Abstract
Background
One complication of TKA is postoperative anterior knee pain. Balancing retinacular tissue tension to improve patellar tracking is essential in preventing pain. Lateral release might help balance tension although the quantitative changes in patellofemoral force and pressure differentials after lateral release are unknown.
Questions/purposes
We asked if there are differences in patellofemoral forces and pressures for knees resurfaced with standard and gender-specific components and whether lateral release changes these differentials.
Methods
We studied six fresh-frozen cadaver knees with native knees and knees that had TKAs with patellofemoral resurfacing using traditional and gender-specific components. The knees were taken through passive ROM, and the means for medial and lateral peak pressure and maximum force were calculated before and after a lateral release was performed.
Results
In traditional resurfaced knees, lateral peak pressure was greater than medial peak pressure by 727.6 ± 550.0 kPa and lateral maximum force was greater than medial maximum force by 29.6 ± 15.9 N. Lateral release decreased the pressure (71.4 ± 826.0 kPa) and force (10.0 ± 32.1 N) differentials in the traditional but not in the gender-specific design. In gender-specific resurfaced knees, lateral peak pressure was greater than medial peak pressure by 158.7 ± 360.0 kPa and lateral maximum force was greater than medial maximum force by 15.5 ± 10.4 N. Lateral release increased the pressure (285.7 ± 565.0 kPa) and force (16.8 ± 10.8 N) differentials.
Conclusions
Our preliminary data suggest lateral release is more effective in reducing peak pressure and maximum force differentials in knees resurfaced with traditional standard components than with gender-specific components.
Clinical Relevance
The lateral release technique might help with tissue balancing when using standard components in TKA.
Introduction
TKA is among the most clinically successful orthopaedic operations. The number of primary TKAs has been predicted to substantially increase owing to aging of the baby boomer population [9]. Achieving visually acceptable patellar tracking intraoperatively may play an important role in preventing postoperative complications [7, 8, 16]. Static and dynamic factors influence patellar tracking [18], and any alteration in these factors can result in maltracking. Patellar maltracking can result from excessive or unbalanced tension in the soft tissue constraints surrounding the patella, which may lead to postoperative anterior knee pain [4, 5, 15]. For the purposes of this article, we defined visually acceptable patellar tracking as intraoperative observation of the patella remaining in contact with both femoral condyles during full passive ROM after resurfacing. Maltracking is defined as incomplete patellar contact with the femoral condyles during part or all of the passive ROM.
Static factors, such as component alignment and soft tissue balance, and dynamic factors, such as quadriceps action during knee flexion and extension, all play important roles in affecting patellar tracking [5, 18]. Retinacular soft tissue imbalance negatively affects the patient after surgery. In 13 patients requiring revision surgery owing to anterior knee pain, Schuh and Hönle [16] found all 13 had hypertrophic lateral facets of the patella and lateral tracking of the patella during ROM of the knee. After lateral release and resection of the hypertrophic facets, all 13 patients were pain-free 9 months after surgery. Ostermeier et al. [13] reported that lateral release reduced pressure on the lateral patellar facet during flexion. Ritter and Campbell [15] studied more than 550 TKAs, 84 of which had a lateral release, and found no difference in knee pain, function, or ROM in those without and with release. Eighteen incidences of patellar fractures were documented, but 17 of those occurred in patients who did not undergo a lateral release. Kusuma et al. [7] similarly compared postoperative complications in 314 TKAs with a release with those in 794 without a release and reported no differences in rates of patella fracture or wound complications. Thus, it appears lateral release has no untoward consequences.
Currently, only the surgeon’s subjective examination, using techniques such as the ‘no thumb’ or ‘towel clip’ during intraoperative passive ROM testing, determines whether soft tissue balancing is adequate to maintain visually acceptable patellar tracking [3, 17]. It would be desirable to integrate subjective observations of patellar tracking with data describing the forces and pressures across the patellofemoral joint during an intraoperative ROM test. Such measurements would serve to augment the definition of patellar stability and assist in developing a more precise definition of maltracking [6, 11]. Modification techniques, such as soft tissue procedures, might be effective in reducing lateral to medial force and pressure differentials, which if large enough, may lead to patellar maltracking. One such modification is an intraoperative lateral retinacular release.
This pilot study addresses two questions: (1) What are the lateral to medial differentials in patellofemoral forces and pressures for knees resurfaced with standard and gender-specific components; and (2) what is the quantifiable effect of lateral retinacular tissue release on the pressure and force differentials?
