Abstract
Characterizing relationships between diet, body weight, and health is complicated by reporting errors in dietary intake data that are associated with body weight. The objectives of this study were to assess changes in reporting across days (reactivity) on food checklists and associations between reactivity and body mass index (BMI) using data from two cross-sectional studies: 1) the Recontacting Participants in the Observing Protein and Energy Nutrition study (n = 297), which was conducted in 2003–2004 and included a 7-day checklist and a 4-day food record (FR), and 2) the America’s Menu Daily Food Report Study (n=530), which was conducted in 1996 and included a 30-day checklist. Zero-inflated Poisson regression was used to assess effects of reporting day on frequency of consumption for the checklists and number of items reported for the FR. Interactions between day and BMI were tested using contrast statements. Frequency of reported consumption declined across days among males and females for total items and many of the eight food groups on the 7-day checklist; among females, the effect of reporting day differed by BMI category for the meat, fish, and poultry group. Smaller declines across days were observed for some of the 22 food groups on the 30-day checklist; no interactions with BMI were apparent. No reporting day effects were observed in the FR data. The results suggest inconsistent reactivity across days, possibly reflecting changes in reporting or consumption behavior. However, the effects are generally small and independent of body weight, suggesting that checklists are potentially useful for the study of body weight and diet.
Keywords: dietary assessment, food checklist, measurement error, reactivity, body mass index, obesity
Introduction
Self-report instruments such as 24-hour recalls (24HR), food records (FR), and food frequency questionnaires (FFQ) are commonly used to assess dietary intake, but it is well recognized that such instruments are subject to measurement error (1–6). Reporting error is particularly salient in the context of the obesity epidemic given that accurately assessing differences in intakes among individuals of different body weights is critical to furthering our understanding of relationships between diet, body weight, and health outcomes (7–9). In addition, a growing body of literature has documented associations between reporting errors, particularly energy underreporting, and body weight (7, 9–15), suggesting that measures of dietary intake derived from self-report instruments may be more likely to inaccurately capture the dietary intakes of overweight and obese individuals compared to those of normal weight.
A source of reporting error unique to FR, which may or may not be associated with body weight, is that data collection concurrent with actual intake has the potential to create measurement reactivity; i.e., individuals may change their dietary behaviors and/or reporting of their behaviors as a result of the activity of recording (16–19). Reactivity may be particularly salient when FRs are administered over consecutive days (20). The question of whether this reactivity bias differs by body weight status is key to understanding whether the FR has a place in the study of diet and health. Although one study has not found body weight-specific reactivity in 4-day FR data (18), this question has not been extensively studied.
One type of FR is a pre-coded “checklist” composed of a short, closed-ended food list (21–29); the respondent places a check beside a food each time she or he eats it. Typically, checklists ask about a subset of foods consumed and query only frequency of consumption and not portion size. There is interest in this type of brief instrument for use in studies with limited resources or for which diet might not be the primary exposure or outcome of interest. However, little research has focused on the extent and nature of reporting errors affecting data from such instruments, including checklists. The objectives of the current analyses are to determine if reactivity, one potential source of error, affects reporting of frequency of food consumption on checklists across multiple days and whether any reactivity is associated with body mass index (BMI).
Methods
Samples and measures
This analysis employed data from the Recontacting Participants in the Observing Protein and Energy Nutrition (ReOPEN) and the America’s Menu Daily Food Report studies. The Observing Protein and Energy Nutrition (OPEN) study was conducted in 1999–2000 with 482 healthy volunteers aged 40–69 y (4, 6). Participants were recruited from a sampling frame of households with addresses listed in residential telephone directories in Montgomery County, MD. The sample was predominately non-Hispanic White and approximately 91 percent of men and 78 percent of women had an education beyond high school. Participants answered questionnaires, had height and weight measured, were dosed with doubly labeled water, and gave urine and blood samples. In October 2003, participants were contacted to participate in the ReOPEN follow-up study; a total of 345 (72%) responded. Follow-up clinic visits were conducted with 301 individuals and in-home visits were conducted with an additional 7; during these visits, participants were weighed. Self-reported weight data were available for 37 participants who moved out of the area since the OPEN study was conducted and provided ReOPEN data via mailed forms. Height data for all respondents were obtained from the original OPEN dataset.
Drawing upon an existing validated food frequency questionnaire (30), a 7-day food daily checklist (available at http://riskfactor.cancer.gov/diet/screeners/daily.html) composed of 32 foods was developed to represent general dietary patterns. The instrument underwent extensive cognitive testing prior to mail out to ReOPEN participants in January and February of 2004. Participants were instructed to record the day of the week, indicate each time they consumed a listed food, and return the checklist booklet by mail at the end of the 7-day reporting period. A total of 303 participants returned the booklet; data for 297 (86% of the ReOPEN sample) participants (n = 158 men and 139 women) with complete data for 7 consecutive days were analyzed. The ReOPEN protocol also included a 4-day food record (FR). A FR booklet, including instructions, portion size photos, and recording sheets, was mailed to participants for completion in November of 2003. For comparison purposes, the total number of items reported across food record days was examined. Complete FR data were available for 274 of the 297 participants.
