Abstract
Background
Laparoscopic totally extraperitoneal (TEP) repair has been accepted as a popular procedure for inguinal hernia repair, but surgeons still encounter technical difficulties owing to unfamiliar pelvic anatomy and limited working space. We sought to estimate the learning curve for laparoscopic TEP repair without supervision.
Methods
We retrospectively analyzed the medical records of patients scheduled for laparoscopic TEP repair of an inguinal hernia from December 2000 to October 2007.
Results
We reviewed medical records for 700 patients. The cases were divided into 8 groups: 20 patients each in groups I–V and 200 patients each in groups VI–VIII. No significant difference in demographic characteristics was identified among the groups. The mean duration of surgery significantly decreased (p < 0.001) in relation to experience; it reached a plateau of less than 30 minutes (mean 28 min) after 60 cases. The mean length of stay in hospital was 0.97 days, reaching a plateau after 20 cases. Six patients were converted to other techniques: 1 patient each in groups III and VIII and 4 patients in group VII. Three recurrences were detected; however, 2 were excluded because the patient had bilateral inguinal hernias.
Conclusion
We estimate the learning curve for laparoscopic TEP repair is 60 cases for a beginner surgeon. The presence of an experienced supervisor during the first 60 cases can help prevent unnecessary complications and shorten the duration of surgery.
Abstract
Contexte
La réparation par laparoscopie totalement extrapéritonéale (TEP) est populaire pour réparer une hernie inguinale, mais les chirurgiens font toujours face à des difficultés techniques à cause de l’anatomie pelvienne mal connue et de l’espace de travail limité. Nous avons cherché à évaluer la courbe d’apprentissage de la réparation par laparoscopie TEP sans supervision.
Méthodes
Nous avons analysé rétrospectivement les dossiers médicaux des patients qui devaient subir la réparation d’une hernie inguinale par laparoscopie TEP de décembre 2000 à octobre 2007.
Résultats
Nous avons étudié les dossiers médicaux de 700 patients. Les cas ont été répartis en 8 groupes : 20 patients dans chacun des groupes I à V et 200 dans chacun des groupes VI à VIII. Il n’y avait aucune différence significative entre les groupes quant aux caractéristiques démographiques. La durée moyenne de l’intervention chirurgicale a diminué considérablement (p < 0,001) en fonction de l’expérience : elle s’est stabilisée à moins de 30 minutes (moyenne de 28 minutes) après 60 cas. La durée moyenne du séjour à l’hôpital s’est établie à 0,97 jours et s’est stabilisée après 20 cas. On a changé de technique dans le cas de 6 patients : 1 patient chacun des groupes III et VIII et 4 patients du groupe IV. On a repéré 3 récidives, mais 2 ont été exclues parce que le patient avait une hernie inguinale bilatérale.
Conclusion
Nous estimons à 60 cas pour le chirurgien débutant la courbe d’apprentissage de la réparation par laparoscopie TEP. La présence d’un superviseur chevronné au cours des 60 premiers cas peut aider à éviter les complications inutiles et raccourcir la durée de l’intervention chirurgicale.
Laparoscopic repair is widely used to treat inguinal hernias. Laparoscopic totally extraperitoneal (TEP) repair is favoured since the preperitoneal approach is considered more appropriate for dealing with abdominal wall problems. Laparoscopic TEP repair gains access to the preperitoneum without the associated pain and morbidity of a large incision, and it potentially allows for a more rapid recovery.1–4 Nevertheless, many surgeons are concerned about laparoscopic TEP repair since it is difficult to learn the unfamiliar pelvic anatomy and, compared with that of other techniques, the working space is limited.
Some studies have reported on the learning curve for laparoscopic TEP repair;5–8 one suggested a learning curve of 80 cases,6 and another suggested 20–50 cases.7 Lal and colleagues8 recommended that a minimum of 10 independent open Stoppa preperitoneal procedures might be helpful to learn how to perform laparoscopic TEP repair. The aim of the present study was to estimate the learning curve of a single inexperienced surgeon (K.Y.H.) performing laparoscopic TEP repair without any supervision.
