Abstract
Ocular angiogenesis, characterized by the formation of new blood vessels in the avascular area in eyes, is a highly coordinated process involved in retinal vasculature formation and several ocular diseases such as age-related macular degeneration, proliferative diabetic retinopathy and retinopathy of prematurity. This process is orchestrated by complicated cellular interactions and vascular growth factors, during which endothelial cells acquire heterogeneous phenotypes and distinct cellular destinations. To date, while the vascular endothelial growth factor has been identified as the most critical angiogenic agent with a remarkable therapeutic value, the Notch signaling pathway appears to be a similarly important regulator in several angiogenic steps. Recent progress has highlighted the involvement, mechanisms and therapeutic potential of Notch signaling in retinal vasculature development and pathological angiogenesis-related eye disorders, which may cause irreversible blindness.
INTRODUCTION
Retinal vasculature and choroidal vasculature, two major portions of the ocular vasculature, constitute a finely ordered vascular system that guarantees blood supply to the highly oxygen-consuming retina. The primary function of the choroidal vasculature is to provide nutrients and oxygen to the outer retina, whereas the retinal vascular network supplies the inner retina. The physiological functions of the retina are confined by this normal ocular vasculature, which is established primarily by ocular angiogenesis in late embryogenesis (human) or early postnatal days (mouse) (1). However, the anatomical and physiological properties of posterior ocular segments make the ocular vasculature vulnerable to exogenous and endogenous insults, leading to pathological ocular angiogenesis and vision loss in a number of eye diseases (2), such as exudative age-related macular degeneration (AMD) and proliferative diabetic retinopathy (PDR). Systemic reasons or local microenvironmental factors in these diseases stimulate abnormal neovascular growth from the existing retinal capillaries in and out of the inner surface of the retina (retinal neovascularization) (1) and from the choroidal vessels breaking into Bruch’s membrane beneath the retinal pigment epithelium (RPE) or neural retina (choroidal neovascularization [CNV]) (3). PDR is the leading cause of irreversible blindness in working-age adults (4), with 40,000 new patients per year in 16 million diabetic Americans (5). AMD is considered as the major reason for blindness in elderly populations, which affects as many as 15 million Americans with 200,000 new cases each year. In AMD patients, although exudative AMD with the common complication of CNV constitutes only 10% of AMD, it accounts for nearly 90% of blindness in AMD patients. Retinopathy of prematurity (ROP), in contrast, occurs in premature infants with the disruption of retinal vascular development due to exposure to hyperoxic circumstance and is one of the most common causes of childhood blindness worldwide (6). An inadequate supply of angiogenic factors in the early stages of retinal vasculature formation in ROP results in vasoobliterative changes followed by compensatory new vessels growing between vascularized and avascularized areas in the retina. These pathological vessels can induce fibrotic scarring in the retina, vitreous and lens.
Antiangiogenic therapies have already been successfully used in treating these ocular diseases (5). The currently representative therapy is the neutralization of vascular endothelial growth factor (VEGF) activity (6). VEGF is not only required for retinal and choroidal vessel formation during developmental stages, but also for the maintenance of these capillaries after birth (7,8). More importantly, distorted expression of VEGF in pathological settings is the key stimulus to abnormal vessel growth (6). Blocking VEGF signaling by using VEGF aptamer, neutralizing anti-VEGF antibody or soluble VEGF receptor (VEGFR)-1 (sVEGFR1 or VEGF trap) has been shown not only to stop the pathological angiogenic process, but also to improve vision in a great proportion of AMD patients during a 2-year follow-up (6). However, this field is now facing the challenge of drug resistance and recurring cases while using these agents. Further investigation of alternative signals regulating ocular angiogenesis might elicit potentially new therapeutic targets. Recent intensive studies, mainly on the basis of models of ocular angiogenesis and gene-modified mice, have revealed the significance of Notch signaling in angiogenesis-associated ocular diseases.
CELLULAR AND MOLECULAR ASPECTS OF OCULAR ANGIOGENESIS
The retinal vasculature in mice develops as angiogenic sprouts protruding from the optic disc immediately after birth. During the first postnatal week, sprouts from retinal vessels constantly extend over the superficial retinal layer to form a two-dimensional vascular network. Then the retinal vessels continue to sprout and penetrate into deeper retinal layers, finally leading to the formation of a three-layered vascular system by the end of the third postnatal week (9). Sharing the common steps and molecular mechanisms with angiogenesis in the whole body, the postnatal retinal development in mice provides an ideal platform to angiogenesis studies on imaging and intervention without the difficulties associated with investigating embryonic development.
The primary signal initiating retinal angiogenesis is VEGF, which is secreted by retinal astrocytes and forms a radial gradient of concentration to guide the direction of vessel sprouts (12). In response to VEGF, quiescent endothelial cells (ECs) differentiate into subpopulations with coordinating cellular behaviors to fulfill the angiogenic process. Tip cells are specialized ECs located at the tips of angiogenic sprouts and respond to the VEGF gradients by migration to guide the sprout extending through the extracellular matrix. Stalk cells are located behind tip cells in a sprout and respond to VEGF by proliferation, while being responsible for extracellular matrix production and lumen formation. A third type of EC in angiogenesis is phalanx cells, which do not proliferate but align and form a smooth monolayer of cells. Thus, during angiogenesis, in each new vascular sprout, a single tip cell pioneers an angiogenic pathway by using filopodia to guide a sprouting vessel to follow the VEGF gradient. This pioneering tip cell is highly motile but proliferates minimally or not at all. Trailing behind it are stalk cells, which react to the lower levels of VEGF and proliferate to elongate the new vascular tube. Therefore, the tip-stalk paradigm formed by the endothelial specification, together with VEGF, guides retinal angiogenesis in the physiological and pathological angiogenic process (10–12).
Recent advances have shown that ocular vascularization requires not only sprouting angiogenesis from preexisting vasculature, but also postnatal vasculogenesis involving bone marrow (BM)-derived endothelial precursor cells (EPCs) (13–15). The specific molecular markers of EPCs are currently controversial; however, the hallmarks include the progenitor cell phenotype and a partially EC-specific phenotype with a strong proangiogenic activity. EPCs are mobilized from BM in response to tissue-derived signals and are homed to sites of neovascularization, contributing to vascular growth either directly via incorporation into newly formed vascular structures or indirectly via the secretion of proangiogenic factors.
THE NOTCH SIGNALING PATHWAY AND ITS ROLE IN OCULAR VASCULATURE AND VASCULAR DISEASES
The Notch Signaling Pathway
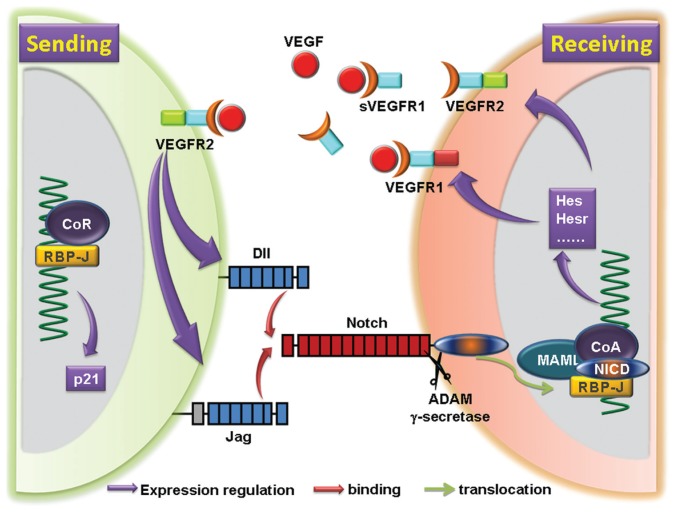
Notch signaling is an evolutionarily highly conserved pathway mediating direct signaling between neighboring cells in metazoans (16). In mammals, five canonical Notch ligands [jagged 1 (Jag1) and Jag2 and delta-like 1 (Dll1), Dll3 and Dll4] and four Notch receptors (Notch1–4) have been described (17). The single-pass transmembrane Notch receptors are activated by binding to the ligands, which are expressed also as single-pass transmembrane proteins. This ligand–receptor interaction triggers sequential receptor cleavages within the transmembrane domain, resulting in the release of the Notch intracellular domain (NICD). Disintegrin, metalloproteinase family members and the γ-secretase complex (disintegrin and metalloproteinase domain-containing protein 10 [ADAM-10], ADAM-17 and presenilin) have been identified to mediate the receptor cleavages. NICD moves into the nucleus and binds to transcriptional factor CSL (C promoter–binding factor 1 [CBF-1]/suppressor of hairless [Su(H)]/Lin-12 and Glp-1 [LAG-1], also known as J kappa-recombination signal-binding protein [RBP-J] in rodents), which is normally repressed by a corepressor complex. Association of NICD and CSL replaces the corepressors with a coactivating complex containing Mastermind-like (MAML) protein and activates the transcription of downstream genes (Figure 1).
