Abstract
Background
Posterior cruciate ligament injuries can occur as isolated ligament ruptures or in association with the multiligament-injured knee. Delayed reconstruction, at 2–3 weeks post-injury, is predominantly recommended for posterior cruciate ligament tears in the multiligament-injured knee. While acute bone and soft tissue avulsion patterns of injury can be amenable to repair, the described techniques have been associated with some difficulties attaching the avulsed ligament.
Description of Technique
As part of a reconstruction/repair of a multiligament-injured knee, we performed arthroscopic primary repair of the posterior cruciate ligament by passing Bunnell-type stitches into the substance of the ligament using a reloadable suture passer. We then passed the sutures through drill holes into the femoral footprint of the ligament and tied them over a bony bridge.
Patients and Methods
We retrospectively reviewed three patients with posterior cruciate ligament tears associated with a multiligament-injured knee. All patients had posterior cruciate ligament soft tissue avulsions or “peel off” injuries diagnosed by MRI. The described repair technique was used to repair the posterior cruciate ligament avulsion. Minimum followup was 64 months (mean, 68 months; range, 64–75 months). ROM, stability testing, and functional outcome scores (Lysholm and modified Cincinnati) were recorded.
Results
Mean ROM was 0° to 127°. Posterior drawer testing was negative in all three patients. The mean Lysholm score was 92 and the mean modified Cincinnati score was 94. Followup MRI confirmed ligament healing in all patients.
Conclusions
We believe arthroscopic posterior cruciate ligament repair for soft tissue peel off injuries is a technique that, when applied to carefully selected patients, may be helpful to the surgeon treating patients with a multiligament-injured knee.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-011-2034-4) contains supplementary material, which is available to authorized users.
Introduction
Posterior cruciate ligament (PCL) injuries of the knee can occur as isolated ligament ruptures or in association with a multiligament-injured knee (MLIK). Surgery is generally reserved for isolated injuries with Grade 3 laxity or with a MLIK [17–19, 21]. Recent literature regarding surgical management focuses almost entirely on delayed ligament reconstruction rather than acute repair [2, 3, 5, 7, 32, 40].
The majority of recently published articles related to repair of the PCL focus on the open and arthroscopic repair of PCL avulsion fractures and could be more accurately described as fracture fixation rather than ligament repair [6, 13–15, 41]. However, one case series from the 1990s, reported in 2002 by Wheatley et al. [39], described an arthroscopic repair of PCL soft tissue avulsions. The authors used a Caspari suture punch (Biomet Inc, Warsaw, IN) to pass multiple nonabsorbable monofilament sutures through the PCL stump in different planes. They reported on 13 patients, with International Knee Documentation Committee (IKDC) scores of normal or near normal in the 11 repairs available for followup at an average of 51 months [39].
We describe a modification to the technique of Wheatley et al. [39], using modern arthroscopic instrumentation borrowed from the rotator cuff sets, to repair soft tissue avulsions of the PCL and reviewed three patients to determine whether (1) femoral “peel off” type soft tissue avulsions can be identified by preoperative MRI; (2) the peel off avulsion is amenable to arthroscopic repair; (3) the described technique restores ROM, stabilizes the knee to posterior drawer testing, and returns patients to a pain-free functional status; and (4) the technique has a low complication rate.
Surgical Technique
Once the patient was indicated, surgery was performed 2 to 3 weeks after injury to allow capsular healing that minimized extravasation of irrigation fluid and enabled maintenance of arthroscopic fluid pressure. Further delays would result in a time-dependent decrease in tissue quality and ligament length.
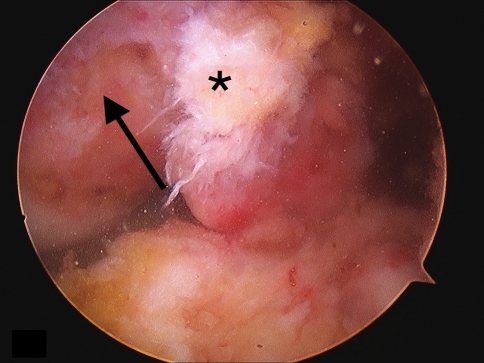
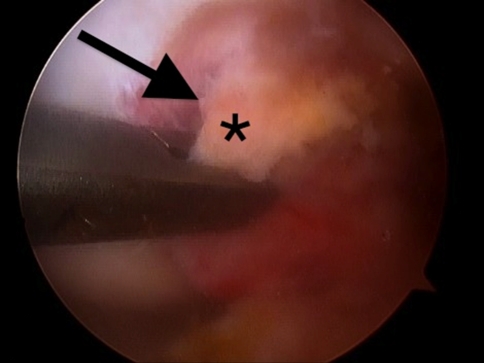
Anterolateral viewing and anteromedial working portals were created in standard fashion. General inspection of the knee and workflow were planned. When addressed, the PCL was inspected, mobilized, and gently débrided (Fig. 1). Using the grasper, the free end of the PCL was assessed to confirm there were both adequate tissue quality and length required for the repair technique (Fig. 2).
