Abstract
Background: Sub-Saharan Africa has a disproportionate burden of disease and an extreme shortage of health workers. There are already too few doctors to train doctors in specialities and sub-specialties. E-health is seen as a possible solution through distance education, telemedicine, and computerized health information systems but there are few people trained in e-health. We describe 12 years of experience at the University of KwaZulu-Natal (UKZ-N) in education and training in postgraduate medical disciplines, medical informatics, and telemedicine. Medical Education: Videoconferencing of seminars and grand rounds to regional training hospitals commenced in 2001 and has grown to 40 h of interactive conferencing taking place weekly during academic terms involving over 33,000 participants in 2010. Videoconferenced sessions are directly recorded to DVD and DVDs are sent to other medical schools in Africa that do not have the infrastructure to directly connect. E-health Education: Students and academic staff were initially sent to the United States for training in medical informatics and workshops were held in South Africa for people from sub-Saharan Africa. This led to the development of postgraduate academic programs in medical informatics and telemedicine at UKZ-N. African students were then brought to UKZ-N for training. The model was changed from UKZ-N to students and staff based at their home universities with the aim of building capacity in the staff at partner institutions so that they can in time offer their own e-health academic programs. Conclusions: The need for capacity development in all aspects of e-health in sub-Saharan Africa is great and innovative solutions are required.
Introduction
Sub-Saharan Africa faces many problems. Its countries are poor, infrastructure is limited, the burden of disease is disproportionately high, and there is an extreme shortage of health workers.1 E-health has been proposed as a potential solution to some of the health problems.2 This requires connectivity which is expensive and limited.3 The digital divide is a term that is no longer in vogue but the divide is still there and a new digital health divide is emerging.
Adding to Africa's woes is its rapidly growing population which will double in the next 40 years, despite HIV, TB, Malaria, droughts, and conflict.4 Its medical schools cannot produce and retain sufficient doctors to serve its people. Already the number of doctors per 100,000 people is falling in some countries.5 Specialists tend to live in large cities adding geographical inequity to healthcare provision. Some countries have no specialists in certain disciplines and many medical schools have no staff in subspecialties. Pediatric surgery is an example. It is estimated that outside Nigeria and South Africa there are only 50 pediatric surgeons serving 46 countries.6 So who teaches doctors in specialist surgical training and medical students about pediatric surgery in the 110 medical schools outside Nigeria and South Africa?
Telemedicine has the potential to improve access to higher levels of health professionals, but both synchronous and asynchronous telemedicine add work to already overburdened health professionals at both the send and receive sites. International cross border telemedicine is a logical solution but raises legal, licensure, and remunerative issues. Philanthropic telemedicine services like the Swinfen Charitable Trust, where legislation, licensure, and remuneration are not barriers, have been poorly utilized by African physicians.7 A number of possible reasons for this have been proposed.7,8
Until recently there has been little political will within sub-Saharan Africa to embrace e-health. This is beginning to change with the African Union now talking of working toward harmonizing telemedicine and e-health in Africa. The reality is however that few countries have e-health policies or strategies.9 Widespread poverty leaves governments with small budgets and health budgets must be spent prudently. There is limited evidence of the economic benefits of e-health from the developed world and even less from the developing world. So governments must ask the question, if e-health is a solution which aspect of e-health will provide the most value for the limited budget? Will it be a partially or completely computerized District Health Information System, improved supply chain management, hospital information systems, an electronic medical record, or telemedicine?
Whatever the answer, there are insufficient trained people to support and implement the solution. Government, donor and vendor driven implementation of telemedicine and health informatics initiatives in sub-Saharan Africa will increase but their sustainability will be largely dependent on a skilled workforce to implement, use, support, and maintain these programs. This will require the development of human capacity across all sectors of e-health. Who will do this and is there the capacity within African Universities to meet the demand?
The aim of this paper is to describe a 12 years experience in KwaZulu-Natal (KZ-N), South Africa using different forms of tele-education and e-learning to develop capacity in the health sector in South Africa and Africa and the evolution of a model of developing the capacity to develop capacity.
