Abstract
Background
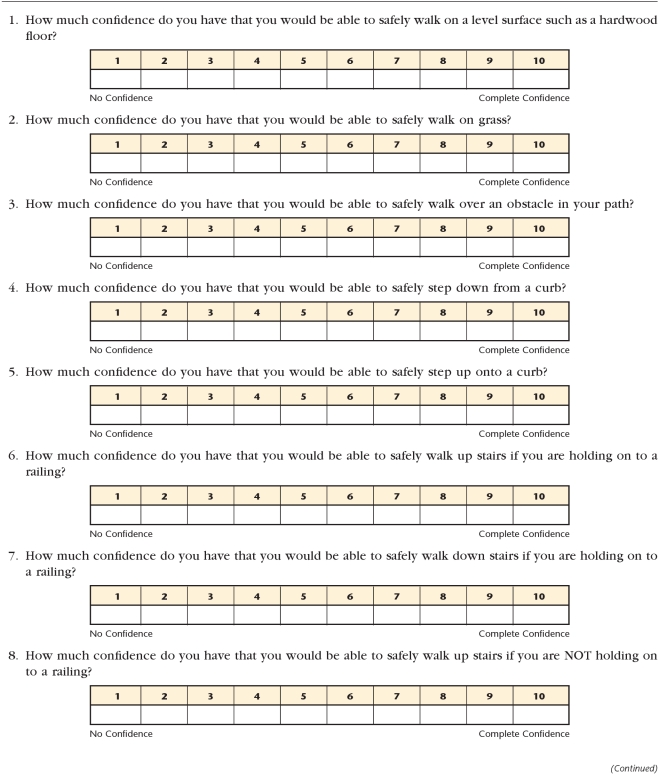
Perceived ability or confidence plays an important role in determining function and behavior. The modified Gait Efficacy Scale (mGES) is a 10-item self-report measure used to assess walking confidence under challenging everyday circumstances.
Objective
The purpose of this study was to determine the reliability, internal consistency, and validity of the mGES as a measure of gait in older adults.
Design
This was a cross-sectional study.
Methods
Participants were 102 community-dwelling older adults (mean [±SD] age=78.6±6.1 years) who were independent in ambulation with or without an assistive device. Participants were assessed using the mGES and measures of confidence and fear, measures of function and disability, and performance-based measures of mobility. In a subsample (n=26), the mGES was administered twice within a 1-month period to establish test-retest reliability through the intraclass correlation coefficient (ICC [2,1]). The standard error of measure (SEM) was determined from the ICC and standard deviation. The Cronbach α value was calculated to determine internal consistency. To establish the validity of the mGES, the Spearman rank order correlation coefficient was used to examine the association with measures of confidence, fear, gait, and physical function and disability.
Results
The mGES demonstrated test-retest reliability within the 1-month period (ICC=.93, 95% confidence interval=.85, .97). The SEM of the mGES was 5.23. The mGES was internally consistent across the 10 items (Cronbach α=.94). The mGES was related to measures of confidence and fear (r=.54–.88), function and disability (Late-Life Function and Disability Instrument, r=.32–.88), and performance-based mobility (r=.38–.64).
Limitations
This study examined only community-dwelling older adults. The results, therefore, should not be generalized to other patient populations.
Conclusion
The mGES is a reliable and valid measure of confidence in walking among community-dwelling older adults.
Mobility is an essential component of independent living for older adults.1,2 When evaluating mobility, it is important to examine both the person's ability and perception of his or her ability to complete a task.3 To determine the individual's perception of walking, the Gait Efficacy Scale (GES) was developed to specifically capture an individual's confidence to safely perform walking tasks.4,5 The GES was developed based on the social-cognitive theory principle of self-efficacy (ie, a person's belief that he or she can successfully perform a behavior).5,6 Efficacy expectations are thought to precede performance of behavior and, consequently, may influence when, where, and how the behavior is performed.4 For the behavior of walking, low self-efficacy could lead older adults to limit frequency or environments regardless of their actual walking ability. The self-imposed limitations could lead to further decline in actual and perceived ability overtime. It is important, therefore, to identify a reliable and valid measure to capture self-efficacy for walking in an older adult population.