Methods
We performed a retrospective analysis of the medical records of patients scheduled for laparoscopic TEP repair for unilateral inguinal hernia from December 2000 to October 2007. The outcome measurements included the demographic characteristics and the postoperative results of patients.
Surgical technique
Laparoscopic TEP repair was performed using the 3-port technique. To create the preperitoneal space, a 12-mm skin incision was made at the inferior edge of the umbilicus, and it was carried down to the anterior rectus sheath. Then a small incision was made on the anterior rectus sheath, exposing the rectus abdominal muscle. A channel between the rectus muscle and the posterior rectus sheath was created by blunt dissection with blunt endopeanuts (Tyco Healthcare) aiming toward the pubic symphysis. A small tunnel was made in the direction of the pubis between the rectus abdominal muscle and the peritoneum. A preperitoneal space was attained using a 45° telescope and 12 mm Hg of CO2 gas pressure. Two 5-mm working ports were made, one 2 cm above the pubic symphysis and the other half-way between the 2 previous ports. After reduction of the hernia sac and parietalization of the spermatic cord, a 13 × 8–cm Surgipro mesh (Covidien) was placed at the hernia site.
The duration of surgery was considered to be the time from skin incision to skin closure. A complex hernia was defined as any 2 or more types of hernias combined at 1 location. The length of stay in hospital was defined as the total number of nights spent in hospital after the operation. Seroma was defined as the presence of a palpable fluid collection over the operation site or scrotum during follow-up. After the operation, the patients who needed more than 2 doses of analgesics for operative site pain were recorded. Most patients were discharged from hospital the day after the operation. The patients were followed up regularly at the outpatient hernia clinic. We attempted to contact patients lost to follow-up by telephone, but if we were unable to reach them, we used the last recorded follow-up data for our analysis.
Statistical analysis
We compared the demographic characteristics and postoperative data using the χ2 test and independent Student t tests. Continuous data were reported as means (and standard deviations [SD]). All the data collected in the database were analyzed using SPSS version 12.0. We considered results to be significant at p < 0.05.
Results
A single surgeon performed 809 laparoscopic TEP repairs. We excluded 109 because they were bilateral hernias; therefore 700 laparoscopic TEP repairs were included in our analysis. Patients were divided into 8 groups: 20 patients each in groups I–V and 200 patients each in groups VI–VIII.
The follow-up period was 2–58 months (mean 39 mo). The mean age of patients was 46.6 (SD 16.9) years. There were 637 men and 63 women. There were 424 cases of right inguinal hernia and 276 cases of left inguinal hernia. The types of hernia were as follows: 555 indirect, 108 direct, 3 femoral and 34 complex hernias. Table 1 shows the demographic characteristics of patients and types of hernias for each group.
Table 1.
Demographic characteristics and types of hernias, by patient group
| Characteristic | Group | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | ||
| Mean age, yr | 46.75 | 56.65 | 52.25 | 48.70 | 44.80 | 45.98 | 44.79 | 47.46 | 0.06 |
| Male:female ratio | 18:2 | 19:1 | 19:1 | 19:1 | 17:3 | 189:11 | 178:22 | 178:22 | 0.10 |
| Left:right ratio | 5:15 | 8:12 | 8:12 | 9:11 | 8:12 | 81:119 | 76:124 | 81:119 | 0.30 |
| Hernia type, no. | 0.06 | ||||||||
| Indirect | 19 | 20 | 14 | 17 | 17 | 152 | 156 | 160 | |
| Direct | 1 | 0 | 6 | 3 | 2 | 36 | 32 | 28 | |
| Femoral | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | |
| Complex | 0 | 0 | 0 | 0 | 1 | 12 | 10 | 11 | |
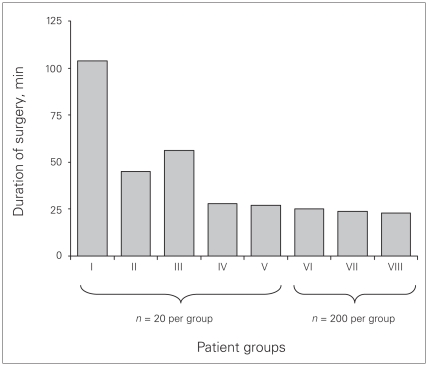
Figure 1 shows the significant differences among each group for the mean duration of surgery (p < 0.001); the mean duration of surgery was 27.97 (SD 22.25) minutes, and after 60 cases of laparoscopic TEP repair, duration of surgery reached a plateau of less than 30 minutes (mean 28 min). Six operations were converted to a Lichtenstein procedure: 1 patient each in groups III and VIII and 4 patients in group VII. The reasons for conversion were as follows: 1 owing to bladder injury, 1 to peritoneal tearing and 4 to a previous operation scar for prostate cancer.
