Abstract
Background
Malignant pelvic tumors frequently pose challenges to surgeons owing to complex pelvic anatomy and local extension. External hemipelvectomy frequently allows adequate margins but is associated with substantial morbidity and reduced function. Limb salvage is an alternative approach when adequate margins can be achieved, but long-term function and survival are unclear.
Questions/purposes
We therefore determined the long-term survival; development of late local recurrence and metastases; function; and need for further reconstructive procedures for patients undergoing limb salvage for treatment of malignant pelvic tumors.
Patients and Methods
We retrospectively reviewed 60 patients treated with pelvic limb salvage before 1989. We reviewed medical records and sent questionnaires incorporating Musculoskeletal Tumor Society (MSTS) and Toronto Extremity Salvage scores to the 38 patients who had no evidence of disease in 1989; 15 patients responded. Minimum followup was 23 years (median, 30 years; range, 23–38 years).
Results
Overall survival rate of the 60 patients was 45%: 100% Stage IA, 75% Stage IB, 31% Stage IIB, and 0% Stage III were alive. Late local recurrence developed only in patients with chondrosarcoma (three of 24). Two patients developed late distant bone metastases. Function declined: the MSTS score of the 15 patients who completed a questionnaire decreased 23%. Two patients had further reconstructive procedures.
Conclusions
At 23- to 38-year followup, we believe pelvic limb salvage is a reasonable treatment if satisfactory margins can be achieved. If a patient with pelvic sarcoma is free of disease 5 years after sarcoma resection, the subsequent risk of death from sarcoma appears to be low. Late local recurrence remains a risk in patients with pelvic chondrosarcoma. Patient-reported function of the salvaged limb declined with long-term followup.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Malignant tumors of the pelvis remain one of the most challenging problems for the orthopaedic oncologist [3, 5–10]. Resection of these tumors is difficult due to their location, local extension, often large size, and complex regional and local anatomy. The resultant defects from internal hemipelvectomy cause substantial postoperative morbidity and functional impairment. We previously reported on 60 patients with pelvic limb salvage for malignant pelvic tumors with an average followup of slightly greater than 5 years [8]. Most reports include an average followup of less than 10 years [1, 3, 5–7, 9, 10, 12, 13].
In 1989, we reported patient demographics, surgical margins, and histologic diagnoses in 60 patients who underwent pelvic limb salvage for malignant tumors between 1970 and 1985 [8]. At that time, 41 of the original 60 patients were alive, 38 of which were alive with no evidence of disease.
To update our 1989 study, we determined the following: (1) long-term survival, (2) risk of developing late local recurrence, (3) risk of developing late metastases, (4) possible change in function at long-term followup, and (5) incidence of further reconstructive procedures at long-term followup.
Patients and Methods
We retrospectively reviewed the records of 41 of the 60 patients who underwent limb-sparing surgery of the pelvis for a malignant pelvic tumor between 1970 and 1985 at our institution and were alive at the time of the original report in 1989 [8]. The index study group demographics included 32 male and 28 female patients, with an age range of 9 to 71 years (mean, 36 years) [8]. Diagnoses of the 60 patients included 34 chondrosarcomas, 13 osteosarcomas, six fibrosarcomas, four Ewing’s sarcomas, and three others. Preoperative staging studies included routine radiographs, CT scan, MRI, and nuclear scanning. A musculoskeletal oncologist determined the patient’s Enneking stage, while a musculoskeletal pathologist determined the histologic grade. Indications for surgery were (1) the tumor could be resected with satisfactory surgical margins and amputation would not provide a better margin and (2) the anticipated functional result would be superior to external hemipelvectomy with prosthetic fitting [8–10]. Contraindications for surgery were (1) inability to achieve a satisfactory surgical margin with limb salvage, (2) inability to preserve a functional limb due to tumor involvement of the sciatic nerve and/or iliac vessels, and (3) unresectable and/or widely metastatic disease on presentation. Of the 41 patients, the three patients who were alive with evidence of disease in 1989 subsequently died of their disease. Of the 38 patients alive with no evidence of disease in 1989, four were lost to followup, two died of their disease in 1990, four died of causes unrelated to their pelvic tumors, and one died of an unknown cause, leaving 27 survivors. The minimum clinical followup of the 27 survivors was 23 years (mean, 29 years; range, 23–38 years). The minimum followup for the 15 patients who filled out questionnaires was 24 years (mean, 30 years; range, 24–38 years). We did not recall any patients specifically for this study; all data were obtained from medical records and questionnaires. We obtained prior Institutional Review Board approval.