Other self-report questionnaires have been designed to assess older adults' confidence and fear of falling, including the Falls Efficacy Scale [FES],7,8 the Activities-specific Balance Confidence [ABC] Scale,9 and the Survey of Activities and Fear of Falling in the Elderly [SAFFE].10 Each of these measures has been demonstrated to be reliable and valid for its intended purpose but poses limitations when the desired objective is to assess an individual's confidence in his or her walking during everyday activities.7–10 By focusing on the assessment of walking, the measure can be used to capture older adults' confidence in walking to perform a task and not other aspects of the performance, such as upper-extremity strength or coordination and balance required for transfers. The narrowed focus of walking confidence for the GES is in agreement with Bandura's advisement that self-efficacy can only be generalized to highly similar situations and task requirements.6
To maintain concurrence with Bandura's theory, we propose a modified version of the GES. The main reason to modify the GES was to include items that we believe are encountered in everyday walking. In the original scale, 4 of the 10 items focus on mobility related to an escalator. We thought the task of negotiating an escalator was not a common everyday activity and decided to substitute other, more common walking activities to expand the conditions assessed while staying within the parameters of daily mobility requirements of older adults. The modified GES (mGES) includes items to assess a person's confidence to safely walk on level surfaces and on grass, step over an obstacle, step up and down a curb, ascend and descend stairs (with and without a handrail), and walk a long distance. Collectively, the items cover walking tasks that reflect a range of difficulty but are part of daily mobility for older adults, thereby maintaining the specificity required to apply self-efficacy principles to overall walking ability in the older adult population.
For the variety of other versions of the GES reported in the literature, the only psychometric property reported is the internal consistency (α=.91–.93).4,5,11,12 Recently, the mGES was used in the validation of the Figure-of-8 Walk Test.13 To support the usage of the mGES in the future, it is essential to establish its reliability and validity. Therefore, the purpose of our study was to determine the reliability and validity of the mGES in community-dwelling older adults.
Psychometric properties establish the strength of a measurement tool, determine whether the tool measures what it was intended to measure, and give clinicians the inherent error of the tool.14 In this assessment of the older adults' scores on the mGES, we expected to estimate test-retest reliability and internal consistency and to determine the standard error of the measure (SEM). Furthermore, we will begin to establish the validity of the mGES by comparison with measures of confidence, fear, gait, physical function, and disability—all of which we expect to be related to the level of confidence in walking.
The mGES was designed to measure confidence in walking; therefore, we expected that individuals who reported low confidence on the mGES would report low confidence in activities of daily living (ADL) and fear with walking-related activities. We also expected that individuals who reported low confidence in walking would demonstrate poorer gait performance, worse physical function, and greater disability. Within our given comparison measures, we expected the largest correlation with measures of confidence and fear, as they assess the same concept, followed by our performance-based measures that focus on gait. Within the performance-based measures, we expected to see larger correlations with measures that include activities that are represented in the mGES than those not specifically stated. Finally, we expected the measure of function and disability to have the least correlation.
Method
Participants
The participants were community-dwelling older adults participating in an observational cohort study at the University of Pittsburgh Pepper Center, Pittsburgh, Pennsylvania (N=120), which included baseline testing with 6-month and 12-month follow-up visits. Individuals were recruited from a research registry of older adults who had previously consented to be contacted for mobility and balance-related research participation. Participants were included if they were 65 years of age or older and had the ability to walk household distances (15.24 m [50 ft]) with or without an assistive device and without the assistance of another person. Participants were excluded if they had any of the following conditions, which would affect safety during testing or would affect mobility over the following year: neuromuscular disorders that impair movement, cancer with active treatment, hospitalization for a life-threatening illness or major surgery in the previous 6 months, severe pulmonary disease, chest pain with activity, or a cardiac event such as a heart attack in the previous 6 months. Participants were determined to be cognitively intact if they had a score greater than 24 on the Mini-Mental State Examination (MMSE) and were able to converse about the contents of the study after reviewing the consent form.
Procedure
The study was a cross-sectional design and used the data from the 12-month visit. The 12-month data were limited to 102 participants for the following reasons: deceased (n=5), withdrew (n=4), missed visit (n=2), and incomplete self-report data (n=7). A subsample (n=26) participated in a second visit within 1 month of their 12-month visit to provide data for the test-retest reliability analysis. All testing was conducted at the University of Pittsburgh Pepper Center SMART (Senior Mobility Aging Research Training) Center by physical therapists or researchers trained in the measures. Testing sessions lasted, on average, 3 to 4 hours, with adequate rest breaks. Physical-based measures were alternated with questionnaires in a standardized order. All participants provided written informed consent.
The mGES
The modified Gait Efficacy Scale (mGES) is a 10-item measure that addresses older adults' perception of their level of confidence in walking during challenging circumstances. The items include walking on a level surface and on grass, stepping over an obstacle, stepping up and down a curb, ascending and descending stairs (with and without a handrail), and walking over a long distance (Appendix). The questions regarding level surface, grass, and a long distance were added to Rosengren and colleagues' 1998 version5 to expand the conditions assessed while staying within the parameters of daily mobility requirements of older adults. Ascending and descending stairs (and curbs) are unique items due to the biomechanical differences required to complete the tasks.15,16 Curbs were assessed in addition to stairs to distinguish between stepping onto and off of a single obstacle and the physical challenges of stair negotiation.5 The use of a handrail during stair negotiation increases older adults' safety and was assessed in the mGES to determine the impact of older adults' confidence with the task.17 The items are scored individually on a 10-point Likert scale, with 1 denoting no confidence and 10 representing complete confidence, giving a total score range of 10 to 100, with 100 representing complete confidence in all tasks.
