result that was at least 3 mm greater than the negative control was considered positive.
Case 1
Fifty min after blue dye was administered a 46-year-old woman developed an urticarial rash at the operative site and dropped her systolic BP to 70 mmHg - this responded rapidly to treatment with adrenaline IV boluses (total 50 µg). Peak MCT measured within the 72 h following her reaction was 12.1 ng/mL (baseline was 3.2, Table 1). In the DAC a 6 mm positive reaction was recorded on SPT with PBV in the context of a negative reaction to all the other drugs used and the negative control. She had no previous history of allergy or atopy.
Case 2
Twenty min after the administration of PBV a 56-year-old woman showed a drop in her systolic blood pressure to 70 mmHg and lung compliance was noted to reduce. She developed laryngeal oedema. Sustained improved blood pressure and ventilation pressures were achieved after 1 h following the administration of chlorpheniramine, hydrocortisone, 5 mg of nebulised salbutamol, two litres of fluid and three 0.5 mg boluses of metaraminol. She was transferred to ICU from theatre, without the need for ongoing inotrophic support, and extubated the next day. Serial MCT showed no rise (Table 1). SPT a month later showed a positive response to PBV (5 mm) and negative response to all the other drugs tested. She reported a history of mild hay fever in the tree pollen season, but this was well controlled and was not investigated with SPT.
Case 3
A 64-year-old woman developed hypotension and discrete areas of angioedema and wheals that stained blue with the dye shortly after PBV was administered. The intended surgery was abandoned. MCT taken at the time of the reaction was found to be 8.8, and was 8.4 and 5.4 ng/mL 2 h later and at baseline. Two months later on SPT she developed positive response (4 mm) to PBV only. She had no history of atopy but complained of nasal congestion and dizziness after eating food containing wheat. She did not show a reaction to wheat on SPT and had not consumed it on the day of her surgery.
Case 4
Thirty min after the administration of PBV a 63-year-old lady showed a drop in her systolic blood pressure to 65 mmHg. There was no cutaneous involvement and no laryngeal oedema or bronchospasm were reported. Sustained improvement was achieved with the administration of three 3 mg boluses of ephedrine, 200 mg of hydrocortisone, 10 mg of chlorpheniramine, one litre of crystalloid and 500 mL of colloid over a period of 30 min. When seen in the DAC 6 weeks later, she showed a 6 mm positive response on SPT with PBV; her response to all other drugs tested was negative. She had a history of mild asthma and allergy/intolerance to ibuprofen (wheeze occurring within 2 h of ingestion on two occasions without any other associated features).
DISCUSSION
All of the cases described here had clinical histories consistent with anaphylaxis, showed positive SPT tests to PBV, and did not show a reaction with any of the other drugs used. Although the negative predictive value for SPT with any drug is not 100% (and therefore there is a chance that one of the other drugs administered concurrently caused the reaction), it is known that only a small proportion of control individuals show a positive reaction to PBV on skin testing (15/566 (2.6%) in the study by Kalimo et al. [5]), suggesting that false positives to PBV are quite rare. Therefore, on the balance of probabilities PBV is the most likely causal agent for the anaphylactic reaction in each case.
In common with the previously published case series, also derived from patients attending DACs, our patients showed relatively severe (grade III) reactions. This is in contrast to the observed rates in NEW START/ALMANAC where the milder grade I and II reactions were more common than the severe grade III reactions (grade I had a frequency of 0.3%, grade II 0.2%, grade III 0.06% and grade IV 0%). Given that allergy to PBV was a prospectively collected, predefined data point in NEW START/ALMANAC, the quoted rates of allergy are likely to be accurate. While these numbers are too small to draw any firm conclusions, it is possible that this discrepancy represents a referral bias, with the less severe reactions not being referred for drug-allergy testing. This is of concern because repeated SLNB (and therefore further exposure to PBV) is increasingly being advocated for the small proportion of patients who develop a local (in-breast) recurrence. There are several reports in the literature of individuals who have had more than one reaction to PBV, the first one not having been recognised or correctly attributed to the dye [8, 12, 13, 16].
In our series of four patients, none showed a MCT peak that was above the upper limit of normal although one showed a greater than 3-fold increase. This in keeping with a recent study which reports the sensitivity of MCT measurement following anaphylaxis to PBV is just 0.54 [17].
In summary, in common with the other published case series, we found that the majority of patients referred with suspected PBV allergy seen in our DAC had experienced relatively severe reactions. A rise in MCT is of limited sensitivity in identifying patients who show evidence of type-1 hypersensitivity to PBV and we recommend that whenever there is a clinical suspicion of anaphylaxis associated with PBV the patient is referred to specialist drug allergy services for further assessment.
References
- 1.National Institute for Health and Clinical Excellence. Early and locally advanced breast cancer: diagnosis and treatment. Available from: http://www.nice.org.uk/nicemedia/pdf/CG80NICEGuideline.pdf.
