Abstract
Background
Young, active, skeletally mature patients have higher failure rates after various surgical procedures, including stabilization for shoulder instability and primary ACL reconstruction. It is unclear whether young, active, skeletally mature patients share similarly high failure rates after revision ACL reconstruction.
Questions/purposes
We therefore determined whether revision ACL reconstruction restores knee stability and allows young (younger than 18 years), active, skeletally mature patients to return to preinjury activity levels.
Patients and Methods
We retrospectively identified 36 patients who had an initial ACL reconstruction between the ages of 12 and 17 years (mean, 15.4 years) and subsequent revision between the ages of 13 and 18 years (mean, 16.9 years); of these, 2-year followup was available for 21 (75%). Mechanisms of primary graft failure included traumatic rerupture (23 noncontact, seven contact), persistent instability (five), and infection (one). One patient had open physes at the time of revision. All revisions were single-stage transosseous reconstructions. The minimum followup was 24 months (mean, 36 months; range, 24–63 months).
Results
At last followup, 19 of 21 patients had a negative or IA Lachman and 20 of 21 had a negative pivot shift. Mean International Knee Documentation Committee subjective score was 89 (range, 64–99). Eleven of the 21 patients returned to the same or higher activity/sport level as before their original injury. Two patients reported subjective knee instability, with two having repeat revision reconstruction for failure.
Conclusions
Single-stage transosseous revision ACL reconstruction in young, active, skeletally mature patients restores knee stability but returns only 52% of patients to their prior level of activity or sport.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The incidence of ACL rupture in adolescents and young adults is reportedly 60.9 per 100,000 persons per year [21]. Population-based studies show the most important risk factor for an ACL injury in a young, skeletally mature patient is increased activity level [21]. Indications for ACL reconstruction in these younger patients include symptomatic instability and a desire to return to high-level activities involving pivoting and/or cutting maneuvers. One study showing rates of subsequent chondral and meniscal injuries of 68% and 79%, respectively, at 20 years in young athletes who return to sports with an ACL-deficient knee further supports the recommendation for ACL reconstruction in these patients [19].
ACL reconstruction in skeletally immature pediatric patients, via both transphyseal and physeal-sparing techniques, reportedly restores knee stability and returns 88% to 100% of patients to their preinjury levels of activity [4, 15–18]. Similar average levels of return to activity are present for primary ACL reconstruction in adults [2, 27]. Despite the relative success of primary ACL reconstructions, a percentage of these procedures fail. Without explicitly defined criteria for graft failure, the true incidence is difficult to determine. Many things are perceived as “graft failure,” including recurrent objective laxity, subjective knee instability, infection, knee pain/stiffness, and/or inability to return to preinjury activity levels. The causes of graft failure can be technical, biologic, or related to patient comorbidities. In skeletally immature patients, failure rates range from 0% to 12.5% [16, 18, 26]. Survivorship of ACL grafts in adolescent patients at 5 years is 93% in one report [24].
Compared to the results seen in primary ACL reconstruction, revision ACL reconstructions, while limited in the literature and diluted by heterogeneity of graft and fixation choices, are less successful. In studies with patients of various ages, up to 40% of patients undergoing revision ACL reconstruction are unable to return to their preinjury levels of competition [1, 5, 9, 20, 23]. It is unclear whether revision ACL reconstruction in a young, active, skeletally mature patient population would yield similar results, as there is no study in the literature reporting on ACL reconstruction for this isolated patient cohort. Therefore, we have to look to other literature for insight. For example, in young, active patients with shoulder instability, numerous studies implicate patient age and activity level as risk factors for Bankart repair failure and recurrent dislocation [11, 14, 22, 28]. Specifically, studies find recurrent dislocation after shoulder stabilization to be higher in patients younger than 20 years old when compared to patients in their 20s and 30s [11, 28].
Therefore, we (1) determined whether revision ACL reconstruction restores knee stability in athletes 18 years old and younger who were active and skeletally mature; (2) determined the ability of these patients to return to preinjury activity levels after revision ACL reconstruction; and (3) reported the incidence of revision ACL reconstruction failure in this patient cohort.