The latest clinical followup for these patients typically included a clinical examination by a local physician or a musculoskeletal oncologist at our institution. Twenty seven patients had a chest CT scan or chest radiograph obtained at latest followup, radiograph of their pelvis, and/or a CT scan or MRI of their pelvis. We reviewed all medical records. Clinic visits and radiographic examinations were supplemented by letters and questionnaires provided by our institutional cancer registry to obtain survival, local recurrence, metastases, and incidence of late reconstructive procedures. We developed a specific questionnaire (Appendix 1) and sent it to all 38 patients who were alive with no evidence of disease in 1989 to assess tumor recurrence, tumor metastases, and functional scores, including Musculoskeletal Tumor Society (MSTS) score and Toronto Extremity Salvage score (TESS). There were 27 survivors, 15 of whom returned the questionnaire. We did not perform functional assessment for the 12 patients who did not return the functional questionnaire, but we were able to obtain their clinical data from their medical records for determination of survival of their tumor, local recurrence, metastases, and further reconstructive procedures. The patients filled out the functional questionnaires, which limited bias. We calculated the patient’s MSTS and TESS scores by utilizing standard scoring, as previously published [2, 4]. We compared individual patients’ 1989 MSTS scores to their current MSTS scores at long-term followup (range, 24–38 years). Although we were only able to obtain 15 of 27 questionnaires for functional scores, each patient who returned the functional questionnaire served as his/her own control since we could compare 1989 and current MSTS scores for each patient. We performed subgroup analysis of the functional scores based on type of resection. The classification of internal hemipelvectomies was based on the resected region of the innominate bone from posterior to anterior: Type 1 = ilium; Type 2 = periacetabular region, and Type 3 = pubis. En bloc resection of the ilium and sacral ala was classified as an extended Type 1 [3, 4, 8, 10].
Results
At 23 to 38 years, the overall survival was 45% (27 of 60): 59% (20 of 34) of patients with chondrosarcoma and 23% (three of 13) patients with osteosarcoma were alive. The survival rate for all causes, assuming the four patients lost to followup were deceased, of the 38 patients reported alive with no evidence of disease in 1989 was 71% (27 of 38) (Table 1): 100% Stage IA (one of one), 75% Stage IB (15 of 20), 31% Stage IIB (11 of 36), and 0% Stage III (none of three) were alive (Table 2). Of the 34 patients with long-term followup data, two died late of their disease (Table 1).
Table 1.