Figure 1.
Canonical Notch signaling and crosstalk with VEGF signaling. VEGF signaling up-regulates the expression of Notch ligands and receptors on ECs. Notch ligands on the signal-sending cell trigger Notch receptors on the adjacent signal-receiving cell, leading to receptor cleavage by ADAM and γ-secretase and the release of NICD. NICD translocates into the nucleus, where it associates with RBP-J, and converts RBP-J from a transcriptional repressor into an activator by recruiting transcriptional coactivators (CoA) to replace coreppressors (CoR). The transcription of target genes such as Hes are turned on. The p21 expression is also regulated by Notch activation. Notch signaling downregulates VEGFR2 and upregulates VEGFR1, leading to differentiation of tip and stalk cells, among other changes of ECs during angiogenesis.
The Notch pathway is critically involved in vasculature development (18). Notch1, Notch4, Dll1, Dll4, Jag1 and Jag2 are expressed by ECs during physiological and pathological angiogenesis (19–24). Key components of Notch signaling including RBP-J (25), MAML1 (26), Numb (22) and downstream target hairy/enhancer-of-split related with YRPW motif 1 (Hey1), Hey2 and hairy and enhancer of split 1 (Hes1) (26–28) are also detected in vessels. In mouse retinal vasculature, active Notch1, Jag1, Dll1 and Dll4 with distinct distribution patterns have been described (29, see below). Cellular analysis and genetic inactivation or mutation in mice or zebrafish retina, in combination with ocular disease models, have demonstrated that Notch signaling plays a fundamental role during embryonic and postnatal ocular angiogenesis and participates in angiogenic ocular diseases.
Roles of Notch Signaling in Ocular Vasculature
Notch signal in retinal angiogenic sprouting
Notch receptor–ligand distribution follows a distinct pattern during angiogenesis (29). In the developing retinal vasculature of mice, Dll4 is expressed in tip cells leading the growing vascular sprouts. In addition, the Notch1 receptor keeps active but is periodically expressed during the whole process of retinal vascular formation. This expression pattern is in accordance with Notch signaling controlling angiogenic sprouting via tip cell selection (29). Indeed, several studies, using Dll4 haploinsufficient mice (Dll4+/−), VecadCreER-Notch1flox/flox mice, Tie1Cre-Jag1flox/flox mice and PdgfbCreER-Jag1flox/flox mice or molecules including Dll4-Fc, γ-secretase inhibitors and Jag1 peptide, have demonstrated that Notch signaling regulates retinal angiogenesis by restricting tip cell specification and sprouting (30–33). Insufficient Notch signaling increases the number of tip cells and promotes EC proliferation in the postnatal mouse retina (30,31) and developing zebrafish vasculature (34). A transcriptome analysis of tip cell–enriched genes in the retina suggests that Dll4/Notch signaling possibly functions on matrix remodeling, basement membrane formation and release of secreted molecules (35). Dll1, another critical Notch ligand in vascular development, is expressed in both arteries and veins of the developing vascular network, but is absent in the mature arterial branch points. Though Dll1 and Dll4 share similar protein structure, the involvement of Dll1 in retinal angiogenic sprouting remains unclear. Future investigations may illustrate whether Dll1 participates in this angiogenic step and deduce its therapeutic value.
It is notable that the spatial expression pattern of Dll4 is not fully compatible with a simple tip–stalk signaling interaction. Jag1 is detected in stalk cells in the developing vasculature front and at arterial branch points, a site where Dll4 is clearly absent (29). A recent study identified Jag1 as an additional critical component in the process of tip cell selection. Jag1 enriched in the stalk cells could antagonize Dll4/Notch signaling in cells via Fringe family glycosyltransferases (32). Consequently, stalk cells should have little ability to activate Dll4/Notch signaling in adjacent tip cells, thus allowing the latter with high VEGFR2 expression to respond to external VEGF. Jag1 may also counteract Dll4/Notch signaling interactions between stalk ECs, which helps to sustain elevated VEGFR2 expression in the freshly formed and therefore immature vascular plexus at the angiogenic front (Figure 2).
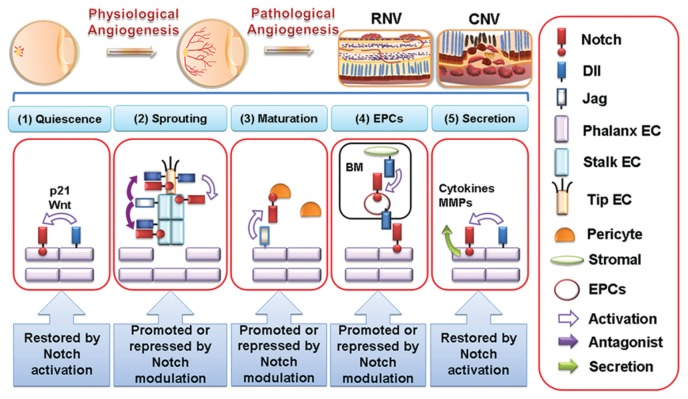
Figure 2.
Diverse roles of Notch signaling in regulating angiogenic ocular angiogenesis. Ocular vasculature formation is a finely ordered vascular system that relies on physiological angiogenesis. Pathological angiogenesis, on the other hand, results in a various angiogenesis related ocular diseases such as retinal neovascularization (RNV) and CNV. Notch signaling participates in vasculature formation and angiogenic ocular diseases by regulating vascular quiescence through p21 and Wnt signaling (1), angiogenic sprouting through tip formation and guidance (2), vessels maturation through EC-pericyte communication (3), EPC mobilization and function (4) and EC functions (5). Therefore, intervention of Notch signaling in each step of angiogenesis might have therapeutic potentials.
Notch signal in retinal vasculature maturation
Vessel maturation is marked by pericyte coverage, although the extent varies depending on the type and location of vessels (36). Capillaries in the retina and central nervous system possess a high density of pericytes (37), implying the critical significance of vascular maturity in these tissues. The Notch signal functions in pericyte recruitment via communications between ECs and pericytes. Notch3 is highly expressed in pericytes, and disruption of Notch3 signaling results in enlarged vessels due to the lack of pericyte coverage (38). In Notch3-deficient mice, retinal vascularization is reduced with diminished sprouting and vascular branching (39), as a result of progressive loss of vessel coverage due to impaired mural cell recruitment. In a mouse ROP model, loss of vessel coverage caused by Notch3 deficiency decreases pathological neovascularization, implying that proper modulation on pericytes by Notch activity could be an alternative treatment of pathological angiogenesis. The proangiogenic function of Notch3 requires EC-expressed Jag1, indicating that heterotypic Notch signaling between ECs and pericytes is critical in vascular maturation (40). In addition, modulation of Dll4 also results in altered EC and pericyte phenotypes in tumor angiogenesis (41,42). Thus, since the expressions of Jag1 and Dll4 exhibit distinct temporal and spatial pattern in retinal vasculature, Notch signaling seems to be involved in retinal vasculature maturation in multiple stages and regions.
