Abstract
Objective
To assess whether outcomes of strabismus surgery are improved by using the adjustable suture technique and to determine which subgroups of strabismus patients benefit most from the adjustable suture technique.
Design
A retrospective chart review.
Participants
Five hundred thirty-five adults who had strabismus surgery between 1989–2010.
Methods
Success was defined as ≤10 prism diopters (PD) for horizontal deviations and ≤2 PD for vertical deviations. Differences in the proportion of successful strabismus surgery were analyzed using a chi-square test with an alpha of 0.05.
Main outcome measures
Ocular alignment in primary position at a 7-day to 12-week follow-up examination.
Results
491 patients met the inclusion criteria (adjustable suture, n=305; non-adjustable, n=186). The success rates for non-adjustable and adjustable groups were 61.3% and 74.8% respectively (χ2=9.91, p=0.0016). Adjustable suture use was particularly beneficial for patients undergoing a reoperation for childhood strabismus (success rate: non-adjustable, 42.4%; adjustable, 65.7% p=0.0268; n=100). The differences in outcomes were not statistically significant for patients with childhood strabismus undergoing a primary surgery (non-adjustable, 65.0%; adjustable, 81.4% p=0.1354; n=90) or with thyroid orbitopathy (non-adjustable, 76.7%; adjustable, 74.1% p=0.8204; n=57).
Conclusions
Strabismus surgery using adjustable sutures was associated with improved short-term ocular alignment compared to strabismus surgery without the use of adjustable sutures. Adjustable sutures were most beneficial for patients undergoing reoperations for childhood strabismus.
BACKGROUND
The prevalence of adult strabismus is estimated to be 4%.1 Strabismus may be present in adults for a variety of reasons including uncorrected or residual childhood strabismus, intracranial injury or disease, thyroid orbitopathy, impaired vision in one eye, and surgically induced trauma to the extraocular muscles. Strabismus in adults may be associated with diplopia, torticollis, impaired stereopsis, and negative psychosocial effects, which may negatively impact daily living and the quality of life.2,3 Strabismus surgery in adults has a high rate of success, and has been shown to be beneficial in improving diplopia, binocular fusion, and psychosocial functioning.3–6 Furthermore, adult strabismus surgery has been shown to be cost effective, with a health value similar to that of cataract surgery.7
The use of adjustable sutures has been advocated to improve the outcome of strabismus surgery; however, its efficacy has not been established.8 While some case series have reported improved outcome using adjustable sutures, others have shown no benefit.8, 9, 10 A recent Cochrane survey found no evidence to support the use of adjustable sutures when performing strabismus surgery.8 We performed a retrospective study of over 500 adults who had undergone strabismus surgery at one institution with and without adjustable sutures to determine whether our patients who underwent strabismus surgery using an adjustable technique had better outcomes than our patients who underwent non-adjustable surgery.
MATERIALS AND METHODS
Subjects and Data Collection
A retrospective chart review was conducted on adults who had strabismus surgery at the Emory Eye Center between 1989–2010. Approval for the study was obtained from the Emory University Institutional Review Board. A list of adults who underwent strabismus surgery between 1989–2010 was generated using surgical logs and current procedural terminology (CPT) codes. 629 charts were acquired for review based on availability; 94 patients were excluded for the following reasons: insufficient information in the chart, the strabismus was secondary to a congenital fourth nerve palsy, or the surgery was to correct congenital nystagmus rather than strabismus. We excluded patients with congenital fourth nerve palsies because they are generally treated with an inferior oblique recession, which is not amenable to the adjustable suture technique. Patients with acquired fourth nerve palsy were included in the study.
Three surgeons (SRL, AKH, AVD) performed all of the surgeries; two frequently used adjustable sutures, whereas the third used them infrequently. Several different adjustable suture techniques were used. One surgeon primarily used a “bowtie” technique while the other surgeons used a “cinch knot” technique. Surgery was carried out using regional anesthesia, conscious sedation, or general anesthesia. Regional anesthesia was primarily used for the first few years of the study, whereas general anesthesia was primarily used for the last 15 years of the study. The majority of the muscles placed on adjustable sutures were recessed. Patients who underwent the adjustable suture technique had the adjustment performed either on the same day or the following day, using topical 0.5% proparacaine instilled prior to adjustment.