Materials and Methods
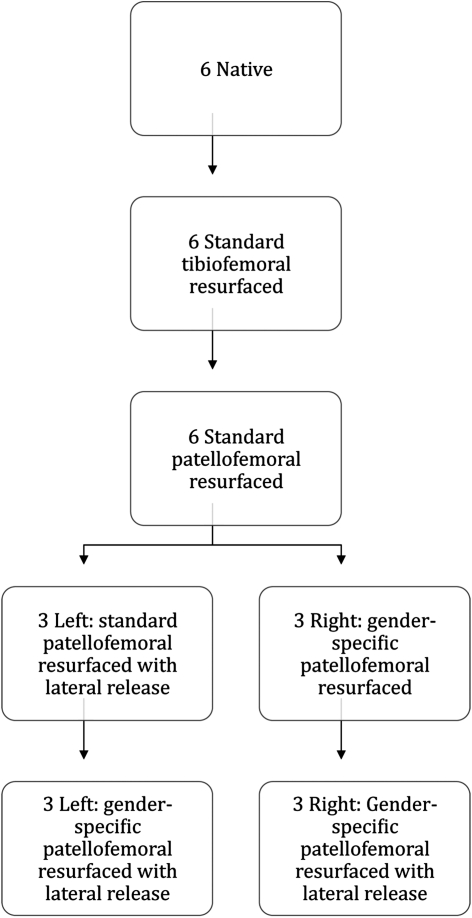
Fresh-frozen knees were obtained from three human female cadavers (mean age, 82 years). The three left knees were examined in the following sequential order: the native state, standard component patellofemoral resurfaced state, standard component patellofemoral resurfaced with lateral release state, and gender-specific component patellofemoral resurfaced with lateral release state (Fig. 1). The three right knees were examined in the following sequential order: the native state, standard component patellofemoral resurfaced state, gender-specific component patellofemoral resurfaced, and gender-specific component patellofemoral resurfaced with lateral release state. In every stage of resurfacing, mean values for medial peak pressure, lateral peak pressure, medial maximum force, and lateral maximum force were recorded. Two component types were evaluated: NexGen standard knee components and Gender Solutions NexGen High-Flex components (Zimmer Inc, Warsaw, IN, USA).
Fig. 1.
The flow of cuts is shown.
Cadavers were placed in the supine position with pelvic stabilization matching the positioning technique used for TKA. Knee ROM for arthrotomy, bone cuts, component implantation, and testing simulated that of an actual procedure. Preoperative passive ROM was documented for each knee.
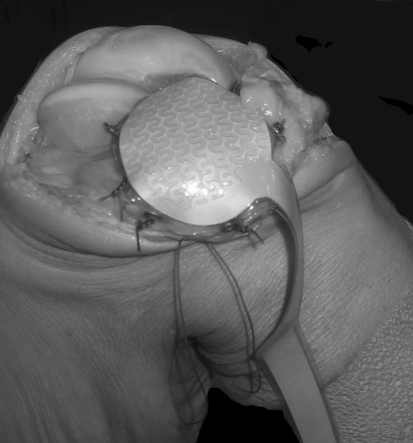
For the native state, all knees were exposed using a standard medial parapatellar approach and the articular cartilage was classified using the Outerbridge system [14]. Knees were flexed and the patella everted in the standard fashion. The sensor device was sutured over the articular surface of the native patella (Fig. 2) and the joint capsule was tacked closed with three sutures (one superior, one inferior, one central). The sensor and patella combination was manually elevated from the joint and zeroed in the unloaded state. Then, the sensor and patella were placed onto the joint and recordings were initiated while the native knee was taken through three to four consecutive, continuous ranges of motion. We recorded maximum forces (N) and peak pressures (kPa) over a complete ROM. During the repeated measures, we described data points by laterality (medial/lateral).
Fig. 2.
The sutured sensor is shown. (Published with permission from Johanson NA, Cerynik DL, Pasquale M. Measuring patellofemoral forces and pressures in a simulated operating room environment. J Arthroplasty. 2011;26:137–143.)