Setting
KZ-N is a province on the Eastern seaboard of South Africa. It is approximately 98,000 km2 in area, with a population of about 10.6 million people, of whom 84% are dependent on the public health sector for medical services and 54% live in rural areas. In the public health sector there are 33 doctors per 100,000 people and six medical specialists per 100,000 people. There is a high prevalence of HIV in the province, and 39.5% of women attending antenatal clinics are HIV positive.10
KZ-N has 67 public sector hospitals and one medical school, the Nelson R Mandela School of Medicine (NRMSM), situated in Durban, the largest seaport in Africa. The school has approximately 1,100 undergraduate medical students and 500 doctors undergoing postgraduate medical training to become specialists in different fields. Postgraduate training is decentralized with students based at 10 hospitals in the province, the furthest of which is some 285 km from the medical school. There is a shortage of skilled medical clinicians to teach medical specialties at peripheral hospitals.
The NRMSM formed an academic department of telehealth in mid 2002, tasked with establishing and running postgraduate academic programs in both Medical Informatics and Telemedicine, facilitating e-learning within the medical school, assisting the KZ-N Department of Health (DOH) in establishing and running telemedicine programs and conducting international outreach through e-health. It is unique in Africa.
Videoconferencing for Medical Education
Infrastructure
In 1999, as part of a National Telemedicine Project, videoconferencing equipment was provided for synchronous point to point teleophthalmology and antenatal tele-ultrasonography projects. This linked 11 hospitals using leased integrated services digital network (ISDN) connections at 256 kbps. Internet protocol (IP)-based videoconferencing is not feasible as hospitals are only allocated 128 kbps bandwidth, which serves all hospital activities. The situation has not changed. It is not that bandwidth is unobtainable, but the KZ-N DOH cannot currently afford to purchase more bandwidth.
For various reasons the pilot telemedicine projects failed. In cooperation with the KZ-N DOH it was agreed that the videoconferencing infrastructure could be used by the NRMSM for medical education.11 The number of video conference units in the province has increased over the past 10 years to 41, through external donor funding. The first multipoint control unit (MCU) was introduced in 2004 and seven sites now have MCUs. In the absence of a videoconferencing bridge, on an occasion it has been necessary to “daisy-chain” two or more MCUs within the medical school to provide access to more than five sites at a time.
Only one video-camera is used at each site and no special lighting is provided. The videoconference sessions are saved directly to DVD. The four sites at the medical school and the postgraduate teaching hospital are administered by three people who are responsible for scheduling, record keeping, and maintenance of the equipment at all sites in KZ-N. The venues range from large lecture theatres seating up to 200 people to small meeting rooms or offices, seating 5–10 people.
The ISDN calls are initiated by the peripheral hospitals and their costs are borne by the KZ-N DOH. The Medical School pays for the rental of ISDN lines for its four videoconferencing sites.
Educational Programming
A principle was established at the outset that where possible, academic departments should not have to do any extra work to provide videoconferenced teaching. As most disciplines run weekly postgraduate seminars, grand rounds, journal clubs, and research meetings, participating disciplines have used one or more of their existing programs for videoconferenced teaching to reach their trainees at peripheral hospitals. Participation is not limited to trainees; other staff at these hospitals are free to attend any sessions for continuing medical education (CME). In 2004, a new postgraduate academic program in HIV Management was established, aimed at doctors and senior nursing staff in rural hospitals. This program was the first to be designed and planned to be offered by videoconferencing to participants at four regional hospitals around the province.
Use
After a slow start, tele-education has grown. (Table 1) Its adoption reflects Rodgers' diffusion of technology curve. Average monthly use has reached 4 h a day, 7 days a week throughout the year. Use is cyclical, following the academic calendar, with little activity during the vacation periods of January, July, and December. During academic terms an average of 6 h of teaching is broadcast 7 days a week.
Table 1.