Confidence and Fear Measures
FES.
The FES evaluates older adults' level of confidence in performing 10 ADL tasks (eg, taking a bath or shower, preparing simple meals, walking around the house) on a 10-point Likert scale. Lower scores represent greater confidence. The measure has established test-rest reliability (Pearson r=.71) and internal consistency (Cronbach α=.90–.91), and FES scores have been correlated with the ABC Scale scores (Pearson r=.82–.84) in community-dwelling older adults.7–10
ABC Scale.
The ABC Scale was used to assess older adults' confidence that they will not fall or lose their balance during a number of progressively challenging balance and mobility tasks. Compared with the FES, the ABC Scale provides a wider continuum of activity difficulty, has more situation-specific questions, and specifically poses the question of the level of confidence in completing a task without falling or losing balance. The ABC Scale has 16 questions, with answers ranging from 0% (no confidence) to 100% (complete confidence), and has established test-retest reliability (Pearson r=.92). The ABC Scale has been validated by comparison with the Physical Self-Efficacy Scale (Pearson r=.49) and has internal consistency (Cronbach α=.96) in community-dwelling older adults.9
SAFFE.
The SAFFE was used to assess the role of fear of falling in activity restriction. The questionnaire contains 11 activities necessary for independent living. Three subscale scores are derived: (1) SAFFE activity—number of activities performed (0–11), (2) SAFFE fear—composite score of the severity the participant worries about falling during the activities (0–3), and (3) SAFFE restriction—number of activities performed less often than 5 year previously (0–11). In community-dwelling older adults, the SAFFE has an internal consistency of α=.90 and has been associated with the FES (SAFFE activity: Pearson r=.69; SAFFE fear: Pearson r=−.76, and SAFFE restriction: Pearson r=−.59).10
Function and Disability Measure
The Late-Life Function and Disability Instrument (Late-Life FDI) was used to evaluate function and disability in older adults. The Late-Life FDI has 3 main subscales: (1) overall function, (2) disability frequency, and (3) disability limitation. The overall function subscale evaluates the amount of difficulty in performing ADL tasks, while the disability components ask how often and how limited the older adult feels in performing ADL tasks (disability frequency and disability limitation subscales, respectively). Each component is scaled to a 0 to 100 score, with 100 representing higher function or less disability. Intraclass correlation coefficients for test-retest reliability range from .68 to .98 for the 3 components.18,19 The overall function and disability limitation subscales were correlated with the Short Physical Performance Battery (SPPB) (Pearson r=.65 and r=.37, respectively) and with 400-m gait speed (Pearson r=.69 and r=.44, respectively), whereas the disability frequency subscale was not significantly correlated with the SPPB or with 400-m gait speed in community-dwelling older adults.20
Performance-Based Mobility Measures
Gait speed.
Participants' gait speed was determined by walking on a 4-m computerized walkway (GaitMat II, E.Q. Inc, Chalfont, Pennsylvania) with additional 2-m panels at each end to allow for acceleration and deceleration. The participant's “usual walk” gait speed was averaged over 4 passes and has demonstrated test-retest reliability (ICC=.98).21 In community-dwelling older adults, slow gait speed is associated with older age and an increased fear of falling.21,22
Six-Minute Walk Test (6MWT).
The 6MWT measures walking endurance and exercise capacity by having participants walk as far as possible in 6 minutes. In community-dwelling older adults, the 6MWT has demonstrated test-retest reliability (Pearson r=.95).23 The distance covered during the 6MWT has been shown to decrease with age and worsening health status and is correlated with gait speed (Pearson r=−.73).23–25
Figure-of-8 Walk Test.
The Figure-of-8 Walk Test was used to determine participants' curved-path walking ability, which is necessary for daily living in the home and community.26 The participants walked in a figure-of-8 pattern at their usual pace around 2 cones that were 1.5 m (5 ft) apart, and the time to complete the Figure-of-8 was recorded. The Figure-of-8 Walk Test has demonstrated test-retest reliability (ICC=.84) and interrater reliability (ICC=.90). The Figure-of-8 Walk Test is correlated with gait speed (Pearson r=−.57) and the Late-Life FDI (Pearson r=−.47) in community-dwelling older adults.13
Timed “Up & Go” Test (TUG).