Fig. 1.
The PCL stump (asterisk) is avulsed from its insertion at the footprint on the medial femoral condyle (arrow).
Fig. 2.
A trial reduction of the PCL (asterisk) is made with a grasper to its footprint on the medial femoral condyle (arrow).
Posterior sag is commonplace with PCL injuries, more so in the setting of the MLIK. Therefore, great care was taken to ensure the knee was properly reduced in the sagittal plane when assessing ligament length. If the posterior sag was not reduced, the ligament appeared of insufficient length when, in fact, it was adequate for repair.
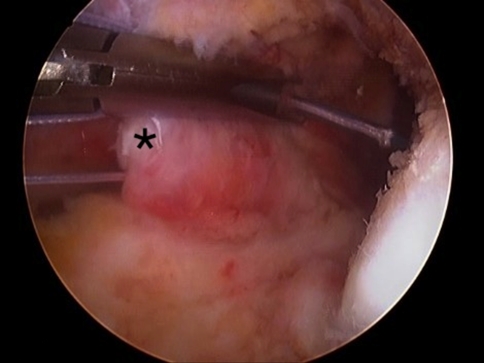
Most often, the repair was performed through standard anterior portals; however, accessory portals were made as required. A large-bore cannula, preferably malleable (PassPort® Cannula; Arthrex, Inc, Naples, FL), was extremely helpful in the anteromedial working portal to enable easier suture management. Next, a reloadable suture passing device (Scorpion®; Arthrex) was used to pass a newer-generation polyester suture (Number 2 FiberWire®; Arthrex) through the ligament substance as close to the tibial insertion as possible (Fig. 3).
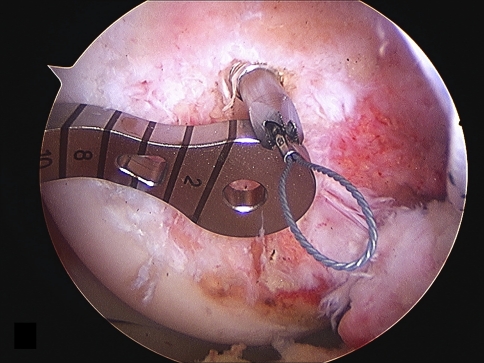
Fig. 3.
The Scorpion® suture passer is used to pass a Number 2 TigerWire® (Arthrex) through the PCL base (asterisk).
Each suture limb was then sequentially reloaded into the device and passed across the ligament substance in opposite directions while advancing toward the free end of the ligament. The feel of the needle passage through the tissue was noted so as to avoid cutting or damaging the suture that was already passed. If substantial resistance was met, the suture passer was repositioned until resistance to passage was light. This created a Bunnell-type stitch allowing the limbs of the sutures to be interlocked to increase strength to pullout. Typically, three passes were made, thus enabling robust purchase in the tissue.
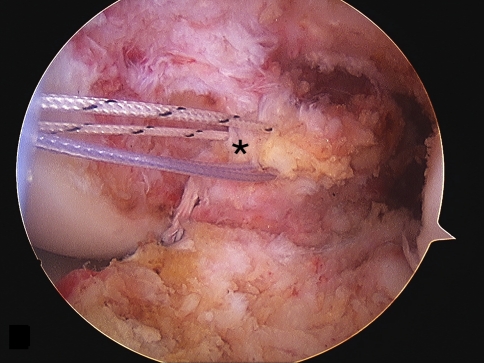
If individual bundles were identified, each was addressed separately; otherwise, the sutures were passed irrespective of bundles. In general, two sutures were passed per repair, resulting in four free suture limbs in a single-bundle repair (Fig. 4) and eight free suture limbs in a double-bundle repair. The sutures were protected by placing them through the anterolateral portal while the femoral footprint of the ligament was roughened with an arthroscopic burr.