Data for the 38 patients with no evidence of disease in 1989 [8]
| Diagnosis | Current status | Followup (years) | Initial resection | Enneking stage | Grade | Margin | Reconstruction | Pelvic recurrence | Metastases | 1989 MSTS score | Current MSTS score | Current TESS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chondrosarcoma | Alive | 30 | III | IB | 1 | Wide | None | No | No | 30 (100%) | 28 (93%) | 77 |
| Chondrosarcoma | Alive | 31 | III | IB | 1 | Marginal | None | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 32 | II/III | IB | 1 | Wide | None | No | No | 30 (100%) | 22 (73%) | 69 |
| Chondrosarcoma | Alive | 24 | IIA/III | IIB | 2 | Wide | Iliofemoral arthrodesis | No | No | 26 (73%) | 16 (53%) | 54 |
| Chondrosarcoma | Alive | 30 | Extended I | IB | 1 | Wide | 3 wires | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 25 | I | IB | 1 | Wide | None | Yes: 1999, surgically resected | No | 30 (100%) | 24 (80%) | 68 |
| Chondrosarcoma | Alive | 38 | I | IB | 1 | Marginal | None | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 28 | III | IB | 1 | Marginal | None | Yes: converted to external hemipelvectomy 2002 | No | 30 (100%) | 1 (3%) | 48 |
| Chondrosarcoma | Alive | 33 | I | IB | 1 | Marginal | Bone grafting | Yes: 1977, surgically resected; none since | No | 30 (100%) | 28 (93%) | 100 |
| Chondrosarcoma | Alive | 29 | I | IB | 1 | Marginal | None | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 25 | II/III | IIB | 2 | Wide | Iliofemoral arthrodesis | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 34 | IIA/III | IB | 1 | Wide | Iliofemoral arthrodesis | No | No | 9 (27%) | 4 (13%) | 44 |
| Chondrosarcoma | Alive | 29 | I | IB | 1 | Wide | None | No | No | 22 (83%) | 22 (73%) | 81 |
| Chondrosarcoma | Alive | 29 | III | IB | 1 | Wide | None | No | No | 29 (96%) | 30 (100%) | 96 |
| Chondrosarcoma | Alive | 33 | I/IIA/III | IIB | 2 | Contaminated wide | Attempted iliofemoral arthrodesis, failed, pseudoarthrosis | No | No | 25 (83%) | 16 (53%) | 39 |
| Chondrosarcoma | Alive | 29 | II/III | IB | 1 | Contaminated wide | Steinmann pin and cast | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 32 | III | IIB | 2 | Contaminated wide | None | No | No | 28 (93%) | 24 (80%) | 61 |
| Chondrosarcoma | Alive | 28 | III | IB | 1 | Marginal | None | Yes: 2003, surgically resected | No | 30 (100%) | 18 (60%) | 58 |
| Chondrosarcoma | Alive | 28 | I/II/III | IB | 1 | Wide | None | No | No | NA | NA | NA |
| Chondrosarcoma | Alive | 25 | II/III | IIB | 2 | Wide | Attempted Iliofemoral arthrodesis, failed, pseudoarthrosis | No | No | NA | NA | NA |
| Telangiectatic osteosarcoma | Alive | 29 | Extended I | IIB | 3 | Marginal | None | No | No | 28 (93%) | 28 (93%) | 77 |
| Osteoblastic osteosarcoma | Alive | 26 | I/IIA/III | IIB | 4 | Wide | Iliofemoral arthrodesis | No | No | 7 (23%) | 9 (30%) | 60 |
| Osteosarcoma | Alive | 38 | Extended I | IIB | 4 | Wide | None | No | Yes: lung 1972/1973; none since | 7 (23%) | 8 (27%) | 49 |
| Multifocal epithelioid hemangioendothelioma | Alive | 26 | I | IA | I | Marginal | None | No | Yes: right humerus 1994, left scapula 1985 | NA | NA | NA |
| Ewing’s sarcoma | Alive | 26 | I/IIA/III | IIB | 4 | Wide | None | No | No | NA | NA | NA |
| Ewing’s sarcoma | Alive | 25 | III | IIB | 4 | Wide | None | No | No | NA | NA | NA |
| Dermatofibrosarcoma | Alive | 23 | I | IIB | 2 | Wide | None | No | Yes: clavicular region, surgically resected | NA | NA | NA |
| Osteosarcoma | Dead of disease | Died 1990 (6 years) | Extended I | IIB | 2 | Wide | Bone grafting | No | Metastatic disease in thoracic spine | NA | NA | NA |
| Chondroblastic osteosarcoma | Dead of disease | Died 1990 (6 years) | II/III | IIB | 3 | Wide | Iliofemoral arthrodesis | No | Pulmonary metastases resections 1984, 1986 | NA | NA | NA |
| Myxoid fibrosarcoma | Dead of prostate cancer | Died 2003 (21 years) | Extended I | IIB | 3 | Marginal | None | No | No | NA | NA | NA |
| Chondrosarcoma | Dead of other causes | Died 2008 (36 years) | I | IB | 1 | Wide | Bone grafting | No | No | NA | NA | NA |