Fig. 1.
Comparison of mean duration of surgery in each group.
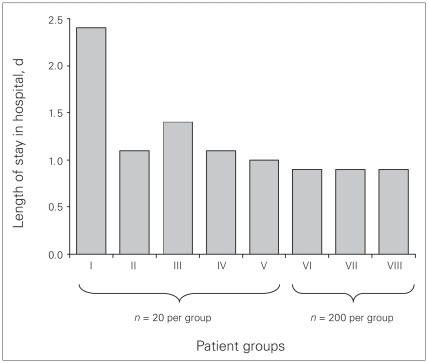
The overall mean length of stay in hospital was 0.97 (SD 0.79) days, and the mean length of stay when individual groups were considered was close to 1 day except for group I, which was closer to 2.5 days (Fig. 2). There were 77 cases (11%) of postoperative pain and 51 cases (7.3%) of postoperative seroma. There were 3 cases (0.4%) of recurrence; however, 2 cases were excluded since the patients had bilateral hernias. One case of recurrence was detected in group VIII.
Fig. 2.
Comparison of mean length of stay in hospital in each group.
Discussion
Numerous reports have suggested that laparoscopic TEP repair is safe and effective for treating inguinal hernias, and the advantages over open repair are less pain, better cosmesis and quicker recovery.1–3 Yet, many surgeons hesitate to perform laparoscopic TEP repair since the pelvic anatomy is unfamiliar and the working space is narrow. Moreover, the learning curve for laparoscopic TEP repair is steep, and the technique is difficult.9
Lal and colleagues8 suggested that any laparoscopic procedure should be a copy of the basic open procedure, with modifications of the technique where applicable, and that 10 or more cases of open Stoppa preperitoneal procedures might be helpful to train for laparoscopic TEP repair. On the other hand, Haidenberg and colleagues7 suggested that laparoscopic TEP repair is simple, straightforward, logical and conceptually easier to teach than the modified Bassini, Lichtenstein or the mesh-plug techniques. Edwards and Bailey9 reported that the factors that may influence the learning curve include the surgeon’s experience with laparoscopic procedures, sound knowledge of the pelvic anatomy and the ability to use a 2-handed technique. In our study, the surgeon did not have any experience with open Stoppa procedures, but he had considerable experience with other laparoscopic procedures, such as laparoscopic cholecystectomy. He also had previously observed laparoscopic TEP repair, and he performed the procedure successfully without supervision.
Even though the exact definition of the learning curve is unclear, it has been defined previously as the number of operations required for the stabilization of the duration of surgery and complication rates.10 Liem and colleagues5 examined the learning experience of 4 different surgeons, each having performed 30 consecutive laparoscopic TEP repairs; however, no conclusions were drawn on the exact duration of the learning curve for the procedure. Lau and colleagues6 suggested that the learning curve for laparoscopic TEP repair was 80 procedures, and Aeberhard and colleagues11 reported that the duration of surgery dropped significantly to less than 1 hour after performing 100 repairs. In our study, the duration of surgery stabilized after 60 cases.