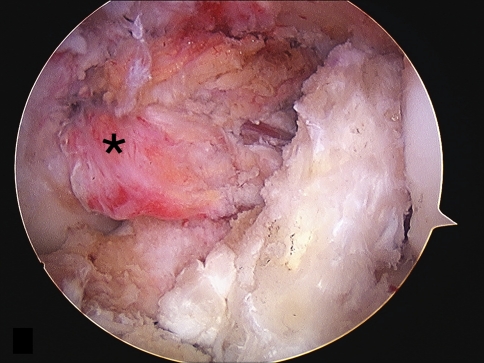
Fig. 4.
The image demonstrates both FiberWire® and TigerWire® sutures within the PCL stump (asterisk) without tension.
A cannulated drill (RetroDrill®; Arthrex) was then used with a PCL femoral guide (Constant PCL Guide; Arthrex) to encourage the drill to exit at the femoral footprint of the anterolateral bundle of the ligament. To allow the guide to be placed down to bone, a small incision was made over the medial femoral condyle. A nitinol passing wire was then shuttled down the cannulation of the drill to retrieve the repair sutures (Fig. 5). If cannulated instrumentation is not available, a standard 2.4-mm hole can be drilled and spinal needles can be used to pass the nitinol wire. We recommend all drill holes be made before suture retrieval so as to avoid damage to intraosseous sutures from errant drill passage during subsequent hole placement. If a double-bundle repair was performed, four drill holes were required, two at the anterolateral bundle femoral origin and two at the posteromedial bundle femoral origin; otherwise, only the two at the anterolateral femoral origin were utilized.
Fig. 5.
The nitinol passing wire is seen exiting the cannulated RetroDrill® next to the paddle of the RetroDrill® guide.
Once the repair sutures were passed, ligament tensioning was performed. An anterior drawer force was applied to the knee at 90° of flexion, reducing the tibia anatomically as confirmed by the step-off. Suture limbs were tensioned in pairs and tied together over the bone bridge between the drill holes. We currently prefer to use ligament buttons (RetroButton®; Arthrex) so as to minimize compression of the soft tissues at the bone bridge, which could otherwise result in increased laxity secondary to creep. Reduction of the ligament to the femoral origin during tensioning was visualized arthroscopically (Fig. 6), and a gentle posterior drawer examination was performed to confirm integrity of the repair. (For a demonstration of the surgical procedure, see Video 1 [supplemental materials are available with the online version of CORR].)
Fig. 6.
The final repair of the PCL (asterisk) is shown with complete coverage of the insertional footprint.
Patients and Methods
We retrospectively reviewed three patients with PCL avulsions associated with the MLIK treated with this repair technique from 2003 to 2010 who had minimum 24 months’ followup (Table 1). (For descriptions of individual patients, see Appendix 1 [supplemental materials are available with the online version of CORR].) The indications for this approach were (1) soft tissue avulsion of the PCL from the femur in the setting of a MLIK as identified on MRI; (2) confounding variables that limited more extensive surgery; and (3) adequate tissue length and quality as determined intraoperatively. During the study period, we treated seven patients with similar PCL injuries associated with a MLIK in this manner, but only the three included here had more than 24 months’ followup. The minimum followup of these three patients was 64 months (mean, 68 months; range, 64–75 months). Each patient was contacted for final followup and to fill out the objective outcome measures for this study; otherwise, all data were obtained from previous medical records and radiographs.
Table 1.
Patient data
| Patient | Age (years) | Wascher KD classification [38] | Injury pattern | Surgical intervention | Followup (months) | ROM (°) | Posterior drawer test | Lysholm knee score (points) | Modified Cincinnati knee score (points) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 33 | 5 (fracture/dislocation) | PCL (femoral avulsion) LCL PLC MMT |
PCL, LCL, and PLC primary repair | 75 | 0–125 | Negative | 92 | 90 |
| 2 | 17 | 2 (anterior) | PCL (femoral avulsion) ACL LCL MCL |
PCL primary repair | 64 | 0–120 | Negative | 95 | 96 |
| 3 | 18 | 5 (fracture/dislocation) | PCL (femoral avulsion) ACL MCL MRA |
ACL all-inside reconstruction; PCL, MCL and MRA primary repairs | 64 | 0–135 | Negative | 90 | 96 |
| Average | 23 | 68 | 0–127 | 92 | 94 |
KD = knee dislocation; PCL = posterior cruciate ligament; LCL = lateral collateral ligament; PLC = posterolateral corner; MMT = medial meniscal tear; ACL = anterior cruciate ligament; MCL = medial collateral ligament; MRA = meniscal root avulsion.