Case report forms (CRFs) were completed for each patient. Each patient was de-identified and assigned an identification number. If the patient had more than one preoperative examination, the examination temporally closest to the surgery or the examination with the most complete information was used for the analysis. The following clinical information was recorded on the preoperative CRF: best-corrected visual acuity, versions, etiology of strabismus, ocular co-morbidities, type of strabismus, previous surgical treatment, and if there was a reason for excluding the patient from the adjustable procedure. Preoperative deviation(s) in primary, near, and downward gaze were recorded. We did not exclude patients who had both horizontal and vertical deviations. The surgery CRF detailed the surgical procedure, use of adjustable suture and amount adjusted, and any intraoperative complications. For this study, we only looked at the initial strabismus surgery that each patient had at our institution; we did not look at any subsequent surgeries they may have had at our institution.
Information from the initial follow-up examination was recorded on postoperative CRFs. The initial follow-up examination ranged from 7 days to 12 weeks. We used the examination between 2 and 4 weeks for the initial follow-up if it was available or if there were multiple follow-up examinations between the 7-day to 12-week period, as it was the most consistent initial follow-up period between the three surgeons. The initial follow-up CRF detailed postoperative parameters, such as best-corrected visual acuity, any postoperative complications, and ocular alignment in primary, near, and downgaze. The appropriate forms for each patient were faxed, validated, and stored in the DataFax System.
Statistical analysis
We chose to focus on the success of ocular alignment in the distance in primary gaze because it was the most consistently recorded data point and the goal of most strabismus surgeries is to achieve acceptable alignment in primary gaze. Prior to starting the chart review, success, based on ocular alignment in primary gaze position, was defined as ≤10 prism diopters (PD) for horizontal deviations and ≤2 PD for vertical deviations, as they have been defined in previous studies.1, 11, 12 Patients who only had a dissociated vertical deviation (DVD) at follow-up examinations were considered orthotropic, since DVDs are usually a latent phenomenon. The means and percentages for patient characteristics were compared across adjustable suture groups using the Student t-test and the chi-square test. Differences in the proportion of successful strabismus surgery were analyzed using a chi-square test. The chi-square test was used to compare the success rate of all those surgeries done without adjustable sutures to those performed with adjustable sutures. Statistical calculations were performed using SAS and statistical significance was set as a two-sided p-value of 0.05.
Subgroup analysis
We conducted analyses on subgroups that met the 7-day to 12-week inclusion criteria. For our subgroup analyses, we focused on the etiologies with the greatest number of patients: childhood onset strabismus undergoing a primary surgery, childhood onset strabismus undergoing a reoperation, and thyroid orbitopathy. We did not perform a subgroup analysis on patients with strabismus arising from multiple etiologies (e.g. childhood strabismus and thyroid orbitopathy) in order to minimize confounding factors. Differences in the proportion of successful strabismus surgery for the childhood strabismus group undergoing a primary surgery were analyzed using the Fisher exact test. Differences in the proportion of successful strabismus surgery for the other subgroups were analyzed using a chi-square test.
Histograms
Histograms were created using the vertical and horizontal deviation measurements that were available for all 491 patients. These measurements were taken from the postoperative visit closest to 4 weeks for the adjustable and nonadjustable groups.
RESULTS
Preoperative results
Five hundred and thirty five patients met the initial inclusion criteria. Of these patients, 491 had ocular alignment in primary gaze recorded in the chart during the 7-day to 12-week postoperative follow-up period. There were 285 women and 206 men. The predominant etiologies included childhood strabismus, trauma, thyroid orbitopathy, vision loss, retinal detachment surgery, cerebral vascular accidents, and myotoxicity from regional anesthesia (Table 1). The total number of etiologies listed exceeds 535 as some of the patients fit into multiple categories (eg. a patient with a traumatic etiology may have also had a cranial nerve palsy). The 79 patients in the “miscellaneous” category had etiologies that included: chronic progressive external ophthalmoplegia, arteriovenous malformations, meningiomas, brainstem tumors, aneurysm clippings, etc. The patients were also divided into groups based on the type of deviation they had: esotropia, exotropia, hypertropia, or combined horizontal and vertical deviations. Within the non-adjustable group, 22.5% had an esotropia only and 19.3% had an exotropia only. Within the adjustable group, 15.0% had an esotropia only and 13.8% had an exotropia only. We believe that this balance of patients with esotropia only and exotropia only within each group is important, since there may be an improved outcome with strabismus surgery for patients with esotropia compared to patients undergoing strabismus surgery for an exotropia. For the non-adjustable group with only a horizontal or a vertical deviation, the mean preoperative deviations were: esotropia, 41 PD; exotropia, 40 PD; and hypertropia, 15 PD. In the adjustable group with only a horizontal or a vertical deviation, the mean preoperative deviations were: esotropia, 34 PD; exotropia, 39 PD; and hypertropia, 12 PD. For those with a combined horizontal and vertical deviation in the non-adjustable group, the mean preoperative horizontal and vertical deviations were: esotropia, 25 PD; exotropia, 34 PD; and hypertropia, 12 PD. For those with combined horizontal and vertical deviation in the adjustable group the mean preoperative deviations were: esotropia, 24 PD; exotropia, 29 PD; hypertropia, 12 PD (Table 2).