Annual Use of Videoconferenced Tele-Education at the NRMSM
| YEAR | NO. OF ACADEMIC PROGRAMMES | ANNUAL HOURS OF VC | AVERAGE MONTHLY USE (HR) | TOTAL NO. OF PEOPLE PARTICIPATING | TOTAL NO. OF CME POINTS GENERATED | TOTAL NO. OF SITES USED |
|---|---|---|---|---|---|---|
| 2001 | 1 | 98 | 8.2 | 493 | 493 | 2 |
| 2002 | 2 | 117 | 9.8 | 680 | 680 | 4 |
| 2003 | 2 | 119 | 9.9 | 2,495 | 2,495 | 4 |
| 2004 | 4 | 186 | 15.5 | 8,791 | 25,066 | 6 |
| 2005 | 6 | 473 | 39.4 | 15,088 | 58,627 | 12 |
| 2006 | 17 | 765 | 63.8 | 23,125 | 72,308 | 26 |
| 2007 | 30 | 886 | 73.8 | 30,256 | 68,846 | 36 |
| 2008 | 31 | 1,298 | 108.2 | 39,781 | 96,793 | 33 |
| 2009 | 32 | 1,190 | 99.2 | 32,727 | 75,581 | 35 |
| 2010 | 35 | 1,477 | 123.1 | 33,250 | 84,777 | 37 |
VC, videoconference; NRMSM, Nelson R Mandela School of Medicine; CME, continuing medical education.
In total, 60 different videoconferencing sites have participated, 32 in KZ-N, 13 in other Provinces in South Africa, and 15 in other countries, six of which are in Africa (Rwanda, Senegal, Sudan, Mozambique, Morocco, and Egypt). Over the last 6 years there has been a steady annual increase in the number and percentage of participants at peripheral sites, from 39.6% in 2005 to 45.5% in 2010.
The number of academic programs fluctuate as some programs are not annually run.
Assessment
Satisfaction with videoconferenced programs is routinely undertaken using a standardized questionnaire. Review of the HIV Management program showed no differences in the examination and evaluation results between students at each of the distant sites and those who attended lectures face to face. Fewer than 2% of respondents were negative about videoconferencing and their complaints related to the quality of PowerPoint® (Microsoft, Redmond, WA) slides.11
Of 68 people who delivered lectures or seminars by video conference on various programs, only one person felt that videoconferencing was a poor teaching tool, with 85% rating it as good or excellent. In the postgraduate seminar program in surgery, 83% of participants rated videoconferencing as a good or excellent teaching tool, with no one rating it as, poor or bad.11 Recent evaluations of two nursing programs for registered midwives and senior nurses at rural hospitals offered for the first time by videoconferencing found that over 90% of participants would recommend videoconferenced education to a friend and over 95% would attend future videoconferenced teaching.12
Problems were relatively uncommon and most related to sound quality in some venues and dissatisfaction with the visual quality of transmitted PowerPoint slides containing too many lines of text in a small font or using inappropriate color contrasts. The absence of site coordinators or local technical support resulted in some missed sessions due to malfunctioning equipment, usually following electrical storms or power outages and reconnecting after a dropped call caused problems to some new users. Fewer than 1% of teaching sessions have had to be cancelled because of failure to make a connection.
Alternatives to Videoconferencing
DVD Recordings
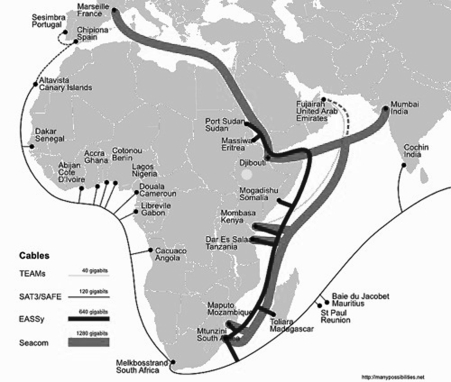
After participating in local videoconferenced teaching sessions, visiting colleagues from sub-Saharan Africa have requested to link their medical schools to NRMSM by videoconferencing. All see this as a means of providing teaching in subspecialties and helping to overcome their shortages of academic staff. Few medical schools in sub-Saharan Africa currently have the infrastructure or bandwidth to participate in videoconferencing. This is likely to change as new undersea cables bringing bandwidth to Africa from Europe, the United Arab Emirates, and India come on line. The current undersea cables providing bandwidth to Africa are shown in Figure 1.