The patients in this series were all admitted at the time of initial injury for stabilization. They were then brought back for elective surgery at approximately 2 weeks postinjury. Postoperatively, the patient received standard perioperative antibiotics and pain control. Patients were immediately placed in a hinged knee arthrosis (Bledsoe Brace Systems, Grand Prairie, TX) locked in full extension. When medically stable and cleared by physical therapy (PT) (according to their individual weightbearing status), the patients were discharged.
Rehabilitation was focused on early protection of the joint and repair while gently ranging the knee to prevent stiffness. Weightbearing status was dictated by concomitant fractures, repairs, or reconstructions to the ipsilateral knee. There were no limitations to weightbearing due to the PCL repair. PT was initiated immediately for quadriceps isometrics in full extension and gait training with bilateral axillary crutches. At 2 weeks, formal, supervised, outpatient PT was initiated. Early PT focused on ROM activities in the brace with a goal of at least 0° to 90° at 1 month postoperatively. While there were no restrictions to brace ROM during PT or home exercise, the brace was maintained in full extension for all weightbearing activities. At 6 weeks, the crutches were discontinued and the brace was unlocked during weightbearing activities as long as the patient was able to perform a straight-leg raise against gravity without an extension lag. PT was now focused on continuing ROM gains and performing progressive resistive exercises with an emphasis on the closed-kinetic-chain activities. Open-kinetic-chain activities were discouraged. At 12 weeks, the brace was discontinued and PT was progressed until strength and ROM gains were maximized. At 6 months, if the patient had at least 4+/5 strength and had achieved full extension and flexion within 15° of the opposite knee, the patient was cleared for gradual return to sport and/or strenuous work activities.
Followup visits were scheduled at 1, 4, 8, 12, and 24 weeks postoperatively to monitor healing, strength, and ROM. Strength was assessed using the standard 0 to 5 grading and ROM was assessed by goniometric evaluation of knee flexion and extension. Patients were then generally seen at 1 year after surgery and as needed thereafter. However, the three patients reported here were specifically called back for long-term followup; at that visit, ROM, strength, and a clinical examination including posterior drawer tests were performed to see if the stability of the repair was maintained. Also, at that time, the functional outcomes, as assessed by Lysholm and modified Cincinnati knee scores, were recorded. For these patients, we also performed MRI followup.
Results
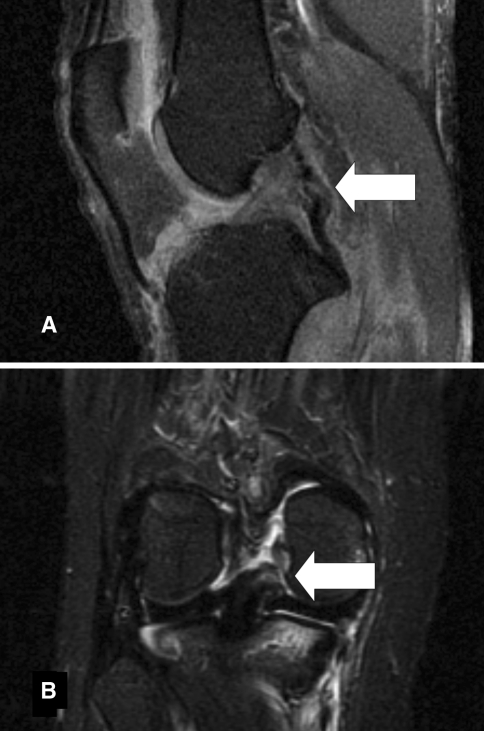
All three patients in our series had a soft tissue avulsion or peel off injury of the PCL from its femoral insertion. All tears were accurately identified on preoperative MRI (Fig. 7). Intraoperative inspection confirmed adequate tissue quality and length for a stable repair as predicted by MRI.
Fig. 7A–B.
(A) A sagittal view MR image from Patient 1 shows the PCL avulsed from the medial femoral condyle (arrow). (B) A coronal view MR image from Patient 3 shows the PCL avulsed from the medial femoral condyle (arrow).
Once confirmed as a peel off injury intraoperatively, all three cases were amenable to arthroscopic repair as described above. No accessory portals were required.
