Abstract
Objectives
The main objective of this study is to ensure all patients undergone kidney transplantation receives appropriate standard PCP prophylaxis soon after transplantation, unless contraindicated.
Methods
A prospective study included all kidney transplantation recipients from January 2008 to August 2008. A data collection sheet was designed and reviewed in focus group meetings and modified accordingly. The subjects were followed-up during the admission for transplantation to the date of discharge. The discharge prescriptions were screened to ensure all the kidney transplantation recipients were prescribed appropriate PCP prophylaxis before discharge. All prescriptions with NO PCP prophylaxis were intervened by the clinical pharmacist. The focus group meetings suggested designing a questionnaire using likerts scale. The purpose was to highlight doctors’ perception towards PCP prophylaxis for renal transplant recipients. The questionnaires were distributed to all the nephrology doctors (consultants, senior specialists and medical officers). The data were entered in the data collection sheet and were analyzed by using simple statistical methods.
Results
Almost 80% of the prescriptions did not included (TMP/SMX) for PCP among which 20% of the prescriptions were for patients with G6PD deficiency. The clinical pharmacist’s interventions resulted that all discharge prescriptions were modified and (TMP/SMX) was prescribed for patients who were legible for a PCP prophylaxis
Conclusion
In the absence of prophylaxis, the incidence of PCP in solid organ transplant recipients ranges from 6.8% to 22%, necessitating PCP prophylaxis for at least 6 months following transplantation. Despite the widespread knowledge on PCP prophylaxis, most of the patients were discharged with no prophylactic treatment for PCP. After pharmacist’s intervention the prescriptions were edited and PCP prophylaxis was added.
Introduction
Opportunistic infections (pneumocystic carnii/jiroveci, toxoplasmosis) remain the most common life-threatening infection among immnuocompromised patients such as HIV patients and patients underwent solid organ transplantations.1 Trimethoprim-sulfamethoxazole (TMP/SMX) is highly effective in preventing pneumocystic carnii pneumonia (PCP) and is the preferred agent for chemoprophylaxis in kidney transplant recipients.2 In addition, TMP/SMX may also be effective against bacterial infections and toxoplasmosis.2 The standard regimen for PCP prophylaxis in our centre is (TMP/SMX) 480 mg once daily or 960 mg thrice a week for 6 months post transplant. Prophylactic therapy with (TMP/SMX) should be prescribed soon after the kidney transplantation for a period of not less than 6 months.3
Prior to initiation of PCP prophylaxis there are several pharmaceutical care issues to be ackled by the clinical pharmacist to make sure all transplant patients received individualized suitable medication. The aim of this study is to highlight those issues and ensure all legible kidney transplant recipients receive appropriate PCP prophylaxis.
Objectives
The main objective of this study is to ensure all patients undergone kidney transplantation receives appropriate standard PCP prophylaxis soon after transplantation, unless contraindicated.
Study Design
• Prospective, single, cohort study
• Tertiary referral hospital (capacity of 700 beds)
• Inclusion criteria (all adult patients underwent kidney transplantation from January 2008 to August 2008)
• Exclusion criteria (paediatrics and patients with kidney transplantation on dates other then those in inclusion criteria)
Methods
• A prospective study included all kidney transplantation recipients (n=16) from January 2008 to August 2008.
• A data collection sheet including patients demographics and discharge prescription details was designed by the author and validated by focus group (consisted of 3 clinical pharmacists) and the final version of the form was modified consequently.
• The subjects were followed-up during the admission for transplantation to the date of discharge by the renal clinical pharmacist.
• The discharge prescriptions were screened to ensure all the kidney transplantation recipients were prescribed appropriate PCP prophylaxis before discharge.
• All prescriptions with NO PCP prophylaxis were intervened by the renal clinical pharmacist to ensure the prescriptions are modified and a standard PCP prophylaxis is prescribed, unless contraindicated.
• The data collected (demographics, medical history, drug history, updated laboratory results, and discharge details) were entered in the designed form, then were evaluated for completeness and analyzed by using Microsoft excel program 2003 version.
• As an outcome of the results, the focus group also suggested to design a self assessment questionnaire using 5-points likerts scale (strongly agree to strongly disagree).