Fig. 1.
Current undersea cables providing bandwidth to sub-Saharan Africa (Teams, SAT-3/SAFE, EASSy, and SEACOM).
As videoconference-based teaching sessions are routinely recorded to DVD, a simple, albeit asynchronous solution has been to record several seminar sessions to DVD and mail them to interested medical schools. A pilot project of sending DVD recordings in pediatric surgery to four medical schools in Central and East Africa has recently been reported.6 All sites have incorporated the DVD seminars into their own postgraduate general surgical training programs, pediatric surgical programs where available, and into their undergraduate medical training. The content and the quality of the DVD recordings have been considered acceptable by local faculty and users. Three more medical schools have requested and joined this program. Over 250 people, undergraduate students, surgical trainees, and faculty are exposed to the DVDs. The shortcoming is that the sessions are not interactive. It was initially planned to link to the various medical schools by Skype® (Skype Limited, Luxembourg City, Luxembourg) for interactive discussion immediately after their use of a DVD seminar but this has proved too onerous for the local staff. All centers have expressed the desire to synchronously link by videoconference when they have the necessary infrastructure.
One of the weaknesses of the DVD recordings is that the images have passed through the coder/decoder technology (CODEC) of the videoconferencing unit. The text of PowerPoint presentations is always slightly blurred. To overcome this, a trial is underway using commercial software AuthorPoint® (AuthorGen, Chandigarh, India). This allows synchronization of audio and video input to produce a PowerPoint-like presentation with a “talking head”. A feature of the software is the option of linking the Web uniform resource locators or documents to individual slides. This then allows for additional material to be included on a DVD. The recording can also be sharable content object reference model compliant for use with learning management systems on a local server. The process however requires a separate video and audio feed necessitating the presence of a technician to start the software program and the video recording. Initial results are promising and these recordings have been mailed out on DVDs to collaborating African medical schools and are being assessed.
Learning Management Systems
Six academic programs use a free open source learning management system Moodle, in addition to videoconferencing. Moodle allows educators to create online dynamic Web sites and is used as a repository of learning materials, a forum for topic discussions using online synchronous and asynchronous chat, a secure site for the submission of assignments and for student administration. Two of the nursing programs have found that student use of the learning management system has been less than anticipated because nurses have not been able to access computers at their hospitals during working hours for their educational requirements and few have computers at home. A recent unpublished survey of 207 rural and urban nurses in KZ-N has found that 72 nurses did not have access to a computer at home and 56 could not access a computer at work. Nineteen of 83 nurses working solely in the public sector had no access to a computer either at work or at home. Nurses also report that computers are often available only in the offices of senior staff and are largely inaccessible during working hours.
E-Health Capacity Development
The Department of Telehealth at the NRMSM operates postgraduate coursework programs at Postgraduate Diploma and Masters level in both Telemedicine and Medical Informatics. Students are locally based, in other Provinces in South Africa and in African countries. Desktop videoconferencing at lower bandwidths was seen as a possible solution for synchronous videoconferenced teaching. A free and open source desktop videoconferencing program DimDim® (Salesforce.com, San Francisco, CA) which can be integrated into an open source learning management system, Moodle® was evaluated. The program utilized a server in India with a resultant unacceptable latency of 3–4 s. Installation of the software on a local server reduced the latency but some of the additional features like desktop sharing and the use of a white board were unstable.
