Abstract
The current study examines how poverty and education in both the family and school contexts influence adolescent weight. Prior research has produced an incomplete and often counterintuitive picture. We develop a framework to better understand how income and education operate alone and in conjunction with each other across families and schools. We test it by analyzing data from Wave 1 of the U.S.-based National Longitudinal Study of Adolescent Health (N= 16,133 in 132 schools) collected in 1994–1995. Using hierarchical logistic regression models and parallel indicators of family- and school-level poverty and educational resources, we find that at the family-level, parent’s education, but not poverty status, is associated with adolescent overweight. At the school-level, the concentration of poverty within a school, but not the average level of parent’s education, is associated with adolescent overweight. Further, increases in school poverty diminish the effectiveness of adolescents’ own parents’ education for protecting against the risks of overweight. The findings make a significant contribution by moving beyond the investigation of a single socioeconomic resource or social context. The findings push us to more fully consider when, where, and why money and education matter independently and jointly across health-related contexts.
Keywords: U.S.A., adolescent, overweight, obesity, income, education, family, school, multilevel modeling
Most studies examining the role of social inequalities for adolescent overweight and obesity in the United States focus on differences in family income. An underlying assumption motivating this area of research is that money protects individuals from obesity in today’s “obesogenic” society. Several theoretical and practical arguments have been used to buttress this supposition, yet most prior studies do not support this assumption. They do not find a significant negative association between family income and adolescent overweight or obesity in nationally representative samples of U.S. youth (Goodman et al., 2003b; Gordon-Larsen et al., 2003; Martin, 2008; Troiano & Flegal, 1998; Wang & Zhang, 2006; Zhang & Wang, 2007). Nonetheless, many scholars still assert that money should be an important resource that protects adolescents from being overweight.
We seek to better understand how socioeconomic resources matter for adolescent weight in two important ways. First we consider whether a different stratified resource is important – parents’ education. Second, we consider whether adolescent weight is associated with the financial and educational resources in schools – another social context that is highly influential for adolescent well-being (Teitler & Weiss, 2000). Both families and schools are highly stratified with regard to both income and parents’ education. Thus, we investigate how these two resources in these two contexts influence adolescents’ risk of being overweight by analyzing data from the National Longitudinal Study of Adolescent Health (Add Health).
FAMILY AND SCHOOL-LEVEL RESOURCES INFLUENCING ADOLESCENT WEIGHT
Researchers often study family income and parents’ education together as indicators of socioeconomic status and predict that they have a similar association with adolescent weight given that family income and parents’ education are positively correlated (Balistreri & Van Hook, 2009; Goodman, 1999; Goodman et al., 2003a; Goodman et al., 2003b; Haas et al., 2003; Kimm et al., 1996; Strauss & Knight, 1999). We depart from this general approach and seek to unpack how parental education and income are distinctly associated with adolescent weight. This line of investigation and the hypotheses we derive are driven by prior research, which suggests that family income and parents’ education may influence adolescent weight in different ways.
We also examine how income and education are associated with adolescent weight across two contexts: the family- and school-level. Research on the latter is relatively novel, which leads us to be more speculative about how school-level income and education are associated with adolescent overweight. Our hypotheses about their importance derive from empirical results in two prior studies and from weaving together several strands of prior research on schools. Bringing schools’ socioeconomic resources into the research on adolescent overweight and obesity is a significant contribution given the paucity of research on this topic and the strong influence of schools on adolescents’ lives (Teitler & Weiss, 2000).
Family Resources and Adolescent Overweight
Because most American adolescents are dependent on their parents, adolescent stratification is a function of their families’ socioeconomic status, meaning their parents’ income and education. We argue that parents’ education and family income capture unique resources and patterns that can influence adolescent weight.
Family income provides family with the power to purchase goods and services, depending on their relative prices. In general, “healthy” food is relatively expensive and “bad” food is cheap (Drewnowski & Specter, 2004). Furthermore, the costs for adolescents’ physical activity are rising as schools implement pay-to-play policies for organized sports (McNeal, 1998). As such, scholars have argued that greater family income can affect an adolescent’s ability to maintain a healthy weight because it increases their ability to purchase “healthy” weight-related goods (Cawley, 2004). This theoretical perspective is pervasive in the literature and leads to the argument that family income should be negatively correlated with adolescent weight.
Despite the dominance of the supposition of a negative correlation between family income and adolescent weight, income could also be positively correlated with adolescent weight. Instead of using money to promote a healthy weight, families and adolescents could spend their money on goods that generate risks for adolescent overweight, such as video games, or meals prepared away from home.
The empirical evidence regarding the association between income and adolescent weight is mixed and generally does not fit with the dominant perspective that the correlation between income and adolescent weight is negative. Only one study finds a significant, negative association between family income and adolescents’ weight in a nationally representative sample (Goodman, 1999), while other studies find a negative association only for narrowly-defined adolescent subpopulations (Balistreri & Van Hook, 2009; Goodman et al., 2003b; Gordon-Larsen et al., 2003; Kimm et al., 1996; Miech et al., 2006; Troiano & Flegal, 1998; Zhang & Wang, 2007). Evidence supporting a positive association is also scarce: only one study finds a positive association among a nationally representative sample of adolescents (Haas et al., 2003). The majority of studies find no link between either family income or poverty and adolescent weight (Goodman et al., 2003b; Gordon-Larsen et al., 2003; Martin, 2008; Troiano & Flegal, 1998; Wang & Zhang, 2006; Zhang & Wang, 2007).
More consistent is a small body of literature demonstrating that parents’ education is significantly and negatively associated with adolescent weight among U.S. adolescents (Goodman, 1999; Goodman et al., 2003b; Haas et al., 2003; Martin, 2008; Sherwood et al., 2009). Some may interpret this finding as a different way of measuring family income, but that interpretation ignores evidence that parents’ education captures other resources, net of family income, that shape adolescents’ health and well-being.
First, schooling contributes to learned effectiveness – a sense of control to accomplish goals, including those that are health-related (Mirowsky & Ross, 2003). More highly educated parents, thus, have more learned effectiveness, which should make them more likely to believe that they can influence their child’s weight. Further, prior research shows that when parents try to regulate what their children eat (Ogden et al., 2006) and how active they are (Arluk et al., 2003), their children are generally leaner and less likely to be overweight.
Second, education provides parents with general capabilities, skills and knowledge (Becker, 1993) and correlates with the volume and breadth of their health-related knowledge (Link et al., 1998). We expect that education is positively correlated with an understanding of obesity’s etiology and possible consequences. Research bears this out. Lower educated parents tend to rely on folk understandings about what signifies a healthy weight for youth (Jain et al., 2001) and underestimate the incidence of youth overweight and obesity (Goodman et al., 2000). One factor that might explain this is that higher educated parents are more likely to engage with medical professionals about their child’s health (Lareau, 2003). Furthermore, a better understanding of obesity has been shown to prevent weight gain. Highly educated adults are less likely to be obese because of their greater awareness of the association between diet and disease (Nayga, 2000). We anticipate that this awareness carries over into how more educated parents feed and socialize their adolescent children and, thus, could influence adolescents’ own weight-related choices.