Notch signal in retinal vascular stability
In the physiological condition, ECs in vessels remain quiescent to prevent excessive vessel sprouting in the existing vascular architecture. Sainson et al. (43), by using a three-dimensional in vitro system, first reported that cell-autonomous Notch signaling in ECs regulates vessel diameter, limits branching at the tip of sprouts and thereby establishes a mature, quiescent vascular phenotype. In retinal ECs, the Notch signal downstream gene basic helix–loop–helix transcription factor (HESR1) also participates in maintaining retinal vasculature stability (44). By using Cre-LoxP–mediated conditional gene deletion of RBP-J, Dou et al. (45) first confirmed in vivo that a lack of Notch signaling disrupted vascular homeostasis. Disruption of RBP-J induces spontaneous angiogenesis in the retina and cornea, as well as in internal organs such as the liver and lung, demonstrating that Notch signaling is critical in maintaining EC quiescence (45). A potential interpretation is that Notch activation induces EC cycle arrest through repression of p21 (cyclin-dependent kinase inhibitor-1) expression and participates in contact inhibition (46). Moreover, increased Notch activity due to a lack of Nrarp, an inhibitor of Notch signaling, has been reported to stabilize nascent blood vessels during retinal angiogenesis in mice and intersegmental vessel formation in zebrafish (47). This stabilization of nascent vessels requires Nrarp-mediated crosstalk between Notch and Wnt signaling to control stalk cell proliferation. More recently, Liu et al. (48) reported that loss of Notch1 caused cornea neovascularization, widespread vascular tumors and organism lethality secondary to massive hemorrhage, further supporting a cell-autonomous role of Notch signaling in maintaining the vascular stability.
Notch signal in adult vasculogenesis
The Notch signaling pathway, known to be important for the maintenance and differentiation of various stem and progenitor cell populations, is also involved in EPC regulation (49–51). A study from Kwon et al. (52) identified that the perturbation of Jag1 function leads to a reduction in the number of EPCs and an impaired biological activity and regenerative capacity of these cells (52). We have observed that Notch signaling participates in the development of CNV by regulating the proliferation, migration and differentiation of EPCs (45). The exact molecular mechanisms of Notch signaling on EPCs still remain elusive. Dll4 expression by BM-derived EPCs may affect their communication with tumor vessel ECs, thereby modulating tumor angiogenesis by affecting vascular stability (53). It has been identified that stromal-derived factor 1 (SDF1) and its receptor CXCR4 play an important role in angiogenesis by recruiting EPCs from BM to angiogenic sites (54). We have shown that Notch signaling dynamically regulates the expression of CXCR4 on EPCs in BM and peripheral blood, which might explain in part how the Notch signal influences EPCs in tissue regeneration (55). More studies are necessary to elucidate the involvement and mechanisms of BM-derived EPCs in ocular angiogenesis and diseases, as well as the regulatory role of Notch signaling, before reaching novel diagnostic and therapeutic strategies.
Notch signal in EC function
ECs function not only as building blocks of vessel walls, but also respond to microenvironments by producing bioactive molecules such as cytokines, growth factors and so on (56). During partial hepatectomy–induced liver regeneration, for example, liver sinusoidal ECs are triggered at the early stage to produce interleukin (IL)-6, which is critical in the upregulation of hepatocyte growth factor receptor in hepatocytes and consequent hepatocyte proliferation (57). We have shown that Notch signaling may regulate the function of liver sinusoidal ECs in liver regeneration through the expression of VEGFR1 and VEGFR2 (58). In addition, Notch signaling can modulate the secretion of matrix metalloproteases by ECs and influence cell matrix refolding (59). The role of ECs in stem/progenitor cell differentiation in vascular niches also involves Notch signaling (60), at least partly through regulating the secretion of the trophic factors such as hepatocyte growth factor (58). Whether Notch signaling participates in ocular vascular angiogenesis and related diseases through the regulation of EC function is an open question. Also, it will be interesting to investigate if Notch signaling modulates the secretion of paracrine factors such as platelet-derived growth factor (PDGF) (61) by EPCs in ocular angiogenesis.
Notch signaling in nonvascular cells during retinal angiogenesis
Apart from ECs, nonvascular cells such as astrocytes, microglia and macrophages are closely associated with sprouting ECs in retinal angiogenesis (62–64). Roles of Notch signaling in regulating astrocyte activation, microgial response and macrophage recruitment in retinal angiogenesis and neurodegenerative diseases have emerged recently. It is reported that Notch1 controls macrophage recruitment to influence EC anastomosis during retinal angiogenesis (65). Notch1 could also modulate the innate responses of microglia and astrocytes to microenvironmental insults (66). In solid tumors, Notch activation favors classic (M1) macrophage polarization while skewing down alternative (M2) macrophage polarization, which is a promoting factor for tumor angiogenesis (67). Modulating Notch signaling might therefore be a potential therapeutic approach in ischemic-related retinal degenerative disorders and inflammation-induced ocular angiogenesis.
Notch Signaling in Ocular Vascular Diseases
Since Notch signaling plays a fundamental role in the vascular system, deregulated Notch signaling has been identified in human cardiovascular- and neurovascular-related diseases such as CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy) syndrome caused by mutations in Notch3 (68). Similarly, haploinsufficiency in Jag1 causes cardiac malformation, a complication observed in 60–70% of patients suffering from Alagille syndrome (69). Notably, >90% of children with Alagille syndrome have an unusual abnormality of the eyes, including posterior embryotoxon, optic disc drusen, angulated retinal vessels and a pigmentary retinopathy (70).
The specific role of Notch signaling in modulating pathologic ocular angiogenesis was first identified in the pathologic angiogenic models of ROP, also called oxygen-induced retinopathy (33). The exposure of mouse pups to hyperoxia results in a rapid obliteration of capillaries in the central retina. The avascular retinal area initiates extensive abnormal neovascularization upon return to normoxia, exhibiting ectopic growth of epiretinal vascular tufts into the vitreous and subsequent re-growth of the lost superficial retinal vessels. According to a series of studies by Lobov and colleagues (33,71), Dll4/Notch signaling acts in at least two ways to participate in oxygen-induced retinopathy. These authors have demonstrated that genetic deletion of Dll4 or administration of Dll4-Fc, which inhibits Dll4/Notch signaling, caused enhanced angiogenic sprouting and regrowth of lost retinal vessels while suppressing ectopic pathologic neovascularization in the oxygen-induced retinopathy model. The administration of Dll4-Fc to oxygen-induced retinopathy mice stimulates more extensive angiogenic sprouting from capillaries and veins bordering the avascular zone, resulting in a more rapid regrowth of blood vessels into the avascular central retina. This could be because the lack of Dll4/Notch signaling leads to increased number and activity of filopodia-bearing tip cells and enhanced EC proliferation, which, when combined, induce more sproutings and vessel growth. On the other hand, Dll4-Fc dramatically suppressed the ectopic growth of pathologic neovascular tufts into the vitreous, as well as the formation of abnormal arteriovenous shunts. As shown by the same group recently, this might be due to the Dll4/Notch regulating vessel remodeling and regression through rapidly fine-tuning the expression of a distinct subset of vasoactive genes (71). Dll4/Notch inhibition upregulates the expression of vasodilators and suppresses the expression of vasoconstrictors, therefore reducing vessel occlusion and maintaining blood flow that is essential for survival of microvessels. Thus, pharmacologic inhibition of Dll4 might have therapeutic applications to treat eye disorders characterized by pathologic angiogenesis. However, some evidence has suggested that Notch inhibition might also aggravate pathologic angiogenesis after ischemia (72–75). A distinct microenvironment possibly directs Notch signal to play diverse roles under ischemic context. For instance, hypoxia could skew the expression pattern of Notch targets, thereby influencing pathologic angiogenesis in retinopathy (76).
