Abstract
Background
Conventional MRI is limited for characterizing the posterolateral corner of the knee due to the region’s anatomic variability and complexity; further, MRI is a static study and cannot demonstrate pathologic laxity. Stress radiography may provide additional information about instability.
Questions/purposes
We therefore (1) correlated varus stress radiography with MRI findings, (2) compared opening in patients who underwent surgical posterolateral corner stabilization versus those who did not, and (3) determined whether stress radiography findings could supplement MRI for making treatment decisions.
Patients and Methods
We retrospectively studied 26 patients (27 knee injuries) and correlated lateral compartment opening on varus stress radiography with severity of posterolateral corner injury on MRI. We compared radiographic findings in 18 patients with complete injuries who underwent posterolateral corner stabilization with five who did not.
Results
A complete posterolateral corner injury on MRI was associated with an average of 18.6 mm (10.0–36.5 mm) of varus opening versus 12.8 mm (7.5–17.0 mm) in partial injuries. Opening in operative cases that underwent stabilization was 16.5 mm (11.0–36.5 mm) versus 11.0 mm (7.5–13.5 mm) for those that did not. Ten of 15 partial injuries underwent stabilization, for which the varus opening was 13.6 mm (11.0–17.0 mm). Average varus opening in partial injuries that did not undergo stabilization was 11.0 mm (7.5–13.5 mm).
Conclusions
Varus stress radiography correlated to MRI findings for posterolateral corner injury. The injuries we treated with reconstruction were associated with increased varus opening. In patients with partial posterolateral corner injury on MRI, we used degree of opening on varus stress radiography to aid the decision for stabilization.
Level of Evidence
Level IV, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The posterolateral corner (PLC) of the knee presents unique diagnosis and treatment challenges due to the complexity of its structure and function [24]. Injury to the PLC compromises the rotatory and angular stability of the knee, leading to persistent instability, gait abnormalities, and/or degenerative changes [4, 6–8, 10, 24]. Delay in diagnosis complicates surgical treatment, rendering repair less reliable and more difficult, with excessive scar tissue potentially concealing vital ligamentous, capsular, and neurovascular structures [3, 14, 17, 18, 23, 24]. Deficiency of the PLC generates excessive force on anterior cruciate ligament (ACL) [15] and posterior cruciate ligament (PCL) [14] grafts, and unrecognized injury is associated with failure of cruciate reconstruction [21].
While unquestionably important for diagnosing knee ligament injuries, MRI has limitations for characterizing the PLC. The anatomic complexity, variability, and oblique orientation of its individual structures make it difficult to reliably identify all major PLC injuries on conventional MRI sequences [1, 2, 23, 32]. The diagnostic specificity of MRI for knee ligament injury decreases when more than one ligament is injured [26], as is usually the case with PLC injury [24], and chronic injuries may not be well demonstrated [22]. As a static study, MRI also has inherent limitations for diagnosing clinically relevant instability, and partial tears or edema revealed on MRI may not correlate with laxity [32]. High-power magnets [1, 12], thin-slice scans [12], and coronal oblique technique [1, 12, 34] have improved MRI of the PLC, but access to this technology and experienced musculoskeletal radiologists may not be universally available, particularly in community hospitals or clinics [23].
Recognizing these potential limitations of MRI for PLC injury, our clinic implemented a stress radiography protocol in 2007 to obtain dynamic images to supplement MRI in our treatment algorithm for patients with suspected knee ligament injuries. Dynamic imaging provides an objective representation of the functional laxity resulting from ligament deficiency [5, 9, 13, 19, 25, 28–30]. Stress radiography is an established technique for measuring posterior laxity from PCL insufficiency [5, 9, 19, 20, 28, 30] and is evolving as a diagnostic tool for evaluating PLC injury as well. Cadaver studies support the usefulness of a posterior drawer test [30] and varus stress radiography [13] for diagnosing PLC injuries, and some propose dynamic varus stress ultrasound [29] for making clinical decisions. Some authors have used stress radiography to follow patients who undergo PLC reconstruction [16, 25, 31].
We therefore (1) correlated stress radiography findings to the degree of PLC injury as demonstrated on MRI, (2) compared varus opening in patients who underwent PLC reconstruction versus those who did not, and (3) determined whether stress radiography findings could supplement MRI to influence the decision to surgically stabilize the PLC.
