Abstract
Background
Gastroesophageal reflux disease (GERD) is a prevalent condition leading to poor quality of life (QOL) in patients with refractory symptoms. Laparoscopic antireflux (LAR) surgery has been shown to improve QOL, and I sought to examine the surgical and QOL outcomes associated with LAR surgery over a 3-year period at a regional hospital.
Methods
Patients were given GERD–health related quality of life (GERD-HRQL) and SF-36 questionnaires preoperatively, at 6 months and at 12 or more months after surgery. I collected data on demographic and clinical characteristics and surgical outcomes.
Results
Of the 342 patients referred for GERD or dysphagia, 26 received LAR surgery during the study period. All 26 patients had symptoms refractory to medications; 19 had atypical symptoms and 8 had some form of chronic pain syndrome (CPS). The mean duration of surgery was 125 minutes. There were no conversions, complications, 30-day readmissions or deaths. Three patients stayed 2 days in hospital and 23 stayed overnight. One patient required esophageal dilation for persistent dysphagia. Two patients resumed medication for recurrent symptoms and 24 remained medication free. There were significant improvements in GERD–HRQL scores in all patients. Patients with CPS had no improvements in SF-36 scores, whereas patients without CPS showed significant improvement.
Conclusion
Excellent surgical outcomes in LAR surgery can be obtained with careful patient selection at a nonacademic regional hospital. Although GERD-HRQL improved in all patients, patients with CPS showed no improvement in general health QOL scores after LAR surgery. Careful patient counselling should be employed when offering LAR surgery to patients with CPS.
Abstract
Contexte
Le reflux gastro-œsophagien pathologique (RGOP) chronique est un problème prévalent qui entraîne une mauvaise qualité de vie (QDV) chez les patients atteints de symptômes réfractaires. Il a été démontré que la laparoscopie antireflux (LAR) améliore la QDV, et j’ai cherché à analyser les résultats chirurgicaux et liés à la QDV associés à une LAR pendant une période de trois ans dans un hôpital régional.
Méthodes
Les patients ont eu à remplir un questionnaire sur le RGOP–qualité de vie liée à la santé (RGOP-QVLS) et SF-36 avant l’intervention, et 6 et 12 mois ou plus après celle-ci. J’ai recueilli des données sur les caractéristiques démographiques et cliniques et sur les résultats chirurgicaux.
Résultats
Des 342 patients référés à cause d’un RGOP ou d’une dysphagie, 26 ont subi une LAR au cours de la période à l’étude. Ces 26 patients présentaient tous des symptômes réfractaires aux médicaments : 19 avaient des symptômes atypiques, et 8 une forme quelconque de syndrome de douleur chronique (SDC). L’intervention chirurgicale a duré en moyenne 125 minutes. Il n’y a pas eu de conversion, de complication, de réhospitalisation à 30 jours ou de décès. Trois patients sont demeurés 2 jours à l’hôpital et 23 y ont passé la nuit. Un patient a dû subir une dilatation œsophagienne à cause d’une dysphagie persistante. Deux patients ont recommencé à prendre des médicaments pour les symptômes récurrents et 24 ont pu se passer de médicaments. On a constaté des améliorations importantes des scores RGOP-QVLS chez tous les patients. Les scores SF-36 ne se sont pas améliorés chez les patients qui avaient un SDC, mais ils se sont améliorés considérablement chez ceux qui n’avaient pas de SDC.
Conclusion
Il est possible d’obtenir d’excellents résultats chirurgicaux d’une LAR en choisissant attentivement les patients dans un hôpital régional non universitaire. Même si les résultats du RGOP-QVLS se sont améliorés chez tous les patients, les scores QDV représentant l’état de santé général ne seront pas améliorés chez les patients qui avaient un SDC après une LAR. Lorsque l’on offre une LAR aux patients qui ont un SDC il faut les conseiller avec prudence.
Gastroesophageal reflux disease (GERD) is a prevalent medical condition for which open or laparoscopic Nissen fundoplication has been shown to be an effective long-term alternative to medical therapy.1–3 Patients with chronic GERD refractory to medical treatment have a poor quality of life (QOL),4 and surgery has been shown to improve QOL in these patients.5–8
The 36-item short-form health survey (SF-36)9 and the GERD–health related quality of life scale (GERD–HRQL)10 have both been validated to quantify generic and disease-specific QOL, respectively, for patients with GERD.5–8 Excellent outcomes for laparoscopic antireflux (LAR) surgery in the community hospital setting have been previously described.11 The objective of this study was to examine the surgical and QOL outcomes of all patients who underwent LAR surgery over a 3-year period at a Canadian regional hospital.