Table 1.
Etiology of strabismus
| Etiology | Number |
|---|---|
| Childhood strabismus | 210 |
| Trauma | 105 |
| Thyroid orbitopathy | 68 |
| CN VI palsy | 37 |
| Vision loss | 31 |
| Retinal detachment surgery (+/− scleral buckle placement) | 27 |
| CN III palsy | 24 |
| Cerebral Vascular Accident (CVA) | 20 |
| CN IV palsy (non-congenital) | 17 |
| Myotoxicity from local anesthesia | 12 |
| Duane syndrome | 9 |
| Glaucoma shunt surgery | 5 |
| Brown syndrome | 1 |
| Miscellaneous | 79 |
Table 2.
Preoperative alignment in primary position
| Alignment type | Non-adjustable group | Adjustable group |
|---|---|---|
| ET1 only | ||
| Number of patients | n=42 | n=74 |
| Amount (average PD2) | 41Δ 3± 22Δ (range 10–95) | 34Δ ± 18Δ (range 12–110) |
|
| ||
| XT4 only | ||
| Number of patients | n=36 | n=68 |
| Amount (average PD) | 40Δ ± 22Δ (range 4–95) | 39Δ ± 19Δ (range 5–90) |
|
| ||
| Vertical deviation only | ||
| Number of patients | n=16 | n=20 |
| Amount (average PD) | 15Δ ± 8Δ (range 5–35) | 12Δ ± 5Δ (range 2–25) |
|
| ||
| Horizontal and vertical deviation combination | ||
| Horizontal ET | ||
| Number of patients (average PD) | n=38 25Δ ± 20Δ (range 2–90) |
n=48 24Δ ± 17Δ (range 1–85) |
| Horizontal XT | ||
| Number of patients (average PD) | n=51 34Δ ± 23Δ (range 2–90) |
n=84 29Δ± 16Δ (range 2–65) |
| Vertical | ||
| Number of patients (average PD) | n=89 12Δ ± 15Δ (range 1–90) |
n=132 12Δ ± 11Δ (range 1–60) |
ET = Esotropia
PD = Prism diopter
Δ = Prism diopter
XT = Exotropia
Surgery results
Of the 491 patients analyzed, 305 underwent surgery when at least 1 muscle was put on an adjustable suture whereas 186 patients underwent surgery without adjustable sutures. One hundred and seventy-four women and 131 men underwent surgery using adjustable sutures and 111 women and 75 men underwent surgery without adjustable sutures (χ2=0.3277, p=0.5670). The mean age at surgery for the adjustable group was 45.0 years (range, 12.4–85.7 years) versus 45.4 years (range, 12.4–88.1 years) for the non-adjustable sutures (t-test=0.26, p=0.7922). Of the 305 patients who underwent surgery using the adjustable suture technique, 251 (82.3%) subsequently needed adjustment postoperatively. In most cases, the use of adjustable sutures was dictated by surgeon preference. However, in 17 (3.46%) patients, adjustable sutures were not used due to patient preference, poor patient cooperation, or intraoperative findings that would preclude the use of an adjustable suture. The intraoperative complications for the non-adjustable group included 2 corneal abrasions, 2 cases of ptosis, 1 case of conjunctival laceration, and 1 case of postoperative bleeding. In the adjustable group, there were 11 cases of corneal abrasions, 5 cases of ptosis, and 1 conjunctival buttonhole.