Patients and Methods
We retrospectively reviewed all patients with knee injuries between September 2007 and September 2010 who had an MRI study with a positive reading for partial or complete PLC injury and an associated varus stress radiograph of the knee available for review. Potential study patients were identified by searching a radiology database prospectively maintained at our institution for MRIs with a positive reading for PLC injury defined as edema, sprain, partial or complete tear, increased signal intensity, or abnormal appearance of any of the following PLC structures: fibular collateral ligament (FCL), popliteofibular ligament, popliteus muscle or tendon, or posterolateral capsule. With these search strings, we identified 96 MRI records, of which 14 knee injuries in 13 patients had associated varus stress radiographs. To capture additional patients referred to our clinic with outside MRIs, we also searched stress radiograph series obtained in our clinic to evaluate for potential PLC injury. Of 42 such stress radiographs, we found an additional 13 referral patients with available MRIs. We obtained MRIs from the outside institution by either compact disc or uploading them onto our radiology server, which our institution’s musculoskeletal radiologist (CMG) then reviewed. We therefore identified a total of 26 patients with 27 knee ligament injuries. There were 18 men and eight women with an average age of 35.4 years (range, 18–72 years). Fourteen cases involved the right knee and 13 involved the left. Twelve were acute injuries at the time of clinical evaluation (within 3 weeks of injury), while 15 were chronic injuries.
One of the authors (FWG) categorized the integrity of the ACL, PCL, and PLC by grade of ligament injury as read on MRI [27]. Grade 0 corresponded with no injury. Grade 1 indicated potential or low-grade partial injury in which local edema was present, but the majority of fibers appeared to be intact. Grade 2 indicated high-grade partial injury with fluid signal extending into the ligament but some fibers intact. A Grade 3 injury corresponded to a complete tear with no intact fibers visible on MRI. We recorded the highest grade injury to any of the primary component structures of the PLC (FCL, popliteus muscle/tendon, popliteofibular ligament).
Of the 27 knee ligament injuries identified in the database search, 16 had a partial injury (Grade 1 or 2) to the PLC demonstrated on MRI while complete (Grade 3) injuries were present in 11. We observed no isolated PLC injuries since all cases included at least one additional injured ligament. Seven had an associated high-grade ACL injury, one had a high-grade ACL and medial collateral ligament injury, one had a high-grade PCL injury, eight had ACL and PCL injuries, and 10 had injuries to all four major ligament structures.
Our clinic radiograph protocol included an AP radiograph of the injured knee flexed at 30° with physician-applied varus stress. Two independent examiners (FWG, MAT) measured absolute lateral compartment opening on each varus stress radiograph. Opening was defined as the absolute perpendicular distance between the subchondral bone at the most distal point on the lateral femoral condyle to the corresponding point on the lateral tibial plateau on a physician-applied varus stress AP radiograph (Fig. 1) as described by LaPrade et al. [13]. The final value reported in this study represented the mean of measurements obtained by the two examiners. The intraclass correlation coefficient reflecting interexaminer reliability between the two examiners was 0.963.
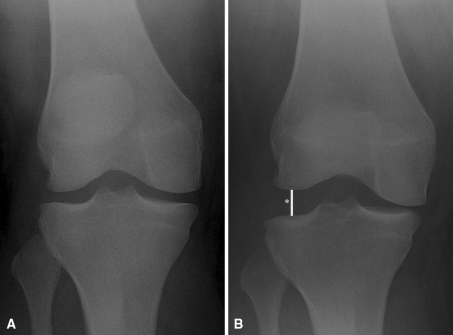
Fig. 1A–B.
(A) A nonweightbearing, neutral AP radiograph shows a suspected knee ligament injury. (B) A radiograph shows how physician-applied varus stress reveals lateral compartment opening (*), indicative of a PLC injury.
Indication for surgery was compromised knee stability secondary to high-grade cruciate injury, with or without an associated PLC injury, as diagnosed by physical examination and MRI. The decision to reconstruct the PLC depended on physical examination, MRI, and stress radiography findings and was confirmed at the time of surgery with positive varus opening and dial testing on examination under anesthesia and/or positive lateral compartment drive-through sign [11] during arthroscopy. The primary contraindication for surgery was the presence of substantial medical comorbidities.
Twenty-three of 27 injuries underwent surgery. One 71-year-old patient with bilateral high-grade multiligament injuries did not undergo operative treatment because of substantial medical problems. One patient with a high-grade ACL/PCL/PLC injury, for which surgery was recommended, was lost to followup. Surgeons nonoperatively treated one ACL/PLC injury with an associated bony avulsion of the proximal fibula in a 63-year-old patient using a brace. Of the 23 knee injuries treated surgically, 18 underwent PLC reconstruction. In the other five operative cases, surgeons did not perform PLC reconstruction due to perceived posterolateral stability at the time of surgery.