Together, the arguments and empirical evidence lead us to expect that parents’ education but not income will be related to adolescent overweight because of the knowledge, skills, experiences, and perspectives that are associated with more formal education. We do not discount the importance of income. Instead, we hypothesize that income matters at the school-level because money strongly shapes the amenities and stressors in adolescents’ non-familial environments.
School Resources and Adolescent Overweight
We focus on schools, because outside of families, schools are the primary social institutions that organize adolescents’ lives. During the academic year, adolescents spend the majority of their day at school (Zick, 2010). Schools also shape adolescents’ daily activities and friendships through their extracurricular offerings (Guest & Schneider, 2003) and by organizing students into grade levels and academic tracks (Kubitschek & Hallinan, 1998).
Schools also influence what adolescents eat, do and value (Story et al., 2006; von Hippel et al., 2007). Most adolescents eat at least one meal per day at schools, which serve breakfast and lunch and have vending machines available on campus (Delva et al., 2007). Adolescents’ physical activity is affected by the availability and quality of a school’s physical education courses, extracurricular activities, and exercise facilities (Leviton, 2008; Sallis et al., 2001). Finally, school-based cliques influence students’ weight-related norms and values (Ali et al., 2011b; Paxton et al., 1999), which in turn shape their dieting and weight-control behaviors (Ali et al., 2011a; Mueller et al., 2010).
Despite the large role that schools have in adolescent’s lives, few studies have examined how school-level resources influence adolescent weight. Two exceptions focus on parallel resources to those that we investigate at the family level: the average family income of schools (Richmond & Subramanian, 2008) and the average education level of parents in the school (O’Malley et al., 2007). In these studies, both school-level resources have a significant, negative association with adolescent weight. Unfortunately, neither study addresses whether the associations they uncover are confounded by other school-level resources, including the alternate measure of school socioeconomic resources. Other potential confounders are also not addressed well. O’Malley and colleagues (2007) control for many school characteristics, the adolescent’s race/ethnicity and parents’ education in their statistical models, but not other individual- or family-level factors that predict adolescent weight. Richmond and Subramanian (2008) account for a limited number of individual- and family-level predictors of adolescent weight, but only include one school-level confounder – the school’s racial/ethnic composition.
A primary contribution and strength of this study is the examination of whether the average family income and parental education level in schools are related to adolescent overweight net of each other and other school-, family-, and individual-level confounders. Furthermore, as the first study to examine parallel income and educational resources across family and school contexts, we can present a more complete picture of how these resources are related to weight across the two most important social institutions in adolescents’ lives.
An additional contribution is that we develop explanations for how and why school-level income and parents’ education are associated with adolescent overweight. Given the paucity of research on this topic, we offer new, but speculative arguments and predictions, bringing in related research where possible. We hypothesize that the average family income of a school better predicts adolescent overweight than does the average education level of parents within a school. Furthermore, we expect the estimated effect of school-level income to be nonlinear. We hypothesize that poor schools are particularly risky for adolescent overweight relative to both middle- and high-income schools.
These suppositions stem from several factors. First, school-level income is highly correlated with the school funding, despite states’ redistributive efforts (Corcoran et al., 2004; U.S. Government Accountability Office, 1997). Further, school funding plays a direct and important role in a school’s food provisions and ability maintain facilities and curricula that promote physical activity. Richer schools generally offer healthier à la carte and vending options than poorer schools (Delva et al., 2007) and can fully finance school physical education programs and extracurricular activities (Leviton, 2008; Story et al., 2006). Poorer schools have frequently had to cut physical activity programs given recent pressure to focus on academic test scores (Leviton, 2008; Story et al., 2006). Yet physical education and extracurricular programs are particularly important for middle and high school students given that physical activity falls precipitously during adolescence (Must & Tybor, 2005). In addition, after-school programs (of any kind) could help adolescents maintain a healthy weight because their participation limits adolescents’ time available for snacking and watching television (von Hippel et al., 2007).
Second, school poverty may also be associated with adolescents’ weight indirectly. Poor schools have a greater prevalence of juvenile delinquency, disorder, and classroom disruption (Mrug et al., 2008), making them stressful environments that induce individuals’ stress response. Unfortunately, chronic activation of the stress response increases abdominal fat (Anagnostis et al., 2009; Bjorntorp & Rosmond, 2000; Fraser et al., 1999). This further buttresses our hypothesis that poor schools are adverse weight-related environments.
We speculate that a school’s average parental education level and the prevalence of highly educated parents, in particular, could indirectly be associated with adolescent weight. Because highly educated parents make more demands for school improvements (Lareau, 2003), we expect that schools would face more pressure to maintain or improve aspects related to adolescent weight as the average of parents’ education increases. Yet these efforts may be futile if the associated financial costs are high. For example, seemingly simple suggestions like eliminating advertisements for and availability of high-calorie foods and beverages in schools come at a cost because many schools rely on food industry subsidies to fund academic and extracurricular programs (Nestle, 2002). Therefore, we predict that school poverty constrains the relative influence of parents’ collective education within a school.
The Intersection between School Poverty and Own Parents’ Education
Our study asks one final question about family- and school-level resources: Does family-level parental education and school-level poverty work in conjunction to produce a joint association with adolescent weight? We speculate that school-level poverty modifies the association between family-level parental education and adolescent weight. This proposed interaction is motivated by theories of resource multiplication and resource substitution (Ross & Mirowsky, 2006). Resource multiplication theory argues that various resources accumulate to impact health (Ross & Mirowsky, 2006). In our study, this would imply that adolescents of highly educated parents in rich schools have more opportunities for maintaining a healthy weight. Those opportunities would cascade and amplify the effects of each other. As such, differences in adolescent weight by parents’ education would be larger in rich versus poor schools.
Conversely, resource substitution theory predicts that various resources can have a compensatory dynamic that offsets the risks (or advantages) of another resource for one’s health (Ross & Mirowsky, 2006). In our analysis, this would lead us to expect that adolescents with more educated parents are better buffered against the weight-related risks of attending a poor school. In this scenario, differences in adolescent weight by parents’ education are greatest in poor schools and relatively diminished in rich schools. A priori, we think both processes are plausible.
In summary, we argue that the relationships between financial resources, educational resources and adolescent weight are complicated. We agree with scholars who argue that money is important for weight and we agree that parental education is important. But we argue that the function and relative importance of these resources varies across families and schools. We offer an initial examination of these parallel resources by exploring whether there is any evidence for the differential associations we propose across the family- and school-level by analyzing cross-sectional, nationally representative data.
DATA AND METHODS
Add Health is a United States school-based sample of 20,745 1994–1995 7th–12th graders from over 140 high schools and middle schools (Udry, 2003). The original sample, which was followed up in 1995–1996, 2001–2002 and 2007–2008, includes oversamples of Cubans, Puerto Ricans, Chinese, and high socioeconomic status African Americans (Harris et al., 2003). Human subjects approval for this study was obtained from the Pennsylvania State University’s IRB. We received an expedited review for secondary data.