The America’s Menu Daily Food Report Study was a mail survey conducted in 1996 with a sample of 623 volunteers aged 25–70 years. Participants were recruited from a sampling frame of households with addresses listed in residential telephone directories in the Washington, DC metropolitan area (29). The sample was predominately non-Hispanic White and 86 percent had an education beyond high school. A 30-day checklist instrument composed of 88 foods was developed to serve as a reference instrument in comparing two different food frequency questionnaires with regard to specific design issues, such as asking about foods in single versus multiple questions and querying about additions to foods (29). The selection of items for inclusion was based on their relevance to these design issues and on other data indicating whether an item could be expected to be consumed frequently enough over a 30-day period to provide useful data. Participants were asked to check each time a listed item was consumed and mail each completed form daily. Participants’ heights and weights were self-reported. Data for 530 (85% of the America’s Menu sample) participants (n = 189 men and 341 women) with complete checklist data for 30 consecutive days and height and weight data were analyzed.
Body mass index (BMI, kg/m2) was calculated and respondents were grouped into three BMI categories. Those with BMI of 25 or greater but less than 30 were categorized as overweight and respondents with BMI of 30 or greater were categorized as obese (31). Those with a BMI less than 25 were considered neither overweight nor obese.
Statistical methods
Analyses were conducted using SAS (version 9.2, 2008, SAS Institute Inc., Cary, NC). Models were stratified by sex to account for the possibility that reactivity may differ among men and women. The foods on the ReOPEN 7-day checklist were organized into eight food groups for analysis (Table 1) based on the groupings used on that checklist. For the America’s Menu 30-day checklist, 22 food and beverage groups were analyzed (Table 2), again based on the groupings used on that checklist. To assess whether reported frequency of consumption changed across reporting days for total items (all foods grouped together) and each individual food group, Poisson regression, a form of regression used to model count data, was used. Specifically, zero-inflated Poisson models were utilized to allow for the possibility that some participants did not consume any items in a given food group on a given day. To account for multiple observations per person, the model was fit using generalized estimating equations in PROC GENMOD. Models included covariates for reporting day, age, weekday versus weekend, and BMI category. Friday was considered a weekend day based on other analyses suggesting that intakes on Fridays are typically more similar to Saturday and Sunday then to weekdays (32). Initial models for each food group included interaction terms for BMI category and reporting day to allow the slope for reporting day to vary across the three BMI categories; a contrast statement was included to test for statistically significant interactions. If no significant interactions were observed, the model was refit without interaction terms. Reporting day effect was calculated as the percentage change per day, which is equal to 100% × (eβ − 1), where β is the regression slope for reporting day. This Poisson modeling approach was also used to examine the effect of reporting day on the total number of food items reported on the ReOPEN 4-day FR.
Table 1.
7-day mean reported frequency of consumption and percentage changea per reporting day for total items and food groups by sex and BMI categoryb, 7-day food checklist, ReOPEN, n = 297
| Males (n = 158) | Females (n = 139) | |||
|---|---|---|---|---|
| Mean (SE) | % change (95% CI) | Mean (SE) | % change (95% CI) | |
| Total items | ||||
| Overall | 12.12 (0.14) | −2.0 (−3.2, −0.8)** | 13.11 (0.21) | −1.7 (−2.8, −0.5)** |
| BMI<25 | 12.11 (0.29) | 13.11 (0.31) | ||
| 25≤BMI<30 | 12.06 (0.23) | 13.91 (0.46) | ||
| BMI≥30 | 12.24 (0.24) | 12.19 (0.34) | ||
| Meat, poultry, fish | ||||
| Overall | 1.71 (0.03) | −0.2 (−1.8, 1.5) | 1.60 (0.04) | |
| BMI<25 | 1.48 (0.07) | 1.49 (0.07) | −0.4 (−3.5, 2.8) | |
| 25≤BMI<30 | 1.72 (0.05) | 1.70 (0.08) | 3.6 (1.2, 6.0)** | |
| BMI≥30 | 1.87 (0.05) | 1.69 (0.06) | −3.9 (−7.3, −0.5)* | |
| Dairy | ||||
| Overall | 1.03 (0.03) | −0.4 (−2.7, 2.0) | 1.19 (0.04) | 0.1 (−2.3, 2.5) |
| BMI<25 | 0.93 (0.06) | 1.25 (0.05) | ||
| 25≤BMI<30 | 1.02 (0.05) | 1.24 (0.08) | ||
| BMI≥30 | 1.14 (0.06) | 1.02 (0.06) | ||
| Fruit | ||||
| Overall | 1.32 (0.05) | −3.0 (−5.6, −0.3)* | 1.64 (0.06) | −3.1 (−6.0, −0.3)* |
| BMI<25 | 1.25 (0.10) | 1.67 (0.09) | ||
| 25≤BMI<30 | 1.54 (0.08) | 1.83 (0.12) | ||
| BMI≥30 | 1.06 (0.07) | 1.37 (0.11) | ||
| Vegetables | ||||
| Overall | 2.90 (0.07) | −2.3 (−4.4, −0.1 )* | 3.56 (0.10) | −0.7 (−3.0, 1.7) |
| BMI<25 | 2.90 (0.14) | 3.45 (0.13) | ||
| 25≤BMI<30 | 2.82 (0.10) | 3.94 (0.21) | ||
| BMI≥30 | 3.01 (0.13) | 3.34 (0.16) | ||
| Cereal, breads, grains | ||||
| Overall | 2.18 (0.04) | −2.3 (−4.4, −0.1)* | 2.03 (0.05) | −1.2 (−3.1, 0.8) |
| BMI<25 | 2.42 (0.08) | 2.24 (0.08) | ||
| 25≤BMI<30 | 2.09 (0.07) | 1.99 (0.08) | ||
| BMI≥30 | 2.13 (0.07) | 1.70 (0.08) | ||
| Mixed dishes | ||||
| Overall | 0.37 (0.02) | 0.9 (−3.6, 5.5) | 0.35 (0.02) | 0.0 (−4.8, 5.0) |
| BMI<25 | 0.42 (0.04) | 0.34 (0.03) | ||
| 25≤BMI<30 | 0.32 (0.02) | 0.38 (0.04) | ||
| BMI≥30 | 0.41 (0.04) | 0.33 (0.03) | ||
| Snacks and desserts | ||||
| Overall | 1.79 (0.05) | −1.8 (−4.1, 0.6) | 1.81 (0.05) | −4.1 (−6.2, −2.0)** |
| BMI<25 | 1.90 (0.11) | 1.73 (0.06) | ||
| 25≤BMI<30 | 1.79 (0.07) | 1.96 (0.10) | ||
| BMI≥30 | 1.72 (0.07) | 1.80 (0.10) | ||
| Spreads | ||||
| Overall | 0.82 (0.03) | −5.9 (−8.6, −3.1)** | 0.91 (0.03) | −4.7 (−8.0, −1.3)** |
| BMI<25 | 0.80 (0.06) | 0.93 (0.05) | ||
| 25≤BMI<30 | 0.77 (0.04) | 0.88 (0.07) | ||
| BMI≥30 | 0.90 (0.05) | 0.92 (0.06) | ||
Adjusted for age and weekday/weekend.