For the patellofemoral-resurfaced state, NexGen components were implanted using standard procedures. The joint capsule was reopened and bone cuts made to the femur and tibia. Trial components were implanted for the femur and tibia. The patella was exposed by partially removing the sensor from the field. Standard patella cuts were made and a domed 32-mm patellar component was implanted. The sensor was resutured over the component, the capsule was closed, and assessment was performed as previously described. In similar fashion, this procedure was repeated for 34-mm and 36-mm patellar components.
Subsequently, the three left patellofemoral-resurfaced knees underwent lateral release and were reassessed in a similar fashion. Lateral release was performed using a continuous incision through the capsule and lateral retinaculum extending from, and including, the vastus lateralis tendon to the joint line, passing 1 to 1.5 cm lateral to the patella.
Next, Gender Solutions components were implanted in all six knees. The joint capsule was reopened and the femoral component removed. Using the necessary bone cuts, all six knees were fitted with Gender Solutions femoral trial components. As this point, the three right knees (without lateral release) and three left knees (with lateral release) were assessed using the steps previously described. Finally, the three right knees underwent lateral release, using the surgical technique and assessment protocol described above. Passive ROM was performed with both of the surgeon’s hands on the leg, the tibia held in neutral rotation, and three sutures closing the medial parapatellar arthrotomy. Before suturing the arthrotomy for sensor readings, patellar tracking was checked by putting the knee through ROM in the same manner with the joint open using a classic ‘no thumbs’ test. Each knee was taken through a minimum of three passive ranges of motion, and a fourth recording was taken only if, in the opinion of the operator who monitored the sensor output, there was an irregularity in the data collection process in any of the ROM cycles.
All trials had visually acceptable patellar tracking by visual examination and showed maximum peak pressures and forces with the knee in maximum flexion. Visually acceptable tracking was defined as patellar contact with both femoral condyles throughout the entire ROM; return to preoperative patellar tracking was not our goal. All procedures, ROM tests, and visual examinations of patellar tracking were completed by the senior author (NAJ).
We used the capacitive-based Novel pliance pressure measurement system (Novel Electronics Inc, St Paul, MN, USA) to record pressures. The patella sensor consists of 87 sensor elements. Sixty sensor elements measure 5 mm × 5 mm × 1.8 mm, including waterproof coating, whereas the size of the remaining 20 varies. The total sensing area equals 1955 mm2 [2]. The sensor matrix consists of two equal and opposite conducting grids separated by dielectric material. The two grids intersect to make a capacitive sensing element. Decreasing separation of the grids during matrix loading causes changes in capacitance. The sensor was calibrated using the manufacturer’s true-blue calibration device and Pliance-x Expert calibration software. The sensor was placed inside the true-blue device and subjected to homogenous air pressure across its surface. A calibrated manometer read air pressure in the device. During this time, the software calibrated each sensor element across the entire range of measurement and displayed these data during experimental data collection.
Data were collected at 50 Hz and sent wirelessly to the pliance-x Expert software, which displayed a real-time two- or three-dimensional model of the pressures. For each frame of data, the individual pressure values were captured for each sensor in the matrix. The force was calculated by summing all the pressures multiplied by the active area. The maximum force was the maximum value of the force versus time graph, or the maximum force value throughout the capture frames. The entire sensor surface area reported calibrated pressure values of peak pressure, mean pressure, force, force-time integral, and pressure-time integral and displayed online time-process graphs and bar graphs. Values and graphs were grouped according to the specified medial and lateral parameters.
We computed descriptive statistics and then used a univariable analysis to compare values in maximum force and peak pressure from native knees with those of knees in the patellofemoral-resurfaced and lateral release groups. Mean values for medial and lateral maximum forces and peak pressures were established via plots of averages, determined by the GPLOT procedure, across design points to determine whether differences in means between the medial and lateral sides were consistent. Mean values were categorized by type of prosthesis and treatment of the patella and compared between medial and lateral sides in a pairwise manner [12]. Differences were determined using a Student’s t-test with a pooled sample variance via the t-test procedure. An f-test (folded) was used to assess the assumption of equal sample variances between medial and lateral sides [1]. The Satterthwaite t-test and Wilcoxon rank-sum nonparametric test were used when sample variances differed at an unadjusted alpha (type I) error level of 0.05 via the NPAR1WAY procedure [1]. We used SAS software (version 8.02; SAS Inc, Cary, NC, USA) for all analyses.