Patients and Materials
We reviewed our hospital’s operative records to identify all 36 patients who had revision ACL reconstructions between the ages of 12 and 18 years of age since 1995 (Table 1). At the time of primary reconstruction, the physes were open (both femur and tibia) in 10 patients (28%), closed in 19, partially open in four (either tibia or femur open), and unknown in three. Patients underwent primary ACL reconstructions at our institution (28 patients) or an outside facility (eight patients). For patients who underwent primary reconstruction elsewhere, we reviewed clinical office notes and radiographs or MRI (where available) to determine the growth status of the distal femoral and proximal tibial physes. There were 22 girls and 14 boys. The mean patient age at the time of revision ACL reconstruction was 16.9 years (range, 13–18 years), with open distal femoral and proximal tibial physes in one patient. The mean time between primary and revision reconstruction was 18 months (range, 3.5–49 months). Mechanism of failure or reason for revision of these primary grafts included traumatic rerupture in 30 patients (23 noncontact reinjuries, seven contact reinjuries), persistent instability in five, and infection in one (Table 2). At the time of primary reconstruction, 13 patients (36%) underwent additional procedures for concomitant injuries, and during revision reconstruction, 20 patients (56%) underwent additional surgeries (Table 3).
Table 1.
Patient characteristics and perioperative details for primary ACL reconstruction
| Patient | Gender | Age (years, months) | Status of physes* | Primary ACL graft† | Tunnel technique | Method of fixation‡ | |
|---|---|---|---|---|---|---|---|
| Femur | Tibia | ||||||
| 1 | Female | 15, 4 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 2 | Female | 17 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 3 | Male | 15, 7 | Open | HS auto | Transphyseal | Eb | B Ifsc + W |
| 4 | Male | 15, 8 | Open | HS auto | Transphyseal | Eb | St |
| 5 | Male | 14, 2 | Open | HS auto | Transphyseal | Eb | St |
| 6 | Male | 15, 3 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 7 | Female | 15, 4 | Closed | Tib post allo | Transphyseal | B Isfc | B Ifsc |
| 8 | Female | 15, 5 | Open | Tib ant allo | Transphyseal | M Ifsc | B Ifsc |
| 9 | Male | 15 | Closed | HS auto | Transphyseal | St | St |
| 10 | Female | 16 | Closed | HS auto | Transphyseal | B Ifsc | B Ifsc |
| 11 | Male | 16 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 12 | Female | 13, 2 | Open | HS auto | Partial transphyseal | St | St |
| 13 | Male | 17, 11 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 14 | Female | 16, 2 | Closed | HS auto | Transphyseal | M Ifsc | M Ifsc + post |
| 15 | Female | 14 | Unknown | HS auto | Transphyseal | Eb | M Ifsc |
| 16 | Female | 13, 7 | Unknown | Achilles allo | Transphyseal | Eb | B Ifsc |
| 17 | Male | 17 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 18 | Female | 15. 8 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc + Eb |
| 19 | Female | 16 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 20 | Male | 16 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 21 | Female | 15, 7 | Closed | HS auto | Transphyseal | B Ifsc | B Ifsc |
| 22 | Female | 14, 5 | Open | HS auto | Partial transphyseal | St | St |
| 23 | Male | 16 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 24 | Female | 15 | Closed | BTB auto | transphyseal | M Ifsc | B Ifsc |
| 25 | Male | 15 | Open | HS auto | Physeal-sparing | St | St |
| 26 | Female | 14, 9 | Unknown | Achilles allo | Transphyseal | M Ifsc | B Ifsc + St |
| 27 | Male | 17 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 28 | Female | 13, 4 | Open | HS auto | Transphyseal | Eb | St |
| 29 | Female | 14, 11 | Partial (femur) | BTB auto | Transphyseal | M Ifsc | M Ifsc + Eb |
| 30 | Female | 15, 9 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 31 | Female | 14, 8 | Partial (tibia) | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 32 | Male | 17, 9 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 33 | Female | 14, 8 | Partial (femur) | HS auto | Transphyseal | Eb | Post + W |
| 34 | Female | 14, 6 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 35 | Male | 14, 8 | Open | HS auto | Physeal-sparing | St | St |
| 36 | Female | 12, 11 | Open | Achilles allo | Physeal-sparing | St | St |
* Open = both femur and tibial physes; closed = both femur and tibial physes; partial = tibia or femur shown in parentheses indicates this physis was open; †BTB auto = bone-patella tendon-bone autograft; HS auto = hamstring tendon autograft; Achilles allo = Achilles tendon allograft; tib post allo = tibialis posterior allograft; tib ant allo = tibialis anterior allograft; ‡M Ifsc = metal interference screw; Eb = endobutton; St = staple; B Ifsc = biointerference screw; W = washer
Table 2.