Our analysis relies on the 1994–1995 Wave 1 data. This is the only survey wave when parents were interviewed (and, thus, family income measured) and when school-level characteristics were obtained. Changes in family and school resources cannot be assessed. In addition, a significant proportion of adolescents are not in their Wave 1 schools by Wave 2. Some students have made normative transitions from middle school to high school and some have made non-normative transfers to other schools (Riegle-Crumb et al., 2005). In addition, adolescents who were high school seniors in Wave 1 were not followed in Wave 2. Thus, for nearly a third of our sample, Wave 1 school characteristics no longer characterize their Wave 2 schools. By Waves 3 and 4, Add Health respondents are no longer in secondary school. Despite these limitations, Add Health is still the best data source for our study. No other nationally representative data set collected since Add Health contains the requisite information on adolescents’ schools and families or has data on so many factors that are confounded with socioeconomic status and weight.
We make the following sample restrictions. We randomly select one adolescent per family using STATA’s random number generator if a family contributes more than one sibling to the Add Health sample. We do this because siblings cannot be treated as independent observations and, to estimate a more complicated three-level HLM model (with individual students nested within families within schools), we would need to drop 70% of the sampled families because they have only one sampled adolescent in Add Health. We exclude adolescents who were pregnant or had an unknown pregnancy status between 1994 and 1996 to avoid confounding due to the joint determination of weight and fertility. Finally, we dropped adolescents who did not have a valid sampling weight or did not attend an Add Health school.
We utilize multiple imputation to replace any missing data on analytic variables, which replaces missing values with predictions from information observed in the sample (Rubin, 1987). We use the supplemental program “ice” within STATA 9.0 (Royston, 2005a, b) to create five imputed data sets. The imputation models include all of the variables included in the empirical models, as well as each parents’ occupation and adolescents’ Wave 2 weight. We estimate the empirical models for each imputed data set and then combine the results, accounting for variance within and between imputed samples to calculate the coefficients’ standard errors (Acock, 2005; Rubin, 1987). The final sample is 16,133 adolescents in 16,133 families attending one of 132 schools. Given Add Health’s design (Chantala & Tabor, 1999), there are, on average, 128 interviewed students per school (range: 16–1,443; interquartile range: 67–136).
Overall, 33% of our sample has missing data on at least one analytic variable. The variable with the most missing data is family income, the variable that we use to assess poverty status. Among sample members, 26% has missing data on income, where 15% are missing because parents did not complete a parent questionnaire and 11% is due to item non-response. Because this is a primary study variable of interest, we confirm in several supplemental tests that neither missing income data nor our imputation procedure biases our study results. The robustness checks include (1) estimating the models on a listwise deletion sample, (2) substituting an alternative indicator of poverty (i.e., parents cannot pay bills) that has less missing data (only 2.3% due to item non-response), and (3) including flags for whether family income or any other data are missing. Regarding the latter, we find that the flag for missing family income is never statistically significant, but the flag for any missing data is positive and statistically significant. Yet our substantive conclusions about our key variables do not change with any of the three robustness checks. (Results available upon request.)
Despite the importance of schools for adolescents, some may worry that our school measures are simply capturing neighborhood characteristics. Yet American schools, especially high schools, typically draw from multiple neighborhoods. For the schools in our sample, the median number of census block groups (each containing approximately 1,000 residents) per school is 29 (range: 2–286), the median number of census tracts (a common measure of U.S. neighborhoods containing approximately 4,000 residents) is 15 (range: 2–231), and the median number of counties is 3 (range: 1–9). In our sample, schools are not reducible to neighborhoods.
Measures
Adolescent Overweight
This dichotomous variable is based on adolescents’ Wave I self-reported height and weight, which we use to construct age- and sex-specific BMI percentiles using U.S. Centers for Disease Control and Prevention guidelines (Ogden et al., 2002b). We then classify adolescents as overweight or obese (BMI ≥ 85th percentile) versus normal weight or underweight. In supplemental models, we also predict BMI z-scores with a linear model and arrive at the same substantive conclusions. (Results available upon request.)
Family Resources
We measure parents’ education, as years of completed schooling (Ross & Mirowsky, 1999). In two-parent families, it is the average of both parents’ education. These data are first obtained from the parent, but are supplemented with the adolescent’s report when parent-reported data are missing. If both reports are missing, it is multiply imputed. Supplemental models find nearly identical results using maternal education.
For income, we create a dichotomous variable indicating that the family is poor (=1) based on parental reports of the total, pre-tax income the family received in 1994, the family’s composition, and the U.S. Census Bureau official poverty thresholds for 1994 (United States Census Bureau, 2005). We focus on poverty rather than other income specifications for ease of interpretation and comparability to other studies. That said, we also estimated models using several alternative measures to ensure that our findings are insensitive to how family income is operationalized. The specific measures are as follows: (1) a linear measure of the family’s originally reported total, pre-tax income, (2) the started log of income (i.e., ln[income + 1]) to have a more normal distribution of income and allow for nonlinearities whereby a $1 increase in income is more consequential at the bottom versus the top of the income distribution, (3) five dichotomous variables to indicate where, within six income percentile categories, the family income falls to examine nonlinearities throughout the income distribution, and (4) a linear measure of the family’s income-to-needs ratio, which is calculated as the ratio of the family’s income to the U.S. Census Bureau’s official 1994 poverty threshold for their family type. The substantive results are identical across these measurements (see Appendix Table 1).
Appendix Table 1.
Select coefficients from hierarchical logistic regression models predicting adolescent overweight with different measures of income (N = 16, 133)
| Model 3 | Model 4 | |
|---|---|---|
| Panel A. Income | ||
| Own Parental Education | −0.046*** (0.01) | −0.019 (0.02) |
| Family Income | −0.001 (0.00) | −0.001 (0.00) |
| School Median Parental Education | −0.057* (0.03) | −0.065* (0.03) |
| School Mean Income | −0.003† (0.00) | 0.006 (0.01) |
| Own Parents’ Education * School Mean Income | -- | −0.001 (0.00) |
| Panel B. Log Income | ||
| Own Parental Education | −0.049*** (0.01) | 0.115† (0.07) |
| Log(Family Income) | 0.006 (0.03) | 0.005 (0.03) |
| School Median Parental Education | −0.038 (0.03) | −0.032 (0.03) |
| School Mean Log Income | −0.357*** (0.10) | 0.287 (0.29) |
| Own Parents’ Education * School Mean Log Income | -- | −0.048* (0.02) |
| Panel C. Income-to-Needs Ratio | ||
| Own Parental Education | −0.047*** (0.01) | −0.021 (0.02) |
| Family Income-to-Needs Ratio | −0.006 (0.01) | −0.005 (0.01) |
| School Median Parental Education | −0.066* (0.03) | −0.076** (0.03) |
| School Mean Income-to-Needs Ratio | −0.041 (0.03) | 0.170 (0.12) |
| Own Parents’ Education * School Mean Income-to-Needs Ratio | -- | −0.013† (0.01) |
| Panel D. Income Percentile Categories | ||
| Own Parental Education | −0.046*** (0.01) | −0.255† (0.14) |
| Family Income Categories (Omitted: 50th percentile ≤ Income < 75th) | ||
| Income < 10th percentile | −0.064 (0.09) | −0.050 (0.09) |
| 10th percentile q Income < 25th | 0.019 (0.07) | 0.024 (0.07) |
| 25th percentile q Income < 50th | 0.047 (0.07) | 0.046 (0.07) |
| 75th percentile Income < 90th | −0.018 (0.08) | −0.014 (0.08) |
| Income ≥ 90th percentile | −0.091 (0.08) | −0.063 (0.08) |
| School Median Parental Education | −0.031 (0.03) | −0.041 (0.03) |
| School Percentage in Different Income Categories (Omitted: % Income ≥ 50th & < 75th percentiles) | ||
| % where Income < 10th percentile | 1.113* (0.55) | 0.691 (2.90) |
| % where 10th percentile q Income < 25th | 0.185 (0.74) | −7.335* (3.51) |
| % where 25th percentile q Income < 50th | 0.047 (0.62) | −2.811 (3.34) |
| % where 50th percentile q Income < 90th | −0.332 (0.75) | −6.124 (4.10) |
| % where Income ≥ 90th percentile | −0.392 (0.48) | 0.262 (2.58) |
| Own Parents’ Education * School Percentage in Different Income Categories (Omitted: % Income ≥ 50th & < 75th percentiles) | ||
| Own Parents’ Education * % where Income < 10th percentile | -- | 0.031 (0.22) |
| Own Parents’ Education * % where 10th percentile q Income < 25th | -- | 0.589* (0.27) |
| Own Parents’ Education * School Percentage in Different Income Categories (Omitted: % Income ≥ 50th & < 75th percentiles) | ||
| Own Parents’ Education * % where 25th percentile q Income < 50th | -- | 0.223 (0.25) |
| Own Parents’ Education * % where 75th percentile q Income < 90th | -- | 0.424 (0.30) |
| Own Parents’ Education * % where Income ≥ 90th percentile | -- | 0.004 (0.18) |
Source: National Longitudinal Study of Adolescent Health, In-School survey and Wave 1 In-Home Survey with only one randomly selected child per multi-sibling household
Note: Standard errors in parentheses.