Recent studies have also indicated the involvement of Notch signaling in CNV. We have investigated the role of Notch signaling in laser-induced CNV in mice by using the Cre-LoxP–mediated conditional deletion of RBP-J (45). Lack of the Notch signal enhances the angiogenic responses to injury in a laser-induced CNV model, accompanied by the upregulation of VEGFR2 and downregulation of VEGFR1 that might lead to enhanced EC proliferation. Meanwhile, excessive tip cells are induced in the angiogenic responses in this context (unpublished data). A recent study further supports the role of Notch signaling in CNV by activating or inhibiting Notch signaling with a Jag1 peptide or a γ-secretase inhibitor, respectively (77). These authors demonstrated that the activation of the Notch pathway reduced the volume of CNV lesions, whereas inhibition of the Notch pathway promoted CNV growth, as shown by the development of hyperdense retinal vasculature. Groups of proangiogenic (VEGFR2, Ccr3 and PDGF-B) and antiangiogenic (VEGFR1 and Unc5b) genes are associated with the Notch-mediated CNV alterations in this study. In vitro, enhanced Notch signal by ectopic Dll4 overexpression in the retinal–choroidal EC line RF/6A reduces cell proliferation, migration and transmigration across a monolayer of RPE cells (78). In addition to ECs, RPE cells may be another target of the Notch signal in CNV, because the Notch signal is of importance in RPE development, and constitutive Notch activity leads to RPE hyperproliferation (79). Altogether, these data suggest that Notch signaling is a key regulator of CNV and may be an alternative target for therapeutic intervention in wet AMD.
In PDR, diabetic microangiopathy is characterized by abnormal interactions between ECs and pericytes (80). Although to date no direct evidence of the Notch signal in PDR has been shown, the Notch signal in mediating EC–pericyte communication has been firmly established (39). In the retinal microvasculature, the Notch signal is also involved in EC and pericyte apoptosis, a process requiring interaction with the Hedgehog pathway and modulation by aberrant blood flow (81). In addition, modulation of the Notch signal has been reported to enhance neovascularization and reperfusion in diabetic mice by regulating the responsiveness of ECs to VEGF (82), which is pathologically high in diabetic retinopathy (83,84). Thus, the Notch signal might interact with the VEGF signal at multiple levels to modulate EC proliferation and differentiation, as well as vessel structure, which are frequently abnormal in PDR.
Molecular Mechanisms of Notch Signaling in Regulating Ocular Vasculature Formation and Diseases
Interaction with VEGF signaling
VEGF signaling is the master regulator in ocular angiogenesis (85). The three VEGF receptors, VEGFR1, VEGFR2 and VEGFR3, are expressed by ECs and are receptor tyrosine kinases activated upon VEGF triggering. Numerous studies have highlighted the crosstalk between Notch signaling and VEGF signaling, which has been reviewed elsewhere by different authors (86,87). Notably, because both Notch ligands and receptors are transmembrane proteins and mediate cell–cell contact signaling, they most likely play a fine-tuning function in physiological and pathological angiogenesis, which are initiated primarily by VEGF signaling. The current understanding is that VEGF initiates angiogeneic sprouting through different mechanisms and signal transduction pathways and also induces Notch signaling in ECs simultaneously. The consequent activated Notch signaling promotes differentiation of the tip versus stalk cells and inhibits VEGF-induced EC proliferation through p21 (88–90). Therefore, Notch signaling guarantees proper EC differentiation, on one hand, and acts in a feedback fashion as a “brake” or negative regulator of VEGF-induced angiogenesis, on the other, to control overexuberant vascular sprouting and EC proliferation and thereby promote the timely formation of a productive and well-differentiated vascular network (Figure 1).
Vascular sprouting in the postnatal mouse retina has been extensively exploited to illustrate how Notch signaling coordinates with VEGF signaling (12). VEGF gradients established by microenvironmental cells such as astrocytes induce the initial migratory sprouting response, whereas the tip–stalk cell paradigm is patterned out via distinct Notch ligand expression leading to unequivalent responses to VEGF. The leading tip cells express Dll4 and activate the Notch signal in the adjacent stalk cells that express Jag1 and attenuate the effects of VEGF on stalk cells. This result is achieved primarily through differential regulation of VEGFRs, namely downregulating VEGFR2 and up-regulating VEGFR1 (87,91). VEGFR1 can be expressed as a truncated version, resulting in the formation of soluble VEGFR1 (sVEGFR1), which is a potent paracrine inhibitor of VEGF signaling and plays an essential role in keeping the cornea transparent (56). It is of note that the Dll4/Notch signal upregulates the expression of VEGFR1, providing a novel mechanism for the Notch signal to inhibit VEGF responses in distant ECs, not just in adjacent ECs. Moreover, VEGFR1 mediates the upregulation of IL-6 production by liver sinusoidal ECs in partial hepatectomy–induced liver regeneration (92), suggesting a potential role of Notch signaling in regulating EC function, such as in cytokine secretion. In addition, VEGFR1-specific ligand placenta growth factor is reduced by Notch activation (56), although the precise regulation remains poorly understood. On the other hand, reduced expression of VEGFR2 in stalk cells by Notch activation leads to a discrepancy of VEGFR2 between tip cells and stalk cells. The integrated output of these effects is that stalk cells acquire the phenotype of lower migration and higher proliferation in response to VEGF. Furthermore, differential VEGFR levels in turn modulate Dll4 expression for ECs to compete for tip selection (93). The Notch signal downstream gene HESR1 is assumed to mediate the transcriptional regulation of VEGFRs (94). The regulation of Notch signaling on VEGFR3 is currently controversial. The NICD complex has been demonstrated to bind directly to the VEGFR3 promoter to initiate its transcription (95). Paradoxically, induced expression of VEGFR3 is observed in Dll4+/− and γ-secretase inhibitor–treated retinas (96).
Interaction with EphrinB2/EphB4 signaling
EphrinB2 and EphB4 are membrane-bound receptor tyrosine kinases that play essential roles in vasculogenesis and angiogenesis by mediating cell-to-cell communication (97). EphrinB2 is specifically expressed in arterial angioblasts, ECs and perivascular mesenchymal cells, whereas EphB4 is expressed only in ECs of venous lineage. In artery–vein endothelium specification during vasculogenesis, EphrinB2 is identified as a direct Notch target for which expression is induced by Dll4/Notch signaling (98), rendering ECs an arterial identity (99). In postnatal angiogenesis, such as tumor angiogenesis, VEGF-induced Dll4/Notch signaling upregulates EphrinB2 expression to coordinately regulate abnormal remodeling of tumor vessels (100). Djokovic et al. (101) recently reported that combined intervention of Dll4/Notch and EphrinB2/EphB4 targeting tumor neovascularization could provide increased efficacy and increased safety over Dll4/Notch inhibition alone. This finding implies that the functions of EphrinB2 and Notch signaling in angiogenesis are not redundant even though EphrinB is downstream from the Notch signal. Notably, a recent study by Sawamiphak et al. (102) offers a possible underlying mechanism for the crosstalk between Notch and EphrinB2 in tip cell guidance. Whereas Notch signaling regulates the expression of VEGFR2, EphrinB2 could control the internalizations of VEGFR2 to direct filopodial extension on tip cells.