| Chondrosarcoma | Dead of other causes | Died 1998 (15 years) | II/III | IB | 3 | Wide | Iliofemoral arthrodesis | No | No | NA | NA | NA |
| Osteosarcoma | Dead of other causes | Died 1999 (16 years) | II/III | IIB | 4 | Wide | Iliofemoral arthrodesis | No | No | NA | NA | NA |
| Chondrosarcoma | Dead of unknown causes | Died 1995 (12 years) | Extended I | IB | 3 | Wide | Bone grafting | No | Pulmonary metastases resection 1986 and 1987 | NA | NA | NA |
| Fibrosarcoma | Lost to followup (presumed dead) | Lost to followup after 1991 (14 years) | II/III | IB | 1 | Marginal | Bone grafting | None known, lost after 1991 | None known, lost after 1991 | NA | NA | NA |
| Chondrosarcoma | Lost to followup (presumed dead) | Lost to followup after 1989 (7 years) | II/III | IB | 1 | Wide | None | None known, lost after 1989 | None known, lost after 1989 | NA | NA | NA |
| Ewing’s sarcoma | Lost to followup (presumed dead) | Lost to followup after 1989 (4 years) | III | IIB | 4 | Wide | None | None known, lost after 1989 | None known, lost after 1989 | NA | NA | NA |
| Hemangiopericytoma | Lost to followup (presumed dead) | Lost to followup after 1991 (8 years) | Extended I | IB | 1 | Marginal | Bone grafting | None known, lost after 1991 | None known, lost after 1991 | NA | NA | NA |
MSTS = Musculoskeletal Tumor Society; TESS = Toronto Extremity Salvage score; NA = not available.
Table 2.
Survival based on surgical stage of 60 malignant pelvic tumors
| Enneking stage | Number of patients | Number of patients alive at 23- to 38-year followup | Survival rate |
|---|---|---|---|
| IA | 1 | 1 | 100% |
| IB | 20 | 15 | 75% |
| IIA | 0 | ||
| IIB | 36 | 11 | 31% |
| III | 3 | 0 | 0% |
Of the 34 patients with long-term followup data, 24 had pelvic chondrosarcoma; of these, three had a late local recurrence (12.5%). All late recurrences were Stage IB, Grade 1 pelvic chondrosarcoma. Wide excision had a 7% late local recurrence (one of 14) and marginal excision had a 33% late local recurrence (two of six). Three patients had a contaminated wide margin but no recurrence. Treatment of these late local recurrences consisted of surgical resection, including conversion to external hemipelvectomy in one patient, and all remain disease-free.
In 1989, 21 patients had metastatic disease of our original index 60 patients (35%). Late metastatic disease to bone developed in two additional patients, resulting in an overall metastasis rate of 38% (23 of 60), 87% (20 of 23) of whom died of their disease. Both of the late metastases were bone metastases (Table 1), and these patients underwent resection and were disease-free at last followup. No patient developed late pulmonary metastases; one patient alive at long-term followup had pulmonary metastasis resection in 1972 [8].
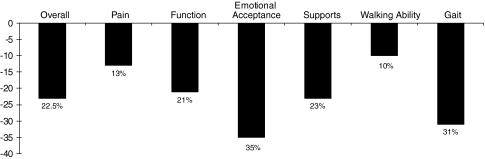
We saw a decline in function at long-term followup. In the 15 patients who filled out questionnaires, the current average TESS score was 66 (range, 39–100) (Fig. 1) and the current average MSTS score was 18.5 (range, 1–30) or 62% (range, 3%–100%), compared with an average MSTS score of 24 (range, 7–30) or 80% (range, 23%–100%) reported in 1989, which represents a 22.5% functional decline in MSTS score over 30 years. The largest decline occurred in emotional acceptance (35%), followed by gait (31%) (Fig. 2). Subgroup analysis of functional outcome based on type of resection demonstrated the largest decline (35%) in Type II/III or IIA/III resections (Table 3). We attempted to perform an analysis on the change in patients’ functional scores based on the specific type of pelvic reconstructive procedure; however, only three of 15 patients with functional data had an iliofemoral arthrodesis, while the rest had no reconstructive procedure performed, so no such an analysis could be performed (Table 1). Two case examples of patients with chondrosarcoma treated with internal hemipelvectomy are shown at long-term followup (Figs. 3, 4).