Methods
I prospectively enrolled patients who were referred to me over a period of 3 years (July 2006 to June 2009) for GERD or dysphagia and underwent LAR surgery. I excluded patients who were naïve to antireflux medications and had full symptom control after starting these medications. I also excluded patients who after investigation were found not to have GERD or who had GERD but elected to be treated medically despite being offered surgery. Patients with a body mass index (BMI) greater than 35 were not offered surgery.
I reviewed the results of all investigations with each patient in detail and obtained informed consent from all patients after an in-depth discussion of potential side effects of surgery, particularly dysphagia and gas bloat syndrome. Patients were scheduled for LAR surgery at the Vernon Jubilee Hospital, a regional hospital with a catchment population of about 130 000. Analysis was performed in March 2010.
Patients were given GERD–HRQL and SF-36 questionnaires at the time of scheduling for surgery or on the day of surgery. The GERD–HRQL scale provides a numeric score from 0 to 50, with 50 indicating the worst severity of symptoms. In addition, the questionnaire assesses whether patients are satisfied, neutral or dissatisfied with their present condition. The SF-36 provides an overall score from 0 to 100, with a low score indicating poor health. The domains of the SF-36 that were analyzed in this study were overall scores for mental health and physical health in addition to the overall composite SF-36 score. Patients completed the same questionnaires 6 months postoperatively; the returned questionnaires were scanned and stored electronically. At the conclusion of the study, patients who had undergone surgery 12 or more months previously completed a third set of questionnaires. Patients were asked to score their symptoms on the preoperative questionnaires while on antireflux medications; and for the postoperative questionnaires, patients were asked to score their symptoms off antireflux medications.
Statistical analysis
I recorded data on patient demographic characteristics, clinical parameters, duration of surgery, length of stay in hospital and complications. I used the paired Wilcoxon signed rank test on an Internet-based statistical calculator12 to compare scores on the pre- and postoperative GERD-HRQL and SF-36 questionnaires. Results were considered to be significant at p < 0.05.
Results
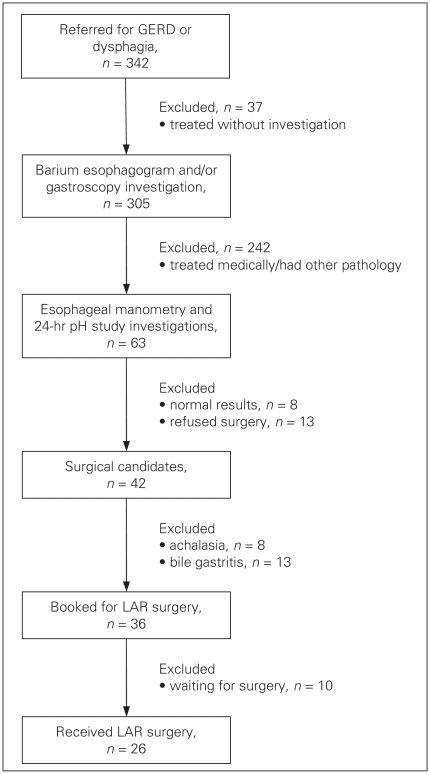
A total of 342 patients were referred during the study period: 273 were referred for GERD and 69 for dysphagia. Of these, 37 were treated medically without further investigation as they were naïve to antireflux medications and had full symptoms control after starting medication. In all, 305 patients were investigated with barium esophagogram and/or gastroscopy. Of these patients, 242 were treated medically or were found to have other pathology, including 7 patients with large paraesophageal hernias treated with open operations. The remaining 63 patients were further investigated with esophageal manometry and 24-hour pH studies (patients had to be referred to Vancouver for these studies at their own expense). After investigation, 8 patients were found not to have GERD and 13 with confirmed GERD elected to be treated medically despite being offered surgery. Of the remaining 42 patients, 5 had achalasia and were treated with open (n = 1) or laparoscopic (n = 4) Heller myotomy, and 1 patient with severe bile reflux post–Bilroth I gastrectomy was converted to a roux-en-Y gastro-jejunostomy. The remaining 36 patients were scheduled for LAR surgery; 10 were waiting for surgery at the time of this study, leaving 26 patients for analysis (Fig. 1).