Initial post-operative follow-up
The initial follow-up examination ranged from 7 days to 12 weeks. The mean follow-up time was 33.8 days for the non-adjustable surgery group and 32.7 days for the adjustable group. The success rates for the non-adjustable and adjustable groups were 61.3% and 74.8% respectively (χ2=9.91, p=0.0016) for the 7-day to 12-week follow-up period. The difference in success rate between the three surgeons was not statistically significant (p=0.5594). The mean postoperative deviations for the non-adjustable group at the initial follow-up examination were: esotropia, 10 PD; exotropia, 18 PD; and hypertropia, 8 PD. The mean postoperative deviations for the adjustable group at the initial follow-up examination were: esotropia, 8 PD; exotropia, 13 PD; and hypertropia, 5 PD. For those with combined horizontal and vertical deviation in the non-adjustable group, the mean deviations were: esotropia, 13 PD; exotropia, 14 PD; and hypertropia, 11 PD. For those with combined horizontal and vertical deviation in the adjustable group, the mean deviations were: esotropia, 10 PD; exotropia, 14 PD; and hypertropia, 8 PD (Table 3).
Table 3.
Postoperative alignment in primary position
| Alignment type | Non-adjustable group | Adjustable group |
|---|---|---|
| ET1 only | ||
| Number of patients | n=21 | n=41 |
| Amount (average PD2) | 10Δ3± 5Δ (range 2–20) | 8Δ± 8Δ (range 1–40) |
|
| ||
| XT4 only | ||
| Number of patients | n=26 | n=32 |
| Amount (average PD) | 18Δ± 19Δ (range 1–95) | 13Δ± 8Δ (range 1–35) |
|
| ||
| Vertical deviation only | ||
| Number of patients | n=13 | n=28 |
| Amount (average PD) | 8Δ± 9Δ (range 1–35) | 5Δ± 5Δ (range 1–25) |
|
| ||
| Horizontal and vertical deviation combination | ||
| Horizontal ET | ||
| Number of patients (average PD) | n=28 13Δ± 13Δ (range 2–60) |
n=22 10Δ± 6Δ (range 1–20) |
| Horizontal XT | ||
| Number of patients (average PD) | n=24 14Δ± 19Δ (range 1–90) |
n=30 14Δ± 23Δ (range 1–134) |
| Vertical | ||
| Number of patients (average PD) | n=52 11Δ± 14Δ (range 1–90) |
n=52 8Δ± 5Δ (range 1–30) |
ET = Esotropia
PD = Prism diopter
Δ = Prism diopter
XT = Exotropia
Figures 1 and 2 show histograms comparing postoperative ocular deviations for horizontal and vertical deviations respectively for the adjustable and nonadjustable groups in 5 PD bins. For horizontal deviations, there is a higher percentage of patients in the orthotropic, 5 PD and 10 PD bins in the adjustable group compared to the non-adjustable group. While there is a small percentage of patients in the 25 and 30 PD bins, there are many more extreme outliers in the non-adjustable group including a patient with a 90 PD deviation. For vertical deviations, there is also a higher percentage of patients in the orthotropia and 5 PD bins in the adjustable group. In addition, aside from one extreme outlier, there are fewer extreme outliers in the adjustable group compared to the non-adjustable group.
Figure 1.
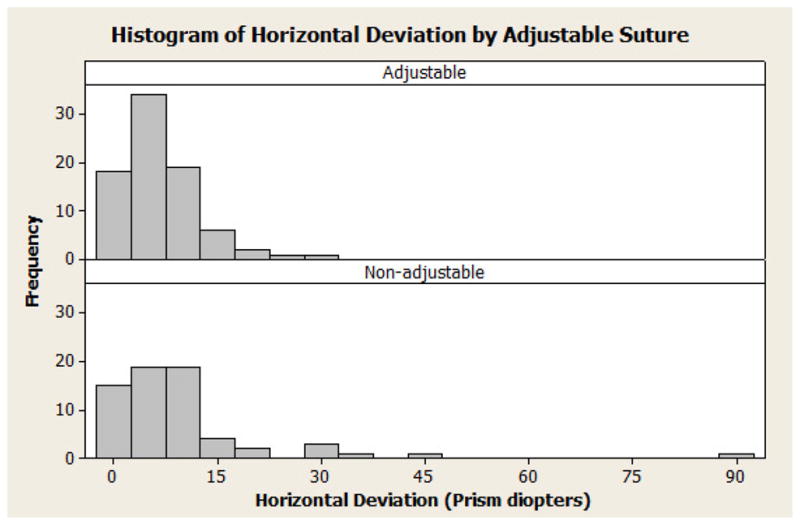
Histogram of horizontal deviations in 5 prism diopter bins for adjustable (top) and nonadjustable (bottom) groups.
Figure 2.