Reasons for revision ACL reconstruction
| Mechanism of failure | Number of patients |
|---|---|
| Traumatic rerupture (noncontact) | 23 (64%) |
| Traumatic rerupture (contact) | 7 (19%) |
| Persistent instability | 5 (14%) |
| Infection | 1 (3%) |
Table 3.
Concomitant procedures performed during primary and revision ACL reconstruction
| Procedure | Primary surgery (number of patients) | Revision surgery (number of patients) |
|---|---|---|
| Partial meniscectomy (lateral) | 5 | 6 |
| Partial meniscectomy (medial) | 4 | 8 |
| Meniscal repair (medial) | 4 | 5 |
| Meniscal repair (lateral) | 2 | 2 |
| Chondroplasty | 1* | 1* |
| Microfracture | 0 | 1* |
| Removal loose body | 0 | 1 |
* Procedure performed on the medial femoral condyle
Surgeons performed all surgeries (primary and revision) arthroscopically. Surgeon preference dictated the type of graft chosen for the revision and the technique that they selected included transosseous tibial and femoral tunnels in all 36 patients (Table 4). Graft choice for the primary ACL reconstruction consisted of 28 autografts (15 bone-patella tendon-bone [BTB], 13 hamstring tendon [HS]) and eight allografts (six Achilles tendon, one tibialis posterior, one tibialis anterior). Grafts utilized for revision included 17 autografts (16 BTB, one hamstring tendon) and 19 allografts (18 Achilles tendon, one BTB). Surgeons performed all revisions in a single stage, except one (Patient 25), which they performed in a two-stage fashion due to infection. Only one patient, with a vertical femoral tunnel, had bone grafting.
Table 4.
Patient characteristics and perioperative details for revision ACL reconstruction
| Patient | Age (years, months) | Status of physes* | Revision ACL graft† | Tunnel technique | Methods of fixation‡ | |
|---|---|---|---|---|---|---|
| Femur | Tibia | |||||
| 1 | 17, 3 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc + Eb |
| 2 | 18 | Closed | Achilles allo | Transphyseal | M Ifsc | Screw + W |
| 3 | 16, 6 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 4 | 16, 10 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 5 | 17, 2 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc + Eb |
| 6 | 16, 7 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc + Eb |
| 7 | 16, 6 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 8 | 16, 10 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 9 | 18 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 10 | 17 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 11 | 17 | Closed | BTB allo | Transphyseal | M Ifsc + Eb | M Ifsc + Eb |
| 12 | 15, 4 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 13 | 18, 4 | Closed | Achilles allo | Transphyseal | M Ifsc | M Ifsc + Eb |
| 14 | 18, 5 | Closed | Achilles allo | Transphyseal | B Ifsc + Eb | M Ifsc + Eb |
| 15 | 17 | Closed | Achilles allo | Transphyseal | B Ifsc | B Ifsc |
| 16 | 17, 8 | Closed | Achilles allo | Transphyseal | B Ifsc | B Ifsc |
| 17 | 18 | Closed | BTB auto | Transphyseal | M Ifsc | B Ifsc |
| 18 | 17 | Closed | Achilles allo | Transphyseal | B Ifsc | M Ifsc |
| 19 | 17 | Closed | Achilles allo | Ttransphyseal | M Ifsc | B Ifsc |
| 20 | 17 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 21 | 15, 10 | Closed | HS auto | Transphyseal | Eb | B Ifsc |
| 22 | 15, 3 | Closed | BTB auto | Ttransphyseal | M Ifsc | M Ifsc |
| 23 | 16 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc + St |
| 24 | 16 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 25 | 15 | Open | Achilles allo | Transphyseal | M Ifsc | M Ifsc |
| 26 | 17 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 27 | 17, 7 | Closed | Achilles allo | Transphyseal | M Ifsc | B Ifsc |
| 28 | 14, 4 | Closed | Achilles allo | Transphyseal | M Ifsc | M Ifsc |
| 29 | 18 | Closed | Achilles allo | Transphyseal | M Ifsc | M Ifsc |
| 30 | 16, 9 | Closed | Achilles allo | Transphyseal | M Ifsc | M Ifsc |
| 31 | 16, 2 | Closed | Achilles allo | Transphyseal | M Ifsc | M Ifsc |
| 32 | 18, 5 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 33 | 15, 5 | Closed | BTB auto | Ttransphyseal | M Ifsc | M Ifsc |
| 34 | 17, 7 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 35 | 16, 6 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
| 36 | 13, 11 | Closed | BTB auto | Transphyseal | M Ifsc | M Ifsc |
* Open = both femur and tibial physes; closed = both femur and tibial physes; † BTB auto = bone-patella tendon-bone autograft; BTB allo = bone-patella tendon-bone allograft; HS auto = hamstring tendon autograft; Achilles allo = Achilles tendon allograft; ‡ M Ifsc = metal interference screw; B Ifsc = biointerference screw; Eb = endobutton; W = washer; St = staple
Of the original 36 patients, we excluded eight patients due to their date of surgery being within the last 2 years. This left 28 patients, but we were unable to contact seven patients, leaving a final study sample of 21 patients (75%) for inclusion with a mean age of 17 years (range, 13–18 years). The minimum clinical followup was 24 months (mean, 36 months; range, 24–63 months). We obtained prior approval for this case series from our institutional review board.