Fig. 1.
Selection of patients for laparoscopic antireflux (LAR) surgery referred for gastroesophageal reflux disease (GERD) or dysphagia.
Questionnaire compliance was 100% for the preoperative questionnaire (though 1 patient forgot to fill in the SF-36 component). Twenty-three of 24 patients completed the 6-month postoperative questionnaire for a compliance rate of 96%, and 17 of 18 patients completed the questionnaire 12 or more months after surgery for a compliance rate of 94%. One patient did not return the questionnaire at 6 months but did at 12 or more months.
Of the 26 patients who had surgery, the mean age was 50.6 (range 17–79) years, 9 patients were male, the mean American Society of Anesthesiologists (ASA) class was 2.19 and the mean BMI was 27.7 (range 22–35). All patients in this study had reflux symptoms refractory to medical therapy. Nineteen of 26 patients had atypical symptoms such as chest pain, choking, reactive airway disease and coughing. No patients had only atypical symptoms. Eight patients were noted to have some kind of chronic pain syndrome (CPS) identified by a separate office questionnaire or through medical history. One had nonvascular leg pain, 2 had noncardiac chest pain, 1 had arthritis, 2 had vague abdominal pain, 1 had neck pain and 1 had fibromyalgia with multiple sites of pain. Six of these 8 patients had atypical reflux symptoms.
All patients were investigated with gastroscopy, barium esophagogram, esophageal manometry and pH studies. One patient could not tolerate the manometry catheter but had pathologically confirmed esophagitis so was offered surgery on that basis. Seventeen patients were noted to have a hiatal hernia. Three patients had Barrett esophagus and 5 had esophagitis, confirmed by pathology. No patient had delayed gastric emptying.
Two patients had severe esophageal dysmotility and were offered partial fundoplications of the Dor type. One patient had intermittent dropped propulsion and another was noted to have nutcracker esophagus, and these patients underwent standard Nissen fundoplication. The remaining patients had normal or near-normal motility, and all underwent Nissen fundoplication. The mean lower esophageal pressure was 9 (0–22) mmHg and the mean DeMeester score was 40 (5.1–227.3). Of the 8 patients who had a DeMeester score lower than 14.7, all had a positive symptom association index of 71.3% or greater.
The mean duration of surgery was 125 (70–161) minutes, and total operative time was 168 (115–210) minutes. In all cases, a 48- or 50-French bougie dilator was used, except the 2 patients who had Dor anterior fundoplications. There were no conversions or intraoperative complications. The length of stay in hospital was 2 days for 3 patients and overnight for the remaining patients.
There were no apparent postoperative complications, and the 30-day readmission rate was zero. There were no deaths. One patient required esophageal dilation for persistent dysphagia more than 3 months after surgery. Two patients had to resume medication for recurrent reflux symptoms, but the remaining 24 were off medications at the time of analysis. The symptom recurrences were not confirmed with pH studies because of the travel barrier.
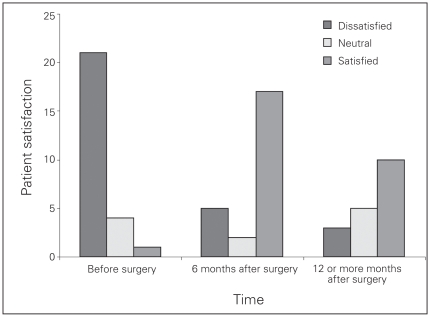
Figure 2 summarizes patient satisfaction with their present condition. It should be noted that some patients who indicated they were dissatisfied postoperatively explained that this was owing to other conditions, such as depression or diabetes, and not GERD; these patients wrote comments on their questionnaires to this effect.
Fig. 2.
Patient satisfaction with quality of life pre- and postoperatively.
Table 1 summarizes overall QOL scores. Compared with preoperative scores, there was a significant improvement in the GERD–HRQL and overall SF-36 scores 6 months postoperatively. However, when the SF-36 was broken down into physical health and mental health scores, only the physical health component showed significant improvement at the 6-month mark. Of the patients who were at a follow-up stage of 12 or more months postoperative at the conclusion of the study, the mean length of follow-up was 21 (range 12–34) months. Compared with the preoperative scores, there was significant improvement in the GERD–HRQL scores but not in any of the SF-36 scores.