Separate estimates for the regression coefficient by BMI category are provided only for meat, poultry and fish for women. No other interactions between BMI category and reporting day were observed.
p<0.05,
p<0.01
Abbreviations: BMI, body mass index; ReOPEN, Recontacting Participants in the Observing Protein and Energy Nutrition Study; SE, standard error; CI, confidence interval.
Table 2.
30-day mean reported frequency of consumption and percentage changea per reporting day for total items and food groups by sex and BMI categoryb, 30-day food checklist, America’s Menu Daily Food Report Study, n = 530
| Males (n = 189) | Females (n = 341) | |||
|---|---|---|---|---|
| Mean (SE) | % change (95% CI) | Mean (SE) | % change (95% CI) | |
| Total items | ||||
| Overall | 12.95 (0.08) | 0.03 (−0.09, 0.15) | 11.98 (0.05) | −0.14 (−0.22, −0.06)** |
| BMI<25 | 12.70 (0.12) | 12.13 (0.07) | ||
| 25≤BMI<30 | 13.42 (0.12) | 11.62 (0.09) | ||
| BMI≥30 | 12.21 (0.24) | 11.93 (0.14) | ||
| Meat & poultry | ||||
| Overall | 0.76 (0.01) | −0.26 (−0.59, 0.07) | 0.73 (0.01) | −0.33 (−0.58, −0.08)* |
| BMI<25 | 0.68 (0.02) | 0.69 (0.01) | ||
| 25≤BMI<30 | 0.81 (0.02) | 0.76 (0.02) | ||
| BMI≥30 | 0.83 (0.03) | 0.86 (0.02) | ||
| Meat & poultry not in mixtures | ||||
| Overall | 0.44 (0.01) | 0.03 (−0.40, 0.46) | 0.38 (0.01) | −0.05 (−0.42, 0.32) |
| BMI<25 | 0.39 (0.01) | 0.35 (0.01) | ||
| 25≤BMI<30 | 0.47 (0.01) | 0.40 (0.01) | ||
| BMI≥30 | 0.50 (0.03) | 0.48 (0.02) | ||
| Meat in mixtures | ||||
| Overall | 0.28 (0.01) | −0.57 (−1.22, 0.08) | 0.31 (0.01) | −0.56 (−1.01, −0.11)* |
| BMI<25 | 0.27 (0.01) | 0.31 (0.01) | ||
| 25≤BMI<30 | 0.30 (0.01) | 0.33 (0.01) | ||
| BMI≥30 | 0.27 (0.02) | 0.32 (0.02) | ||
| Reduced fat meats | ||||
| Overall | 0.03 (0.01) | −1.46 (−3.38, 0.46) | 0.04 (0.01) | −1.15 (−2.54, 0.24) |
| BMI<25 | 0.02 (0.01) | 0.03 (0.01) | ||
| 25≤BMI<30 | 0.04 (0.01) | 0.03 (0.01) | ||
| BMI≥30 | 0.06 (0.01) | 0.06 (0.01) | ||
| Milk to drink | ||||
| Overall | 0.35 (0.01) | −0.04 (−0.47, 0.39) | 0.29 (0.01) | −0.60 (−1.07, −0.13)* |
| BMI<25 | 0.32 (0.01) | 0.30 (0.01) | ||
| 25≤BMI<30 | 0.39 (0.02) | 0.27 (0.01) | ||
| BMI≥30 | 0.31 (0.02) | 0.28 (0.02) | ||
| Milk on cereal | ||||
| Overall | 0.35 (0.01) | −0.43 (−0.82, −0.04)* | 0.31 (0.01) | −0.21 (−0.52, 0.10) |
| BMI<25 | 0.40 (0.01) | 0.33 (0.01) | ||
| 25≤BMI<30 | 0.32 (0.01) | 0.31 (0.01) | ||
| BMI≥30 | 0.27 (0.02) | 0.21 (0.01) | ||
| Eggs | ||||
| Overall | 0.28 (0.01) | 0.49 (−0.14, 1.12) | 0.20 (0.01) | 0.16 (−0.39, 0.71) |
| BMI<25 | 0.27 (0.01) | 0.18 (0.01) | ||
| 25≤BMI<30 | 0.27 (0.01) | 0.18 (0.01) | ||