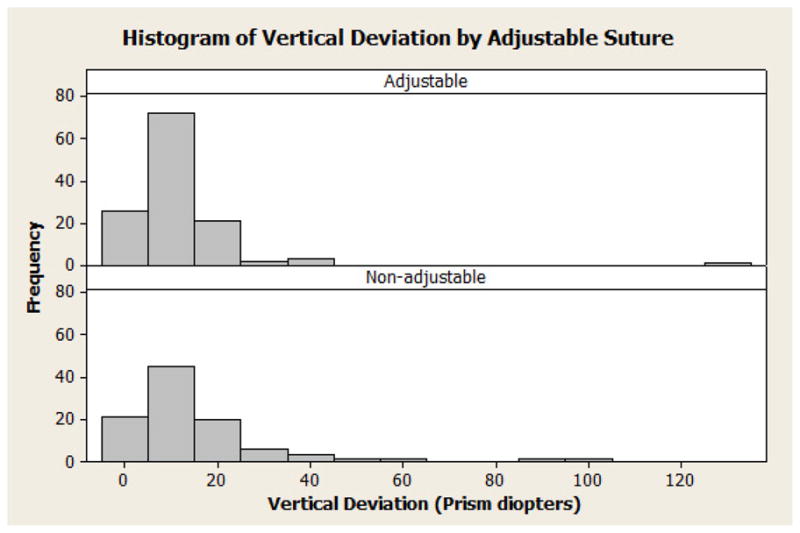
Histogram of vertical deviations in 5 prism diopter bins for adjustable (top) and non-adjustable (bottom) groups.
The postoperative complications for the non-adjustable group at the initial follow-up examination included 1 case each of cellulitis, conjunctival inclusion cyst, dellen, conjunctival abscess, traumatic mydriasis, ectropion, and pyogenic granuloma. The postoperative complications for the adjustable group included 4 cases of suture granulomas, and 1 case each of cellulitis, conjunctival inclusion cyst, eyelid retraction, pyogenic granuloma, and spastic entropion.
Subgroup Analyses
Childhood Strabismus
There were 90 patients with childhood strabismus only who had not had surgery previously and 100 patients with childhood strabismus only who had undergone strabismus surgery previously. In the group undergoing primary surgery the success rate was 65.0% in the non-adjustable group and 81.4% in the adjustable group (p=0.1354). In the group undergoing a reoperation, the success rate was 42.4% in the non-adjustable group and 65.7% in the adjustable group (χ2=4.91, p=0.0268) (Table 4).
Table 4.
Success Rates by Group
| Group | Non-adjustable group (n) | Non-adjustable group success (%) | Adjustable group (n) | Adjustable group success (%) | p-value |
|---|---|---|---|---|---|
| Overall | 186 | 61.3% | 305 | 74.8% | 0.0016 |
| Childhood strabismus— reoperation (n=100) | 33 | 42.4% | 67 | 65.7% | 0.0268 |
| Childhood strabismus— primary operation (n=90) | 20 | 65.0% | 70 | 81.4% | 0.1354 |
| Thyroid orbitopathy (n=57) | 30 | 76.7% | 27 | 74.1% | 0.8204 |
Thyroid Orbitopathy
There were 57 patients with thyroid orbitopathy who underwent strabismus surgery, 27 using the adjustable method and 30 using the non-adjustable technique. The success rates were 76.7% for the non-adjustable group and 74.1% for the adjustable group (χ2=0.05, p=0.8204). Of 57 patients, 54 patients were undergoing a primary operation and 3 a reoperation. The reoperation group was not sufficiently large to conduct a test of significance to compare the outcome between primary operations and reoperations (Table 4).
DISCUSSION
Overall, we found that there was a statistically significant difference in the proportion of patients who have a successful surgical outcome as defined in this study. Patients who underwent strabismus surgery using adjustable sutures were more likely to have a successful outcome than patients who underwent surgery using a non-adjustable technique, as determined at the seven-day to twelve-week follow-up period. The success rate improved from 61.3% to 74.8% when adjustable sutures were used. A high percentage of patients in the adjustable group received postoperative adjustment (82.3%). This is a higher percentage than what has been reported by Velez et al. (45%), Bishop and Doran (54%), and Tripathi et al. (69.5%).9, 10, 13 This may reflect differences in our surgical nomograms, surgical techniques or patient selection. The adjustable technique was particularly helpful in patients with childhood onset strabismus undergoing a reoperation. In this group, the success rate in aligning the patient within 10 horizontal PD and/or within 2 vertical PD of orthotropia in primary position increased from 42.4% to 65.7% when adjustable sutures were used—a statistically significant difference. While we found an improved success rate with adjustable sutures in patients with childhood onset strabismus undergoing their first operation the difference was not statistically significant. We did not find any improvement in the ocular alignment of patients with thyroid orbitopathy using the adjustable suture technique. The combined intraoperative and postoperative rate of complications for the non-adjustable and adjustable groups were 7.0% and 8.5% respectively. These rates, however, may not include all complications, since some minor complications, such as conjunctival buttonholes and tears, were not always documented. There were no vision-threatening complications in either treatment group.