- 2.Kopp WL. Anaphylaxis from alphazurine 2G during lymphography. JAMA. 1966;198:668–669. [PubMed] [Google Scholar]
- 3.Sinclair DJ, Perera FA. Allergic reactions: following patent blue dye injection. Can Med Assoc J. 1969;101:100–101. [PubMed] [Google Scholar]
- 4.Barthelmes L, Goyal A, Newcombe RG, McNeill F, Mansel RE. Adverse reactions to patent blue V dye - The NEW START and ALMANAC experience. Eur J Surg Oncol. 2010;36:399–403. doi: 10.1016/j.ejso.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Kalimo K, Jansén CT, Kormano M. Sensitivity to Patent Blue dye during skin-prick testing and lymphography. A retrospective and prospective study. Radiology. 1981;141:365–367. doi: 10.1148/radiology.141.2.7291558. [DOI] [PubMed] [Google Scholar]
- 6.Beenen E, de Roy van Zuidewijn DB. Patients blue on patent blue: an adverse reaction during four sentinel node procedures. Surg Oncol. 2005;14:151–154. doi: 10.1016/j.suronc.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Mansouri R, Chicken DW, Keshtgar MR. Allergic reactions to patent blue dye. Surg Oncol. 2006;15:58. doi: 10.1016/j.suronc.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Keller B, Yawalkar N, Pichler C, Braathen LR, Hunger RE. Hypersensitivity reaction against patent blue during sentinel lymph node removal in three melanoma patients. Am J Surg. 2007;193:122–124. doi: 10.1016/j.amjsurg.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Forschner K, Kleine-Tebbe A, Zuberbier T, Worm M. Type I sensitization towards patent blue as a cause of anaphylaxis. Allergy. 2003;58:457–458. doi: 10.1034/j.1398-9995.2003.00131.x. [DOI] [PubMed] [Google Scholar]
- 10.Wöhrl S, Focke M, Hinterhuber G, Stingl G, Binder M. Near-fatal anaphylaxis to patent blue V. Br J Dermatol. 2004;150:1037–1038. doi: 10.1111/j.1365-2133.2004.05931.x. [DOI] [PubMed] [Google Scholar]
- 11.Johansson SG, Nopp A, Oman H, Stahl-Skov P, Hunting AS, Guttormsen AB. Anaphylaxis to Patent Blue V. II. A unique IgE-mediated reaction. Allergy. 2010;65:124–129. doi: 10.1111/j.1398-9995.2009.02191.x. [DOI] [PubMed] [Google Scholar]
- 12.Woltsche-Kahr I, Komericki P, Kränke B, Brabek E, Horn M, Schuller-Petrovic S, Richtig E, Aberer W. Anaphylactic shock following peritumoral injection of patent blue in sentinel lymph node biopsy procedure. Eur J Surg Oncol. 2000;26:313–314. doi: 10.1053/ejso.1999.0888. [DOI] [PubMed] [Google Scholar]
- 13.Mertes PM, Malinovsky JM, Mouton-Faivre C, Bonnet-Boyer MC, Benhaijoub A, Lavaud F, Valfrey J, O'Brien J, Pirat P, Lalourcey L, Demoly P. Anaphylaxis to dyes during the perioperative period: reports of 14 clinical cases. J Allergy Clin Immunol. 2008;122:348–352. doi: 10.1016/j.jaci.2008.04.040. [DOI] [PubMed] [Google Scholar]
- 14.Harper NJ, Dixon T, Dugué P, Edgar DM, Fay A, Gooi HC, Herriot R, Hopkins P, Hunter JM, Mirakian R, Pumphrey RS, Seneviratne SL, Walls AF, Williams P, Wildsmith JA, Wood P, Nasser AS, Powell RK, Mirakhur R, Soar J. Suspected anaphylactic reactions associated with anaesthesia. Anaesthesia. 2009;64:199–211. doi: 10.1111/j.1365-2044.2008.05733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haque RA, Wagner A, Whisken JA, Nasser SM, Ewan PW. Anaphylaxis to patent blue V: a case series and proposed diagnostic protocol. Allergy. 2010;65:396–400. doi: 10.1111/j.1398-9995.2009.02248.x. [DOI] [PubMed] [Google Scholar]
- 16.Hunting AS, Nopp A, Johansson SG, Andersen F, Wilhelmsen V, Guttormsen AB. Anaphylaxis to Patent Blue V. I. Clinical aspects. Allergy. 2010;65:117–123. doi: 10.1111/j.1398-9995.2009.02192.x. [DOI] [PubMed] [Google Scholar]
- 17.Barthelmes L, Goyal A, Sudheer P, Mansel RE. Investigation of anaphylactic reaction after patent blue V dye injection. Breast. 2010;19:516–520. doi: 10.1016/j.breast.2010.05.016. [DOI] [PubMed] [Google Scholar]