The postoperative rehabilitation program at our institution consisted of five phases spanning 22 weeks, beginning with patella mobilization and normalizing knee ROM, followed by re-establishing normal gait, improving quadriceps strength and control, restoring flexibility and agility, and gradually returning to functional activity and running. Criteria for completion of the program included performing a hop test at greater than 85% of the contralateral normal side, lack of apprehension with sport-specific movements, and acceptable flexibility for levels of sport performance. We required patients to complete the program before returning to sports.
We conducted routine office followups at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year, with variability thereafter. We assessed clinical outcomes using the latest physical examinations documented in the office notes and telephone interviews. Physical examination, conducted by an attending surgeon, consisted of inspection and palpation for the presence of an effusion, knee ROM, the Lachman examination for anterior translation [10], and the pivot shift test. We assessed patient-based outcomes using the International Knee Documentation Committee (IKDC) subjective knee evaluation form as a validated measure of function and limitations/symptoms related to sports activity [12]. We also asked patients to subjectively evaluate their pain at rest, during activity, and during sports using a numerical pain rating scale from 0 (no pain) to 10 (worst pain). Finally, we used a questionnaire to evaluate subjective instability of the knee and episodes of knee swelling. We assessed patient activity level and participation in sports using the IKDC subjective knee evaluation form and by directly questioning patients on their level of sports competition before primary reconstruction, between primary and revision surgeries, and at latest followup. We defined levels of activity as Level 0 (unable due to knee pain), Level 1 (light, ie, walking), Level 2 (moderate, ie, running), Level 3 (strenuous, ie, skiing or tennis), or Level 4 (very strenuous, ie, jumping or pivoting sports). We classified level of competition as (1) recreational, (2) intramural/low-level organized team sports, (3) high school/college team sports, and (4) elite/professional team participation. Before primary ACL reconstruction, 34 patients (94.4%) participated in sports at the high school/college level or higher (Level 3 or 4). Before revision reconstruction, 24 patients (71%) returned to Level 3 or 4 sports.
We reviewed operative reports from the primary reconstructions for documentation of graft type, graft fixation, reconstructive technique (transphyseal, partial transphyseal, physeal-sparing), and concomitant procedures performed for concurrent injuries. In addition to the above operative details, we reviewed the operative reports from the revision surgeries to determine the necessity for bone graft, type of bone graft, and whether the revision was single- or two-staged. We obtained the reason for failure of the primary graft from prerevision clinic notes and the indications section of the revision operative reports.
We calculated descriptive statistics for discrete variables of interest, using means and SDs to evaluate continuous variables, and frequency tables to examine categorical and binary outcome variables. Only patients with complete data were included in the study and analyses. We performed all statistical analyses using SPSS® Version 16.1 (SPSS Inc, Chicago, IL).