• The purpose of the questionnaire was to highlight doctors' perception towards PCP prophylaxis for renal transplant recipients. The questionnaires were distributed to all the nephrology doctors (consultants, senior specialists and medical officers) and the completed questionnaires were assessed and analyzed.
The results were discussed with the focus group and it was decided to come up with recommendations to improve the practice and ensure that all eligible patients MUST receive standard PCP prophylaxis soon after the transplantation for 6 months.
Results
During the study period (January 2008-August 2008) 16 End Stage Renal Disease (ESRD) patients received kidney transplantation; most of them received live related kidney donor transplantation at the Royal hospital while 12.5% recipients were transplanted commercially abroad, one in china and the other one in Iran.
Demographic data of the patients are shown in the Table 1.
Table 1. Patients Demographic data.
| n=16 | % | |
|---|---|---|
| Sex | ||
| Male Female |
6 10 |
37.5 62.5 |
| Age | ||
| Mean (±SD) Max (Min) |
37.25 54 (14) |
|
| Type of transplant | ||
| Living related Commercial |
14 2 |
87.5 12.5 |
| Immunosuppressant regimen | ||
| Cyclosporin based Tacrolimus based |
1 15 |
93.75 6.25 |
SD: Standard Deviation
The average stay post transplant was 22.5 days per patient (maximum of 53 days and minimum of 9 days). Most of the patients had their renal function back within normal reference range (CrCl was estimated using the MDRD equation), 62.5% had a creatinine clearance >60 ml/min/1.73 m2.
All the patients had their discharge prescriptions reviewed by the clinical pharmacist upon discharge. TMP-SMX was the standard drug used for PCP prophylaxis in our setting. The results showed that 11 (69%) of the prescriptions did not included a PCP prophylaxis, while 5 (31%) included a standard PCP prophylaxis (TMP-SMX 480mg once a day). Among the 11 prescriptions with no PCP prophylaxis, 2 (19%) patients were G6PD deficient and where not eligible for the standard therapy, while the other 9 (81%) prescriptions were modified after pharmacists intervention and PCP prophylaxis was added to the prescriptions accordingly.
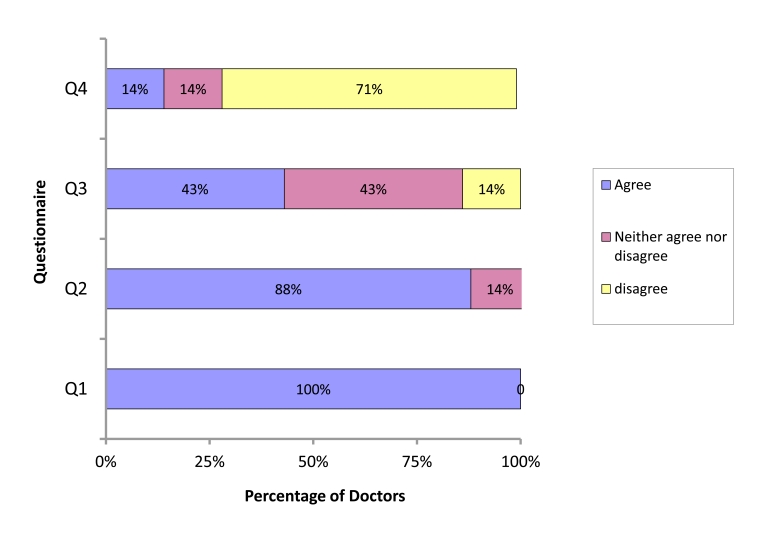
Out of 9 doctors, who were given the questionnaire, only 7 (78%) of the doctors responded and the other 2 (22%) did not respond because they were on leave at the time of submission. Almost 100% of the doctors agreed that PCP prophylaxis is of significant importance for patients recently underwent kidney transplantation. About 43% were not sure whether or not an alternative is required when the patient is ineligible for the standard therapy. The results of the questionnaire are listed in (Figure 1).
Figure 1.