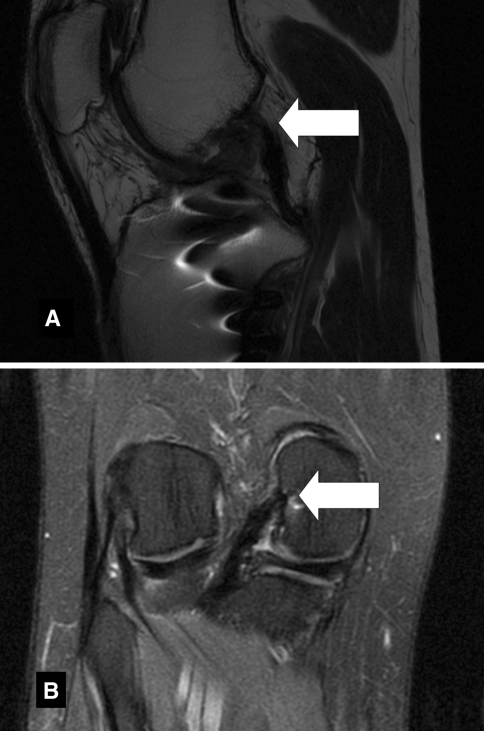
At an average followup of 68 months, average ROM was 0° to 127°. All three patients had a negative posterior drawer test immediately after repair that was maintained at most recent followup, indicating a stable, sustained repair. In addition, followup MRI was performed on all patients more than 2 years postoperatively and ligament healing was confirmed (Fig. 8). The procedure was effective at returning patients to a pain-free functional status. The average Lysholm score was 92 and the average modified Cincinnati knee score was 94.
Fig. 8A–B.
(A) A sagittal view MR image from Patient 1 at 6-year followup shows the PCL inserting into the medial femoral condyle (arrow). (B) A coronal view MR image from Patient 3 at 5-year followup shows the PCL inserting into the medial femoral condyle (arrow).
None of the seven patients operated on using our technique have had intraoperative or postoperative complications.
Discussion
The majority of operative PCL injuries are found in conjunction with MLIK. Although these injuries are rare, they present with a myriad of different injury mechanisms, patterns, and severity [23, 28]. Controversy exists in the literature regarding treatment algorithms [10]. Delayed reconstruction is the current gold standard of treatment [1, 5, 16]. This is likely influenced by the fact that midsubstance ruptures are the most commonly encountered pattern. However, there are specific anatomic injury patterns to the PCL that lend themselves to successful acute repair, and there are certain clinical scenarios that increase the risk of formal reconstruction. We described a technique to repair soft tissue avulsions of the PCL and reviewed three patients to determine whether (1) femoral peel off type soft tissue avulsions can be identified by preoperative MRI; (2) the peel off avulsion is amenable to arthroscopic repair; (3) the described technique restores ROM, stabilizes the knee to posterior drawer testing, and returns patients to a pain-free functional status; and (4) the technique has a low complication rate.
Our study is subject to a few important limitations. First, we had a small number of patients. PCL injuries reportedly occur in 3% to 40% of acute knee injuries [5, 16, 22, 34]. PCL injuries, in general, are approximately 50 times less common than anterior cruciate ligament (ACL) injuries [10]. The PCL injuries eligible for repair represent a smaller subset of all PCL injuries. Second, given that the PCL injuries were in the setting of a MLIK, there was substantial variability in the associated injury patterns and rehabilitation performed among the patients. Finally, certain well-accepted objective measurements of PCL stability such as Telos stress radiography were not performed.
With the advent and acceptance of delayed ligament reconstruction procedures as the surgery of choice for cruciate ligament ruptures [4, 5, 7, 8, 12, 29, 31, 32, 37], discussion of acute ligament repair has largely faded from the literature. However, open-repair techniques reportedly restore stability and function [24]. A study by Owens et al. [24] in 2007 looked at open primary repair of the PCL and other injured ligaments in 28 knee dislocations. At an average of 48 months, the mean Lysholm score was 89, which was considered “comparable to recent reports of ligament reconstruction.” Arthroscopic PCL soft tissue repair publications are limited to two case reports and two small case series [20, 25, 30, 39]. In these reports, the repair technique entails simple sutures passed through the PCL using a Caspari suture punch. These are then tensioned and tied over a bone bridge. With this technique of simple sutures in the stump, it is difficult to gain purchase of the tissue to enable repair. In fact, Wheatley et al. [39] reported several arthroscopic PCL repairs were converted to open procedures to gain purchase of the tissue using a Kessler-type stitch.