The TUG was designed as a basic measure of mobility in older adults. The TUG was used to measure the time required for the participant to stand up from a chair, walk 3 m, turn around, walk back, and sit down. In community-dwelling older adults, the TUG has demonstrated test-retest reliability (ICC=.99) and has been correlated with the ABC Scale (Pearson r=−.70).27
Narrow and obstacle walk tests.
The narrow and obstacle walk tests were administered following the protocol from the Walking InCHIANTI Toolkit (WIT). The narrow walk test required the participant to walk 4 m at his or her usual pace within a 15-cm corridor marked on the floor. The time for the participant to complete the walk and the number of deviations from the 15-cm-wide path were recorded. Participants who could not complete the test independently or who stepped outside of the walkway more than 10 times were classified as unable. The obstacle walk test involved stepping over 2 obstacles within a 7-m distance. A small (6-cm-high) obstacle was placed at 2 m, and a large (30-cm-high) obstacle was placed at 4 m, according the WIT protocol.28 The time for the participant to complete the walk was recorded. Participants completed 2 trials of each walk (narrow and obstacle), and the mean time was calculated for each condition. These tasks require an individual to modify his or her gait kinematics during the walk. Standardized narrow and obstacle walk tests are valuable tools that simulate challenging circumstances older adults face on a daily basis.29,30 In community-dwelling older adults, the narrow and obstacle walk tests have demonstrated test-retest reliability (ICC=.76 and .89, respectively).31
Simple and complex walking while talking (WWT) tests.
The WWT tests were developed as a cognitive challenge during walking to predict falls by imposing the need to divide attention. During the simple WWT test, participants were asked to say the letters of the alphabet out loud while walking down a 6.2-m (20-ft) corridor. The complex WWT test differs from the simple WWT test in that individuals are asked to say every other letter of the alphabet out loud over the 6.2-m corridor. Each test was repeated twice, and an average time for each test was recorded. The interrater reliability for the simple WWT test was Pearson r=.60. The simple WWT test demonstrated a specificity of 89.4% and sensitivity of 46.1% with a time of 20 seconds or longer (on a 12.2-m [40-ft] corridor) as a predictor of falls in community-dwelling older adults.31 The complex WWT test predicts falls in older adults with a time of 33 seconds or longer (on a 12.2-m corridor) with a specificity of 95.6% and sensitivity of 38.5% in community-dwelling older adults.32
Data Analysis
The IBM SPSS Statistics version 18.0 (SPSS Inc, an IBM Company, Chicago, Illinois) was utilized for all data analysis. Descriptive statistics, including mean and standard deviation, were reported for continuous data, and number and percentage of participants for categorical data were calculated for the sample characteristics for the total sample and reliability subsample. The mean and median were presented as the measures of central tendency for the mGES and for the measures of confidence, fear, function, disability, and performance-based mobility. The sample distribution was supported by the standard deviation, observed range, and percentage at the floor and ceiling for the questionnaires with a defined range. A ceiling effect was defined as a measurement limitation of an instrument whereby the scale cannot determine increased performance beyond a certain level. In contrast, a floor effect was defined as a measurement limitation of an instrument that cannot determine decreased performance beyond a certain level.
The test-retest reliability was determined in a subsample of participants (n=26) who repeated the mGES within a 1-month period of their 12-month visit. Independent sample t tests and chi-square analyses were conducted to compare the reliability subsample with the total sample. An ICC (2,1) and 95% confidence interval (CI) were calculated to represent the test-retest reliability. The SEM was calculated as the square root of the error variance (mean square error term) from the analysis of variance used to calculate the ICC, and the 95% CI of the SEM was calculated following the method described by Stratford and Goldsmith.33 The SEM provides an estimate of the measurement error in the tool, and changes in test results equal to or greater than the SEM can be considered real change.34 Cronbach α was calculated to determine the internal consistency and was evaluated for consistency as each item was deleted in a stepwise fashion.35
The mGES was designed as a measure of confidence in walking. Therefore, to begin to establish the validity of the measure, we compared the mGES with measures of confidence and fear in walking-related activities and with performance-based measures of gait. Because walking plays an important role in physical function and disability, we also compared the mGES with a self-report measure of physical function and disability. Spearman rank order correlation coefficients were calculated to determine the associations between the mGES and the measures of confidence, fear, gait, physical function, and disability. The Fisher Z transformation was used to calculate the 95% CI for the correlation coefficient.
Our analyses mainly involved assessing correlations with other measures for validity and correlations of mGES at 2 different times for reliability. Standard sample size and power estimation techniques showed that our analyses had the ability to detect statistical significance of correlation coefficients as small as .52 and .27, respectively, with n=26 (for reliability analyses) and n=102 (for validity analyses) and with 80% statistical power in 2-tailed tests conducted at α=.05.