| BMI≥30 | 0.31 (0.03) | 0.27 (0.02) | ||
| Fruit & vegetables | ||||
| Overall | 0.92 (0.01) | −0.25 (−0.62, 0.12) | 0.96 (0.01) | −0.19 (−0.43, 0.05) |
| BMI<25 | 0.94 (0.02) | 0.95 (0.01) | ||
| 25≤BMI<30 | 0.90 (0.02) | 0.88 (0.02) | ||
| BMI≥30 | 0.91 (0.04) | 1.10 (0.03) | ||
| Juices | ||||
| Overall | 0.46 (0.01) | −0.05 (−0.50, 0.40) | 0.37 (0.01) | −0.33 (−0.76, 0.10) |
| BMI<25 | 0.51 (0.01) | 0.38 (0.01) | ||
| 25≤BMI<30 | 0.44 (0.01) | 0.35 (0.01) | ||
| BMI≥30 | 0.37 (0.02) | 0.34 (0.02) | ||
| Cereals | ||||
| Overall | 0.43 (0.01) | −0.25 (−0.70, 0.20) | 0.39 (0.01) | −0.07 (−0.44, 0.30) |
| BMI<25 | 0.52 (0.01) | 0.41 (0.01) | ||
| 25≤BMI<30 | 0.38 (0.01) | 0.39 (0.01) | ||
| BMI≥30 | 0.30 (0.02) | 0.29 (0.01) | ||
| Rolls, bagels, & breads | ||||
| Overall | 1.33 (0.01) | 0.01 (−0.23, 0.25) | 1.13 (0.01) | −0.14 (−0.32, 0.04) |
| BMI<25 | 1.30 (0.02) | 1.09 (0.01) | ||
| 25≤BMI<30 | 1.35 (0.02) | 1.13 (0.02) | ||
| BMI≥30 | 1.38 (0.04) | 1.30 (0.02) | ||
| Pasta | ||||
| Overall | 0.26 (0.01) | −0.05 (−0.62, 0.52) | 0.29 (0.01) | −0.58 (−0.97, −0.19)** |
| BMI<25 | 0.27 (0.01) | 0.30 (0.01) | ||
| 25≤BMI<30 | 0.23 (0.02) | 0.28 (0.01) | ||
| BMI≥30 | 0.26 (0.01) | 0.26 (0.01) | ||
| Soup | ||||
| Overall | 0.21 (0.01) | 0.53 (−0.14, 1.20) | 0.22 (0.01) | 0.12 (−0.37, 0.61) |
| BMI<25 | 0.23 (0.01) | 0.22 (0.01) | ||
| 25≤BMI<30 | 0.20 (0.01) | 0.21 (0.01) | ||
| BMI≥30 | 0.17 (0.01) | 0.19 (0.01) | ||
| Sweets | ||||
| Overall | 0.96 (0.01) | 0.27 (−0.12, 0.66) | 1.00 (0.01) | −0.07 (−0.32, 0.18) |
| BMI<25 | 1.01 (0.02) | 0.98 (0.01) | ||
| 25≤BMI<30 | 0.92 (0.02) | 1.03 (0.02) | ||
| BMI≥30 | 0.96 (0.04) | 1.05 (0.03) | ||
| Salty snacks | ||||
| Overall | 0.52 (0.01) | −0.06 (−0.51, 0.39) | 0.56 (0.01) | −0.69 (−1.00, −0.38)** |
| BMI<25 | 0.45 (0.01) | 0.57 (0.01) | ||
| 25≤BMI<30 | 0.57 (0.02) | 0.52 (0.01) | ||
| BMI≥30 | 0.55 (0.03) | 0.59 (0.02) | ||
| Soft drinks | ||||
| Overall | 0.69 (0.01) | −0.26 (−0.61, 0.09) | 0.68 (0.01) | −0.16 (−0.41, 0.09) |
| BMI<25 | 0.57 (0.02) | 0.64 (0.01) | ||
| 25≤BMI<30 | 0.61 (0.02) | 0.65 (0.02) | ||
| BMI≥30 | 1.31 (0.05) | 0.91 (0.03) | ||
| Coffee & tea | ||||
| Overall | 2.03 (0.03) | 0.03 (−0.15, 0.21) | 1.73 (0.02) | 0.06 (−0.08, 0.20) |
| BMI<25 | 1.84 (0.03) | 1.80 (0.02) | ||
| 25≤BMI<30 | 2.40 (0.04) | 1.73 (0.03) | ||
| BMI≥30 | 1.43 (0.06) | 1.45 (0.04) | ||
| Additions to coffee & tea | ||||
| Overall | 2.01 (0.03) | 0.09 (−0.13, 0.31) | 1.77 (0.02) | 0.04 (−0.14, 0.22) |
| BMI<25 | 2.00 (0.05) | 1.90 (0.03) | ||
| 25≤BMI<30 | 2.18 (0.05) | 1.69 (0.04) | ||
| BMI≥30 | 1.50 (0.08) | 1.34 (0.05) | ||