Strabismus in adults can be challenging to correct with surgery. The success of this procedure may be improved with the use of adjustable sutures. Previous studies have shown that the use of adjustable sutures may be particularly beneficial for certain types of strabismus. Currie et al. reported a success rate of 77% in 26 adults after surgical correction of large-angle exotropias using the adjustable suture technique.14 Keech and Heckert reported a success rate of 78% in a cohort of 51 patients who underwent strabismus surgery with adjustable sutures for acquired vertical deviations.11 Keech et al. reviewed 333 patient s who had undergone strabismus surgery using the adjustable suture technique and proposed that the use of adjustable sutures was most helpful for patients with vertical and complex deviations.15
We found the adjustable suture technique to be most helpful in patients with childhood strabismus undergoing reoperations. This is not surprising since the success rate of strabismus surgery is generally acknowledged to be lower with reoperations. Weston reported a lower success rate for patients with esotropia or exotropia undergoing reoperations (81% and 74% respectively) compared to patients undergoing primary surgeries (88% for both groups).12 We also found that patients with childhood strabismus undergoing a reoperation (non-adjustable group, 42.4%; adjustable group, 65.7%) had a lower success rate than patients undergoing a primary operation (non-adjustable group, 65.0%; adjustable group, 81.4%). The lower success rate associated with reoperations likely arises from many factors including postoperative adhesions and a selection bias for deviations that are less amenable to accurate surgical alignment.16, 17
Our histograms of postoperative ocular deviations for both vertical and horizontal deviations show that there was a higher percentage of patients who were orthotropic or had only a small postoperative deviation. In addition, there were fewer outliers in the adjustable group compared to the non-adjustable group. This was particularly true for vertical deviations. The improved mean ocular alignment in the adjustable group therefore reflects a reduction in the number of outliers as well as a higher percentage of patients who had excellent alignment.
We found a nearly identical success rate for the adjustable and non-adjustable groups in patients with thyroid eye disease. Lueder et al. followed 47 patients with thyroid orbitopathy treated with adjustable sutures for a mean of 41 months.18 Of those patients, only 47% had an “excellent” outcome, defined as the resolution of their double vision in the primary and reading positions without the use of prisms. It is difficult to compare our success rate with that reported by Lueder, since we used a different definition of “success.” Thyroid eye disease typically has a restrictive component that may limit surgical options as well as postoperative attempts to adjust muscle placement. Postoperative changes from inflammation or disease flare further contribute to making surgical outcomes less predictable. Fawcett et al. determined that a shorter duration of constant eye misalignment and the pre-surgical capacity for binocularity are the factors most predictive of the restoration of macular binocular vision for adults with acquired strabismus.19 Since thyroid eye disease is an acquired form of strabismus that begins after binocular visual maturation, as compared to most forms of childhood strabismus, the excellent fusional potential of these patients may allow them to overcome residual deviations that patients with poor fusion would not be able to control.