Role of the Funding Source
This work was supported by Pitt Clinical Research Training in Geriatrics and Gerontology (T32 AG021885), the Pittsburgh Older Americans Independence Center (NIA P30 AG024827), and a Beeson Career Development Award (NIA K23 AG026766).
Results
Descriptive Statistics
Of the 102 community-dwelling older adults studied, the majority were women (74.5%), Caucasian (87.2%), married (60.8%), and college educated (72.5%) and had a mean (SD) age of 78.6 (6.1) years. The subsample (n=26) used to determine test-retest reliability was chosen to provide a typical range of mobility, based on gait speed, seen in community-dwelling older adults. This group demonstrated sociodemographic characteristics similar to those of the total sample (Tab. 1).
Table 1.
Characteristics of the Total Sample and the Reliability Subsample
a P value determined by t test for continuous variables (age, body mass index, and height) and by chi-square analysis for categorical variables (sex, race, marital status, education, and employment).
Our reliability subsample (n=26) provided a spread of mGES scores (28–100), with a low ceiling effect (7.8%) and a mean (SD) of 79.25 (19.25). On the second administration of the mGES, the subsample had a lower mean (SD) 78.00 (21.81) and higher percentage at the ceiling (11.5%), but the differences from the total sample were not significant (P=.77). The mGES was able to capture the level of confidence of 23 of the 30 participants who scored the lowest (ie, most confident or ceiling effect) on the FES. Table 2 provides the central tendencies and distributions for the measures of confidence and fear, the measures of function and disability, and the performance-based measures of mobility.
Table 2.
Central Tendency and Distribution of Confidence and Fear Measures, Function and Disability Measures, and Performance-Based Mobility Measures
a mGES=modified Gait Efficacy Scale, FES=Falls Efficacy Scale, ABC Scale=Activities-specific Balance Confidence Scale, SAFFE=Survey of Activities and Fear of Falling in the Elderly, Late-Life FDI=Late-Life Function and Disability Instrument, 6MWT=Six-Minute Walk Test, TUG=Timed “Up & Go” Test, simple WWT test=simple walking while talking test, complex WWT test=complex walking while talking test.
b Total sample.
c Subsample, first administration.
d Subsample, second administration.
Reliability, SEM, and Internal Consistency
The mGES demonstrated test-retest reliability within the 1-month period (ICC [2,1]=.93, 95% CI=.85, .97) (n=26). The SEM of the mGES was 5.23 (95% CI=4.10, 7.22). The Cronbach α was .94 and revealed no change with a stepwise deletion of any single item (n=102).
Validity
The associations between the mGES and confidence, fear, function, and disability are shown in Table 3. The mGES correlated with the FES (r=−.80), ABC Scale (r=.88), and Late-Life FDI overall function subscale (r=.88). The mGES also was associated with performance-based mobility measures (Tab. 3). Faster gait speed during the usual walk, narrow walk, obstacle walk, simple WWT, and complex WWT tests were associated with higher levels of confidence. A greater distance covered in the 6MWT, less time to complete the TUG, and less time for the Figure-of-8 Test was associated with greater gait efficacy (ie, greater mGES scores).
Table 3.
Spearman Rank Order Correlations of Modified Gait Efficacy Scale (mGES) and Confidence and Fear Measures, Function and Disability Measures, and Performance-Based Measures of Mobility
a 95% CI=95% confidence interval, FES=Falls Efficacy Scale, ABC Scale=Activities-specific Balance Confidence Scale, SAFFE=Survey of Activities and Fear of Falling in the Elderly, Late-Life FDI=Late-Life Function and Disability Instrument, 6MWT=Six-Minute Walk Test, TUG=Timed “Up & Go” Test, simple WWT test=simple walking while talking test, complex WWT test=complex walking while talking test.
Discussion
Older adults' confidence in their walking ability during everyday activities may be as important for their social participation as their actual ability. In our evaluation of community-dwelling older adults with moderate to high functioning, as evident by their gait speed, TUG, and ABC Scale results (Tab. 2), lower levels of confidence in walking were reported on the mGES by participants who also demonstrated poorer performance on physical-based mobility measures and reported increased disability limitations on the Late-Life FDI.
As proposed by Bandura, self-efficacy can be shaped by performance accomplishments.6,36 Through increasing older adults' confidence, the potential to improve their function and lessen their risk of decline due to self-imposed activity restriction may be possible. Physical therapists are uniquely positioned to provide older adults with a safe, supervised environment in which to practice walking skills. With the enhancement in their walking abilities, improvements in their self-efficacy might be expected as well. To initiate this approach, the first step is to identify deficits in self-efficacy using a measure that can be repeated over the time of intervention. The mGES appears to be a reliable and valid measure of confidence of older adults in everyday walking tasks. The demonstrated test-retest reliability of the mGES illustrates its dependability, and based on the SEM, the threshold for a “true” change in score appears to be 6 points.