Doctors perception towards PCP prophylaxis
Key: Q1=PCP prophylaxis is of significant importance for patients recently underwent kidney transplantation
Q2= All kidney transplant recipients should receive PCP prophylaxis
Q3= Patients not tolerating standard PCP prophylaxis should receive an alternative
Q4= Transplanted recipients must receive PCP prophylaxis long life
Discussion
PCP is rare but life-threatening opportunistic infection in immunosuppressed patients. Thus, it is highly preventable by use of effective PCP prophylaxis regimen.4-5 Despite the widespread knowledge on PCP prophylaxis, this study showed that almost 70% of the discharge prescriptions were with no prophylactic treatment for PCP among which 20% were found to be for patients with G6PD deficiency, which justifies the reason for not including a PCP prophylaxis. After pharmacist’s intervention the remaining 80% of the prescriptions were edited and a standard PCP prophylaxis was added (TMP-SMX).
The following are the contributing factors proposed by the focus group, which may or may not be attributed to the reason for not prescribing a standard PCP prophylaxis for eligible patients.
• Lack of knowledge
• Negligence
• Missed to prescribe
• Work load
• No available guideline/policy/protocols
A questionnaire was designed to identify doctors perception towards PCP prophylaxis based on the proposed contributing factors by the focus group.
The results indicated that lack of knowledge was not the motive to explain the failure of missing PCP prophylaxis in most of the prescriptions, although, there was a gap in knowledge to prescribe an alternative when standard PCP prophylaxis regimen was contraindicated.
This study indicates that reasons for discrepancy in the practice could be attributed to other influences as highlighted earlier in the focus group meeting outcomes.
To improve the practice in future, some recommendations were suggested from the focus group (Table 2).
Table 2. The Recommendations.
| Recommendation for improving practice for prescribing PCP prophylaxis |
|---|
| Formulating guidelines /policies/protocols |
| Design a checklist for kidney transplant recipients |
| Generate a computerised reminder |
| Clinical pharmacist involvement in discharge process |
| Educational sessions |
PCP: Pneumocystic Carnii Pneumonia
In spite of high frequency of prescriptions missing an appropriate PCP prophylaxis for patients recently underwent kidney transplantation, pharmacists contribution improved the practice and all eligible patients were discharged with appropriate PCP prophylaxis. A local policy was produced to facilitate clinical pharmacist involvement in discharge process of all kidney transplant recipients. This will ensure that the discharge prescriptions are complete and appropriate.
Conclusion
In the absence of prophylaxis, the incidence of PCP in solid organ transplant recipients ranges from 6.8% to 22%, necessitating PCP prophylaxis for at least 6 months following transplantation. This study showed that doctors were highly knowledgeable on importance of PCP prophylaxis but despite that most of the patients were discharged with no prophylactic treatment for PCP. Clinical pharmacist’s input was able to identify and intervene the prescriptions which did not contain PCP prophylaxis for kidney transplant recipients. To date, prophylaxis is the most effective and novel treatment against PCP in renal transplant recipients. Further studies required to evaluate the outcome of this study as a change in practice towards better.
Acknowledgements
Thanks to all nephrology doctors specially nephrology senior consultant doctor Nabil Mohsin for his kind support. Also many thanks to all pharmacy staff specially my colleagues in clinical pharmacy services. The authors report no conflict of interest and no funding has been received in this work.
References
- 1.Fishman JA. Pneumocystis carinii and parasitic infections in transplantation. Infect Dis Clin North Am 1995. Dec;9(4):1005-1044 [PubMed] [Google Scholar]
- 2.Gordon SM, LaRosa SP, Kalmadi S, Arroliga AC, Avery RK, Truesdell-LaRosa L, et al. Should prophylaxis for Pneumocystis carinii pneumonia in solid organ transplant recipients ever be discontinued? Clin Infect Dis 1999. Feb;28(2):240-246 10.1086/515126 [DOI] [PubMed] [Google Scholar]
- 3.Elinder C-G, Andersson J, Bolinder G, Tydén G. Effectiveness of low-dose cotrimoxazole prophylaxis against Pneumocystis carinii pneumonia after renal and/or pancreas transplantation. Transpl Int 1992. May;5(2):81-84 [DOI] [PubMed] [Google Scholar]
- 4.van Hooff JP. Pneumocystis carinii pneumonia after renal transplantation. Transplantation 1997. May;63(9):1370 10.1097/00007890-199705150-00031 [DOI] [PubMed] [Google Scholar]
- 5.Higgins RM, Bloom SL, Hopkin JM, Morris PJ. The risk and benefits of low-dose cotrimoxazole prophylaxis for pneumocystis pneumonia in renal transplantation. Transplantation 1988;47:55. [PubMed] [Google Scholar]