| Any fat added | ||||
| Overall | 0.70 (0.01) | 0.41 (−0.01, 0.82)* | 0.68 (0.01) | −0.38 (−0.67, −0.09)* |
| BMI<25 | 0.69 (0.02) | 0.69 (0.01) | ||
| 25≤BMI<30 | 0.71 (0.02) | 0.62 (0.02) | ||
| BMI≥30 | 0.70 (0.03) | 0.74 (0.02) | ||
| Regular fats added | ||||
| Overall | 0.62 (0.01) | 0.33 (−0.12, 0.78) | 0.58 (0.01) | −0.31 (−0.62, 0.01) |
| BMI<25 | 0.61 (0.02) | 0.59 (0.01) | ||
| 25≤BMI<30 | 0.64 (0.02) | 0.55 (0.02) | ||
| BMI≥30 | 0.60 (0.03) | 0.61 (0.02) | ||
| Reduced fats added | ||||
| Overall | 0.08 (0.01) | 1.02 (−0.14, 2.18) | 0.10 (0.01) | −0.77 (−1.61, 0.07) |
| BMI<25 | 0.08 (0.01) | 0.10 (0.01) | ||
| 25≤BMI<30 | 0.07 (0.01) | 0.08 (0.01) | ||
| BMI≥30 | 0.10 (0.01) | 0.13 (0.01) | ||
| Reduced fat anything | ||||
| Overall | 0.11 (0.01) | 0.20 (−0.80, 1.20) | 0.14 (0.01) | −0.89 (−1.63, −0.15)* |
| BMI<25 | 0.11 (0.01) | 0.13 (0.01) | ||
| 25≤BMI<30 | 0.11 (0.01) | 0.11 (0.01) | ||
| BMI≥30 | 0.16 (0.01) | 0.19 (0.01) | ||
Adjusted for age and weekday/weekend.
Separate estimates for the regression coefficient by BMI category are not provided because no interactions between BMI category and reporting day were observed.
p<0.05,
p<0.01
Abbreviations: BMI, body mass index; SE, standard error; CI, confidence interval.
Results and Discussion
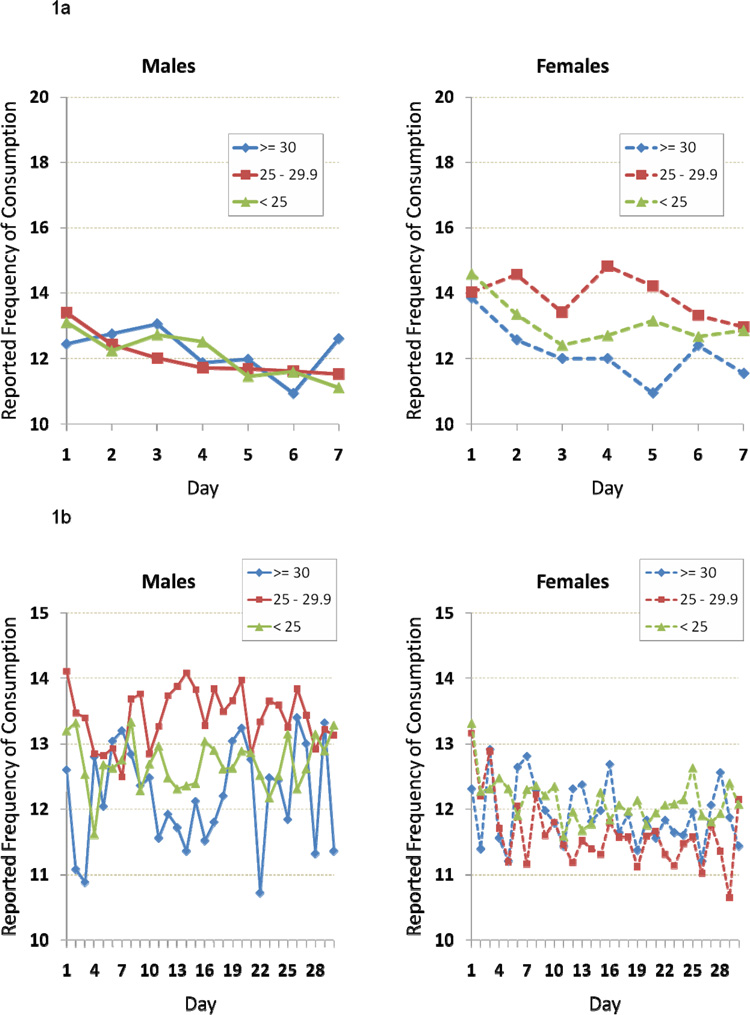
In the ReOPEN sample, 45.6 percent of males and 28.8 percent of females were overweight, 31.0 percent of males and 25.2 percent of females were obese, and 23.4 percent of males and 46.0 percent of females were neither overweight nor obese. In the America’s Menu Study sample, 43.9 percent of males and 23.5 percent of females were overweight, 13.2 percent of males and 14.1 percent of females were obese, and 42.9 percent of males and 62.5 percent of females were neither overweight nor obese. Figures 1a and 1b show the mean reported frequency of consumption by reporting day and sex for total food items on the ReOPEN and America’s Menu Study checklists respectively. Tables 1 and 2 present the 7-day and 30-day mean reported frequency of consumption for each food group and for total food items, along with the percentage change in mean per reporting day.
Figure 1.
1a: Mean reported frequency of consumption for total items across reporting days by sex and BMI category, 7-day food checklist, ReOPEN, n=297
1b: Mean reported frequency of consumption for total items across reporting days by sex and BMI category, 30-day food checklist, America’s Menu Daily Food Report Study, n=530
Abbreviations: BMI, body mass index; ReOPEN, Recontacting Participants in the Observing Protein and Energy Nutrition Study.