There were some limitations to our study. Since this was a retrospective, non-randomized study, bias was inherently present. Since one of the surgeons performed strabismus surgery using adjustable sutures less frequently than the other two surgeons, this could have biased our results, particularly if one surgeon was consistently more or less successful than the other two surgeons in achieving a successful ocular alignment. To explore this confounding variable, we analyzed the success rate of the three surgeons independent of the surgical technique and did not find a statistically significant difference in outcomes. Due to time limitations, we were not able to analyze the medical record of every adult patient who underwent strabismus surgery at our institution between 1989 and 2010. Instead, we randomly reviewed the medical records for a subset of patients who met our inclusion criteria. Ideally, we would have matched each patient in the adjustable group with one in the non-adjustable group. We also used a wide time interval for the initial follow-up examination, although, the mean follow-up time was nearly equal between the two groups. Because of this, certain patients may have experienced more postoperative drift from the time of surgery until they were examined. Weston et al. found that most postoperative drift occurs within the first 8 weeks after surgery when adjustable sutures are used.12 Other studies have reported that strabismus surgery using fixed scleral sutures is associated with a longer duration of postoperative drift compared to strabismus surgery using adjustable sutures.20, 21 We did not look at success rates, changes in ocular alignment, and need for additional surgeries with a longer follow-up interval as there was not a consistent time point for long-term follow-up examinations. In addition, the sample sizes for our subgroups were quite small. Finally, we did not calculate the Intensity/Complexity Index of each surgery performed. The average surgical complexity of the non-adjustable and adjustable groups, as well as each subgroup may have helped us determine whether it was an important parameter in the success of the surgeries. Preferentially utilizing adjustable sutures in higher complexity cases may have created a selection bias that might argue against their efficacy since these cases are inherently less likely to succeed.
Given the retrospective nature of our study, we elected to define success based solely on ocular alignment rather than basing it on the elimination of diplopia or psychosocial considerations, as these factors were not consistently recorded in the chart pre or postoperatively. Hatt and coworkers prospectively analyzed the responsiveness of 2 health-related quality-of-life (HRQOL) questionnaires, which address diplopia, motor function, and psychosocial functioning in adult strabismus patients.22 Their results indicate that the questionnaires are indeed responsive to improved HRQOL in this patient population, particularly the Adult Strabismus-20 questionnaire. These findings warrant the administration of HRQOL questionnaires pre and postoperatively in order to establish a standardized and to provide a more comprehensive definition of a “successful” outcome based on both objective and subjective factors.
The decision to define ocular alignment ≤10 PD for a horizontal deviation and ≤2 PD for a vertical deviation as “successful” was somewhat arbitrary. While this definition has been used in many other strabismus surgery studies, a definition based on physiological considerations might be preferable.1, 11, 12 For instance, Leske and Holmes have reported stereopsis is achieved more often if a patient has a horizontal deviation ≤4 PD.23 Perhaps, a residual horizontal deviation of 4 PD or less would be a better endpoint since it is based on the physiological goal of stereopsis. Since we based our definition of success entirely on ocular alignment, it may not accurately reflect patients’ perception of success. Many patients with what we defined as “unsuccessful” outcomes may have been happy with the outcome if their goal was to restore a more normal appearance to their eyes or to achieve better control of a large intermittent deviation. In contradistinction, other patients who we defined as having a “successful” outcome may have been unhappy with the outcome if they still had diplopia or reduced stereopsis postoperatively. Although our results showed improved ocular alignment outcomes when adjustable sutures are used, potentially negative factors such as patient cooperation and discomfort during adjustment must be weighed against the benefits of their use. Testing patients’ ability to tolerate conjunctival manipulation and assessing cooperation preoperatively may aid in determining which patients would be suitable candidates for adjustable suture use.
In summary, we found strabismus surgery using adjustable sutures to be associated with better short-term alignment compared to strabismus surgery using fixed sutures. Adjustable sutures were most helpful in patients undergoing reoperations for childhood strabismus. Prospective randomized clinical trials with longer follow-up periods and greater numbers of patients with particular etiologies are needed to further elucidate the potential benefits of strabismus surgery using adjustable sutures.
Acknowledgments
We would like to thank Phoebe Lenhart and Natario Couser for their insightful suggestions.
Supported in part by NIH Departmental Core Grant EY06360 and Research to Prevent Blindness, Inc, New York, New York.