Results
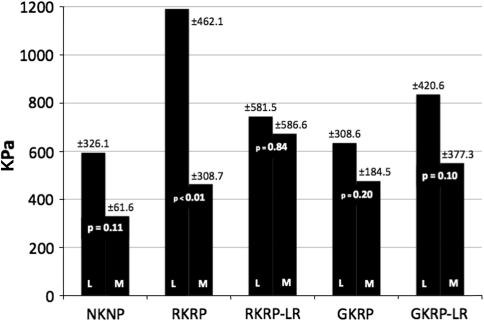
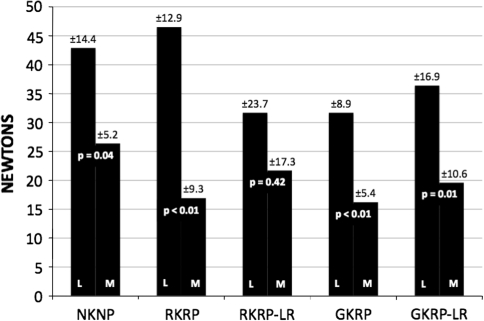
For native knees, lateral peak pressure was greater (p = 0.11) than medial peak pressure by 264.1 ± 331.9 kPa. Maximum force in native knees was greater (p = 0.04) laterally than medially by 16.5 ± 15.3 N. After knees were resurfaced with traditional components, peak pressure remained greater (p < 0.01) laterally than medially by 727.6 ± 550.0 kPa (Fig. 3) and lateral maximum force was greater (p < 0.01) than medial maximum force by 29.6 ± 15.9 N (Fig. 4). After knees were resurfaced with gender-specific components, lateral peak pressure was greater (p = 0.20) than medial peak pressure by 158.7 ± 360.0 kPa and maximum force was greater (p < 0.01) laterally than medially by 15.5 ± 10.4 N.
Fig. 3.
Lateral versus medial comparisons of peak pressure (PP) across study groups are shown: (TKA cadaver knees) (NKNP = native knee/native patella; RKNP = resurfaced knee/native patella; RKRP = resurfaced knee/resurfaced patella; RKRP-LR = resurfaced knee/resurfaced patella post–lateral release; GKRP = resurfaced gender knee/resurfaced patella; GKRP-LR = resurfaced gender knee/resurfaced patella post–lateral release).
Fig. 4.
Lateral versus medial comparisons of maximum force (MF) across study groups are shown: (TKA cadaver knees) (NKNP = native knee/native patella; RKNP = resurfaced knee/native patella; RKRP = resurfaced knee/resurfaced patella; RKRP-LR = resurfaced knee/resurfaced patella post–lateral release; GKRP = resurfaced gender knee/resurfaced patella; GKRP-LR = resurfaced gender knee/resurfaced patella post–lateral release).
After lateral release in knees resurfaced with standard components, peak pressure remained greater (p = 0.84) laterally than medially by 71.4 ± 826.0 kPa. This pressure differential was 656.2 kPa less than the pressure differential present before lateral release. Lateral maximum force remained greater (p = 0.42) than medial maximum force by 10.0 ± 32.1 N. This force differential was 19.6 N less than the force differential present before lateral release. After lateral release in knees resurfaced with gender-specific components, lateral peak pressure was greater (p = 0.10) than medial peak pressure by 285.7 ± 565.0 kPa. This pressure differential was 127 kPa greater than the pressure differential that was present before lateral release. Maximum force remained greater (p = 0.01) laterally than medially by 16.8 ± 10.8 N. This differential was 1.3 N greater than the differential present before lateral release.
Mean lateral peak pressure in traditional component knees was 1190.8 ± 462.1 kPa. This value decreased (p = 0.11) after lateral release to 744.5 ± 581.5 kPa (Table 1). The same relationship was noted for lateral maximum force. Before lateral release, the mean lateral maximum force was 46.5 ± 12.9 N and decreased (p = 0.17) to 31.7 ± 23.7 N (Table 2). However, lateral peak pressure and maximum force increased after lateral release for knees resurfaced with gender-specific components. These knees had a mean lateral peak pressure of 634.5 ± 308.6 kPa before release, which increased (p = 0.92) to a mean of 836.1 ± 420.6 kPa after release. Before lateral release, gender-specific knees had a mean lateral maximum force of 31.7 ± 8.9 N, which increased (p = 0.71) to a mean of 36.4 ± 1.9 N after release.
Table 1.