Six operations (0.8%) were converted to a Lichtenstein procedure. Bladder injury occurred in 1 patient in group III, which was primarily repaired with a combined Lichtenstein procedure. For 1 patient in group VII, the reason for conversion was loss of the extraperitoneal space after peritoneal tearing. In the other patients, the reasons for conversion were previous prostate cancer operation in 2 patients, 3 previous Pfannenstiel incisions in 1 patient and 4 previous lower abdominal incisions in 1 patient. When excluding the patients with a history of abdominal surgery, only 2 patients required conversion.
There was 1 postoperative recurrence out of 700 cases of laparoscopic TEP repair in our study. The patient had a history of contralateral laparoscopic TEP repair and 3 recurrences of ipsilateral inguinal hernia. The recurrence was owing to the improper placement of mesh because of severe adhesion.
Limitations
The limitations of this study include the lack of specific information about postoperative pain and seroma. Since postoperative pain and seroma were not described in detail in the medical records, it was difficult to objectively evaluate the complication rates in terms of the postoperative pain and seroma.
Conclusion
According to our study, the learning curve for laparoscopic TEP repair is 60 cases. The conversion rates and recurrence rates were acceptably low. The presence of an experienced supervisor could be helpful to prevent unnecessary complications and to shorten the duration of surgery.
Footnotes
Competing interests: None declared.
Contributors: All authors contributed to study design, data acquisition and analysis, wrote and reviewed the article and approved its publication.
References
- 1.Chung RS, Rowland DY. Meta-analyses of randomized controlled trials of laparoscopic vs conventional inguinal hernia repairs. Surg Endosc. 1999;13:689–94. doi: 10.1007/s004649901074. [DOI] [PubMed] [Google Scholar]
- 2.Heikkinen TJ, Haukipuro K, Koivukangus P, et al. A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc. 1998;8:338–44. [PubMed] [Google Scholar]
- 3.Liem MS, van der Graaf Y, van Steensel CJ, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med. 1997;336:1541–7. doi: 10.1056/NEJM199705293362201. [DOI] [PubMed] [Google Scholar]
- 4.Smith CD. Laparoscopic totally extraperitoneal inguinal hernia repair. Oper Tech Gen Surg. 1999;1:185–96. [Google Scholar]
- 5.Liem MS, van Steensel CJ, Boelhouwer RU, et al. The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg. 1996;171:281–5. doi: 10.1016/S0002-9610(97)89569-4. [DOI] [PubMed] [Google Scholar]
- 6.Lau H, Patil NG, Yuen WK, et al. Learning curve for unilateral endoscopic totally extraperitoneal (TEP) inguinal hernioplasty. Surg Endosc. 2002;16:1724–8. doi: 10.1007/s00464-001-8298-0. [DOI] [PubMed] [Google Scholar]
- 7.Haidenberg J, Kendrick ML, Meile T, et al. Totally extraperitoneal (TEP) approach for inguinal hernia: the favorable learning curve for trainees. Curr Surg. 2003;60:65–8. doi: 10.1016/S0149-7944(02)00657-8. [DOI] [PubMed] [Google Scholar]
- 8.Lal P, Kajla RK, Chander J, et al. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair: overcoming the learning curve. Surg Endosc. 2004;18:642–5. doi: 10.1007/s00464-002-8649-5. [DOI] [PubMed] [Google Scholar]
- 9.Edwards CC, II, Bailey RW. Laparoscopic hernia repair: the learning curve. Surg Laparosc Endosc Percutan Tech. 2000;10:149–53. doi: 10.1097/00019509-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Voitk AJ. The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg. 1998;41:446–50. [PMC free article] [PubMed] [Google Scholar]
- 11.Aeberhard P, Klaiber C, Meyenberg A, et al. Prospective audit of laparoscopic totally extraperitoneal inguinal hernia repair: a multi-center study of the Swiss Association for Laparoscopic and Thoracoscopic Surgery (SALTC) Surg Endosc. 1999;13:1115–20. doi: 10.1007/s004649901185. [DOI] [PubMed] [Google Scholar]