Fig. 1.
A graph shows an average MSTS score in 1989 of 80%, a current average MSTS score of 62%, and a current TESS score of 66, demonstrating a 22.5% functional decline over 30 years.
Fig. 2.
A graph shows a functional decline in MSTS scores seen over 30 years, with an overall average of 22.5% and the largest declines in emotional acceptance (35%) and gait (31%).
Table 3.
Functional decline of 15 patients based on type of surgical resection
| Type of resection | Number of patients | Functional decline in MSTS score |
|---|---|---|
| Type I or IA and partial sacrum | 2 | 0% |
| Type I | 3 | 7% |
| Type III | 2 | 14% |
| Type I/IIA/III | 4 | 22% |
| Type II/III or IIA/III | 3 | 35% |
MSTS = Musculoskeletal Tumor Society.
Fig. 3.
A radiograph shows a patient with multiple hereditary exostoses with secondary chondrosarcoma 33 years after Type I internal hemipelvectomy. This patient had a 1989 MSTS score of 30 (100%) and currently has a MSTS score of 28 (93%) and a TESS of 100.
Fig. 4.
A radiograph shows a patient with chondrosarcoma who underwent a Type IIA/III internal hemipelvectomy and reconstruction with iliofemoral arthrodesis. In 1989, his MSTS score was 26 (73%), and at 24-year followup, his MSTS score is 16 (53%) and his TESS is 54.
We identified late related surgeries for complications from pelvic limb salvage in two patients. One patient underwent femoral lengthening to improve limb shortening and one underwent three hernia operations (Fig. 5). No patients underwent conversion to another type of pelvic reconstruction or additional late pelvic reconstructive procedures.
Fig. 5.
A radiograph shows a patient who underwent late femoral lengthening to improve limb shortening.
Discussion
Salvage of the limb for patients with malignant pelvic tumors continues to be challenging in terms of adequate resection to minimize the risk of metastases and local recurrences and restore function. External hemipelvectomy frequently allows adequate margins but is associated with substantial morbidity and limited function. Limb salvage offers an alternative approach when adequate margins can be achieved, but long-term function and survival are unclear. In patients who underwent limb-sparing surgery of the pelvis, we determined (1) the long-term survival, (2) risk of developing late local recurrence, (3) risk of developing late metastases, (4) possible change in function at long-term followup, and (5) the incidence of further reconstructive procedures at long-term followup.
There were important limitations of our study. First, due to the retrospective nature of our study, we could not determine the time course for the functional decline we observed as we only were able to compare their 1989 MSTS score to their current MSTS score at most recent followup. Second, during this time, imaging modalities improved (CT/MRI) and new imaging modalities were introduced (positron emission tomography/CT), which may have influenced localization of pelvic disease and accuracy of staging. Third, during the study period of 1970 to 1985, the majority of reconstructions were iliofemoral arthrodesis or no reconstruction at all. While reconstructive capabilities have expanded, no patient in this series underwent additional pelvic reconstructive surgery. Finally, we could not perform an analysis of the patients’ functional scores as a factor of their reconstructive procedure owing to the variations in reconstructions. Therefore, we are uncertain whether these influenced survival or local recurrences.
Our long-term survival of 45% (27 of 60) at 23 to 38 years is comparable to the literature, with a range of 42% to 71% survival at short- to medium-term followup (Table 4). In our series, 75% of patients with Stage IB pelvic sarcoma were alive at 23 to 38 years versus 31% of patients with Stage IIB pelvic sarcoma. All patients with Stage III died within 5 years and were reported in our initial publication [8]. This rate is similar to those in the literature, ranging from 77% to 97% survival for Stage IB and 23% to 75% for Stage IIB [7, 10, 12, 14]. If a patient with pelvic sarcoma is free of disease 5 years after sarcoma resection, the subsequent risk of death from sarcoma for that patient appears to be low.