Incorporating the mGES into clinical practice provides physical therapists with a number of advantages when working with other adults at risk for mobility decline. It is important to remember that self-efficacy not only has a direct effect on an individual's choice of activities and environments but also influences the individual's potential success with the activity.37 Therefore, in addition to the utility of the mGES as an evaluation and outcomes tool, investigation into responses on individual items could potentially help tailor physical therapy intervention targeted at improving walking confidence. For example, if a patient reports low confidence walking on grass, the intervention may target mobility on uneven surfaces. By addressing self-efficacy, clinicians may tighten the gap that sometimes exists between performance on tests of physical function and reported ability for completion of similar or even the same activities.3,38–40
When applying measures of self-efficacy, it is critical for clinicians to consider the objective of the measure and to chose the appropriate tool for their patients. The FES has a narrowed application for community-dwelling older adults with high functioning demonstrated by the high ceiling effect.9 The ABC Scale is a more appropriate tool to evaluate community-dwelling older adults' confidence in maintaining their balance during challenging activities that may or may not require a walking component. If the focus of the evaluation or intervention is older adults' walking abilities, the mGES should be the practitioner's measure of choice because it focuses on confidence in walking among community-dwelling older adults.
Older adults who express fear of falling often state lower confidence in their ability to perform ADL tasks than those who are not afraid, and they restrict the type of and frequency of activities they perform.10,40 The correlation found between the SAFFE and mGES is consistent with these earlier findings. The varying degrees of correlation between the mGES and Late-Life FDI subsections demonstrate that older adults perceive limitations other than confidence in performing activities, such as financial obligations, social interactions, and personal preferences.
Performance-based measures of walking provide valuable information about older adults' physical abilities and, as expected, were correlated with the mGES. One of the most highly related performance-based measures with the mGES was the obstacle walk test. This finding might be expected because the mGES specifically asks about confidence in stepping over obstacles.28 The mGES does not specifically refer to curved path walking or turns in walking, which may explain the low correlations with the Figure-of-8 Walk Test and the TUG, respectively.
The performance-based measures showed a varying degree of relationship with the mGES, which suggests the mGES does provide some different information than what is captured by physical performance, a finding that is supported in the literature.1,2,41 We agree with previous authors who advocated for the use of both types of measures.42–44 Research has shown that self-report and performance-based outcomes after balance intervention may correlate only weakly,45,46 and the same could be expected after walking intervention. For example, an older adult with only modest gains in performance may have made substantial gains in self-efficacy by self-report, which could greatly affect his or her social participation.47–49 Gains in self-efficacy would be missed if only performance-based measures were evaluated because confidence does not necessarily reflect ability.6,36
The practicality of applying the mGES to inpatient, outpatient, and home care physical therapy settings is high. Administration of the tool requires less than 5 minutes and minimal training. The only equipment needed is a copy of the tool (Appendix), and the straightforward summation of item responses allows for quick interpretation of the overall score. Although the mGES was not self-administered in our cohort, we believe that the straightforward and simplistic nature of the tool would easily allow self-administration by older adults. The internal consistency and low ceiling effect of the mGES support its applicability to the majority of community-dwelling older adults. In comparison with the Ambulatory Self-Confidence Questionnaire,49 the mGES has less patient burden (10 items versus 22 items) and maintains the focus on conditions older adults experience on an everyday basis. The Ambulatory Self-Confidence Questionnaire involves community-based conditions, which would limit its applicability to adults with higher functioning and would not be appropriate to apply to inpatient and home care settings. These distinguishing factors potentially make the mGES a more appropriate tool to apply to a wide spectrum of older adults.
In future investigations of the psychometric properties of the mGES, it would be helpful to examine the interrater, self-administration, and individual item reliability. It also would be beneficial to look at the application of the mGES in a sample of older adults in diverse settings, such as inpatient hospitalization and home care. Although the SEM was computed, further investigation into the responsiveness of the mGES in community-dwelling older adults is recommended.
Conclusion
The data provide sufficient evidence to support the reliability and validity of the mGES as a measure of walking confidence during everyday activities in community-dwelling older adults, and the mGES may be useful in identifying older adults who have changed mobility confidence over time or from an intervention.
Appendix.
Appendix.
The Modified Gait Efficacy Scale (mGES)
Footnotes
All authors provided concept/idea/research design and writing. Dr Hile and Dr Brach provided data collection and project management. Ms Newell and Dr Brach provided data analysis. Dr Brach provided fund procurement and participants. Dr VanSwearingen, Dr Hile, and Dr Brach provided consultation (including review of manuscript before submission).