For total items reported on the 7-day checklist in ReOPEN, the percentage change per day was significantly different from zero for both men and women, with a decrease of 2.0% per day for men and 1.7% for women. In contrast, no statistically significant effects of reporting day on the total number of food items reported (which ranged from 5 to 39 per day among both men and women) were observed in the 4-day FR data in ReOPEN (data not shown; p=0.39 for males, 0.73 for females), or in the 30-day checklist data for men in the America’s Menu Study. There was a significant decrease per day in total items reported on the 30-day checklist among women (0.14%) but the decrease was so small as to be of little practical importance. For example, a decrease of 2.0% per day, as seen in ReOPEN, would reduce a mean of 12 on the first day to a mean of 10.6 after 7 days. In contrast, a decrease of 0.14% per day would reduce a mean of 12 on the first day to 11.9 after 7 days and 11.5 after 30 days.
Significant decreases per day were apparent for many food groups in ReOPEN including fruit; vegetables (men only); cereals, breads, and grains (men only); snacks and desserts (women only); and spreads. The largest change was seen for the spreads group, with a decrease of 5.9% per day for men and 4.7% for women. Of 22 food and beverage food groups examined in the America’s Menu Study data, significant decreases were observed for one food group among men and six food groups among women. Interestingly, effects of reporting day on reported frequency of consumption were observed for food groups that might be considered healthy and less prone to underreporting, such as fruits and vegetables and also those hypothesized to be preferentially underreported (11, 33), such as spreads, and snacks and desserts. While variation in frequency of consumption may reflect day-to-day variation in intakes, the declines across days for some food groups suggest a systematic bias associated with record keeping. This bias could be associated with changes in eating stimulated by awareness associated with the act of record keeping, such as eating less or consuming foods that are simpler to report. The declines may also reflect changes in reporting behavior; for example, tracking intakes more conscientiously earlier in the record keeping period. In general, the magnitude of the average declines related to reporting day on the checklists was relatively small. The observed differences in the magnitude of the effects between the two checklists may be due to the specific food items and groups included, the submission of reports in a weekly batch (ReOPEN) versus daily (America’s Menu Study), and the difference in length of reporting (7 days versus 30 days). From inspection of the figures, the frequency estimates for the first few days on the 30-day checklist suggest a decline from day 1 similar to that observed for the 7-day checklist, but this trend does not continue across the full 30-day reporting period. Instead, substantial fluctuations in reported frequencies are apparent; this variability may be masking the effects of reactivity over a longer period of time or reactivity may truly diminish over a longer reporting period. From these data, it is not possible to determine which case applies.
Of all the food groups examined on the 7-day ReOPEN checklist, a significant interaction between reporting day and BMI category was observed for only one food group (meat, poultry and fish) and among women only: the frequency of consumption of foods in this food group decreased 3.9% per day among women in the obese category and increased 3.6% among those in the overweight category; there was no significant change in reporting among those with BMI<25. No interactions between reporting day and BMI category were observed in the ReOPEN 4-day FR data (data not shown). There were no interactions between reporting day and BMI group for any of the food and beverage groups examined for either men or women on the America’s Menu Study 30-day checklist. Consistent with the lack of effects of body weight status, in a study of 176 women in the Women’s Health Trial Feasibility Study in Minority Populations, Rebro found a reduction in the number of food items reported on food records from day 1 to day 4, but changes over the 4 days were not associated with BMI (18).
This study is limited in that the samples of middle-aged adults are not representative of the general population; similar research is needed among different racial/ethnic groups to assess the generalizability of the findings. In addition, the rates of obesity among the sample are lower (particularly for women) than those currently observed among American adults (34). The America’s Menu Study participants and a small number of ReOPEN participants self-reported their weight via mailed forms, possibly resulting in misclassification of BMI. The analysis focused on changes in reporting across days and did not consider other possible sources of measurement error. Intakes reported on the checklists and FR were not compared to a measure of true intakes and it is not possible to tease apart the effects of recording days from true day-to-day variations in diet and any other errors that may be present. In addition, we were not able to assess any reactivity bias that might have affected reporting at the start of record keeping (i.e., on day one), but only whether reporting changed from day one onward. While our results pertain to prospectively collected food records, other research has shown a general but inconsistent decline in mean energy estimates with repeat non-consecutive 24 hour recalls (35). However, to our knowledge, the potential interaction of reactivity with body weight status has not yet been examined in other instruments.
Conclusions
The results of this study suggest some degree of reactivity in responses to food checklist tools across days of record keeping. However, the magnitude of changes in reporting across days appears to be small and, for the most part, not associated with body mass index. The lack of evidence for BMI-specific reactivity suggests that checklists could be useful tools for assessing differences in intakes associated with overweight and obesity. The study also found no evidence of reactivity across days in relation to BMI in the 4-day FR in ReOPEN, supporting the results of an earlier study (18). However, bias in reporting across days associated with reactivity is only one potential source of error and, as with any self-report dietary assessment instrument, other types of error that could affect intake estimates must be borne in mind in analysis and interpretation of data. Further research is needed to facilitate the continued development of strategies to improve the accuracy of dietary intake estimates for individuals of varying body weight status.