Other signaling pathways and downstream targets
Notch signaling also crosstalks with transforming growth factor (TGF)-β signaling to regulate vasculature formation. During mouse retinal vasculature development, the tip cell–stalk cell duality is plastic and tip cells can be “reabsorbed” into the parental vessel. It is believed that tip and stalk cells physically alternate along the leading edge of the retinal plexus, which involves a number of coupled feedback loops associated with VEGF, Notch and TGF-β (102). TGF-β suppresses cell cycle entry of tip and stalk cells through p21waf1 (103). In addition, TGF-β also promotes migration of the tip cells directly through induction of inhibitor of DNA binding 1 (Id1) (104). Li et al. (105) recently demonstrated that the TGF-β signaling molecule Smad4 in association with RBP-J stabilizes cerebrovascular EC–pericyte interactions by regulating the transcription of N-cadherin, suggesting a role of these two pathways in maintaining cerebrovascular integrity.
The Wnt pathway is also critically involved in ocular physiological and pathological vasculature (106). Recently, coordination of Notch and Wnt signaling was investigated in retinal vasculature formation (47). Nrarp counteracts Notch signaling in stalk cells by inducing the degradation of NICD and by inducing Wnt signaling, which together promote vessel stability by tightening intercellular junctions and elongating vessels by overcoming cell-cycle arrest induced by Notch signaling.
CONCLUSION
In conclusion, the Notch signal plays a pivotal role in retinal vascular morphogenesis during development and in pathological angiogenesis associated with ocular diseases. Although the precise mechanisms of Notch signaling are far from being fully illustrated at each stage of angiogenesis, the identification of the Notch signal in tip cell selection, endothelial quiescence, vessel maturation and EPC mobilization and function makes it a prospective candidate for angiogenic therapies (Figure 2). A number of approaches are available or potentially possible to modulate Notch signaling at different levels of the angiogenic cascade, including antibody antagonists (33,71), antisense or interfering RNA (107), soluble ligands and receptor decoys (33,71) and inhibitors of the enzymes involved in glycosylation or cleavage of receptors, such as γ-secretase or ADAM inhibitors (108).
Inhibition of Dll4/Notch signaling promotes the reconstruction of retinal vasculature in oxygen-induced retinopathy, the mouse model of ROP (33,71). Preclinical studies targeting tumor angiogenesis through blockade of Dll4/Notch signaling showed an inhibitory effect on tumor growth (109,110), but this strategy also showed adverse effects of disrupting normal vessel homeostasis and producing significant pathologic changes in multiple organs (111). However, Dll4/Notch blockade might still be used in the treatment of ocular angiogenic diseases by local administration such as intravitreal injection or subretinal injection. Subsequent concerns about this strategy might be the effects of chronic Notch blockade on the structure and/or function of neuroretina, since the role of Notch signaling is indispensable in adult brain involving synaptic plasticity, neural stem cell maintenance and neuron survival (112–114). Moreover, most, if not all, angiogenic ocular diseases are complicated by multiple cell types, such as inflammatory cells. The effects of Notch blockade on these cells must also be determined beforehand.
Artificial activation or enhancement of the Notch signal is also presumed to inhibit angiogenesis. Expression of Dll4 in tumor cells can block sprouting from tumor blood vessels, possibly by suppressing the emergence of tip cells to reduce the tumor growth (115). In the mouse model of CNV, enhancement of Notch signaling by Jag1 peptide greatly reduces angiogenesis in CNV, indicating that Notch signaling enhancement may be a candidate therapy for CNV-related diseases (77). Thus, future investigations are anticipated to explore how to target abnormal angiogenesis by Notch activation, but maintaining the remaining vasculature that gives good access to oxygen, and how to promote the normalization of pathological angiogenesis.
ACKNOWLEDGMENTS
This work was supported by grants from the Ministry of Science and Technology of China (2011CB510200, 2009CB521706, 2011ZXJ09101-02C), National Natural Science Foundation of China (NSFC) (30872818, 30830067) and Natural Science of Shaanxi Province (2011K12-46, XJZT11M03).
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
REFERENCES
- 1.Uemura A, Kusuhara S, Katsuta H, Nishikawa S. Angiogenesis in the mouse retina: a model system for experimental manipulation. Exp Cell Res. 2006;312:676–83. doi: 10.1016/j.yexcr.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 2.Bradley J, Ju M, Robinson GS. Combination therapy for the treatment of ocular neovascularization. Angiogenesis. 2007;10:141–48. doi: 10.1007/s10456-007-9069-x. [DOI] [PubMed] [Google Scholar]
- 3.Kent D, Sheridan C. Choroidal neovascularization: a wound healing perspective. Mol Vis. 2003;9:747–55. [PubMed] [Google Scholar]
- 4.Morello CM. Etiology and natural history of diabetic retinopathy: an overview. Am J Health Syst Pharm. 2007;64:S3–7. doi: 10.2146/ajhp070330. [DOI] [PubMed] [Google Scholar]
- 5.Dorrell M, Uusitalo-Jarvinen H, Aguilar E, Friedlander M. Ocular neovascularization: basic mechanisms and therapeutic advances. Surv. Ophthalmol. 2007;52(Suppl 1):S3–19. doi: 10.1016/j.survophthal.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 6.Kinnunen K, Yl-Herttuala S. Vascular endothelial growth factors in retinal and choroidal neovascular diseases. Ann Med. 2011 2011 Feb 1; doi: 10.3109/07853890.2010.532150. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Provis JM, et al. Development of the human retinal vasculature: cellular relations and VEGF expression. Exp Eye Res. 1997;65:555–68. doi: 10.1006/exer.1997.0365. [DOI] [PubMed] [Google Scholar]
- 8.Saint-Geniez M, Maldonado AE, D’Amore PA. VEGF expression and receptor activation in the choroid during development and in the adult. Invest Ophthalmol Vis Sci. 2006;47:3135–42. doi: 10.1167/iovs.05-1229. [DOI] [PubMed] [Google Scholar]
- 9.Stahl A, et al. The mouse retina as an angiogenesis model. Invest Ophthalmol Vis Sci. 2010;51:2813–26. doi: 10.1167/iovs.10-5176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerhardt H, et al. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J Cell Biol. 2003;161:1163–77. doi: 10.1083/jcb.200302047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Smet F, Segura I, De Bock K, Hohensinner PJ, Carmeliet P. Mechanisms of vessel branching: filopodia on endothelial tip cells lead the way. Arterioscler Thromb Vasc Biol. 2009;29:639–49. doi: 10.1161/ATVBAHA.109.185165. [DOI] [PubMed] [Google Scholar]
- 12.Carmeliet P, De Smet F, Loges S, Mazzone M. Branching morphogenesis and antiangiogenesis candidates: tip cells lead the way. Nat Rev Clin Oncol. 2009;6:315–26. doi: 10.1038/nrclinonc.2009.64. [DOI] [PubMed] [Google Scholar]
- 13.Alev C, Ii M, Asahara T. Endothelial progenitor cells: a novel tool for the therapy of ischemic diseases. Antioxid Redox Signal. 2011;15:949–65. doi: 10.1089/ars.2010.3872. [DOI] [PubMed] [Google Scholar]
- 14.Lima e Silva R, et al. The SDF-1/CXCR4 ligand/receptor pair is an important contributor to several types of ocular neovascularization. FASEB J. 2007;21:3219–30. doi: 10.1096/fj.06-7359com. [DOI] [PubMed] [Google Scholar]