Our technique differs in subtle, but important, ways from previous techniques. While the ligament footprint is débrided to bleeding bone, it is not recessed as in other techniques [39]. We believe there is typically not enough length in the remaining stump for recession to be helpful. Inoue et al. [13] found “the occult PCL mid-substance injury does not significantly affect post-operative posterior stability of the knee.” Our experiences parallel those of Inoue et al. [13]. We have noted well-tensioned repairs intraoperatively and stable knees at followup. Most importantly, newer, reloadable suture passing devices and improved arthroscopic equipment enable the passage of more complex, Bunnell-type stitch patterns through the PCL stump. The Bunnell stitch has a higher maximum load to failure force than the Kessler stitch [11, 26] and certainly more than simple sutures. The Bunnell stitch is complimented by using modern suture material of increased strength. We believe this more robust suture material and stitch pattern enable predictably successful ligament repair in carefully selected patients.
We performed all of the repairs in these patients subacutely in the complex MLIK setting. The impetus for repair attempt was patients with injuries that prohibited an arthroscopic PCL reconstruction. In two patients, there were small plateau fractures that would have created undue risk of fracture propagation if formal tibial bone tunnels were placed, and in one patient, there was concern for postsurgery arthrofibrosis (see Appendix 1 [supplemental materials are available with the online version of CORR]). When treating MLIK surgically, the risks of neurologic injury, compartment syndrome, wound complications, and stiffness/arthrofibrosis can all be related to large open incisions and prolonged operative times [27]. The primary benefit of a successful arthroscopic PCL repair is the avoidance of reconstructive surgery.
Although recent literature has suggested PCL repair may not be as successful as PCL reconstruction [8, 19], our series and that of Owens et al. [24] demonstrated clinically stable knees, minimal loss of ROM, and average Lysholm scores of 92 and 89, respectively. These findings are consistent with a recent systematic review of arthroscopic tibial tunnel PCL reconstruction by Kim et al. [16]. Ten studies were included and Lysholm scores from 81 to 100 were reported. With advancements in MRI, it is now possible to identify soft tissue avulsion tears of the cruciates from the distal femur or proximal tibia more accurately than ever [9, 21, 35, 36]. In appropriately selected patients with specific pathoanatomic patterns of injury (PCL soft tissue avulsions with enough tissue length to span the tibia and femur in a reduced, flexed position) and adequate tissues (able to hold the suture against resistance), performing a repair restored function while minimizing the morbidity associated with reconstruction. In addition, primary repair preserves the native tissues of the knee, thereby theoretically maintaining some proprioception [33] while keeping reconstructive options open should any future surgery be needed. In this study, our patients experienced a return to pain-free activities of daily living and preinjury functional status after an arthroscopic primary repair of the PCL.
The described technique of arthroscopic PCL repair has been utilized with anecdotally similar restoration of stability and high levels of function, but not previously reported by the senior author (GSD) for cruciate ligament soft tissue avulsions of both the ACL and PCL at both the femoral and tibial attachments. Although the technique described discusses tensioning over a bone bridge with a ligament button, it has also been performed by tensioning down to a knotless suture anchor device (SwiveLock™; Arthrex). This simplifies the procedure slightly by obviating the need for both the bone tunnels and the extra incision. However, the security of the fixation in this situation requires further study.
The technique described here is one more tool in the armamentarium of the surgeon dealing with the complex injury patterns inherent to traumatic knee dislocations. We believe, in light of the advancements of the knowledge base in imaging, surgical, and device technologies, the discussion related to ligament repair should be resumed.
Electronic supplementary material
Supplementary material 4 (TIFF 26370 kb)
Supplementary material 5 (TIFF 26370 kb)
Supplementary material 6 (TIFF 26370 kb)
Footnotes
One of the authors (GSD) certifies that he has or may receive payments or benefits from the Speaker’s Bureau for Arthrex, Inc (Naples, FL).
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Jacobi Medical Center, Bronx, NY, and Lenox Hill Hospital, New York, NY.