Table 4.
Comparison of literature reporting results for pelvic tumor treatment
| Study | Mean followup (years) | Total number of patients | Overall survival | Local recurrence | Metastases | Functional MSTS score |
|---|---|---|---|---|---|---|
| Enneking and Dunham [3] | 4 | 32 | 23 (71%) | 9 (28%) | 9 (28%) | 72% good |
| Fuchs et al. [5] | 3.5 | 43 | 13 (30%) | 15 (35%) | 21 (49%) | NA |
| Huth et al. [6] | 5 | 53 | 22 (42%) | 6 (11.3%) | NA | Fair result |
| Mankin et al. [7] | 5.2 | 206 | 104 (50%) | 14 (7%) | 122 (60%) | NA |
| Pring et al. [10] | 11.6 | 64 | 45 (70%) | 12 (19%) | 11 (17%) | 77% |
| Sheth et al. [12] | 9.6 | 67 | 40 (60%) | 19 (28%) | 23 (36%) | NA |
| Shin et al. [13] | 6 | 41 | 21 (51%) | 1 (2%) | 20 (49%) | NA |
| Wirbel et al. [14] | 4 | 93 | 46 (50%) | 17 (18%) | 33 (35%) | 63% good or excellent |
| Sherman et al. | 30 | 60 | 27 (45%) | 13 (22%) | 23 (38%) | 62% |
MSTS = Musculoskeletal Tumor Society; NA = not available.
Patients with pelvic chondrosarcoma appeared to be at particular risk of late local recurrence (three of 24). Our original report demonstrated a 17% rate of local recurrence (10 of 59) in which we performed en bloc excision of the malignant pelvic tumor; therefore, the overall local recurrence rate at 23 to 38 years was 22% (13 of 59). This is comparable to the literature, with a range of 7% to 35% local recurrence rate at short- to medium-term followup (Table 4). We suggest continued monitoring for local recurrence of these patients beyond 5 years after index resection, with CT or MRI of the pelvis performed on an annual basis, particularly for those patients with chondrosarcoma. As previous reports show, a wide margin should be the surgical goal [3, 7, 10, 14]. Our marginal excision patients with long-term followup had a 40% (two of five) rate of local recurrence versus 9% (one of 11) rate of local recurrence with wide excisions. If late local recurrence develops, long-term survival could still be achieved with additional surgery. In our experience, only one of three patients with late local recurrence required conversion to an external hemipelvectomy.
Only two patients had late metastases; both had spread to bone. No patient developed late pulmonary metastases. Our overall metastases rate was 38% (23 of 60), comparable with the literature of 17% to 60%. Based on our limited data, we cannot recommend guidelines for long-term monitoring for the development of metastatic disease, but in our experience, pulmonary metastases after 5 years are rare.
Our long-term functional data demonstrated a functional decline of 22.5% over 23 to 38 years. Ritter et al. [11] demonstrated Harris hip scores decline at an average of 0.67 points per year between 3 and 10 years after THAs with no evidence of radiographic loosening and concluded deterioration in the functional capacity of aging patients is an important factor in longitudinal studies using scoring systems. It is likely the functional capacity of our aging patients influenced the functional decline over 23 to 38 years. However, we saw the largest functional decline in emotional acceptance (35%). We speculated, with longer followup, the focus of patients shifted from being sarcoma survivors to being functionally impaired individuals. This decline in function, especially in emotional acceptance, may be helpful information to provide to patients who are considering undergoing an internal hemipelvectomy.
The incidence of late reconstructive surgery was low. Only two patients underwent further reconstructive procedures related to their pelvic resection but not the tumor: one underwent femoral lengthening and the other had three hernia operations. It is encouraging that patients did not require further conversion to another type of pelvic reconstruction and that there were few late surgical procedures.