The study was approved by the University of Pittsburgh Institutional Review Board.
This research was presented at the Annual Scientific Meeting of the American Geriatrics Society; May 11–14, 2011; National Harbor, Maryland.
This work was supported by Pitt Clinical Research Training in Geriatrics and Gerontology (T32 AG021885), the Pittsburgh Older Americans Independence Center (NIA P30 AG024827), and a Beeson Career Development Award (NIA K23 AG026766).
References
- 1. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 2. Cress ME, Schechtman KB, Mulrow CD, et al. Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc. 1995;43:93–101 [DOI] [PubMed] [Google Scholar]
- 3. Reuben DB, Valle LA, Hays RD, Siu AL. Measuring physical function in community-dwelling older persons: a comparison of self-administered, interviewer-administered, and performance-based measures. J Am Geriatr Soc. 1995;43:17–23 [DOI] [PubMed] [Google Scholar]
- 4. McAuley E, Mihalko SL, Rosengren KS. Self-efficacy and balance correlates of fear of falling in elderly. J Aging Phys Act. 1997;5:329–340 [Google Scholar]
- 5. Rosengren KS, McAuley E, Mihalko SL. Gait adjustments in older adults: activity and efficacy influences. Psychol Aging. 1998;13:375–386 [DOI] [PubMed] [Google Scholar]
- 6. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215 [DOI] [PubMed] [Google Scholar]
- 7. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:239–243 [DOI] [PubMed] [Google Scholar]
- 8. Hauer K, Yardley L, Beyer N, et al. Validation of the Falls Efficacy Scale and Falls Efficacy Scale International in geriatric patients with and without cognitive impairment: results of self-report and interview-based questionnaires. Gerontol. 2010;56:190–199 [DOI] [PubMed] [Google Scholar]
- 9. Powell LE, Myers A. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol. 1995;50:M28–M34 [DOI] [PubMed] [Google Scholar]
- 10. Lachman ME, Howland J, Tennstedt S, et al. Fear of falling and activity restriction: the Survey of Activities and Fear of Falling in the Elderly. J Gerontol B Psychol Sci Soc Sci. 1998;53:P43–P50 [DOI] [PubMed] [Google Scholar]
- 11. Hu L, McAuley E, Elavsky S. Does the Physical Self-Efficacy Scale assess self-efficacy or self-esteem? J Sports Exerc Psych. 2005;27:152–170 [Google Scholar]
- 12. Umstattd MP, McAuley E, Motly RW, Rosengren KS. Pessimism and physical functioning in older women: influence of self-efficacy. J Behav Med. 2007;30:107–114 [DOI] [PubMed] [Google Scholar]
- 13. Hess RJ, Brach JS, Piva SR, VanSwearingen JM. Walking skill can be assessed in older adults: validity of the Figure-of-8 Walk Test. Phys Ther. 2010;90:89–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jewell DV. Guide to Evidence-Based Physical Therapy Practice. Sudbury, MA: Jones and Bartlett Publishers; 2008 [Google Scholar]
- 15. Zachazewski JE, Riley PO, Krebs DE. Biomechanical analysis of body mass transfer during stair ascent and descent of healthy subjects. J Rehabil Res Dev. 1993;30:412–422 [PubMed] [Google Scholar]
- 16. McFayden BJ, Winter DA. An integrated biomechanical analysis of normal stair ascent and descent. J Biomech. 1988;21:733–744 [DOI] [PubMed] [Google Scholar]
- 17. Reeves ND, Spanjaard M, Mohagheghi AA, et al. Influence of light handrail use on the biomechanics of stair negotiation in old age. Gait Posture. 2008;28:327–336 [DOI] [PubMed] [Google Scholar]
- 18. Jette AM, Haley SM, Coster WJ, et al. Late-Life Function and Disability Instrument, I: development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57:M209–M216 [DOI] [PubMed] [Google Scholar]
- 19. Haley SM, Jette AM, Coster WJ, et al. Late-Life Function and Disability Instrument, II: development and evaluation of the functional component. J Gerontol A Biol Sci Med Sci. 2002;57:M217–M222 [DOI] [PubMed] [Google Scholar]
- 20. Sayers SP, Jette AM, Haley SM, et al. Validation of the Late-Life Function and Disability Instrument. J Am Geriatr Soc. 2004;52:1554–1559 [DOI] [PubMed] [Google Scholar]
- 21. Brach JS, Perera S, Studenski S, Newman AB. The reliability and validity of measures of gait variability in community-dwelling older adults. Arch Phys Med Rehabil. 2008;89:2293–2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45:313–320 [DOI] [PubMed] [Google Scholar]
- 23. Steffen T, Hacker T, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–137 [DOI] [PubMed] [Google Scholar]
- 24. Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–841 [DOI] [PubMed] [Google Scholar]