p<.10,
p < .05,
p < .01,
p <.001
All models include sex, age, race/ethnicity, nativity, disability, athleticism, parental obesity, region, urbanicity, school size, if a public school, and school racial/ethnic composition.
School Resources
School-level parental education is measured as the median of parents’ years of schooling for attending students. School income is defined as the percentage of students in poverty, to parallel our measure of family poverty. We operationalize this variable by aggregating Wave 1 family poverty data for children attending each sampled school to calculate the percent who are poor. In supplementary analyses, we also investigate aggregations of the four other family-level measures of income (described above). Results from these supplementary models, shown in Appendix Table 1, reinforce our theoretical emphasis on school poverty; all of the nonlinear models demonstrate that the key differences are at the bottom of the school income distribution.
Control variables
The models control for the adolescent’s age (measured in years), racial/ethnic identity (non-Latino, white = reference, African American, Latino, Asian, other), parental obesity (neither parent obese [reference category], both parents obese, mother obese, father obese), and dummy variables for whether they are female (=1), disabled (=1), born in the United States (=1), and/or athletic (=1). Most individual- and family-level control variables derive from the adolescent’s Wave 1 self-reports. Racial/ethnic identity is based on questions with predetermined categories, but with the option to select more than one. Adolescents’ athleticism is based on reports of participating in an organized school sport and/or playing an active sport or exercising five or more times a week during the past week. We include this variable because BMI conflates fat mass with fat-free mass (i.e., muscle and bones). Parental obesity is based on the parent’s report of whether the adolescent’s biological mother and/or father is “obese.”
We also control for school characteristics to guard against confounding with school resources and to account for Add Health’s complex survey design. These include the school’s size, regional location (west, midwest, south, or northeast [reference category]), urbanicity (suburban, rural, or urban [reference category]), whether it is a public school (yes =1), and the school’s racial/ethnic composition (% African American, % Latino, % Asian, % other, % non-Latino white [reference category]). The school’s racial/ethnic composition is derived from aggregating across attending students’ characteristics, while the others are derived from Add Health’s administrative data.
Statistical analysis
We use hierarchical logistic regression models in HLM 6.0 to model the effects of both family–level (i.e., “level 1”) and school-level (i.e., “level 2”) resources for adolescent overweight. Hierarchical models separate between-group (here, defined as schools) and within-group variance to provide accurate estimates of parameter effects and standard errors, adjusted for the non-independence of people in the same group (Bryk & Raudenbush, 1992). We estimate four models. The null model identifies the extent to which adolescent overweight clusters within schools. The second model includes all individual and family characteristics, as well as the school-level variables used in Add Health’s sampling design (i.e., size, region, urbanicity, and school type). The third model adds school-level income and school-level parental education, as well as their racial/ethnic composition. Fourth, we add interactions between parents’ years of schooling and school-level poverty.
RESULTS
We begin by describing our analytic sample using weighted descriptive statistics presented in Table 1. Similar to national estimates for the mid-1990s (Ogden et al., 2002a; Troiano et al., 1995), 25% of our sample is either overweight or obese. For the remainder of the text we refer to this group as “overweight.” On average, the adolescents’ parents have completed 13.2 years of schooling and approximately 19.6% of the adolescents live in poverty. Given that school resources are aggregates of these adolescent data, it is not surprising that the average level of student poverty and the school mean of parental education are similar to the individual estimates. The sample characteristics generally fit with national patterns.
Table 1.
Weighted descriptive statistics for final analytic sample (N = 16,133), averaged across all imputed data sets
| Mean or Percent | S.D. | |
|---|---|---|
| Individual- and Family-level Variables | ||
| Overweight/Obese | 24.7% | |
| Parental Education | 13.2 | 2.55 |
| Poverty | 19.6% | |
| Female | 47.1% | |
| Age | 15.4 | 1.75 |
| Native Born | 93.4% | |
| Race/Ethnicity | ||
| White | 64.7% | |
| African American | 15.5% | |
| Latino | 12.3% | |
| Asian | 3.7% | |
| Other | 0.8% | |
| Athletic | 60.7% | |
| Disabled | 3.0% | |
| Parental Obesity | ||
| Both Parents Obese | 5.8% | |
| Only Father Obese | 4.6% | |
| Only Mother Obese | 12.5% | |
| Neither Obese | 77.1% | |
| School-level Variables | ||
| Median Parental Education | 13.2 | 1.29 |
| Percent Poor | 19.8% | |
| Racial/Ethnic Composition | ||
| Percent White | 60.6% | |
| Percent African American | 21.2% | |
| Percent Latino | 13.1% | |
| Percent Asian | 4.2% | |
| Percent Other Races | 0.9% | |
| School size | ||
| Small | 23.5% | |
| Medium | 46.2% | |
| Large | 30.3% | |
| Public School | 90.9% | |
| Region | ||
| Northeast | 15.2% | |
| West | 21.2% | |
| Midwest | 22.7% | |
| South | 40.9% | |
| Urbanicity | ||
| Urban | 30.3% | |
| Suburban | 55.3% | |
| Rural | 14.4% | |
Source: National Longitudinal Study of Adolescent Health, In-School survey and Wave 1 In-Home Survey with only one randomly selected child per multi-sibling household
In Table 2 we show calculated correlations between parents’ years of schooling, the dichotomous variable for family poverty, and the log of family income to ensure that there is sufficient variation in these family- and school-level resources to estimate their independent effects. The correlation between parents’ education and family poverty is −0.34, while the correlation between parents’ education and the log of family income is −0.73. These estimates suggest that, while there is notable overlap, there is also sufficient variation to distinguish between these two types of family resources with 16,133 cases. Table 2 also shows that the correlation between family- and school-level poverty is 0.35, the correlation between the log of family income and the school’s mean log of family income is 0.46, and the correlation between parents’ years of schooling and school’s median years of parents’ schooling is 0.43. Thus, there is sufficient variation between family- and school-level resources to examine their differential effects on adolescent overweight.