Acknowledgements
The authors thank Lisa Kahle for her expert programming assistance and Roberta McClimens for creating the figures.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sharon I. Kirkpatrick, Risk Factor Monitoring and Methods Branch, Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, 6130 Executive Boulevard, EPN 4005 Bethesda, MD 20892, Tel: 301-435-1638, Fax: 301-435-3710, kirkpatricksi@mail.nih.gov.
Douglas Midthune, Biometry Research Group, Division of Cancer Prevention, National Cancer Institute, 6130 Executive Boulevard, EPN 3119 Bethesda, MD 20892, Tel: 301-496-7463, Fax: 301-402-0816, midthund@mail.nih.gov.
Kevin W. Dodd, Biometry Research Group, Division of Cancer Prevention, National Cancer Institute, 6130 Executive Boulevard, EPN 3131 Bethesda, MD 20892, Tel: 301-496-7461, Fax: 301-402-0816, doddk@mail.nih.gov.
Nancy Potischman, Office of the Associate Director, Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, 6130 Executive Boulevard, EPN 4005 Bethesda, MD 20892, Tel: 301-594-0831, Fax: 301-435-3710, subara@mail.nih.gov.
Amy F. Subar, Risk Factor Monitoring and Methods Branch, Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, 6130 Executive Boulevard, EPN 4005 Bethesda, MD 20892, Tel: 301-594-0831, Fax: 301-435-3710, subara@mail.nih.gov.
Frances E. Thompson, Risk Factor Monitoring and Methods Branch, Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, 6130 Executive Boulevard, EPN 4005 Bethesda, MD 20892, Tel: 301-435-4410, Fax: 301-435-3710, thomsof@mail.nih.gov.
References
- 1.Beaton GH, Burema J, Ritenbaugh C. Errors in the interpretation of dietary assessments. Am J Clin Nutr. 1997;65 Suppl 4:1100S–1107S. doi: 10.1093/ajcn/65.4.1100S. [DOI] [PubMed] [Google Scholar]
- 2.Freudenheim JL, Marshall JR. Problem of profound measurement and power of epidemiological studies of diet and cancer. Nutr Cancer. 1988;11(4):243–250. doi: 10.1080/01635588809513994. [DOI] [PubMed] [Google Scholar]
- 3.Livingstone MB. Assessment of food intakes: are we measuring what people eat? Br J Biomed Sci. 1995;52(1):58–67. [PubMed] [Google Scholar]
- 4.Subar AF, Kipnis V, Troiano RP, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol. 2003;158(1):1–13. doi: 10.1093/aje/kwg092. [DOI] [PubMed] [Google Scholar]
- 5.Kipnis V, Midthune D, Freedman L, et al. Bias in dietary-report instruments and its implications for nutritional epidemiology. Public Health Nutr. 2002;5(6A):915–923. doi: 10.1079/PHN2002383. [DOI] [PubMed] [Google Scholar]
- 6.Kipnis V, Subar AF, Midthune D, et al. Structure of dietary measurement error: results of the OPEN biomarker study. Am J Epidemiol. 2003;158(1):4–21. doi: 10.1093/aje/kwg091. [DOI] [PubMed] [Google Scholar]
- 7.Heitmann BL, Lissner L. Dietary underreporting by obese individuals--is it specific or non-specific? Br Med J. 1995;311(7011):986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lissner L, Troiano RP, Midthune D, et al. OPEN about obesity: recovery biomarkers, dietary reporting errors and BMI. Int J Obes (Lond) 2007;31(6):956–961. doi: 10.1038/sj.ijo.0803527. [DOI] [PubMed] [Google Scholar]
- 9.Lissner L, Potischman N. Measuring food intake in free-living populations: focus on obesity. In: Allison DB, Baskin ML, editors. Handbook of assessment methods for eating behaviors and weight-related problems: measure, theory, and research. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2009. pp. 255–282. [Google Scholar]
- 10.Lissner L, Habicht JP, Strupp BJ, Levitsky DA, Haas JD, Roe DA. Body composition and energy intake: do overweight women overeat and underreport? Am J Clin Nutr. 1989;49(2):320–325. doi: 10.1093/ajcn/49.2.320. [DOI] [PubMed] [Google Scholar]
- 11.Heitmann BL, Lissner L. Obese individuals underestimate their food intake--which food groups are under-reported? Ugeskr Laeger. 1996;158(48):6902–6906. [PubMed] [Google Scholar]
- 12.Heitmann BL. The influence of fatness, weight change, slimming history and other lifestyle variables on diet reporting in Danish men and women aged 35–65 years. Int J Obes Relat Metab Disord. 1993;17(6):329–336. [PubMed] [Google Scholar]
- 13.Johansson G, Wikman A, Ahren AM, Hallmans G, Johansson I. Underreporting of energy intake in repeated 24-hour recalls related to gender, age, weight status, day of interview, educational level, reported food intake, smoking habits and area of living. Public Health Nutr. 2001;4(4):919–927. doi: 10.1079/phn2001124. [DOI] [PubMed] [Google Scholar]
- 14.Johansson L, Solvoll K, Bjorneboe GE, Drevon CA. Under- and overreporting of energy intake related to weight status and lifestyle in a nationwide sample. Am J Clin Nutr. 1998;68(2):266–274. doi: 10.1093/ajcn/68.2.266. [DOI] [PubMed] [Google Scholar]