Table 1.
Comparison of pre- and postoperative GERD-HRQL and SF-36 scores
Table 2 compares the GERD-HRQL and SF-36 scores between patients with and without CPS. The GERD–HRQL scores improved significantly in both groups at 6 and 12 or more months postoperatively. The SF-36 overall score and the physical health and mental health component scores all improved significantly in patients without CPS at 6 and 12 or more months postoperatively; however, in patients with CPS, there was no improvement at the 12 or more month mark.
Table 2.
Comparison of GERD-HRQL and SF-36 scores of patients with and without chronic pain syndrome at 12 or more months after surgery
| Patient group; test | Time; score* | ||
|---|---|---|---|
| Preoperative | 6 months after surgery | 12 or more months after surgery | |
| No chronic pain | |||
| No. questionnaires completed | 18 | 18 | 10 |
| GERD-HRQL | 26 | 7† | 13† |
| SF-36 | 63 | 75† | 74† |
| Physical health | 58 | 74† | 71† |
| Mental health | 65 | 74† | 72† |
| Chronic pain | |||
| No. questionnaires completed | 8 | 6 | 7 |
| GERD-HRQL | 29 | 7† | 9† |
| SF-36 | 64 | 61 | 62 |
| Physical health | 58 | 51 | 51 |
| Mental health | 64 | 62 | 65 |
The mean preoperative gas bloat score was 2.9 (out of 5). The mean score was 1.9 at 6 months and 2.3 at 12 or more months. These differences were not statistically significant. Similarly, the mean dysphagia score was 2.0 pre-operatively, 1.1 at 6 months and 1.6 at 12 or more months; none was significant.
Discussion
Surgical outcomes in this study were equivalent or better than those reported in other studies.1,2,5,7,8,11,13 Careful selection has been recommended for patients with GERD2,14 and also when introducing other advanced laparoscopic procedures in a nonacademic community hospital setting to ensure excellent outcomes.15 Some studies have shown poor long-term outcomes after laparoscopic Nissen fundoplication in obese patients,16 and on this basis no patients with a BMI greater than 35 were offered surgery in the present study. Once good outcomes are established the indications can be broadened to include patients with a BMI greater than 35. Out of 342 referred patients in this study, only 36 were scheduled for laparoscopic antireflux surgery, which indicates a relatively conservative patient selection. As a result, there were no perioperative complications. There was 1 case of dysphagia requiring dilation, a rate of 3.8%, which is in keeping with the range of 0.3%–20% reported in the literature.13 There were no cases of severe gas bloat syndrome, which is in keeping with the rate of 0%–45% described in the literature. There were 2 cases (7.7%) of recurrent symptoms requiring resumption of medications, which compares with the rate of 3.47% reported in the literature. The length of stay of 1.1 days compared favourably with the reported average of 2.8 days.13
Assuming patients answered the questionnaires honestly in this nonblinded study, improvement in disease-specific QOL scores persisted 12–34 months postoperatively. However, the same was not found for SF-36 scores in patients with CPS, though there was a sustained improvement in SF-36 scores in patients without CPS. This phenomenon has been previously described by Velanovich,17 the same author who developed the GERD–HRQL scale. It is theorized that patients with CPS or psychoemotional disorders in the absence of reflux symptoms become fixated on persistent or new somatic complaints, leading to a decrease in overall health that overshadows improvement in GERD-specific symptoms. The present study concurs with that of Velanovich, especially with the finding of a significant deterioration in SF-36 physical health scores more than a year after surgery in patients with CPS. The recommendation that LAR surgery should be offered with caution to patients with CPS unless there is objective evidence of refractory esophagitis or Barrett esophagus is supported by this study.
It is difficult to identify which patients will not be satisfied with surgery based on whether they have CPS or not. However, some patients identify with their pain to the point of writing “I have chronic pain” when asked to list their medical illnesses on a preconsultation questionnaire, and it is these patients who seem to have fared poorly in terms of QOL scores after LAR surgery.
Conclusion
In general, careful patient counselling and informed consent should be employed when offering LAR surgery to patients with CPS, including discussing the possibility that their pain may become more pronounced after surgery.
Acknowledgements
I gratefully acknowledge help from Susan Caldwell and Janet Redgwell, medical office assistants, who tirelessly reminded patients to fill out the multiple questionnaires needed for this study.