- 15.Friedlander M, et al. Progenitor cells and retinal angiogenesis. Angiogenesis. 2007;10:89–101. doi: 10.1007/s10456-007-9070-4. [DOI] [PubMed] [Google Scholar]
- 16.Kidd S, Lockett TJ, Young MW. The Notch locus of Drosophila melanogaster. Cell. 1983;34:421–33. doi: 10.1016/0092-8674(83)90376-8. [DOI] [PubMed] [Google Scholar]
- 17.Gridley T. Notch signaling in vascular development and physiology. Development. 2007;134:2709–18. doi: 10.1242/dev.004184. [DOI] [PubMed] [Google Scholar]
- 18.Gridley T. Notch signaling in the vasculature. Curr Top Dev Biol. 2010;92:277–309. doi: 10.1016/S0070-2153(10)92009-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phng LK, Gerhardt H. Angiogenesis: a team effort coordinated by Notch. Dev Cell. 2009;16:196–208. doi: 10.1016/j.devcel.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Claxton S, Fruttiger M. Periodic delta-like 4 expression in developing retinal arteries. Gene Expr Patterns. 2004;5:123–7. doi: 10.1016/j.modgep.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Villa N, et al. Vascular expression of Notch pathway receptors and ligands is restricted to arterial vessels. Mech Dev. 2001;108:161–4. doi: 10.1016/s0925-4773(01)00469-5. [DOI] [PubMed] [Google Scholar]
- 22.Favre CJ, et al. Expression of genes involved in vascular development and angiogenesis in endothelial cells of adult lung. Am J Physiol Heart Circ Physiol. 2003;285:H1917–38. doi: 10.1152/ajpheart.00983.2002. [DOI] [PubMed] [Google Scholar]
- 23.Xue Y, et al. Embryonic lethality and vascular defects in mice lacking the Notch ligand Jagged1. Hum Mol Genet. 1999;8:723–30. doi: 10.1093/hmg/8.5.723. [DOI] [PubMed] [Google Scholar]
- 24.Carlson TR, et al. Endothelial expression of constitutively active Notch4 elicits reversible arteriovenous malformations in adult mice. Proc Natl Acad Sci U S A. 2005;102:9884–9. doi: 10.1073/pnas.0504391102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krebs LT, et al. Notch signaling is essential for vascular morphogenesis in mice. Genes Dev. 2000;14:1343–52. [PMC free article] [PubMed] [Google Scholar]
- 26.Liu ZJ, et al. Inhibition of endothelial cell proliferation by Notch1 signaling is mediated by repressing MAPK and PI3K/Akt pathways and requires MAML1. FASEB J. 2006;20:1009–11. doi: 10.1096/fj.05-4880fje. [DOI] [PubMed] [Google Scholar]
- 27.Fischer A, Schumacher N, Maier M, Sendtner M, Gessler M. The Notch target genes Hey1 and Hey2 are required for embryonic vascular development. Genes Dev. 2004;18:901–11. doi: 10.1101/gad.291004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor KL, Henderson AM, Hughes CC. Notch activation during endothelial cell network formation in vitro targets the basic HLH transcription factor HESR-1 and downregulates VEGFR-2/KDR expression. Microvasc Res. 2002;64:372–83. doi: 10.1006/mvre.2002.2443. [DOI] [PubMed] [Google Scholar]
- 29.Hofmann JJ, Luisa Iruela-Arispe M. Notch expression patterns in the retina: an eye on receptor-ligand distribution during angiogenesis. Gene Expr Patterns. 2007;7:461–70. doi: 10.1016/j.modgep.2006.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hellstrom M, et al. Dll4 signalling through Notch1 regulates formation of tip cells during angiogenesis. Nature. 2007;445:776–80. doi: 10.1038/nature05571. [DOI] [PubMed] [Google Scholar]
- 31.Suchting S, et al. The Notch ligand delta-like 4 negatively regulates endothelial tip cell formation and vessel branching. Proc Natl Acad Sci U S A. 2007;104:3225–30. doi: 10.1073/pnas.0611177104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benedito R, et al. The Notch ligands Dll4 and Jagged1 have opposing effects on angiogenesis. Cell. 2009;137:1124–35. doi: 10.1016/j.cell.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 33.Lobov IB, et al. Delta-like ligand 4 (Dll4) is induced by VEGF as a negative regulator of angiogenic sprouting. Proc Natl Acad Sci U S A. 2007;104:3219–24. doi: 10.1073/pnas.0611206104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siekmann AF, Lawson ND. Notch signalling limits angiogenic cell behaviour in developing zebrafish arteries. Nature. 2007;445:781–4. doi: 10.1038/nature05577. [DOI] [PubMed] [Google Scholar]
- 35.del Toro R, et al. Identification and functional analysis of endothelial tip cell-enriched genes. Blood. 2010;116:4025–33. doi: 10.1182/blood-2010-02-270819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.von Tell D, Armulik A, Betsholtz C. Pericytes and vascular stability. Exp Cell Res. 2006;312:623–9. doi: 10.1016/j.yexcr.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 37.Kim JH, Kim JH, Yu YS, Kim DH, Kim KW. Recruitment of pericytes and astrocytes is closely related to the formation of tight junction in developing retinal vessels. J Neurosci Res. 2009;87:653–9. doi: 10.1002/jnr.21884. [DOI] [PubMed] [Google Scholar]
- 38.Wang T, Baron M, Trump D. An overview of Notch3 function in vascular smooth muscle cells. Prog Biophys Mol Biol. 2008;96:499–509. doi: 10.1016/j.pbiomolbio.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 39.Liu H, Zhang W, Kennard S, Caldwell RB, Lilly B. Notch3 is critical for proper angiogenesis and mural cell investment. Circ Res. 2010;107:860–70. doi: 10.1161/CIRCRESAHA.110.218271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu H, Kennard S, Lilly B. NOTCH3 expression is induced in mural cells through an autoregulatory loop that requires endothelial-expressed JAGGED1. Circ Res. 2009;104:466–75. doi: 10.1161/CIRCRESAHA.108.184846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li JL, et al. Delta-like 4 Notch ligand regulates tumor angiogenesis, improves tumor vascular function, and promotes tumor growth in vivo. Cancer Res. 2007;67:11244–53. doi: 10.1158/0008-5472.CAN-07-0969. [DOI] [PubMed] [Google Scholar]
- 42.Scehnet JS, et al. Inhibition of Dll4-mediated signaling induces proliferation of immature vessels and results in poor tissue perfusion. Blood. 2007;109:4753–60. doi: 10.1182/blood-2006-12-063933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sainson RC, et al. Cell-autonomous Notch signaling regulates endothelial cell branching and proliferation during vascular tubulogenesis. FASEB J. 2005;19:1027–9. doi: 10.1096/fj.04-3172fje. [DOI] [PubMed] [Google Scholar]
- 44.Li B, et al. Protective effects of transcription factor HESR1 on retinal vasculature. Microvasc Res. 2006;72:146–52. doi: 10.1016/j.mvr.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 45.Dou GR, et al. RBP-J, the transcription factor downstream of Notch receptors, is essential for the maintenance of vascular homeostasis in adult mice. FASEB J. 2008;22:1606–17. doi: 10.1096/fj.07-9998com. [DOI] [PubMed] [Google Scholar]
- 46.Noseda M, et al. Notch activation induces endothelial cell cycle arrest and participates in contact inhibition: role of p21Cip1 repression. Mol Cell Biol. 2004;24:8813–22. doi: 10.1128/MCB.24.20.8813-8822.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phng LK, et al. Nrarp coordinates endothelial Notch and Wnt signaling to control vessel density in angiogenesis. Dev Cell. 2009;16:70–82. doi: 10.1016/j.devcel.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu Z, et al. Notch1 loss of heterozygosity causes vascular tumors and lethal hemorrhage in mice. J Clin Invest. 2010;121:800–8. doi: 10.1172/JCI43114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Androutsellis-Theotokis A, et al. Notch signalling regulates stem cell numbers in vitro and in vivo. Nature. 2006;442:823–6. doi: 10.1038/nature04940. [DOI] [PubMed] [Google Scholar]