We determined the data we obtained were normally distributed by examining skewness and kurtosis values. Therefore, we used independent-samples t tests to compare varus opening between acute and chronic cases. We performed analyses for patients who had a partial (Grade 1 or 2) injury and for those patients with a complete (Grade 3) injury.
Results
The average (± SD) varus opening on stress radiography for all 27 knees studied (Table 1) was 15.1 ± 5.6 mm (range, 7.5–36.5 mm). Of the 16 knee injuries (seven acute, nine chronic) with a partial (Grade 1 or 2) injury to the PLC on MRI, the average lateral compartment opening was 12.8 ± 2.4 mm (range, 7.5–17 mm). In this group, we found no difference (p = 0.45) in varus opening between acute (12.4 ± 1.8 mm) and chronic (13 ± 2.8 mm) injuries. The 11 knee injuries (five acute, six chronic) with a complete (Grade 3) injury to the PLC had an average lateral compartment opening on varus stress radiography of 18.6 ± 7.1 mm (range, 10–36.5 mm). We also found no difference (p = 0.69) in varus opening between acute (20.5 ± 9.2 mm) and chronic (17.1 ± 5.2 mm) injuries. When the injury pattern included an associated high-grade ACL injury (eight cases) but no major PCL injury, the average varus opening was 12.9 ± 3.0 mm. When an associated high-grade ACL and PCL injury was present (18 cases), the average varus opening was 16.4 ± 6.3 mm.
Table 1.
MRI, varus stress radiography, and operative findings (sorted by amount of varus opening on stress radiograph)
| Age (years) | Gender | Knee | Injury grade on MRI | Varus opening (mm) | Arthroscopic drive-through sign?* | PLC stabilized?† | Note | ||
|---|---|---|---|---|---|---|---|---|---|
| ACL | PCL | PLC | |||||||
| 27 | Male | Right | 3 | 0 | 2 | 7.5 | Not reported | No | |
| 71 | Male | Right | 2 | 3 | 3 | 10.0 | Not reported | Poor operative candidate | |
| 57 | Male | Right | 3 | 3 | 2 | 10.0 | Negative | No | |
| 19 | Male | Left | 0 | 3 | 2 | 11.0 | Positive | Yes | |
| 25 | Female | Left | 3 | 0 | 2 | 11.0 | Positive | Yes | |
| 38 | Male | Right | 3 | 3 | 2 | 11.5 | Not reported | No | |
| 31 | Male | Right | 3 | 3 | 1 | 12.0 | Positive | Yes | |
| 40 | Male | Left | 3 | 3 | 2 | 12.5 | Not reported | Yes | |
| 35 | Male | Right | 3 | 3 | 2 | 12.5 | Negative | No | |
| 28 | Male | Right | 3 | 0 | 2 | 12.5 | Positive | Yes | |
| 27 | Male | Right | 3 | 1 | 1 | 13.0 | Not reported | Yes | |
| 63 | Female | Right | 3 | 0 | 2 | 13.5 | Not reported | Elected nonoperative treatment | |
| 49 | Male | Left | 3 | 3 | 2 | 13.5 | Positive | Yes | |
| 21 | Male | Left | 3 | 0 | 2 | 13.5 | Not reported | No | Contralateral stress radiograph demonstrated 2.5-mm side-to-side difference |
| 19 | Male | Right | 3 | 0 | 1 | 14.0 | Positive | Yes | |
| 23 | Female | Right | 3 | 3 | 3 | 14.0 | Not reported | Yes | |
| 28 | Male | Left | 3 | 3 | 3 | 14.5 | Not reported | Surgery recommended, patient lost to followup | |
| 19 | Female | Left | 3 | 3 | 2 | 15.0 | Positive | Yes | |
| 34 | Male | Right | 3 | 2 | 3 | 16.0 | Positive | Yes | |
| 36 | Female | Right | 3 | 2 | 2 | 16.5 | Positive | Yes | |
| 29 | Female | Left | 3 | 3 | 2 | 17.0 | Positive | Yes | |
| 18 | Male | Left | 3 | 0 | 3 | 18.0 | Positive | Yes | |
| 53 | Male | Right | 3 | 3 | 3 | 19.5 | Not reported | Yes | |
| 71 | Male | Left | 3 | 3 | 3 | 19.5 | Not reported | Poor operative candidate | |
| 28 | Male | Left | 3 | 2 | 3 | 20.5 | Not reported | Yes | |
| 72 | Female | Left | 3 | 3 | 3 | 24.0 | Not reported | Yes | |
| 30 | Female | Left | 3 | 3 | 3 | 36.5 | Positive | Yes | |
* The arthroscopic “drive-through sign” was not consistently reported in all operative records; †four study patients did not undergo operative treatment of knee ligament injuries; ACL = anterior cruciate ligament; PCL = posterior cruciate ligament; PLC = posterolateral corner.