Results
On physical examination at latest followup, the Lachman test was classified as symmetric to the contralateral knee in 13 of the 21 patients (62%), Grade IA (≤ 5 mm of anterior translation difference from the contralateral side with an end point) in six patients (29%), Grade IB (≤ 5 mm of difference from the contralateral side without an end point) in one patient, and Grade IIB (> 5 mm of difference from the contralateral side without an end point) in one patient. The patient with the Grade IIB Lachman also had a 2 + positive pivot shift on physical examination, whereas the remaining 20 patients (95%) had negative pivot shift tests. Two patients reported subjective episodes of instability (10%).
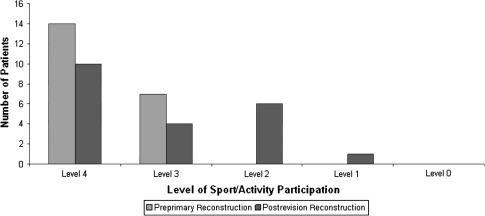
The mean IKDC subjective score was 89 ± 9.0 points (range, 64–99 points) (Fig. 1). Of the 21 patients, 10 (48%) reported regular participation in Level 4 activities, four (19%) in Level 3, six (29%) in Level 2, and one (5%) in Level 1. No patients reported being unable to perform any activity due to knee pain (Level 0). At latest followup, 11 patients (52%) had returned to the same or higher activity/sport level as before their original injury and primary ACL reconstruction (Fig. 1).
Fig. 1.
A graph shows the level of sport/activity participation before primary ACL reconstruction and at latest followup after revision ACL reconstruction. IKDC definitions of sport/activity levels are as follows: Level 0 = unable to perform activities due to knee pain, swelling, or instability; Level 1 = light activities such walking, housework, or yard work; Level 2 = moderate activities such as moderate physical work, running, or jogging; Level 3 = strenuous activities such as heavy physical work, skiing, or tennis; and Level 4 = very strenuous activities such as jumping or pivoting as in basketball or soccer
Two of the 21 revision ACL reconstructions (9.5%) had repeat revision reconstruction for failure. The first was a high school soccer player who underwent primary ACL reconstruction with HS autograft at age 14 years and reruptured the graft twice (the first time while running down the field, the second time suffering a twisting injury to the knee on turf surface). She underwent revision reconstruction both times with Achilles tendon allograft. Eighteen months after her second revision, her subjective IKDC score was 68.9, and due to pain, she was participating in only Level 1 activities despite a negative Lachman and negative pivot shift. The second patient was a 15-year-old high-school lacrosse player. He underwent primary ACL reconstruction with ipsilateral BTB autograft, followed by revision with contralateral BTB autograft due to traumatic rerupture during a contact injury. His graft failed a second time, related to a fall down stairs, but the patient decided to forego a second revision. At latest followup, the patient’s IKDC score was 86.2 and he subjectively returned to Level 4 activities despite a IIB Lachman on physical examination. None of the eight patients we excluded because they underwent revision reconstruction within the last 2 years had failed at the time we prepared this article. Of the seven patients we were unable to contact, none had repeat revision before being lost to followup.
Discussion
Young, active patients represent a challenging population for the sports medicine surgeon. The reason for this is that patient age and activity level are risk factors for failure of a number of surgical procedures, particularly shoulder stabilization and ACL reconstruction [3, 11, 28]. In one series, a patient aged younger than 20 years increases the risk of recurrent shoulder dislocation after arthroscopic repair of anteroinferior glenohumeral instability [11, 28]. Another series on primary ACL reconstructions notes patients with higher activity levels are more likely to experience graft failure than those who are less active (odds ratio, 4.33) [3]. Given this, it seems inevitable that many surgeons face performing revision ACL reconstructions in young, active, skeletally mature patients. However, the results of this procedure are largely unknown and not reported in the literature for an isolated cohort of patients. This study was undertaken to examine the ability of revision ACL reconstruction to restore knee stability and return athletes to preinjury activity levels, particularly in this active patient population aged 18 years or younger.
Our study is subject to a number of limitations. First, limited data in patient records related to this study’s retrospective nature may have introduced selection bias in our inclusion of patients. However, the rarity of this procedure in a patient population with a narrow age range necessitates a retrospective study design. Second, our followup is limited to only 75%, which may be due to patient mobility during a transition time into adulthood, unique to this patient population. Third, we are unable to determine the rate of graft failure because a number of patients underwent primary reconstruction at outside institutions and the total number of reconstructions performed during the time period of this study is unknown.