Table 2.
Correlations amongst indicators of family and school resources
| Family Resources
|
School Resources
|
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Family Resources | ||||||
| (1) Parental Education | 1.00 | |||||
| (2) Poverty | −0.34 | 1.00 | ||||
| (3) Log Family Income | 0.46 | −0.73 | 1.00 | |||
| School Resources | ||||||
| (4) Median Parental Education | 0.43 | −0.22 | 0.33 | 1.00 | ||
| (5) Percent Poor | −0.33 | 0.35 | −0.41 | −0.63 | 1.00 | |
| (6) Mean Log Family Income | 0.37 | −0.34 | 0.46 | 0.73 | −0.95 | 1.00 |
Source: National Longitudinal Study of Adolescent Health, In-School survey and Wave 1 In-Home Survey with only one randomly selected child per multi-sibling household
Note: Correlations corrected for design effects and appropriately combine multiply imputed samples. All correlations significant at p <.001. Shaded boxes indicates cross-level correlations of the same resources.
Results from multivariate, hierarchical logistic regression models predicting adolescent overweight are presented in Table 3. We estimate a null model (Model 1) without any covariates to identify the extent to which adolescent overweight differs across schools. The estimated variance between schools (i.e., the intraclass correlation coefficient) is statistically significant, suggesting that there are school-level differences in the prevalence of overweight. The intraclass correlation provides empirical justification for our exploration of school-level factors in a hierarchical model.
Table 3.
Coefficients from hierarchical logistic regression models predicting adolescent overweight
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | −1.107*** (0.04) | 0.651 (0.44) | 1.03 (0.71) | 1.415 (0.74) |
| Individual- and Family-level Variables (Level 1) | ||||
| Parental Education | −0.055*** (0.01) | −0.048*** (0.01) | −0.09*** (0.02) | |
| Poverty | −0.04 (0.09) | −0.067 (0.09) | −0.051 (0.09) | |
| Female | −0.352*** (0.06) | −0.351*** (0.06) | −0.349*** (0.06) | |
| Age | −0.104*** (0.02) | −0.1*** (0.02) | −0.099*** (0.02) | |
| Native Born | 0.574*** (0.13) | 0.575*** (0.13) | 0.56*** (0.13) | |
| Race/Ethnicity (Omitted = non-Latino White) | ||||
| African American | 0.384*** (0.09) | 0.377*** (0.10) | 0.363*** (0.10) | |
| Latino | 0.392*** (0.09) | 0.354*** (0.10) | 0.353*** (0.10) | |
| Asian | −0.184 (0.24) | −0.233 (0.24) | −0.231 (0.24) | |
| Other Race/Ethnicity | 0.241 (0.38) | 0.174 (0.36) | 0.154 (0.36) | |
| Athletic | −0.261*** (0.05) | −0.257*** (0.05) | −0.256*** (0.05) | |
| Disabled | 0.064 (0.15) | 0.063 (0.15) | 0.057 (0.15) | |
| Parental Obesity (Omitted = Neither Obese) | ||||
| Both Parents Obese | 1.484*** (0.10) | 1.482*** (0.10) | 1.48*** (0.10) | |
| Only Father Obese | 0.492*** (0.14) | 0.492*** (0.14) | 0.488** (0.14) | |
| Only Mother Obese | 0.884*** (0.08) | 0.885*** (0.08) | 0.881*** (0.08) | |
| School-level Variables (Level 2) | ||||
| Median Parental Education | -- | −0.049 (0.03) | −0.037 (0.03) | |
| Percent Poor | -- | 0.013** (0.004) | −0.011 (0.012) | |
| Racial/Ethnic Composition (Omitted = Percent non-Latino White) | ||||
| Percent African American | -- | −0.004* (0.002) | −0.004* (0.002) | |
| Percent Latino | -- | −0.002 (0.003) | −0.002 (0.003) | |
| Percent Asian | -- | 0.008* (0.004) | 0.008* (0.004) | |
| Percent Other Races | -- | 0.005 (0.01) | 0.006 (0.006) | |
| Survey Design Variables | ||||
| School Size | −0.157* (0.07) | −0.101 (0.06) | −0.097 (0.06) | |
| Public School | 0.287 (0.15) | 0.07 (0.16) | 0.028 (0.16) | |
| Region (Omitted = Northeast) | ||||
| West | −0.116 (0.12) | −0.145 (0.10) | −0.148 (0.11) | |
| Midwest | −0.105 (0.13) | −0.119 (0.12) | −0.109 (0.12) | |
| South | −0.051 (0.11) | −0.045 (0.10) | −0.047 (0.11) | |
| Urbanicity (Omitted = Urban) | ||||
| Suburban | 0.075 (0.09) | 0.16 (0.09) | 0.165 (0.09) | |
| Rural | 0.136 (0.12) | 0.045 (0.13) | 0.05 (0.14) | |
| Cross-Level Interactions (Level 1*Level 2) | ||||
| Own Parents’ Education (L1)* | -- | -- | 0.002* (0.001) | |
| School Percent Poor (L2) | ||||
| Variance Between Schools | 0.129*** | 0.084*** | 0.058*** | 0.058*** |
| N | 16,133 | 16,133 | 16,133 | 16,133 |
Source: National Longitudinal Study of Adolescent Health, In-School survey and Wave 1 In-Home Survey with only one randomly selected child per multi-sibling household
Note: Standard errors in parentheses.
p < .05,
p < .01,
p <.001
Model 2 adds family poverty and parental education to the model. Similar to many prior studies, we find that living in a poor family is not significantly related to whether an adolescent is overweight. In supplemental models, we omit parental education from the model and find that family poverty is still not statistically significant. (Results available upon request.) Therefore, issues of multicolinearity are not driving the null finding for family poverty.
In contrast, the association between parental education and adolescent overweight is statistically significant regardless of whether we include family poverty in the model or not. With each additional year of parents’ schooling, the odds that an adolescent is overweight declines by 5% (1−[e−0.055] = 0.053 = 5.3%). This suggests that, for adolescent overweight, how much money a family has is less important than parents’ formal schooling.
Model 3 adds school-level resources and racial/ethnic composition. As expected, the findings for school resources are the opposite of what we find for families. The median level of parental education in a school is not significantly associated with adolescent overweight, but school-level poverty is. The odds that an adolescent is overweight increase by 1% (e0.013 = 1.013 = 1.3%) with each percentage point increase in how many students are poor at one’s school or by 19.5% with a one-standard deviation increase in school poverty (s.d. = 15%). This result is rather robust given that Model 3 includes such a wide range of individual-, family- and school-level confounders. The significant negative association between (own) parents’ education and adolescent overweight is only minimally reduced and remains statistically significant in Model 3. Overall, the results in Model 3 indicate that adolescents are at greater risk of overweight if they attend poor schools and if they have parents with less education.