- 50.Diez H, et al. Hypoxia-mediated activation of Dll4-Notch-Hey2 signaling in endothelial progenitor cells and adoption of arterial cell fate. Exp Cell Res. 2007;313:1–9. doi: 10.1016/j.yexcr.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 51.Kwon SM, Alev C, Asahara T. The role of Notch signaling in endothelial progenitor cell biology. Trends Cardiovasc Med. 2009;19:170–3. doi: 10.1016/j.tcm.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 52.Kwon SM, et al. Specific Jagged-1 signal from bone marrow microenvironment is required for endothelial progenitor cell development for neovascularization. Circulation. 2008;118:157–65. doi: 10.1161/CIRCULATIONAHA.107.754978. [DOI] [PubMed] [Google Scholar]
- 53.Real C, et al. Bone marrow-derived endothelial progenitors expressing delta-like 4 (Dll4) regulate tumor angiogenesis. PLoS One. 2011;6:e18323. doi: 10.1371/journal.pone.0018323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zheng H, Fu G, Dai T, Huang H. Migration of endothelial progenitor cells mediated by stromal cell-derived factor-1alpha/CXCR4 via PI3K/Akt/eNOS signal transduction pathway. J Cardiovasc Pharmacol. 2007;50:274–80. doi: 10.1097/FJC.0b013e318093ec8f. [DOI] [PubMed] [Google Scholar]
- 55.Wang L, et al. Notch-RBP-J signaling regulates the mobilization and function of endothelial progenitor cells by dynamic modulation of CXCR4 expression in mice. PLoS One. 2009;4:e7572. doi: 10.1371/journal.pone.0007572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harrington LS, et al. Regulation of multiple angiogenic pathways by Dll4 and Notch in human umbilical vein endothelial cells. Microvasc Res. 2008;75:144–54. doi: 10.1016/j.mvr.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Ding BS, et al. Inductive angiocrine signals from sinusoidal endothelium are required for liver regeneration. Nature. 2010;468:310–5. doi: 10.1038/nature09493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang L, et al. Disruption of the transcription factor recombination signal-binding protein-Jkappa (RBP-J) leads to veno-occlusive disease and interfered liver regeneration in mice. Hepatology. 2009;49:268–77. doi: 10.1002/hep.22579. [DOI] [PubMed] [Google Scholar]
- 59.Funahashi Y, et al. Notch modulates VEGF action in endothelial cells by inducing matrix metalloprotease activity. Vasc. Cell. 2011;3:2. doi: 10.1186/2045-824X-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Han S, Dziedzic N, Gadue P, Keller GM, Gouon-Evans V. An endothelial cell niche induces hepatic specification through dual repression of Wnt and Notch signaling. Stem Cells. 2011;29:217–28. doi: 10.1002/stem.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rehman J, Li J, Orschell CM, March KL. Peripheral blood “endothelial progenitor cells” are derived from monocyte/macrophages and secrete angiogenic growth factors. Circulation. 2003;107:1164–9. doi: 10.1161/01.cir.0000058702.69484.a0. [DOI] [PubMed] [Google Scholar]
- 62.Otani A, et al. Bone marrow-derived stem cells target retinal astrocytes and can promote or inhibit retinal angiogenesis. Nat Med. 2002;8:1004–10. doi: 10.1038/nm744. [DOI] [PubMed] [Google Scholar]
- 63.Checchin D, Sennlaub F, Levavasseur E, Leduc M, Chemtob S. Potential role of microglia in retinal blood vessel formation. Invest Ophthalmol Vis Sci. 2006;47:3595–602. doi: 10.1167/iovs.05-1522. [DOI] [PubMed] [Google Scholar]
- 64.Scott A, et al. Astrocyte-derived vascular endothelial growth factor stabilizes vessels in the developing retinal vasculature. PLoS One. 2010;29:e11863. doi: 10.1371/journal.pone.0011863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Outtz HH, Tattersall IW, Kofler NM, Steinbach N, Kitajewski J. Notch1 controls macrophage recruitment and Notch signaling is activated at sites of endothelial cell anastomosis during retinal angiogenesis in mice. Blood. 2011;118:3436–9. doi: 10.1182/blood-2010-12-327015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wei Z, et al. Notch activation enhances the microglia-mediated inflammatory response associated with focal cerebral ischemia. Stroke. 2011;42:2589–94. doi: 10.1161/STROKEAHA.111.614834. [DOI] [PubMed] [Google Scholar]
- 67.Wang YC, et al. Notch signaling determines the M1 versus M2 polarization of macrophages in antitumor immune responses. Cancer Res. 2010;70:4840–9. doi: 10.1158/0008-5472.CAN-10-0269. [DOI] [PubMed] [Google Scholar]
- 68.Joutel A, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–10. doi: 10.1038/383707a0. [DOI] [PubMed] [Google Scholar]
- 69.Sainson RC, Harris AL. Regulation of angiogenesis by homotypic and heterotypic Notch signalling in endothelial cells and pericytes: from basic research to potential therapies. Angiogenesis. 2008;11:41–51. doi: 10.1007/s10456-008-9098-0. [DOI] [PubMed] [Google Scholar]
- 70.Kim BJ, Fulton AB. The genetics and ocular findings of Alagille syndrome. Semin Ophthalmol. 2007;22:205–10. doi: 10.1080/08820530701745108. [DOI] [PubMed] [Google Scholar]
- 71.Lobov IB, et al. The Dll4/Notch pathway controls post-angiogenic blood vessel remodeling and regression by modulating vasoconstriction and blood flow. Blood. 2011;117:6728–37. doi: 10.1182/blood-2010-08-302067. [DOI] [PubMed] [Google Scholar]
- 72.Arumugam TV, et al. Gamma secretase-mediated Notch signaling worsens brain damage and functional outcome in ischemic stroke. Nat Med. 2006;12:621–3. doi: 10.1038/nm1403. [DOI] [PubMed] [Google Scholar]
- 73.Kikuchi R, et al. Pitavastatin-induced angiogenesis and arteriogenesis is mediated by Notch1 in a murine hindlimb ischemia model without induction of VEGF. Lab Invest. 2011;91:691–703. doi: 10.1038/labinvest.2011.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Al Haj Zen A, et al. Inhibition of delta-like-4-mediated signaling impairs reparative angiogenesis after ischemia. Circ Res. 2010;107:283–93. doi: 10.1161/CIRCRESAHA.110.221663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Takeshita K, et al. Critical role of endothelial Notch1 signaling in postnatal angiogenesis. Circ Res. 2007;100:70–8. doi: 10.1161/01.RES.0000254788.47304.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cao R, Jensen LD, Soll I, Hauptmann G, Cao Y. Hypoxia-induced retinal angiogenesis in zebrafish as a model to study retinopathy. PLoS One. 2008;3:e2748. doi: 10.1371/journal.pone.0002748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ahmad I, et al. Regulation of ocular angiogenesis by Notch signaling: implications in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52:2868–78. doi: 10.1167/iovs.10-6608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dong X, et al. Influence of Dll4 via HIF-1alpha-VEGF signaling on the angiogenesis of choroidal neovasculariztion under hypoxic conditions. PLoS One. 2011;6:e18481. doi: 10.1371/journal.pone.0018481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schouwey K, Aydin IT, Radtke F, Beermann F. RBP-Jkappa-dependent Notch signaling enhances retinal pigment epithelial cell proliferation in transgenic mice. Oncogene. 2011;30:313–22. doi: 10.1038/onc.2010.428. [DOI] [PubMed] [Google Scholar]
- 80.Pfister F, et al. Pericytes migration: a novel mechanism of pericytes loss experimental diabetic retinopathy. Diabetes. 2008;57:2496–502. doi: 10.2337/db08-0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Walshe TE, et al. Microvascular retinal endothelial and pericyte cell apoptosis in vitro: role of Hedgehog and Notch signaling. Invest Ophthalmol Vis Sci. 2011;52:4472–83. doi: 10.1167/iovs.10-7061. [DOI] [PubMed] [Google Scholar]