The average opening on varus stress radiography in the 18 operative knee injuries that underwent PLC stabilization was 16.5 ± 6.1 mm (range, 11–36.5 mm). In the five operative knee injuries that did not undergo PLC reconstruction, the average opening was 11 ± 2.3 mm (range, 7.5–13.5 mm).
Of the eight operative knee injuries with MRI evidence of a complete (Grade 3) PLC injury, all underwent PLC reconstruction. Ten of 15 operative knee injuries with MRI evidence of a partial (Grade 1 or 2) PLC injury underwent PLC reconstruction. The average varus opening on stress radiography in these cases was 13.6 ± 2.1 mm (range, 11–17 mm). In the five knee injuries with partial PLC that did not undergo PLC reconstruction, the average opening was 11.0 ± 2.3 mm (range, 7.5–13.5 mm).
Discussion
Early and accurate diagnosis of PLC injury is critical to proper treatment. MRI is central to evaluation but may not definitively characterize the injury or functional consequence. Dynamic imaging may provide additional objective information about the instability resulting from PLC injury and aid in diagnosis. We therefore (1) correlated varus stress radiography with MRI findings, (2) compared opening in patients who underwent surgical PLC stabilization versus those who did not, and (3) determined whether stress radiography findings could supplement MRI for making treatment decisions.
Our study is associated with a number of limitations. First, owing to the retrospective nature of this study, there was not a consistent radiographic protocol. In particular, contralateral stress radiographs are not routinely available, which would help establish a control group or evaluate side-to-side differences. Second, a standardized MRI sequence is also not available since several of the MRIs came from outside facilities. Third, the stress radiography technique has limitations since guarding, knee pain, or external fixators can impact the absolute value of varus opening. Fourth, this study is limited by the sample size, which may result in an underpowered study. Finally, no followup clinical examination or imaging after the treatment of these injuries was performed. We recognize these limitations and acknowledge one should view the information obtained from stress radiography in context and use it adjunctively to MRI and physical examination.
We found stress radiography corresponded to the severity of injury demonstrated on MRI. Partial injury to the PLC on MRI resulted in a varus opening of 12.8 mm while 18.6 mm corresponded with complete disruption on MRI. A recent cadaver study showing increased varus opening with increased injury severity corroborates our findings [13]. In that study, sequential sectioning of the FCL and PLC resulted in varus opening on stress radiography of 12.4 and 13.7 mm, respectively, from a baseline tibiofemoral distance of 9.7 mm [13]. While we observed greater varus opening in our study with complete PLC injury, at least one cruciate tore in all of our cases, and high-grade bicruciate injuries were present in 18 of 27 cases, in addition to the PLC injury. The cadaver study demonstrated the contribution of the cruciates to varus stability [13]. After sectioning of the PLC, further sequential sectioning of the ACL and PCL resulted in further opening to 16.3 and 17.5 mm, respectively.
Our patients who underwent PLC reconstruction demonstrated greater varus laxity on stress radiography than those not having surgical stabilization. Due to our study design, we cannot establish a threshold for varus opening that predicts an absolute need for PLC stabilization. A recent study of 16 patients with suspected PLC injury showed lateral compartment opening of greater than 10.5 mm on varus stress ultrasound predicted the need for PLC stabilization in 100% of cases [29]. Three of our five patients with varus opening of greater than 10.5 mm did not undergo PLC reconstruction and were stable to varus stress at the time of surgery. While this discrepancy may reflect a difference between ultrasound and radiography, it highlights the value of multiple modalities in the decision-making process for PLC reconstruction, including MRI and physical examination. One study of 20 patients having FCL reconstruction assessed varus instability using the contralateral knee as a control and found an average side-to-side difference of 3.9 mm of lateral compartment opening on varus stress radiography [16]. Although our radiograph protocol did not routinely include the contralateral knee, obtaining comparison images could help correct for anatomic variability or physiologic laxity and provide more reliable information.