If satisfactory margins are achieved, we believe internal hemipelvectomy with limb salvage remains appropriate for tumor control and function. We found rates of survival similar to those reported in the literature at short- to mid-term followup. Surgical stage of malignant pelvic tumors correlates with long-term survival. Patients with pelvic chondrosarcoma appear to be at risk of late local recurrence, especially with marginal excisions. If a patient with pelvic sarcoma is free of disease 5 years after sarcoma resection, the subsequent risk of death from sarcoma for that patient appears to be low.
Appendix 1
Questionnaire 







Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Mayo Clinic, Rochester, MN.
References
- 1.Beck LA, Einertson MJ, Winemiller MH, DePompolo RW, Hoppe KM, Sim FH. Functional outcomes and quality of life after tumor-related hemipelvectomy. Phys Ther. 2008;88:916–927. doi: 10.2522/ptj.20070184. [DOI] [PubMed] [Google Scholar]
- 2.Davis AM, Wright JG, Williams JI, Bombardier C, Griffin A, Bell RS. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res. 1996;5:508–516. doi: 10.1007/BF00540024. [DOI] [PubMed] [Google Scholar]
- 3.Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978;60:731–746. [PubMed] [Google Scholar]
- 4.Enneking WF, Dunham WK, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 5.Fuchs B, Hoekzema N, Larson DR, Inwards CY, Sim FH. Osteosarcoma of the pelvis: outcome analysis of surgical treatment. Clin Orthop Relat Res. 2009;467:510–518. doi: 10.1007/s11999-008-0495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huth JF, Eckardt JJ, Pignatti G, Eilber FR. Resection of malignant bone tumors of the pelvic girdle without extremity amputation. Arch Surg. 1988;123:1121–1124. doi: 10.1001/archsurg.1988.01400330097015. [DOI] [PubMed] [Google Scholar]
- 7.Mankin HJ, Hornicek FJ, Temple HT, Gebhardt MC. Malignant tumors of the pelvis: an outcome study. Clin Orthop Relat Res. 2004;425:212–217. doi: 10.1097/00003086-200408000-00030. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor MI. Malignant pelvic tumors: limb-sparing resection and reconstruction. Semin Surg Oncol. 1997;13:49–54. doi: 10.1002/(SICI)1098-2388(199701/02)13:1<49::AID-SSU8>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor MI, Sim FH. Salvage of limb in the treatment of malignant pelvic tumors. J Bone Joint Surg Am. 1989;71:481–494. [PubMed] [Google Scholar]
- 10.Pring ME, Weber KL, Unni KK, Sim FH. Chondrosarcoma of the pelvis: a review of sixty-four cases. J Bone Joint Surg Am. 2001;83:1630–1642. [PubMed] [Google Scholar]
- 11.Ritter MA, Thong AE, Davis KE, Berend ME, Meding JB, Faris PM. Long-term deterioration of joint evaluation scores. J Bone Joint Surg Br. 2004;86:438–442. doi: 10.1302/0301-620X.86B3.14243. [DOI] [PubMed] [Google Scholar]
- 12.Sheth DS, Yasko AW, Johnson ME, Ayala AG, Murray JA, Romsdahl MM. Chondrosarcoma of the pelvis: prognostic factors for 67 patients treated with definitive surgery. Cancer. 1996;78:745–750. doi: 10.1002/(SICI)1097-0142(19960815)78:4<745::AID-CNCR9>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 13.Shin KH, Rougraff BT, Simon MA. Oncologic outcomes of primary bone sarcomas of the pelvis. Clin Orthop Relat Res. 1994;304:207–217. [PubMed] [Google Scholar]
- 14.Wirbel RJ, Schulte M, Mutschler WE. Surgical treatment of pelvic sarcomas: oncologic and functional outcome. Clin Orthop Relat Res. 2001;390:190–205. doi: 10.1097/00003086-200109000-00022. [DOI] [PubMed] [Google Scholar]