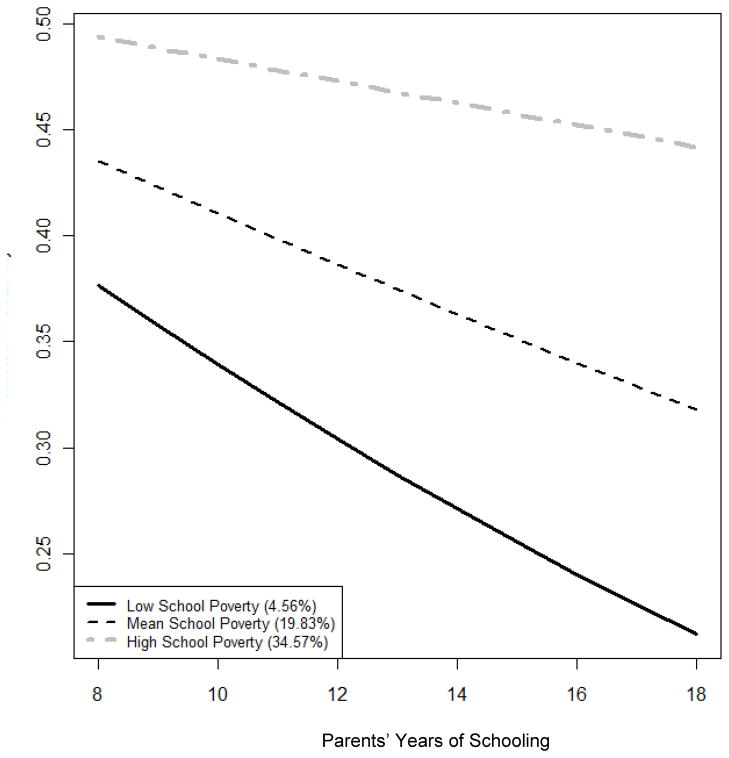
The remaining question is whether these two risk factors moderate each other. The results in Model 4 show that they do. We find a small, but significant and positive interaction between school-level poverty and one’s own parents’ education. The association between parents’ education and adolescent overweight is not uniform across different levels of school poverty. To clarify the patterns, Figure 1 shows the predicted probability of adolescent overweight as parents’ education increases for students who attend schools with average, low, and high proportions of poor students when all other variables in Model 4 are held constant at their mean or modal values. Average school poverty equals the school mean (20%), whereas low and high poverty are defined as one standard deviation (15%) below (i.e., 5%) or above the mean (i.e., 35%), respectively.
Figure 1. Predicted probability of adolescent overweight: The effectiveness of parents’ education across different levels of school poverty.
Note: Levels of school poverty are set relative to the distribution of poverty across schools. Low school poverty is one standard deviation below the school mean. High school poverty is one standard deviation above the school mean. Other variables in the model are set to their means or modal categories.
Figure 1 indicates that the benefits associated with increased parental education are smallest in the poorest schools and greatest in the richest schools. In the poorest schools, the predicted probability of being overweight among students whose parents have 12 versus 16 years of completed schooling is 0.47 and 0.45, respectively. In other words, the risks are almost exactly the same and relatively high, regardless of whether adolescents have parents that are high school or college graduates. Conversely, in the richest schools, the predicted probability of adolescent overweight is lower overall and the same four-year difference between parents who are high school and college graduates nets a larger reduction in the predicted probability of adolescent overweight. In summary, the protective effects of parents’ education are greatest in richer schools and fit patterns of resource multiplication (Ross & Mirowsky, 2006).
CONCLUSIONS AND DISCUSSION
This study aims to clarify how the risk of adolescent overweight is associated with socioeconomic stratification across the two primary social institutions in adolescents’ lives. We contribute to the literature on socioeconomic status and adolescent weight, showing that these patterns are quite complicated, requiring investigators to draw from different research strands to understand why and how family- and school-level poverty and educational resources could matter for adolescent weight both alone and net of each other.
Our findings make three significant contributions to knowledge about how socioeconomic stratification influences adolescent overweight. First, our analysis demonstrates that net of confounders and each other, parents’ education, but not family poverty, is associated with adolescent overweight. We speculate that highly educated parents influence their child’s weight by using their learned effectiveness, knowledge, and skills to help adolescents better navigate obesogenic environments. Educated parents also likely transmit their knowledge to their children, which may help adolescents make better weight-related choices themselves. We suspect that family poverty does not predict adolescent weight because, with more money, parents could just as easily buy a bigger cable TV package, meals out, or a house in a distant, new suburb versus buying goods that encourage more physical activity or a healthier diet. In essence, it may take knowledge or a particular outlook for parents to even consider the weight-related dimensions of their purchases.
Second, we demonstrate that poverty matters for adolescent overweight, but at the school-level. We speculate that school poverty shapes the weight-related structural features of schools. It likely diminishes a schools’ ability to offer students’ healthier food choices and physical activity options and may necessitate food industry corporate sponsorships (Nestle, 2002). The stressful nature of poor school environments may also contribute to adolescent overweight given that repeated activation of the stress response increases abdominal fat. An alternative explanation is that poor schools may engender or reinforce weight-related norms that are more accepting of or less averse to adolescent overweight. Schools and the peer groups they foster help define whom adolescents see as appropriate references for social comparisons (Crosnoe, 2000).
Some may worry that the significant association between school poverty and adolescent weight simply reflects rich parents self-selecting into better schools, especially given that we aggregate family-level data to measure school poverty. Our analysis actually speaks to this concern. If this were the case, then it would imply that school poverty mediates the association between family poverty and adolescent obesity. Thus, family poverty would to be a significant predictor of adolescent overweight before measures of school resources are included in statistical models (see Model 2, Table 3). We find no such association even when we utilize other specifications of family income in supplementary analyses. (Results available upon request.) We also estimated supplemental models that include a dummy variable for whether the parent agreed with the following statement (48% did agree): “You live here because the schools here are better than they are in other neighborhoods.” This variable is never statistically significant in models predicting adolescent overweight, nor is its interaction with family- or school-level poverty. Further, our study results remain unchanged when statistical models include this additional confounder. (Results available upon request.) This further suggests that endogenous sorting into schools does not drive our results.
Our third contribution is that we demonstrate that school-level poverty moderates the association between adolescents’ own parents’ education and their body weight. This is one of our most important and intriguing findings. School poverty impinges on the protective role of increased parents’ education. In high poverty schools, parental education has an almost negligible association with adolescent overweight. This supports Ross and Mirowsky’s (2006) model of resource multiplication. The effectiveness of one resource is hampered when other resources are limited. This finding speaks to the power of larger social environments for setting the opportunities and constraints that youth and their families must navigate. In more obesogenic school environments, parents’ educational resources may be overwhelmed.