An alternative solution has been to use Polycom PVX® software (Polycom, Pleasanton, CA). This has worked well with Asynchronous Digital Subscriber Line connectivity and with rapid deployment of mobile telephony infrastructure this solution effectively works with 3G connectivity. In African countries dependent on satellite links for international Internet connectivity, bandwidth availability is irregular and it is often necessary to fall back to voice only transmission using Skype®. Teaching sessions are regularly undertaken with students linking using different forms of connectivity by ISDN-based videoconferencing, IP or 3G based desktop videoconferencing or Skype®. This requires judicious positioning of microphones and speakers at the host site, so that the participants on Skype® can hear the videoconferenced proceedings and vice versa. If PowerPoint® presentations are used, they are e-mailed to participants likely to connect by Skype®. Connectivity costs in many countries are related to volume of data downloaded. To reduce the size of e-mailed files, PowerPoint® presentations are saved in handout format of six slides per page in Adobe pdf format. The new multipoint Skype® videoconferencing software will provide better capability.
Building the Capacity to Build Capacity: A New Model
Since 1998, University of KwaZulu-Natal (UKZ-N), has with various partners received three Fogarty International Center Training Grants in the International Training for Global Health (ITGH) program which aims to develop medical informatics capacity in sub-Saharan Africa. Based on experience gained, three different models have been used. Initially the standard “U.S. model” was used: students and staff were sent to the U.S. for postgraduate training and short courses. Over 100 people from different African countries were brought to South Africa for workshops or to complete Bachelor degrees not available in their home country. The return on investment was limited as people returned to environments that were not supportive of medical informatics, there were few job opportunities and the model was unsustainable without donor funding. As a planned legacy of the first grant, local postgraduate programs were developed in medical informatics at the NRSM.
In the second cycle of funding the model was changed to a “South African model.” Students from several African countries were brought to Durban to study medical informatics fulltime for a year with local students. This proved to be a less expensive solution but was still unsustainable in the absence of donor funding. In addition, it took people who were already involved in medical informatics projects away from their jobs and families. The project was also designed to build teaching capacity in medical informatics at the NRSM and collaborative medical informatics teaching programs were developed with the local university department of Information Systems and Technology. This has resulted in a regular supply of local students to the medical informatics program. Demand for places on the medical informatics program from South African students remains relatively low as informatics is not yet seen as a career path with salaries equivalent to the computer industry.
Based on experience in teaching various courses by interactive distance learning a new “African model” was proposed and is being implemented within the ITGH training program.
The model is developed around the principle of not moving the students but moving the teaching to academic institutions in their home countries while at the same time developing capacity of staff in the foreign institutions to teach medical informatics. The existing medical informatics graduate programs at UKZ-N are being shared with four other Universities in Uganda, Mozambique, Zimbabwe, and South Africa. Students interactively take their courses from UKZ-N by videoconferenced e-learning in the first instance. Staff at the receiving institutions act as mentors and are also taking the courses to develop their own capacity. It is envisioned that in time, teaching will ultimately be shared between participating institutions, curricula will be shared, and partner institutions will develop sufficient in house capacity to offer medical informatics programs and short courses or training relevant to local need. This is the concept of “building the capacity to build capacity”.
It is hoped that these centers can over time be nurtured to become regional centers of excellence in e-health and act as regional hubs providing e-learning in a range of fields in their regions. A proposal has been made to run a similar graduate training project in telemedicine between UKZ-N and a university in Nigeria.
Discussion
Sub-Saharan Africa's health-related problems are challenging. It is estimated that an additional 820,000 health workers are required to meet a minimum requirement of 23 health professionals per 100,000 people.1 The shortage of doctors extends to a shortage of medical educators. Faced with rapid population growth, it is unlikely that the 168 sub-Saharan African medical schools will be able to keep pace with population growth. The aging population and zero or negative population growth in many developed world countries will lead to a further exodus of doctors from Africa. E-health and international cross border telemedicine is becoming imperative.
Within the constraints of bandwidth, cost, and power, e-learning has been used to provide distributed teaching in the healthcare sector in Africa using appropriate solutions. E-learning opportunities have been well received by students and practitioners. The model of collaborative teaching offers a means of developing capacity in both medicine and e-health in Africa and of fast tracking the development of sustainable academic departments offering e-health programmes. The model can be extended from formal education to needs specific training and shared research endeavors.