- 25. Bautmans I, Lambert M, Mets T. The Six-Minute Walk Test in community dwelling elderly: influence of health status. BMC Geriatr. 2004;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kiriyama K, Warabi T, Kato M, et al. Medial-lateral balance during stance phase of straight and circular walking of human subjects. Neurosci Lett. 2005;388:91–95 [DOI] [PubMed] [Google Scholar]
- 27. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148 [DOI] [PubMed] [Google Scholar]
- 28. Shumway-Cook A, Guralnik JM, Phillips CL, et al. Age-associated declines in complex walking task performance: the Walking InCHIANTI Toolkit. J Am Geriatr Soc. 2007;55:58–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen HC, Ashton-Miller JA, Alexandar NB, Schultz AB. Stepping over obstacles: gait patterns of healthy young and old adults. J Gerontol. 1991;46:M196–M203 [DOI] [PubMed] [Google Scholar]
- 30. Schrager MA, Kelly VE, Price R, et al. The effects of age on medio-lateral stability during normal and narrow base walking. Gait Posture. 2008;28:466–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bandinelli S, Pozzi M, Lauretani F, et al. Adding challenge to performance-based tests of walking: the Walking InCHIANTI Toolkit (WIT). Am J Phys Med Rehabil. 2006;85:986–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Verghese J, Buschke H, Viola L, et al. Validity of divided attention tasks in predicting falls in older individuals: a preliminary study. J Am Geriatr Soc. 2002;50:1572–1576 [DOI] [PubMed] [Google Scholar]
- 33. Stratford PW, Goldsmith GH. Planning and analyzing reliability studies when the standard error of measurement is the reliability coefficient of interest. Phys Ther 1997;77:745–750 [DOI] [PubMed] [Google Scholar]
- 34. Harvill LM. Standard error of measurement. Educ Meas Issues Pract. 1991;10:181–189 [Google Scholar]
- 35. Santos J, Reynaldo A. Cronbach's alpha: a tool for assessing the reliability of scales. Journal of Extension. 1999;37:2 [Google Scholar]
- 36. Bandura A. Self-efficacy mechanism in physiological activation and health-promoting behavior. In: Madden J, ed. Neurobiology of Learning, Emotion and Affect. New York, NY: Raven Press; 1991:229–270 [Google Scholar]
- 37. Hadjistavropoulos T, Martin RR, Sharpe D, et al. A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community-dwelling older adults. J Aging Health. 2007;19:965–984 [DOI] [PubMed] [Google Scholar]
- 38. Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults. J Gerontol. 2001;56:M644–M649 [DOI] [PubMed] [Google Scholar]
- 39. Stratford PW, Kennedy D, Pagura SM, Gollish JD. The relationship between self-report and performance-related measures: questioning the content validity of timed tests. Arthritis Care Res. 2003;49:535–540 [DOI] [PubMed] [Google Scholar]
- 40. Jorstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53:501–510 [DOI] [PubMed] [Google Scholar]
- 41. Fried LP, Young Y, Rubin G, et al. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54:889–901 [DOI] [PubMed] [Google Scholar]
- 42. Alexander NB, Guire KE, Thelen DG, et al. Self-reported walking ability predicts functional mobility performance in frail older adults. J Am Geriatr Soc. 2000;48:1408–1413 [DOI] [PubMed] [Google Scholar]
- 43. Reuben DB, Siu AL, Kimpau S. The predictive validity of self-report and performance-based measures of function and health. J Gerontol. 1992;47:M106–M110 [DOI] [PubMed] [Google Scholar]
- 44. Hatch J, Gill-Body KM, Portney LG. Determinants of balance confidence in community-dwelling elderly people. Phys Ther. 2003;83:1072–1079 [PubMed] [Google Scholar]
- 45. Liu-Ambrose T, Khan KM, Eng JJ, et al. Balance confidence improves with resistance or agility training. Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology. 2004;50:373–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cyarto EV, Brown WJ, Marshall AL, et al. Comparative effects of home- and group-based exercise on balance confidence and balance ability in older adults: cluster randomized trial. Gerontology. 2008;54:272–280 [DOI] [PubMed] [Google Scholar]
- 47. Vellas BJ, Wayne SJ, Romero LJ, et al. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26:189–193 [DOI] [PubMed] [Google Scholar]
- 48. Gill TM, Desai MM, Gahbauer EA, et al. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–321 [DOI] [PubMed] [Google Scholar]
- 49. Asano M, Miller WC, Eng JJ. Development and psychometric properties of the Ambulatory Self-Confidence Questionnaire. Gerontology. 2007;53:373–381 [DOI] [PubMed] [Google Scholar]