Mean peak pressure in knees resurfaced with standard components and gender-specific components*
| Components | Before lateral release | After lateral release | ||
|---|---|---|---|---|
| Standard | Lateral | 1190.8 ± 462.1 | Lateral | 744.5 ± 581.5 |
| Medial | 463.2 ± 308.7 | Medial | 673.1 ± 586.6 | |
| Differential | p < 0.01 | Differential | p = 0.84 | |
| Gender-specific | Lateral | 634.5 ± 308.6 | Lateral | 836.1 ± 420.6 |
| Medial | 475.8 ± 184.5 | Medial | 550.4 ± 377.3 | |
| Differential | p = 0.20 | Differential | p = 0.10 | |
* Data in kPa.
Table 2.
Mean maximum force in knees resurfaced with standard components and gender-specific components*
| Components | Before lateral release | After lateral release | ||
|---|---|---|---|---|
| Standard | Lateral | 46.5 ± 12.9 | Lateral | 31.7 ± 23.7 |
| Medial | 16.9 ± 9.3 | Medial | 21.7 ± 17.3 | |
| Differential | p < 0.01 | Differential | p = 0.42 | |
| Gender-specific | Lateral | 31.7 ± 8.9 | Lateral | 36.4 ± 1.9 |
| Medial | 16.2 ± 5.4 | Medial | 19.6 ± 10.6 | |
| Differential | p < 0.01 | Differential | p = 0.01 | |
* Data in Newtons.
Discussion
Patellar maltracking in total knee replacement currently is determined by a subjective ROM examination performed intraoperatively. Although various evaluation methods have been proposed, the current techniques in judging maltracking are not free of error [3, 18]. Our pilot study quantified forces and pressures across the patellofemoral joint and analyzed the effect of lateral release on these measurements.
The limitations of this study include the following. First, we had a small sample size of six knees. A small sample size, particularly for the standard component resurfaced knees with lateral release and gender-specific resurfaced knees without lateral release groups, limits our ability to interpret and generalize our findings. In these two groups, three knees were studied, whereas six knees were studied for all other groups. This discrepancy arose from the nature of the investigation, mainly that bone cuts and lateral releases could not be undone. The small numbers also create a risk of a Type II error in some trends. Second, we used fresh-frozen cadavers. The use of fresh-frozen cadaver knees might not have produced forces and pressures that accurately represent a knee in a living person performing active ROM. However, this study was designed to simulate operative conditions using passive ROM, without the influence of quadriceps action, to judge patellar tracking. Third, anatomic variations in the knees might have affected the data and the tissue tensions in these specimens might differ from those in patients undergoing TKAs. No knees among these cadavers had severe contracture, deformity, or large osteophytes. However, not all patients who undergo a TKA necessarily have these abnormalities. Therefore, the knees we studied at least simulate conditions seen in a substantial group of patients undergoing TKAs. Fourth, we used only domed patellar components. Domed patellar components might have produced results that are not applicable to asymmetric designs. Asymmetric designs might alter the alignment of the patellofemoral joint and therefore change pressure and force differentials. Most of the patellar components used in our practice, however, are symmetric domes. Fifth, we used a sensor that overlies the patellar component. Suturing the sensor to the soft tissue might have affected measurements as well; however, the sensor used in our study is more reliable than those used in another study [10]. The sensor might have changed the properties of the patellofemoral joint typically seen after TKA because the sensor was interposed between the femoral and patellar components. Sixth, implanting standard components first, then recutting the femur for gender-specific implants, might have affected the data recorded. This process was enacted to maximize the number of conditions with a limited number of specimens while still maintaining the knee in an otherwise unchanged state. Finally, the exclusive use of components from one manufacturer might have produced unique pressure and force differentials not generalizable to knees resurfaced with components from other manufacturers. Further comparative studies are needed to clarify this issue.
We questioned whether lateral to medial differentials in patellofemoral forces and pressures were observed. The findings from this study, in which knees were taken through passive ROM, do not completely agree with those from studies of simulated active ROM. We found lateral peak pressure to be greater than mean medial peak pressure for standard and gender-specific resurfaced unreleased knees. Xu et al. [19] studied lateral and medial patellofemoral pressures in standard component resurfaced knees in various stages of active flexion (Table 3) and reported that lateral peak pressure was greater than medial peak pressure only with the knee actively flexed to 60º. Peak pressure was greater medially than laterally at 30º, 90º, and 120º flexion. We also observed lateral maximum force to be greater than medial maximum force for standard and gender-specific resurfaced unreleased knees. Browne et al. [2] studied lateral and medial patellofemoral forces in standard component resurfaced knees in various stages of active flexion (Table 4) and reported that lateral maximum force was greater than medial maximum force once the knee was flexed beyond approximately 50º. After this point, the differential continued to increase as the knee was flexed up to 90º. However, at no point of flexion was the force differential statistically significant. These comparisons suggest active quadriceps contraction might substantially alter patellofemoral pressures and forces from those observed during passive ROM.