While all eight of our patients with MRI evidence of complete PLC injury underwent reconstruction, five of 15 patients with a partial PLC injury on MRI also had reconstruction. This finding reflects the limitations of MRI since we did not use a positive finding for PLC injury on MRI as an absolute indication for surgical stabilization. Previous studies correlate MRI with surgical findings for PLC injury. In a study of 17 acute knee dislocations, Twaddle et al. [33] found MRI positively predicted surgical FCL, PLC, and arcuate complex injury in 92%, 100%, and 64% of cases, respectively. In a more recent study of 14 suspected PLC injuries, Theodorou et al. [32] reported MRI accuracy for FCL and popliteus injury to be 100% and 86%, respectively. In that study, using conventional MRI sequences, a surgical popliteofibular ligament injury went unnoticed on MRI in three cases. A thin-slice coronal oblique MRI sequence improved evaluation of the PLC [34]. In 20 knees with surgically verified Grade 3 PLC injuries evaluated with an MRI protocol including thin-slice coronal oblique images through the fibular head, LaPrade et al. [12] found MRI to be accurate in diagnosing FCL, popliteus, and popliteofibular ligament injury in 95%, 90%, and 68% of cases, respectively. In our study, we did not routinely implement a thin-slice coronal oblique MRI protocol since several MRIs occurred at outside facilities. The additional information gained by stress radiography helped to clarify the degree of functional laxity, particularly in cases where partial PLC injury was demonstrated on MRI. In such cases, varus opening was an average of 2.6 mm greater in injuries that underwent PLC stabilization compared to those that did not.
In conclusion, MRI is essential to diagnosis of knee ligament injury but has inherent limitations for determining whether or not surgery would be recommended, particularly with partial PLC injury. Advancements in MRI technology affording improved visualization of the PLC are not ubiquitously available. Varus stress radiography contributes to the diagnosis of knee PLC injury by providing objective information about the pathologic laxity resulting from these injuries. Stress radiography generally supports MRI findings but may provide additional information when the degree of injury is unclear.
Acknowledgments
The authors thank David A. Shafique, MS, and Joseph M. Hart, PhD, for their assistance in compiling and analyzing data for this project.
Footnotes
Each author certifies that he has no commercial association (ie, consultancies, stock ownership, equity interest, patent/licensing agreements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Virginia Health System.
References
- 1.Bahk MS, Cosgarea AJ. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc. 2006;14:12–19. doi: 10.1097/00132585-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Bolog N, Hodler J. MR imaging of the posterolateral corner of the knee. Skeletal Radiol. 2007;36:715–728. doi: 10.1007/s00256-006-0271-5. [DOI] [PubMed] [Google Scholar]
- 3.Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83:106–118. doi: 10.1302/0301-620X.83B1.10865. [DOI] [PubMed] [Google Scholar]
- 4.Ellingson CI, Kurtz CA, Sekiya JK. Nonsurgical management of lateral side injuries of the knee. Sports Med Arthrosc. 2006;14:20–22. doi: 10.1097/00132585-200603000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Garavaglia G, Lubbeke A, Dubois-Ferrière V, Suva D, Fritschy D, Menetrey J. Accuracy of stress radiography techniques in grading isolated and combined posterior knee injuries: a cadaveric study. Am J Sports Med. 2007;35:2051–2056. doi: 10.1177/0363546507306466. [DOI] [PubMed] [Google Scholar]
- 6.Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am. 1987;69:233–242. [PubMed] [Google Scholar]
- 7.Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70:88–97. [PubMed] [Google Scholar]
- 8.Hughston JC, Jacobson KE. Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1985;67:351–359. [PubMed] [Google Scholar]
- 9.Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1116–1121. doi: 10.1007/s00167-006-0137-3. [DOI] [PubMed] [Google Scholar]