- 15.Voss S, Kroke A, Klipstein-Grobusch K, Boeing H. Obesity as a major determinant of underreporting in a self-administered food frequency questionnaire: results from the EPIC-Potsdam Study. Z Ernahrungswiss. 1997;36(3):229–236. doi: 10.1007/BF01623369. [DOI] [PubMed] [Google Scholar]
- 16.Thompson FE, Subar AF. Dietary assessment methodology. In: Coulston AM, Boushey CJ, editors. Nutrition in the prevention and treatment of disease. 2nd ed. San Diego, CA: Academic Press; 2008. pp. 3–39. [Google Scholar]
- 17.Buzzard IM, Faucett CL, Jeffery RW, et al. Monitoring dietary change in a low-fat diet intervention study: advantages of using 24-hour dietary recalls vs food records. J Am Diet Assoc. 1996;96(6):574–579. doi: 10.1016/S0002-8223(96)00158-7. [DOI] [PubMed] [Google Scholar]
- 18.Rebro SM, Patterson RE, Kristal AR, Cheney CL. The effect of keeping food records on eating patterns. J Am Diet Assoc. 1998;98(10):1163–1165. doi: 10.1016/S0002-8223(98)00269-7. [DOI] [PubMed] [Google Scholar]
- 19.Vuckovic N, Ritenbaugh C, Taren DL, Tobar M. A qualitative study of participants' experiences with dietary assessment. J Am Diet Assoc. 2000;100(9):1023–1028. doi: 10.1016/S0002-8223(00)00301-1. [DOI] [PubMed] [Google Scholar]
- 20.Gersovitz M, Madden JP, Smiciklas-Wright H. Validity of the 24-hr dietary recall and seven-day record for group comparisons. J Am Diet Assoc. 1978;73(1):48–55. [PubMed] [Google Scholar]
- 21.Andersen LF, Pollestad ML, Jacobs DR, Jr, Lovo A, Hustvedt BE. Validation of a pre-coded food diary used among 13-year-olds: comparison of energy intake with energy expenditure. Public Health Nutr. 2005;8(8):1315–1321. doi: 10.1079/phn2005751. [DOI] [PubMed] [Google Scholar]
- 22.Axelson JM, Csernus MM. Reliability and validity of a food frequency checklist. J Am Diet Assoc. 1983;83(2):152–155. [PubMed] [Google Scholar]
- 23.Haraldsdottir J, Thorsdottir I, de Almeida MD, et al. Validity and reproducibility of a precoded questionnaire to assess fruit and vegetable intake in European 11- to 12-year-old schoolchildren. Ann Nutr Metab. 2005;49(4):221–227. doi: 10.1159/000087276. [DOI] [PubMed] [Google Scholar]
- 24.Johnson F, Wardle J, Griffith J. The Adolescent Food Habits Checklist: reliability and validity of a measure of healthy eating behaviour in adolescents. Eur J Clin Nutr. 2002;56(7):644–649. doi: 10.1038/sj.ejcn.1601371. [DOI] [PubMed] [Google Scholar]
- 25.Kristal AR, Abrams BF, Thornquist MD, et al. Development and validation of a food use checklist for evaluation of community nutrition interventions. Am J Public Health. 1990;80(11):1318–1322. doi: 10.2105/ajph.80.11.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lillegaard IT, Loken EB, Andersen LF. Relative validation of a pre-coded food diary among children, under-reporting varies with reporting day and time of the day. Eur J Clin Nutr. 2007;61(1):61–68. doi: 10.1038/sj.ejcn.1602487. [DOI] [PubMed] [Google Scholar]
- 27.Lillegaard IT, Andersen LF. Validation of a pre-coded food diary with energy expenditure, comparison of under-reporters v. acceptable reporters. Br J Nutr. 2005;94(6):998–1003. doi: 10.1079/bjn20051587. [DOI] [PubMed] [Google Scholar]
- 28.Smith KW, Hoelscher DM, Lytle LA, et al. Reliability and validity of the Child and Adolescent Trial for Cardiovascular Health (CATCH) Food Checklist: a self-report instrument to measure fat and sodium intake by middle school students. J Am Diet Assoc. 2001;101(6):635–647. doi: 10.1016/S0002-8223(01)00161-4. [DOI] [PubMed] [Google Scholar]
- 29.Thompson FE, Subar AF, Brown CC, et al. Cognitive research enhances accuracy of food frequency questionnaire reports: results of an experimental validation study. J Am Diet Assoc. 2002;102(2):212–225. doi: 10.1016/s0002-8223(02)90050-7. [DOI] [PubMed] [Google Scholar]
- 30.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol. 2001;154(12):1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 31.Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 32.Freedman LS, Guenther PM, Krebs-Smith SM, Dodd KW, Midthune D. A population's distribution of Healthy Eating Index-2005 component scores can be estimated when more than one 24-hour recall is available. J Nutr. 2010;140(8):1529–1534. doi: 10.3945/jn.110.124594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lafay L, Mennen L, Basdevant A, et al. Does energy intake underreporting involve all kinds of food or only specific food items? Results from the Fleurbaix Laventie Ville Sante (FLVS) study. Int J Obes Relat Metab Disord. 2000;24(11):1500–1506. doi: 10.1038/sj.ijo.0801392. [DOI] [PubMed] [Google Scholar]
- 34.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 35.Arab L, Wesseling-Perry K, Jardack P, Henry J, Winter A. Eight self-administered 24-hour dietary recalls using the Internet are feasible in African Americans and Whites: the Energetics study. J Am Diet Assoc. 2010;110(6):857–864. doi: 10.1016/j.jada.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]