Table 3.
Comparison of data from two studies*
| Study | Lateral pressure | Medial pressure | Pressure differential (lateral-medial) | |||
|---|---|---|---|---|---|---|
| Xu et al. [18] | 30º | 49.77 ± 35.69 | 30º | 62.84 | 30º | − 13.07 |
| 60º | 77.59 ± 31.66 | 60º | 59.57 | 60º | + 18.02 | |
| 90º | 94.69 ± 23.46 | 90º | 95.59 | 90º | − 0.90 | |
| 120º | 107.83 ± 13.71 | 120º | 109.71 | 12 º | − 1.88 | |
| Current study | SCK | 1.19 ± 0.46 | SCK | 0.46 ± 0.31 | SCK | + 0.73 ± 0.55 |
| GSK | 0.63 ± 0.31 | GSK | 0.48 ± 0.18 | GSK | + 0.16 ± 0.36 | |
* Data in MPa; GSK = knees resurfaced with gender-specific components; SCK = knees resurfaced with standard components.
Table 4.
Comparison of two studies
| Study | Force differential (lateral-medial)* | |
|---|---|---|
| Browne et al. [2]† | 0º | − 20 |
| 15º | − 20 | |
| 30º | − 20 | |
| 45º | − 10 | |
| 60º | + 10 | |
| 75º | + 20 | |
| 90º | + 25 | |
| Current study | SCK | + 29.6 ± 15.9 |
| GSK | + 15.5 ± 10.4 | |
* Data in Newtons; †numbers are approximated from figure (no table with exact values was available); GSK = knees resurfaced with gender-specific components; SCK = knees resurfaced with standard components.
The second purpose of this investigation was to observe what quantitative effect, if any, lateral release had on force and pressure differentials across the patellofemoral joint. We found lateral peak pressure greater than medial peak pressure after lateral release in knees resurfaced with standard and gender-specific components. Mean total peak pressure decreased by 236.4 ± 1000 kPa after lateral release in standard resurfaced knees, but it increased by 276.2 ± 670 kPa after lateral release in gender-specific resurfaced knees. Ostermeier et al. [13] reported lower total peak pressure in knees with lateral release than peak pressure in knees without lateral release up to 80º of active flexion (Table 5). Beyond this point, knees with lateral release had greater total mean peak pressure. Ostermeier et al. [13], however, did not study changes in lateral to medial pressure differentials attributable to lateral release.
Table 5.
Comparison of peak pressure findings*
| Study | Before lateral release | After lateral release | Pressure differential (after-before) | |||
|---|---|---|---|---|---|---|
| Ostermeier et al. [12] | 0º | 2.94 ± 1.86 | 0º | 2.82 ± 1.33 | 0º | − 0.12 ± 2.29 |
| 40º | 3.70 ± 1.38 | 40º | 3.35 ± 1.33 | 40º | − 0.35 ± 1.92 | |
| 80º | 3.75 ± 1.50 | 80º | 3.85 ± 1.38 | 80º | + 0.10 ± 2.04 | |
| 100º | 4.13 ± 1.84 | 100º | 4.53 ± 1.87 | 100º | + 0.40 ± 2.62 | |
| Current study | SCK | 1.65 ± 0.56 | SCK | 1.42 ± 0.83 | SCK | − 0.24 ± 1.00 |
| GSK | 1.11 ± 0.36 | GSK | 1.39 ± 0.57 | GSK | + 0.28 ± 0.67 | |
* Data in MPa; GSK = knees resurfaced with gender-specific components; SCK = knees resurfaced with standard components.
The findings observed in this pilot study, when compared with the relevant literature, present two areas for further investigation. First, how do peak pressure and maximum force differentials change between passively flexed knees and actively flexed knees? Such a study could indicate how relationships observed intraoperatively relate to relationships seen in the patient after surgery. Second, why did lateral release change statistically significant pressure and force differentials into statistically nonsignificant differentials for standard resurfaced knees but not for gender-specific resurfaced knees? The current observations might indicate greater efficacy of lateral release in knees resurfaced with standard components than with gender-specific components. Investigation of the different kinematic effects of gender-specific components, when compared with standard components, might indicate areas for further implant improvement and innovation.