In summary, the manuscript notably advances our understanding of families and schools as stratified health contexts that shape adolescent weight. Our findings are also instrumental in helping explain the counterintuitive null association between family poverty and adolescent overweight. It is not that poverty does not matter. Instead, it matters at a larger level of social organization than the family – the school context, both directly and as a moderator. With additional data, future research should explore the mechanisms that undergird these observed patterns. In addition, future research should consider the degree to which these patterns vary by sex and race/ethnicity. Prior research finds that family income is statistically significant and negatively correlated with adolescent weight among white girls, but not white boys while such sex differences are muted among other racial/ethnic groups (Gordon-Larsen et al., 2003; Wang & Zhang, 2006; Zhang & Wang, 2004). Such research would further reveal how these resources in these two stratified health contexts “get under the skin.”
Our findings must be considered within the boundaries of three study limitations. First, the study design is cross-sectional because Add Health does not have longitudinal data on family or school resources. That said, we do not expect the causal process to work in the opposite direction, whereby adolescent overweight affects family and school resources (i.e., as a “health selection” process (Haas, 2006; Palloni, 2006)). Furthermore, the cross-sectional measures of poverty and parental education that we use ensure that we assess these school-level resources when students are observably within them. This is particularly important given that many adolescents change schools outside of the formal, age-graded process (Riegle-Crumb et al., 2005). Second, with only 132 schools, we have less power to adjudicate between the relative role of poverty and parental education at the school-level. Finally, the measure of income in Add Health is rather limited because it is based on one question. As such, the estimated coefficients for both family- and school-level poverty could be downwardly biased if there is significant and systematic measurement error. This suggests that, if we had a more detailed measure of income, we could find a significant effect of family poverty, but it also implies that we may be under estimating the role of school poverty for adolescent overweight.
Despite limitations, our study makes significant contributions to understanding which socioeconomic resources matter for adolescent overweight. We move beyond thinking about resources solely in terms of their volume and begin to consider variations in their meaning, operation and effectiveness across different health-related contexts. The study’s findings push us to more fully consider why money and education matter independently and the environment within which these different resources are embedded. It is simpler to measure and construct hypotheses about the meaning of different family resources, but given that adolescents spend significant portions of their day outside the home – and, of that time, mostly in schools – it is important to consider the resources of environments outside the home and their associated risks or benefits. Such nuanced lines of investigation are imperative for the development of effective interventions for adolescent overweight and improving population health more generally.
Family-level parental education and school-level poverty predict adolescent overweight.
Family-level poverty and school-level parental education do not predict adolescent overweight.
Family education and school poverty interact: the benefits of having better educated parents are reduced in poor schools.
Footnotes
Funding for this research was provided by NICHD grant R01-HD050144 (PI: G.D. Sandefur) and the Career Development Program in Women’s Health Research at Penn State (K 12HD055882, PI: Carol Weisman). The opinions expressed and analyses conducted herein have been developed by the authors, independent of the granting agency. We thank Jason Houle for his research assistance and comments. We also thank Richard Carpiano, Steven Haas, and Adam Lippert for their comments and suggestions. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acock AC. Working With Missing Values. Journal of Marriage and Family. 2005;67(4):1012–1028. [Google Scholar]
- Ali MM, Amialchuk A, Heiland F. Weight-Related Behaviors among Adolescents: The Role of Peer Effects. PLoS ONE. 2011a;6(6):e21179. doi: 10.1371/journal.pone.0021179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali MM, Amialchuk A, Renna F. Social Network and Weight Misperceptions among Adolescents. Southern Economics Journal. 2011b;77(4):827–842. [Google Scholar]
- Anagnostis P, Athyros V, Tziomalos K, Karagiannis A, Mikhailidis D. The Pathogenetic Role of Cortisol in the Metabolic Syndrome: A Hypothesis. The Journal of Clinical Endocrinology & Metabolism. 2009;94:2692–2701. doi: 10.1210/jc.2009-0370. [DOI] [PubMed] [Google Scholar]
- Arluk SL, Branch JD, Swain DP, Dowling EA. Childhood obesity’s relationship to time spent in sedentary behavior. Military Medicine. 2003;168(7):583–586. [PubMed] [Google Scholar]
- Balistreri KS, Van Hook J. Socioeconomic Status and Body Mass Index Among Hispanic Children of Immigrants and Children of Natives. American Journal of Public Health. 2009;99(12) doi: 10.2105/AJPH.2007.116103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker GS. Human capital : a theoretical and empirical analysis, with special reference to education. Chicago: The University of Chicago Press; 1993. [Google Scholar]
- Bjorntorp P, Rosmond R. Obesity and Cortisol. Nutrition. 2000;16:924–936. doi: 10.1016/s0899-9007(00)00422-6. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park: Sage Publications; 1992. [Google Scholar]
- Cawley J. An Economic Framework for Understanding Physical Activity and Eating Behaviors. American Journal of Preventive Medicine. 2004;37(3S):117–125. doi: 10.1016/j.amepre.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Chantala K, Tabor J. National Longitudinal Study of Adolescent Health: Strategies to Perform a Design-Based Analysis Using the Add Health Data. Carolina Population Center: University of North Carolina; Chapel Hill: 1999. [Google Scholar]
- Corcoran S, Evans WN, Godwin J, Murray SE, Schwab RM. The Changing Distribution of Education Finance, 1972 to 1997. In: Neckerman KM, editor. Social Inequality. New York: Russell Sage Foundation; 2004. pp. 433–465. [Google Scholar]
- Crosnoe R. Friendships in Childhood and Adolescence: The Life Course and New Directions. Social Psychological Quarterly. 2000;63(4):377–391. [Google Scholar]
- Delva J, O’Malley PM, Johnston LD. Availability of More-Healthy and Less-Healthy Food Choices in American Schools: A National Study of Grade, Racial/Ethnic, and Socioeconomic Differences. American Journal of Preventive Medicine. 2007;33(4, Supplement 1):S226–S239. doi: 10.1016/j.amepre.2007.07.018. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Fraser R, Ingram M, Anderson N, Morrison C, Davies E, Connell J. Cortisol Effects on Body Mass, Blood Pressure, and Cholesterol in the General Population. Hypertension. 1999;33:1364–1368. doi: 10.1161/01.hyp.33.6.1364. [DOI] [PubMed] [Google Scholar]
- Goodman E. The Role of Socioeconomic Status Gradients in Explaining Differences in US Adolescents’ Health. American Journal of Public Health. 1999;89(10):1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obesity Research. 2003a;11(8):1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106(1 Pt 1):52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Goodman E, Slap GB, Huang B. The public health impact of socioeconomic status on adolescent depression and obesity. American Journal of Public Health. 2003b;93(11):1844–1850. doi: 10.2105/ajph.93.11.1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in U.S. adolescents. Obesity Research. 2003;11:121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- Guest A, Schneider B. Adolescents’ Extracurricular Participation in Context: The Mediating Effects of Schools, Communities, and Identity. Sociology of Education. 2003;76(2):89–109. [Google Scholar]