- 10.Kannus P. Nonoperative treatment of Grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83–88. doi: 10.1177/036354658901700114. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade RF. Arthroscopic evaluation of the lateral compartment of knees with Grade 3 posterolateral knee complex injuries. Am J Sports Med. 1997;25:596–602. doi: 10.1177/036354659702500502. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee: a prospective study of normal knees and knees with surgically verified Grade III injuries. Am J Sports Med. 2000;28:191–199. doi: 10.1177/03635465000280020901. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade RF, Heikes C, Bakker AJ, Jakobsen RB. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and Grade-III posterolateral knee injuries: an in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30:233–238. doi: 10.1177/03635465020300021501. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force: a biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade RF, Spiridonov SI, Coobs BR, Ruckert PR, Griffith CJ. Fibular collateral ligament anatomical reconstructions: a prospective outcomes study. Am J Sports Med. 2010;38:2005–2011. doi: 10.1177/0363546510370200. [DOI] [PubMed] [Google Scholar]
- 17.LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;402:110–121. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Larsen MW, Moinfar AR, Moorman CT., 3rd Posterolateral corner reconstruction: fibular-based technique. J Knee Surg. 2005;18:163–166. doi: 10.1055/s-0030-1248176. [DOI] [PubMed] [Google Scholar]
- 19.Margheritini F, Mancini L, Mauro CS, Mariani PP. Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy. 2003;19:706–711. doi: 10.1016/S0749-8063(03)00399-2. [DOI] [PubMed] [Google Scholar]
- 20.Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005;21:1354–1361. doi: 10.1016/j.arthro.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 21.O’Brien SJ, Warren RF, Pavlov H, Panariello R, Wickiewicz TL. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am. 1991;73:278–286. [PubMed] [Google Scholar]
- 22.Pacheco RJ, Ayre CA, Bollen SR. Posterolateral corner injuries of the knee: a serious injury commonly missed. J Bone Joint Surg Br. 2011;93:194–197. doi: 10.1302/0301-620X.93B2.25774. [DOI] [PubMed] [Google Scholar]
- 23.Pacholke DA, Helms CA. MRI of the posterolateral corner injury: a concise review. J Magn Reson Imaging. 2007;26:250–255. doi: 10.1002/jmri.21013. [DOI] [PubMed] [Google Scholar]
- 24.Ranawat A, Baker CL, 3rd, Henry S, Harner CD. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16:506–518. [PubMed] [Google Scholar]
- 25.Rios CG, Leger RR, Cote MP, Yang C, Arciero RA. Posterolateral corner reconstruction of the knee: evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med. 2010;38:1564–1574. doi: 10.1177/0363546510363462. [DOI] [PubMed] [Google Scholar]
- 26.Rubin DA, Kettering JM, Towers JD, Britton CA. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170:1207–1213. doi: 10.2214/ajr.170.5.9574586. [DOI] [PubMed] [Google Scholar]
- 27.Sanders TG, Miller MD. A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the knee. Am J Sports Med. 2005;33:131–148. doi: 10.1177/0363546504272374. [DOI] [PubMed] [Google Scholar]
- 28.Schulz MS, Russe K, Lampakis G, Strobel MJ. Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med. 2005;33:502–506. doi: 10.1177/0363546504269723. [DOI] [PubMed] [Google Scholar]
- 29.Sekiya JK, Swaringen JC, Wojtys EM, Jacobson JA. Diagnostic ultrasound evaluation of PLC knee injuries. Arthroscopy. 2010;26:494–499. doi: 10.1016/j.arthro.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 30.Sekiya JK, Whiddon DR, Zehms CT, Miller MD. A clinically relevant assessment of posterior cruciate ligament and PLC injuries: evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90:1621–1627. doi: 10.2106/JBJS.G.01365. [DOI] [PubMed] [Google Scholar]
- 31.Shelbourne KD, Haro MS, Gray T. Knee dislocation with lateral side injury: results of an en masse surgical repair technique of the lateral side. Am J Sports Med. 2007;35:1105–1116. doi: 10.1177/0363546507299444. [DOI] [PubMed] [Google Scholar]
- 32.Theodorou DJ, Theodorou SJ, Fithian DC, Paxton L, Garelick DH, Resnick D. Posterolateral complex knee injuries: magnetic resonance imaging with surgical correlation. Acta Radiol. 2005;46:297–305. doi: 10.1080/02841850510021067. [DOI] [PubMed] [Google Scholar]
- 33.Twaddle BC, Hunter JC, Chapman JR, Simonian PT, Escobedo EM. MRI in acute knee dislocation: a prospective study of clinical, MRI, and surgical findings. J Bone Joint Surg Br. 1996;78:573–579. [PubMed] [Google Scholar]
- 34.Yu JS, Salonen DC, Hodler J, Haghighi P, Trudell D, Resnick D. Posterolateral aspect of the knee: improved MR imaging with a coronal oblique technique. Radiology. 1996;198:199–204. doi: 10.1148/radiology.198.1.8539378. [DOI] [PubMed] [Google Scholar]