Acknowledgment
We thank Diana Winters for technical expertise in editing this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Drexel University College of Medicine.
References
- 1.Armitage P, Berry G, Matthews JN. Statistical Methods in Medical Research. Malden, MA: Blackwell; 2002. pp. 272–306. [Google Scholar]
- 2.Browne C, Hermida JC, Bergula A, Colwell CW, Jr, D’Lima DD. Patellofemoral forces after total knee arthroplasty: effect of extensor moment arm. Knee. 2005;12:81–88. doi: 10.1016/j.knee.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Cho WS, Woo JH, Park HY, Youm YS, Kim BK. Should the ‘no thumb technique’ be the golden standard for evaluating patellar tracking in total knee arthroplasty? Knee. 2011;18:177–179. doi: 10.1016/j.knee.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100–110. doi: 10.1097/01.blo.0000172303.74414.7d. [DOI] [PubMed] [Google Scholar]
- 5.Hsu HC, Luo ZP, Rand JA, An KN. Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty. 1997;12:74–83. doi: 10.1016/S0883-5403(97)90051-6. [DOI] [PubMed] [Google Scholar]
- 6.Johanson NA, Cerynik DL, Pasquale M. Measuring patellofemoral forces and pressures in a simulated operating room environment. J Arthroplasty. 2011;26:137–143. doi: 10.1016/j.arth.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Kusuma SK, Puri N, Lotke PA. Lateral retinacular release during primary total knee arthroplasty: effect on outcomes and complications. J Arthroplasty. 2009;24:383–390. doi: 10.1016/j.arth.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Leblanc J. Patellar complications in total knee arthroplasty: a literature review. Orthop Rev. 1989;18:296–304. [PubMed] [Google Scholar]
- 9.Lee K, Goodman SB. Current state and future of joint replacements in the hip and knee. Expert Rev Med Devices. 2008;5:383–393. doi: 10.1586/17434440.5.3.383. [DOI] [PubMed] [Google Scholar]
- 10.Martinelli L, Hurschler C, Rosenbaum D. Comparison of capacitive versus resistive joint contact stress sensors. Clin Orthop Relat Res. 2006;447:214–220. doi: 10.1097/01.blo.0000218730.59838.6a. [DOI] [PubMed] [Google Scholar]
- 11.Merican AM, Kondo E, Amis AA. The effect on patellofemoral joint stability of selective cutting of the lateral retinacular and capsular structures. J Biomech. 2009;42:291–296. doi: 10.1016/j.jbiomech.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Neter J, Kutner M, Wasserman W, Nachtsheim C. Applied Linear Statistical Models. Boston, MA: Irwin; 1990. pp. 712–780. [Google Scholar]
- 13.Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007;15:547–554. doi: 10.1007/s00167-006-0261-0. [DOI] [PubMed] [Google Scholar]
- 14.Outerbridge RE. The etiology of chondromalaciae patellae. J Bone Joint Surg Br. 1961;43:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 15.Ritter MA, Campbell ED. Postoperative patellar complications with or without lateral release during total knee arthroplasty. Clin Orthop Relat Res. 1987;219:163–168. [PubMed] [Google Scholar]
- 16.Schuh A, Hönle W. [Pathological finding and therapy for anterior knee pain following total knee arthroplasty][in German] Z Orthop Unfall. 2008;146:352–356. doi: 10.1055/s-2008-1038540. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer AI, Vince KG. Patellar considerations in total knee replacement. In: Scuderi G, editor. The Patella. New York NY: Springer; 1995. pp. 309–332. [Google Scholar]
- 18.Strachan RK, Merican AM, Devadasan B, Maheshwari R, Amis AA. A technique of staged lateral release to correct patellar tracking in total knee arthroplasty. J Arthroplasty. 2009;24:735–742. doi: 10.1016/j.arth.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Xu C, Chu X, Wu H. Effects of patellar resurfacing on contact area and contact stress in total knee arthroplasty. Knee. 2007;14:183–187. doi: 10.1016/j.knee.2007.01.005. [DOI] [PubMed] [Google Scholar]