- Haas JS, Lee LB, Kaplan CP, Sonneborn D, Phillips KA, Liang SY. The association of race, socioeconomic status, and health insurance status with the prevalence of overweight among children and adolescents. American Journal of Public Health. 2003;93(12):2105–2110. doi: 10.2105/ajph.93.12.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas SA. Health Selection and the Process of Social Stratification: The Effect of Childhood Health on Socioeconomic Attainment. Journal of Health and Social Behavior. 2006;47:339. doi: 10.1177/002214650604700403. [DOI] [PubMed] [Google Scholar]
- Harris KM, Florey F, Tabor J, Bearman PS, Jones J, Udry JR. The National Longitudinal Study of Adolescent Health: Research Design. Chapel Hill, NC: Carolina Population Center, University of North Carolina; 2003. [Google Scholar]
- Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- Kimm SY, Obarzanek E, Barton BA, Aston CE, Similo SL, Morrison JA, et al. Race, socioeconomic status, and obesity in 9- to 10-year-old girls: the NHLBI Growth and Health Study. Annals of Epidemiology. 1996;6(4):266–275. doi: 10.1016/s1047-2797(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Kubitschek WN, Hallinan MT. Tracking and Students’ Friendships. Social Psychology Quarterly. 1998;61(1):1–15. [Google Scholar]
- Lareau A. Unequal Childhoods: Class, Race, and Family Life. Berkeley: University of California Press; 2003. [Google Scholar]
- Leviton LC. Children’s Healthy Weight and the School Environment. The ANNALS of the American Academy of Political and Social Science. 2008;615(1):38–55. [Google Scholar]
- Link BG, Northridge ME, Phelan JC, Ganz ML. Social Epidemiology and the Fundamental Cause Concept: On the Structuring of Effective Cancer Screens by Socioeconomic Status. The Millbank Quarterly. 1998;73:375–402. doi: 10.1111/1468-0009.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin MA. The intergenerational correlation in weight: How genetic resemblance reveals the social role of families. American Journal of Sociology. 2008;114(Suppl):S67–S105. doi: 10.1086/592203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeal, Ralph B. High School Extracurricular Activities: Closed Structures and Stratifying Patterns of Participation. The Journal of Educational Research. 1998;91(3):183–191. [Google Scholar]
- Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the Association of Poverty With Overweight Among US Adolescents, 1971–2004. JAMA. 2006;295(20):2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Education, Social Status, and Health. New York: Walter de Gruyter, Inc; 2003. [Google Scholar]
- Mrug S, Loosier PS, Windle M. Violence exposure across multiple contexts: Individual and joint effects on adjustment. American Journal of Orthopsychiatry. 2008;78(1):70–84. doi: 10.1037/0002-9432.78.1.70. [DOI] [PubMed] [Google Scholar]
- Mueller AS, Pearson J, Muller C, Frank K, Turner A. Sizing Up Peers: Adolescent Girls’ Weight Control and Social Comparison in the School Context. Journal of Health and Social Behavior. 2010;51(1):64–78. doi: 10.1177/0022146509361191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. International Journal of Obesity. 2005;29:S84–S96. doi: 10.1038/sj.ijo.0803064. [DOI] [PubMed] [Google Scholar]
- Nayga RM. Schooling, health knowledge and obesity. Applied Economics. 2000;32:815–822. [Google Scholar]
- Nestle M. Food Politics. Berkeley, CA: University of California Press; 2002. [Google Scholar]
- O’Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in Obesity Among American Secondary School Students by School and School Characteristics. American Journal of Preventive Medicine. 2007;33(4, Supplement 1):S187–S194. doi: 10.1016/j.amepre.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Ogden C, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. Journal of the American Medical Association. 2002a;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002b;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- Ogden J, Reynolds R, Smith A. Expanding the concept of parental control: A role for overt and covert control in children’s snacking behaviour? Appetite. 2006;47:100–106. doi: 10.1016/j.appet.2006.03.330. [DOI] [PubMed] [Google Scholar]
- Palloni A. Reproducing Inequalities:Luck, Wallets, and the Enduring Effects of Childhood Health. 2006;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Paxton SJ, Schutz HK, Wertheim EH, Muir SL. Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls. Journal of Abnormal Psychology. 1999;108(2):255–266. doi: 10.1037//0021-843x.108.2.255. [DOI] [PubMed] [Google Scholar]
- Richmond TK, Subramanian SV. School Level Contextual Factors Are Associated With the Weight Status of Adolescent Males and Females. Obesity. 2008;16(6):1324–1330. doi: 10.1038/oby.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegle-Crumb C, Muller C, Frank K, Schiller K. Adolescent Health and Academic Achievement (AHAA): User’s guide and codebook, first release. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2005. [Google Scholar]
- Ross CE, Mirowsky J. Refining the Assocation between Education and Health: The Effects of Quantity, Credential, and Selectivity. Demography. 1999;36(4):445–460. [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Social Science & Medicine. 2006;63(5):1400–1413. doi: 10.1016/j.socscimed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values: update. Stata Journal. 2005a;5(2):1–14. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update of ice. Stata Journal. 2005b;5(4):527–536. [Google Scholar]
- Rubin D. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- Sallis JF, Conway TL, Prochaska JJ, McKenzie TL, Marshall SJ, Brown M. The association of school environments with youth physical activity. American Journal of Public Health. 2001;91(4):618–620. doi: 10.2105/ajph.91.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood NE, Wall M, Neumark-Sztainer D, Story M. Effect of Socioeconomic Status on Weight Change Patterns in Adolescents. Preventing Chronic Disease. 2009;6(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, French S. The Role of Schools in Obesity Prevention. The Future of Children. 2006;16(1):109–142. doi: 10.1353/foc.2006.0007. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Knight J. Influence of the Home Environment on the Development of Obesity in Children. Pediatrics. 1999;103(6):e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- Teitler JO, Weiss CC. Effects of neighborhood and school environments on transitions to first sexual intercourse. Sociology of Education. 2000;73:112–132. [Google Scholar]
- Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101(3 Pt 2):497–504. [PubMed] [Google Scholar]
- Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Archives of Pediatrics & Adolescent Medicine. 1995;149(10):1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- U.S. Government Accountability Office. School Finance: State Efforts to Reduce Funding Gaps Between Poor and Wealthy Districts. Washington, D.C.: 1997. p. 323. [Google Scholar]
- Udry JR. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002 [MRDF] Chapel Hill, NC: Carolina Population Center, University of North Carolina [producer and distributor]; 2003. [Google Scholar]
- United States Census Bureau. Poverty Thresholds: 1994. Poverty Thresholds in 1994, By Size of Family and Number of Related Children Under 18 years. Housing and Household Economic Statistics Division, U.S. Census Bureau; 2005. [Google Scholar]
- von Hippel PT, Powell B, Downey DB, Rowland NJ. The Effect of School on Overweight in Childhood: Gain in Body Mass Index During the School Year and During Summer Vacation. American Journal of Public Health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. American Journal of Clinical Nutrition. 2006;84(4):707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: do gender, age, and ethnicity matter? Social Science & Medicine. 2004;58(6):1171–1180. doi: 10.1016/s0277-9536(03)00288-0. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Wang Y. Using concentration index to study changes in socio-economic inequality of overweight among US adolescents between 1971 and 2002. International Journal of Epidemiology. 2007;36:916–925. doi: 10.1093/ije/dym064. [DOI] [PubMed] [Google Scholar]
- Zick CD. The Shifting Balance of Adolescent Time Use. Youth & Society. 2010;41(4):569–596. [Google Scholar]