References
- 1.Bergfeld JA, Graham SM, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33:976–981. doi: 10.1177/0363546504273046. [DOI] [PubMed] [Google Scholar]
- 2.Bovid KM, Salata MJ, Have KL, Sekiya JK. Arthroscopic posterior cruciate ligament reconstruction in a skeletally immature patient: a new technique with case report. Arthroscopy. 2010;26:563–570. doi: 10.1016/j.arthro.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 3.Brunet P, Charrois O, Degeorges R, Boisrenoult P, Beaufils P. Reconstruction of acute posterior cruciate ligament tears using a synthetic ligament] [in French. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:34–43. doi: 10.1016/S0035-1040(05)84273-4. [DOI] [PubMed] [Google Scholar]
- 4.Buchner M, Schmeer T, Schmitt H. Anterior cruciate ligament reconstruction with quadrupled semitendinosus tendon—minimum 6 year clinical and radiological follow-up. Knee. 2007;14:321–327. doi: 10.1016/j.knee.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Chen CH, Chen WJ, Shih CH. Arthroscopic posterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arch Orthop Trauma Surg. 1999;119:86–88. doi: 10.1007/s004020050362. [DOI] [PubMed] [Google Scholar]
- 6.Chen CH, Chen WJ, Shih CH. Fixation of small tibial avulsion fracture of the posterior cruciate ligament using the double bundles pull-through suture method. J Trauma. 1999;46:1036–1038. doi: 10.1097/00005373-199906000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Chen CH, Chuang TY, Wang KC, Chen WJ, Shih CH. Arthroscopic posterior cruciate ligament reconstruction with hamstring tendon autograft: results with a minimum 4-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1045–1054. doi: 10.1007/s00167-006-0113-y. [DOI] [PubMed] [Google Scholar]
- 8.Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2–9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026. doi: 10.1007/s00167-009-0869-y. [DOI] [PubMed] [Google Scholar]
- 9.Gross ML, Grover JS, Bassett LW, Seeger LL, Finerman GA. Magnetic resonance imaging of the posterior cruciate ligament: clinical use to improve diagnostic accuracy. Am J Sports Med. 1992;20:732–737. doi: 10.1177/036354659202000615. [DOI] [PubMed] [Google Scholar]
- 10.Hammoud S, Reinhardt KR, Marx RG. Outcomes of posterior cruciate ligament treatment: a review of the evidence. Sports Med Arthrosc. 2010;18:280–291. doi: 10.1097/JSA.0b013e3181eaf8b4. [DOI] [PubMed] [Google Scholar]
- 11.Herbort M, Haber A, Zantop T, Gosheger G, Rosslenbroich S, Raschke MJ, Petersen W. Biomechanical comparison of the primary stability of suturing Achilles tendon rupture: a cadaver study of Bunnell and Kessler techniques under cyclic loading conditions. Arch Orthop Trauma Surg. 2008;128:1273–1277. doi: 10.1007/s00402-008-0602-1. [DOI] [PubMed] [Google Scholar]
- 12.Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2010 December 12 [Epub ahead of print]. [DOI] [PubMed]
- 13.Inoue M, Yasuda K, Kondo E, Saito K, Ishibe M. Primary repair of posterior cruciate ligament avulsion fracture: the effect of occult injury in the midsubstance on postoperative instability. Am J Sports Med. 2004;32:1230–1237. doi: 10.1177/0363546503262201. [DOI] [PubMed] [Google Scholar]
- 14.Kim SJ, Shin SJ, Cho SK, Kim HK. Arthroscopic suture fixation for bony avulsion of the posterior cruciate ligament. Arthroscopy. 2001;17:776–780. doi: 10.1053/jars.2001.22392. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Shin SJ, Choi NH, Cho SK. Arthroscopically assisted treatment of avulsion fractures of the posterior cruciate ligament from the tibia. J Bone Joint Surg Am. 2001;83:698–708. doi: 10.2106/00004623-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Kim YM, Lee CA, Matava MJ. Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011;39:425–434. doi: 10.1177/0363546510374452. [DOI] [PubMed] [Google Scholar]
- 17.King JJ, 3rd, Cerynik DL, Blair JA, Harding SP, Tom JA. Surgical outcomes after traumatic open knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2009;17:1027–1032. doi: 10.1007/s00167-009-0721-4. [DOI] [PubMed] [Google Scholar]
- 18.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 19.Levy BA, Fanelli GC, Whelan DB, Stannard JP, MacDonald PA, Boyd JL, Marx RG, Stuart MJ. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197–206. doi: 10.5435/00124635-200904000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Lobenhoffer P, Wunsch L, Bosch U, Krettek C. Arthroscopic repair of the posterior cruciate ligament in a 3-year-old child. Arthroscopy. 1997;13:248–253. doi: 10.1016/S0749-8063(97)90164-X. [DOI] [PubMed] [Google Scholar]