- 82.Cao L, et al. Modulating Notch signaling to enhance neovascularization and reperfusion in diabetic mice. Biomaterials. 2010;31:9048–56. doi: 10.1016/j.biomaterials.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shams N, Ianchulev T. Role of vascular endothelial growth factor in ocular angiogenesis. Ophthalmol Clin North Am. 2006;19:335–44. doi: 10.1016/j.ohc.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 84.Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signaling: in control of vascular function. Nat Rev Mol Cell Biol. 2006;7:359–71. doi: 10.1038/nrm1911. [DOI] [PubMed] [Google Scholar]
- 85.Penn JS, et al. Vascular endothelial growth factor in eye disease. Prog Retin Eye Res. 2008;27:331–71. doi: 10.1016/j.preteyeres.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Siekmann AF, Covassin L, Lawson ND. Modulation of VEGF signalling output by the Notch pathway. Bioessays. 2008;30:303–13. doi: 10.1002/bies.20736. [DOI] [PubMed] [Google Scholar]
- 87.Jakobsson L, Bentley K, Gerhardt H. VEGFRs and Notch: a dynamic collaboration in vascular patterning. Biochem Soc Trans. 2009;37:1233–6. doi: 10.1042/BST0371233. [DOI] [PubMed] [Google Scholar]
- 88.Liu ZJ, et al. Regulation of Notch1 and Dll4 by vascular endothelial growth factor in arterial endothelial cells: implications for modulating arteriogenesis and angiogenesis. Mol Cell Biol. 2003;23:14–25. doi: 10.1128/MCB.23.1.14-25.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lawson ND, Vogel AM, Weinstein BM. Sonic hedgehog and vascular endothelial growth factor act upstream of the Notch pathway during arterial endothelial differentiation. Dev Cell. 2002;3:127–36. doi: 10.1016/s1534-5807(02)00198-3. [DOI] [PubMed] [Google Scholar]
- 90.Williams CK, Li JL, Murga M, Harris AL, Tosato G. Up-regulation of the Notch ligand delta-like 4 inhibits VEGF-induced endothelial cell function. Blood. 2006;107:931–9. doi: 10.1182/blood-2005-03-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Krueger J, et al. Flt1 acts as a negative regulator of tip cell formation and branching morphogenesis in the zebrafish embryo. Development. 2011;138:2111–20. doi: 10.1242/dev.063933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.LeCouter J, et al. Angiogenesis-independent endothelial protection of liver: role of VEGFR1. Science. 2003;299:890–3. doi: 10.1126/science.1079562. [DOI] [PubMed] [Google Scholar]
- 93.Jakobsson L, et al. Endothelial cells dynamically compete for the tip cell position during angiogenic sprouting. Nat Cell Biol. 2010;12:943–53. doi: 10.1038/ncb2103. [DOI] [PubMed] [Google Scholar]
- 94.Henderson AM, Wang SJ, Taylor AC, Aitkenhead M, Hughes CC. The basic helix-loop-helix transcription factor HESR1 regulates endothelial cell tube formation. J Biol Chem. 2001;276:6169–76. doi: 10.1074/jbc.M008506200. [DOI] [PubMed] [Google Scholar]
- 95.Shawber CJ, et al. Notch alters VEGF responsiveness in human and murine endothelial cells by direct regulation of VEGFR-3 expression. J Clin Invest. 2007;117:3369–82. doi: 10.1172/JCI24311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tammela T, et al. Blocking VEGFR-3 suppresses angiogenic sprouting and vascular network formation. Nature. 2008;454:656–60. doi: 10.1038/nature07083. [DOI] [PubMed] [Google Scholar]
- 97.Erber R, et al. EphB4 controls blood vascular morphogenesis during postnatal angiogenesis. EMBO J. 2006;25:628–41. doi: 10.1038/sj.emboj.7600949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Grego-Bessa J, et al. Notch signaling is essential for ventricular chamber development. Dev Cell. 2007;12:415–29. doi: 10.1016/j.devcel.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Iso T, et al. Dll4-selective Notch signaling induces ephrinB2 gene expression in endothelial cells. Biochem Biophys Res Commun. 2006;341:708–14. doi: 10.1016/j.bbrc.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 100.Hainaud P, et al. The role of the vascular endothelial growth factor-delta-like 4 ligand/Notch4-ephrin B2 cascade in tumor vessel remodeling and endothelial cell functions. Cancer Res. 2006;66:8501–10. doi: 10.1158/0008-5472.CAN-05-4226. [DOI] [PubMed] [Google Scholar]
- 101.Djokovic D, et al. Combination of Dll4/Notch and Ephrin-B2/EphB4 targeted therapy is highly effective in disrupting tumor angiogenesis. BMC Cancer. 2010;10:641. doi: 10.1186/1471-2407-10-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sawamiphak S, et al. Ephrin-B2 regulates VEGFR2 function in developmental and tumor angiogenesis. Nature. 2010;465:487–91. doi: 10.1038/nature08995. [DOI] [PubMed] [Google Scholar]
- 103.Niimi H, et al. Notch signaling is necessary for epithelial growth arrest by TGF-beta. J Cell Biol. 2007;176:695–707. doi: 10.1083/jcb.200612129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Itoh F, et al. Synergy and antagonism between Notch and BMP receptor signaling pathways in endothelial cells. EMBO J. 2004;23:541–51. doi: 10.1038/sj.emboj.7600065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li F, et al. Endothelial Smad4 maintains cerebrovascular integrity by activating N-cadherin through cooperation with Notch. Dev Cell. 2011;20:291–302. doi: 10.1016/j.devcel.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 106.Ohlmann A, et al. Norrin promotes vascular regrowth after oxygen-induced retinal vessel loss and suppresses retinopathy in mice. J Neurosci. 2010;30:183–93. doi: 10.1523/JNEUROSCI.3210-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Patel NS, et al. Up-regulation of delta-like4 ligand in human tumor vasculature and the role of basal expression in endothelial cell function. Cancer Res. 2005;65:8690–7. doi: 10.1158/0008-5472.CAN-05-1208. [DOI] [PubMed] [Google Scholar]
- 108.Kalen M, et al. Gamma-secretase inhibitor treatment promotes VEGF-A-driven blood vessel growth and vascular leakage but disrupt neovascular perfusion. PLoS One. 2011;14:e18709. doi: 10.1371/journal.pone.0018709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Noguera-Troise I, et al. Blockade of Dll4 inhibits tumour growth by promoting non-productive angiogenesis. Nature. 2006;444:1032–7. doi: 10.1038/nature05355. [DOI] [PubMed] [Google Scholar]
- 110.Ridgway J, et al. Inhibition of Dll4 signalling inhibits tumour growth by deregulating angiogenesis. Nature. 2006;444:1083–7. doi: 10.1038/nature05313. [DOI] [PubMed] [Google Scholar]
- 111.Yan M, et al. Chronic DLL4 blockade induces vascular neoplasms. Nature. 2010;463:E6–7. doi: 10.1038/nature08751. [DOI] [PubMed] [Google Scholar]
- 112.Ables JL, et al. Not(ch) just development: Notch signalling in the adult brain. Nat Rev Neurosci. 2011;12:269–83. doi: 10.1038/nrn3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hu YY, et al. Notch signaling contributes to the maintenance of both normal neural stem cells and patient-derived glioma stem cells. BMC Cancer. 2011;11:82. doi: 10.1186/1471-2407-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Komine O, et al. RBP-J promotes the maturation of neuronal progenitors. Dev Biol. 2011;354:44–54. doi: 10.1016/j.ydbio.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 115.Segarra M, et al. Dll4 activation of Notch signaling reduces tumor vascularity and inhibits tumor growth. Blood. 2008;112:1904–11. doi: 10.1182/blood-2007-11-126045. [DOI] [PMC free article] [PubMed] [Google Scholar]