Telemedicine implementation in sub-Saharan Africa has been poor but tele-education activities, although limited, have proved more successful and sustainable. The Resau Afrique Francophone de Telemedicine (RAFT) project provides 2 h of Web cast continuing medical education weekly, at low bandwidth, to a network of Francophone participants in up to 15 West African countries.13 The African Medical and Research Foundation (AMREF) is involved in a program to improve the qualifications of nurses in Kenya through a mix of face to face sessions and self paced e-learning.14 The Institute for Tropical Medicine provides ongoing education in HIV management.15 The lack of professional interaction and support has been identified as a reason for doctors leaving rural areas. When available, doctors in isolated areas welcome interactive continuing education. In Africa it appears that this also extends to doctors in urban areas who have limited opportunities for continuing medical education.
Capacity development across the full spectrum of e-health activities is vital to the future sustainability of e-health in Africa.
Acknowledgments
Aspects of this work were and are funded by Fogarty International Centre Training Grant for ITGH: Grant Number 5D43TW007004.
Disclosure Statement
No competing financial interests exist.
References
- 1.World Health Organization. World health report 2006: Working together for health. Geneva: WHO Press; 2006. pp. 1–209. [Google Scholar]
- 2.World Health Organization. Building foundations for eHealth. Report of the WHO global observatory for eHealth. Geneva: WHO Press; 2006. pp. 1–327. [Google Scholar]
- 3.International Telecommunications Union. Measuring the information society. Geneva: ITU; 2010. 2010. pp. 1–108. [Google Scholar]
- 4.United Nations DoE, Social Affairs PD. World population prospects. The 2008 revision highlights. New York: United Nations; 2009. pp. 1–89. [Google Scholar]
- 5.World Health Organization. World health statistics 2010. Geneva: WHO Press; 2010. pp. 1–177. [Google Scholar]
- 6.Hadley GP. Mars M. e-Education in paediatric surgery: A role for recorded seminars in areas of low bandwidth in sub-Saharan Africa. Pediatr Surg Int. 2011;27:407–410. doi: 10.1007/s00383-010-2806-z. [DOI] [PubMed] [Google Scholar]
- 7.Wootton R. Telemedicine support for the developing world. J Telemed Telecare. 2008;14:109–114. doi: 10.1258/jtt.2008.003001. [DOI] [PubMed] [Google Scholar]
- 8.Mars M. Health capacity development through telemedicine in Africa. IMIA YearB Med Inform. 2010:87–93. [PubMed] [Google Scholar]
- 9.Mars M. Scott RE. Global e-health policy: A work in progress. Health Aff (Millwood) 2010;29:1–8. doi: 10.1377/hlthaff.2009.0945. [DOI] [PubMed] [Google Scholar]
- 10.Health Systems Trust Health Systems Trust—Health Statistics. 2011. www.hst.org.za/recently-updated-indicators. [Nov 5;2011 ]. www.hst.org.za/recently-updated-indicators
- 11.Mars M. Telemedicine in KwaZulu-Natal, South Africa: From failure to cautious optimism. J Telemed Telecare. 2007;13:57–59. [Google Scholar]
- 12.Chipps J. Mars M. Durban: IIMC International Information Management Corporation; 2010. [Nov 5;2011 ]. Technology enhanced learning for remote nurses in KwaZulu-Natal, in IST-Africa 2010. [Google Scholar]
- 13.RAFT. 2010. http://raft.hcuge.ch/ [Nov 5;2011 ]. http://raft.hcuge.ch/
- 14.AMREF E-Learning programme. 2011. www.amref.org/info-centre/amref-courses—training-programmes/elearning-programme-/ [Jul 15;2011 ]. www.amref.org/info-centre/amref-courses—training-programmes/elearning-programme-/
- 15.Zolfo M. Arnould L. Huyst V. Lynen L. Telemedicine for HIV/AIDS Care in Low Resource Settings. Stud Health Technol Inform. 2005;114:18–22. [PubMed] [Google Scholar]