- 21.Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005;21:1354–1361. doi: 10.1016/j.arthro.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 22.Moore HA, Larson RL. Posterior cruciate ligament injuries: results of early surgical repair. Am J Sports Med. 1980;8:68–78. doi: 10.1177/036354658000800203. [DOI] [PubMed] [Google Scholar]
- 23.Noyes FR, Barber-Westin SD. Treatment of complex injuries involving the posterior cruciate and posterolateral ligaments of the knee. Am J Knee Surg. 1996;9:200–214. [PubMed] [Google Scholar]
- 24.Owens BD, Neault M, Benson E, Busconi BD. Primary repair of knee dislocations: results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma. 2007;21:92–96. doi: 10.1097/BOT.0b013e3180321318. [DOI] [PubMed] [Google Scholar]
- 25.Park IS, Kim SJ. Arthroscopic fixation of avulsion of the posterior cruciate ligament from femoral insertion. Arthroscopy. 2005;21:1397. doi: 10.1016/j.arthro.2005.08.030. [DOI] [PubMed] [Google Scholar]
- 26.Pjanowski GJ, Stein LE, Turner TA. Strength characteristics and failure modes of suture patterns in severed goat tendons. Vet Surg. 1989;18:335–339. doi: 10.1111/j.1532-950X.1989.tb01095.x. [DOI] [PubMed] [Google Scholar]
- 27.Richmond JC. Complications associated with treatment of multiligament-injured/dislocated knee. Sports Med Arthroscopy Rev. 2001;9:255–260. doi: 10.1097/00132585-200107000-00012. [DOI] [Google Scholar]
- 28.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718–727. doi: 10.1177/03635465020300051601. [DOI] [PubMed] [Google Scholar]
- 29.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337–1345. doi: 10.1177/0363546504274145. [DOI] [PubMed] [Google Scholar]
- 30.Ross G, Driscoll J, McDevitt E, Scheller A., Jr Arthroscopic posterior cruciate ligament repair for acute femoral “peel off” tears. Arthroscopy. 2003;19:431–435. doi: 10.1053/jars.2003.50134. [DOI] [PubMed] [Google Scholar]
- 31.Ruiz AL, Kelly M, Nutton RW. Arthroscopic ACL reconstruction: a 5–9 year follow-up. Knee. 2002;9:197–200. doi: 10.1016/S0968-0160(02)00019-4. [DOI] [PubMed] [Google Scholar]
- 32.Schulte KR, Chu ET, Fu FH. Arthroscopic posterior cruciate ligament reconstruction. Clin Sports Med. 1997;16:145–156. doi: 10.1016/S0278-5919(05)70011-9. [DOI] [PubMed] [Google Scholar]
- 33.Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments: a histological study. J Bone Joint Surg Am. 1984;66:1072–1076. [PubMed] [Google Scholar]
- 34.Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27:276–283. doi: 10.1177/03635465990270030201. [DOI] [PubMed] [Google Scholar]
- 35.Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12:209–213. [PubMed] [Google Scholar]
- 36.Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: normal, abnormal, and associated injury patterns. Radiographics. 1995;15:551–561. doi: 10.1148/radiographics.15.3.7624562. [DOI] [PubMed] [Google Scholar]
- 37.Sun K, Tian SQ, Zhang JH, Xia CS, Zhang CL, Yu TB. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft. Arthroscopy. 2009;25:750–759. doi: 10.1016/j.arthro.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 38.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–529. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Wheatley WB, Martinez AE, Sacks T, Schurhoff MR, Uribe JW, Hechtman KS, Zvijac JE. Arthroscopic posterior cruciate ligament repair. Arthroscopy. 2002;18:695–702. doi: 10.1053/jars.2002.32836. [DOI] [PubMed] [Google Scholar]
- 40.Zhang L, Liu JS, Sun J, Li ZY, Ma J. [Arthroscopic posterior cruciate ligament reconstruction with Achilles allograft using transfemoral double-bundle and tibial inlay technique] [in Chinese] Zhongguo Gu Shang. 2008;21:890–893. [PubMed] [Google Scholar]
- 41.Zhao J, He Y, Wang J. Arthroscopic treatment of acute tibial avulsion fracture of the posterior cruciate ligament with suture fixation technique through Y-shaped bone tunnels. Arthroscopy. 2006;22:172–181. doi: 10.1016/j.arthro.2005.10.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 4 (TIFF 26370 kb)
Supplementary material 5 (TIFF 26370 kb)
Supplementary material 6 (TIFF 26370 kb)