Footnotes
Presented May 13, 2010, at the joint meeting of the British Columbia Surgical Society and Alberta Association of General Surgeons in Kelowna, BC
Conflicts of interest: None declared.
References
- 1.Anvari M, Allen C. Five-year comprehensive outcomes evaluation in 181 patients after laparoscopic Nissen fundoplication. J Am Coll Surg. 2003;196:51–7. doi: 10.1016/s1072-7515(02)01604-6. [DOI] [PubMed] [Google Scholar]
- 2.Gee DW, Andreoli MT, Rattner DW. Measuring the effectiveness of laparoscopic antireflux surgery. Arch Surg. 2008;143:482–7. doi: 10.1001/archsurg.143.5.482. [DOI] [PubMed] [Google Scholar]
- 3.Lundell L, Miettinen P, Myrvold HE, et al. Continued (5-year) follow-up of a randomized clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. J Am Coll Surg. 2001;192:172–9. doi: 10.1016/s1072-7515(00)00797-3. [DOI] [PubMed] [Google Scholar]
- 4.Heikkinen T, Koivukangas V, Wiik H, et al. The quality of life of gastroesophageal reflux disease patients waiting for an antireflux operation. Surg Endosc. 2004;18:1712–5. doi: 10.1007/s00464-004-9062-z. [DOI] [PubMed] [Google Scholar]
- 5.Fernando HC, Schauer PR, Rosenblatt M, et al. Quality of life after antireflux surgery compared with nonoperative management of severe gastroesophageal reflux disease. J Am Coll Surg. 2002;194:23–7. doi: 10.1016/s1072-7515(01)01110-3. [DOI] [PubMed] [Google Scholar]
- 6.Dassinger MS, Torquati A, Houston HL, et al. Laparoscopic fundoplication: 5-year follow-up. Am Surg. 2004;70:691–4. [PubMed] [Google Scholar]
- 7.Bonnet G, Khan MI, Ong L. Using quality-of-life instruments to measure outcome after laparoscopic fundoplication. N Z Med J. 2005;118:1594–9. [PubMed] [Google Scholar]
- 8.Balci D, Turkcapar AG. Assessment of quality of life after laparoscopic nissen fundoplication in patients with gastroesophageal reflux disease. World J Surg. 2007;31:116–21. doi: 10.1007/s00268-005-0658-9. [DOI] [PubMed] [Google Scholar]
- 9.McHorney CA, Ware JE. The MOS 36-item short-form health survey (SF-36): psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Velanovich V. Comparison of generic (SF-36) vs. disease-specific (GERD-HRQL) quality-of-life scales for gastroesophageal reflux disease. J Gastrointest Surg. 1998;2:141–5. doi: 10.1016/s1091-255x(98)80004-8. [DOI] [PubMed] [Google Scholar]
- 11.Hwang H, Turner LJ, Blair NP. Examining the learning curve of laparoscopic fundoplications at an urban community hospital. Am J Surg. 2005;189:522–6. doi: 10.1016/j.amjsurg.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Statistics Online Computational Resource. Los Angeles (CA): UCLA Department of Statistics; 2009. [accessed 2009 Nov. 29]. Available from: www.socr.ucla.edu/SOCR.html. [Google Scholar]
- 13.Carlson MA, Frantzides CT. Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg. 2001;193:428–39. doi: 10.1016/s1072-7515(01)00992-9. [DOI] [PubMed] [Google Scholar]
- 14.Spechler SJ, Lee E, Ahnen D, et al. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease. JAMA. 2001;285:2331–8. doi: 10.1001/jama.285.18.2331. [DOI] [PubMed] [Google Scholar]
- 15.Hwang H, Wiseman K. Excellent outcomes after establishing laparoscopic colon surgery in a nonacademic regional hospital. BC Med J. 2009;51:390–3. [Google Scholar]
- 16.Perez AR, Moncure AC, Rattner DW. Obesity adversely affects the outcome of antireflux operations. Surg Endosc. 2001;15:986–9. doi: 10.1007/s004640000392. [DOI] [PubMed] [Google Scholar]
- 17.Velanovich V. The effect of chronic pain syndromes and psychoemotional disorders on symptomatic and quality-of-life outcomes of antireflux surgery. J Gastrointest Surg. 2003;7:53–8. doi: 10.1016/S1091-255X(02)00136-1. [DOI] [PubMed] [Google Scholar]