Revision transosseous ACL reconstruction can restore subjective and objective knee stability in skeletally mature athletes 18 years old and younger. Ninety percent of our patients had a negative or IA Lachman at latest followup and 95% a negative pivot shift. Although no prior series on revision ACL reconstructions in young, active, skeletally mature patients exists in the literature, revision ACL reconstructions in adults show similar results to ours. Battaglia et al. [1] found less than 5 mm of anterior translation side-to-side difference in 83% of adult revisions, and Garofalo et al. [9] reported negative or IA Lachman results in 100% of 28 adult patients after revision ACL reconstruction. Only two patients (10%) in our study report episodes of subjective knee instability at followup.
The average IKDC subjective knee score in this series was 89 (± 9.0) points, similar to the IKDC results after primary ACL reconstruction in adolescents in Shelbourne et al. [26] (95.4 ± 6.9 points) and Kocher et al. [16] (89.5 ± 10.2 points). Despite restoration of objective and subjective knee stability after revision reconstruction, only 52% of patients in our study returned to the same level of sport/activity as before their original ACL injury. This is worse than the results after primary ACL reconstruction in adolescents. Ten of 11 (91%) adolescent patients in one series [25] and 16 of 16 adolescent patients in another series [26] returned to their preinjury sports activity levels after primary ACL reconstruction. Conversely, our findings are similar to those after revision reconstructions in adults, whereby between 56% and 78% of patients return to their preinjury activity levels [1, 5, 23].
We observed a failure rate of 9.5%: two of the 21 patients had a second revision ACL reconstruction. Of these two patients, one went on to fail yet again. Failure rates in adult revisions in the literature are difficult to interpret due to varying definitions of failure but range from 6% to 25% [1, 7, 8, 23]. Surgeons should counsel patients before revision reconstruction of the increased failure rate compared to primary ACL reconstruction, especially if contemplating a second or third revision.
Technical error at the time of primary reconstruction is a major factor in the etiology of ACL graft failure. Studies during the 1990s on revision ACL reconstruction in adults [13, 29] report technical error to be the most common reason for primary graft failure, and this is present in 22% to 79% of cases in more recent series [8, 20, 23]. In patients with early laxity where knee stability is not restored after reconstruction, this may certainly be the case, as in the five patients (13.5%) in our study. However, the most common reason for revision in our young, active patients is traumatic rerupture (83%) from both contact and noncontact reinjuries. In recent series of adults, the incidence of repeat trauma as the cause for graft failure ranges from 24% to 100% [5, 6, 9]. The wide range likely reflects the heterogeneity of graft failure definitions across studies, and there are no prior studies on adolescents for comparison. Nonetheless, the high incidence of repeat trauma in this series is somewhat expected considering the activity level of these young patients, with 94% participating in high-level high school or collegiate athletics at baseline.
Based on our observations, this series provides information that surgeons can utilize when discussing ACL treatment and revision surgery with young athletes and their families. Our results demonstrate revision ACL reconstruction can successfully restore stability in athletes who are 18 years old or younger. Nevertheless, these young athletes and their families can expect inferior results compared with those of their primary reconstruction, and nearly ½ of these athletes may not return to compete at the same level in their sport.
Acknowledgments
The authors thank Answorth Allen, MD, David Altchek, MD, Robert Marx, MD, Scott Rodeo, MD, Russell Warren, MD, and Thomas Wickiewicz, MD, for their contributions of patients to this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Hospital for Special Surgery.