Footnotes
Conflict of Interest: None of the authors have any conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Beauchamp GR, Black BC, Coats DK, et al. The management of strabismus in adults--I. Clinical characteristics and treatment. J AAPOS. 2003;7:233–40. doi: 10.1016/s1091-8531(03)00112-5. [DOI] [PubMed] [Google Scholar]
- 2.Hatt SR, Leske DA, Kirgis PA, et al. The effects of strabismus on quality of life in adults. Am J Ophthalmol. 2007;144:643–7. doi: 10.1016/j.ajo.2007.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills MD, Coats DK, Donahue SP, Wheeler DT Ophthalmic Technology Assessment Committee Pediatric Ophthalmology Panel. Strabismus surgery for adults: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1255–62. doi: 10.1016/j.ophtha.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Merrill K, Satterfield D, O’Hara M. Strabismus surgery on the elderly and the effects on disability. J AAPOS. 2010;14:196–8. doi: 10.1016/j.jaapos.2009.12.282. [DOI] [PubMed] [Google Scholar]
- 5.Jackson S, Harrad RA, Morris M, Rumsey N. The psychosocial benefits of corrective surgery for adults with strabismus. Br J Ophthalmol. 2006;90:883–8. doi: 10.1136/bjo.2005.089516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mets MB, Beauchamp C, Haldi BA. Binocularity following surgical correction of strabismus in adults. J AAPOS. 2004;8:435–8. doi: 10.1016/j.jaapos.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Beauchamp CL, Beauchamp GR, Stager DR, Sr, et al. The cost utility of strabismus surgery in adults. J AAPOS. 2006;10:394–9. doi: 10.1016/j.jaapos.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Sundaram V, Haridas A. Adjustable versus non-adjustable sutures for strabismus. Cochrane Database Syst Rev. 2005;(1):CD004240. doi: 10.1002/14651858.CD004240.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Tripathi A, Haslett R, Marsh IB. Strabismus surgery: adjustable sutures-good for all? Eye (Lond) 2003;17:739–42. doi: 10.1038/sj.eye.6700465. [DOI] [PubMed] [Google Scholar]
- 10.Bishop F, Doran RM. Adjustable and non-adjustable strabismus surgery: a retrospective case-matched study. Strabismus. 2004;12:3–11. doi: 10.1076/stra.12.1.3.29010. [DOI] [PubMed] [Google Scholar]
- 11.Keech RV, Heckert RR. Adjustable suture strabismus surgery for acquired vertical deviations. J Pediatr Ophthalmol Strabismus. 1988;25:159–63. doi: 10.3928/0191-3913-19880701-03. [DOI] [PubMed] [Google Scholar]
- 12.Weston B, Enzenauer RW, Kraft SP, Gayowsky GR. Stability of the postoperative alignment in adjustable-suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1991;28:206–11. doi: 10.3928/0191-3913-19910701-05. [DOI] [PubMed] [Google Scholar]
- 13.Velez FG, Chan TK, Vives T, et al. Timing of postoperative adjustment in adjustable suture strabismus surgery. J AAPOS. 2001;5:178–83. doi: 10.1067/mpa.2001.114661. [DOI] [PubMed] [Google Scholar]
- 14.Currie ZI, Shipman T, Burke JP. Surgical correction of large-angle exotropia in adults. Eye (Lond) 2003;17:334–9. doi: 10.1038/sj.eye.6700347. [DOI] [PubMed] [Google Scholar]
- 15.Keech RV, Scott WE, Christensen LE. Adjustable suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1987;24:97–102. doi: 10.3928/0191-3913-19870301-11. [DOI] [PubMed] [Google Scholar]
- 16.Dunlap EA. Surgery of muscle adhesions and effects of multiple operations. Br J Ophthalmol. 1974;58:307–12. doi: 10.1136/bjo.58.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheha H, Casas V, Hayashida Y. The use of amniotic membrane in reducing adhesions after strabismus surgery. J AAPOS. 2009;13:99–101. doi: 10.1016/j.jaapos.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Lueder GT, Scott WE, Kutschke PJ, Keech RV. Long-term results of adjustable suture surgery for strabismus secondary to thyroid ophthalmopathy. Ophthalmology. 1992;99:993–7. doi: 10.1016/s0161-6420(92)31866-4. [DOI] [PubMed] [Google Scholar]
- 19.Fawcett SL, Felius J, Stager DR. Predictive factors underlying the restoration of macular binocular vision in adults with acquired strabismus. J AAPOS. 2004;8:439–44. doi: 10.1016/j.jaapos.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Pukrushpan P, Isenberg SJ. Drift of ocular alignment following strabismus surgery. Part 1: using fixed scleral sutures. Br J Ophthalmol. 2009;93:439–42. doi: 10.1136/bjo.2007.136390. [DOI] [PubMed] [Google Scholar]
- 21.Isenberg SJ, Abdarbashi P. Drift of ocular alignment following strabismus surgery. Part 2: using adjustable sutures. Br J Ophthalmol. 2009;93:443–7. doi: 10.1136/bjo.2007.136382. [DOI] [PubMed] [Google Scholar]
- 22.Hatt SR, Leske DA, Holmes JM. Responsiveness of health-related quality-of-life questionnaires in adults undergoing strabismus surgery. Ophthalmology. 2010;117:2322–8. doi: 10.1016/j.ophtha.2010.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]