References
- 1.Battaglia MJ, 2nd, Cordasco FA, Hannafin JA, Rodeo SA, O’Brien SJ, Altchek DW, Cavanaugh J, Wickiewicz TL, Warren RF. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35:2057–2066. doi: 10.1177/0363546507307391. [DOI] [PubMed] [Google Scholar]
- 2.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 3.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362–2367. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 4.Cohen M, Ferretti M, Quarteiro M, Marcondes FB, Hollanda JP, Amaro JT, Abdalla RJ. Transphyseal anterior cruciate ligament reconstruction in patients with open physes. Arthroscopy. 2009;25:831–838. doi: 10.1016/j.arthro.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Denti M, Lo Vetere D, Bait C, Schonhuber H, Melegati G, Volpi P. Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med. 2008;36:1896–1902. doi: 10.1177/0363546508318189. [DOI] [PubMed] [Google Scholar]
- 6.Diamantopoulos AP, Lorbach O, Paessler HH. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36:851–860. doi: 10.1177/0363546507312381. [DOI] [PubMed] [Google Scholar]
- 7.Ferretti A, Conteduca F, Monaco E, Carli A, D’Arrigo C. Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88:2373–2379. doi: 10.2106/JBJS.F.00064. [DOI] [PubMed] [Google Scholar]
- 8.Fox JA, Pierce M, Bojchuk J, Hayden J, Bush-Joseph CA, Bach BR., Jr Revision anterior cruciate ligament reconstruction with nonirradiated fresh-frozen patellar tendon allograft. Arthroscopy. 2004;20:787–794. doi: 10.1016/S0749-8063(04)00812-6. [DOI] [PubMed] [Google Scholar]
- 9.Garofalo R, Djahangiri A, Siegrist O. Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy. 2006;22:205–214. doi: 10.1016/j.arthro.2005.08.045. [DOI] [PubMed] [Google Scholar]
- 10.Gurtler RA, Stine R, Torg JS. Lachman test evaluated: quantification of a clinical observation. Clin Orthop Relat Res. 1987;216:141–150. [PubMed] [Google Scholar]
- 11.Imhoff AB, Ansah P, Tischer T, Reiter C, Bartl C, Hench M, Spang JT, Vogt S. Arthroscopic repair of anterior-inferior glenohumeral instability using a portal at the 5:30-o’clock position: analysis of the effects of age, fixation method, and concomitant shoulder injury on surgical outcomes. Am J Sports Med. 2010;38:1795–1803. doi: 10.1177/0363546510370199. [DOI] [PubMed] [Google Scholar]
- 12.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 13.Johnson DL, Swenson TM, Irrgang JJ, Fu FH, Harner CD. Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res. 1996;325:100–109. doi: 10.1097/00003086-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Kim SH, Ha KI, Kim YM. Arthroscopic revision Bankart repair: a prospective outcome study. Arthroscopy. 2002;18:469–482. doi: 10.1053/jars.2002.32230. [DOI] [PubMed] [Google Scholar]
- 15.Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87:2371–2379. doi: 10.2106/JBJS.D.02802. [DOI] [PubMed] [Google Scholar]
- 16.Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89:2632–2639. doi: 10.2106/JBJS.F.01560. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. 2010;468:1971–1977. doi: 10.1007/s11999-010-1255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McIntosh AL, Dahm DL, Stuart MJ. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy. 2006;22:1325–1330. doi: 10.1016/j.arthro.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21:696–702. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med. 2006;34:553–564. doi: 10.1177/0363546505281812. [DOI] [PubMed] [Google Scholar]
- 21.Parkkari J, Pasanen K, Mattila VM, Kannus P, Rimpela A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med. 2008;42:422–426. doi: 10.1136/bjsm.2008.046185. [DOI] [PubMed] [Google Scholar]
- 22.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88:2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 23.Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K. Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med. 2006;34:1604–1614. doi: 10.1177/0363546506288015. [DOI] [PubMed] [Google Scholar]
- 24.Sankar WN, Carrigan RB, Gregg JR, Ganley TJ. Anterior cruciate ligament reconstruction in adolescents: a survivorship analysis. Am J Orthop (Belle Mead NJ) 2008;37:47–49. [PubMed] [Google Scholar]
- 25.Seon JK, Song EK, Yoon TR, Park SJ. Transphyseal reconstruction of the anterior cruciate ligament using hamstring autograft in skeletally immature adolescents. J Korean Med Sci. 2005;20:1034–1038. doi: 10.3346/jkms.2005.20.6.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shelbourne KD, Gray T, Wiley BV. Results of transphyseal anterior cruciate ligament reconstruction using patellar tendon autograft in Tanner stage 3 or 4 adolescents with clearly open growth plates. Am J Sports Med. 2004;32:1218–1222. doi: 10.1177/0363546503262169. [DOI] [PubMed] [Google Scholar]
- 27.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 28.Voos JE, Livermore RW, Feeley BT, Altchek DW, Williams RJ, Warren RF, Cordasco FA. Allen AA; HSS Sports Medicine Service. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 29.Wirth CJ, Kohn D. Revision anterior cruciate ligament surgery: experience from Germany. Clin Orthop Relat Res. 1996;325:110–115. doi: 10.1097/00003086-199604000-00012. [DOI] [PubMed] [Google Scholar]