ABSTRACT
BACKGROUND
In 2005 the Spoken Knowledge in Low Literacy in Diabetes scale (SKILLD) was introduced as a diabetes knowledge test. The SKILLD has not been validated since its introduction.
OBJECTIVE
To perform a validation analysis on the SKILLD.
DESIGN AND PARTICIPANTS
Cross-sectional observational study of 240 patients with diabetes at an academic family practice center.
MAIN MEASURES
SKILLD’s correlation with an oral form of the Diabetes Knowledge Test (DKT) was used to assess criterion validity. A regression model tested construct validity, hypothesizing that SKILLD score was independently related to health literacy and education level. Content validity was tested using Cronbach’s Alpha for inter-item relatedness and by comparing SKILLD items with the content of a National Institutes of Health (NIH) diabetes education website. We assessed inter-rater reliability and bias using Spearman correlation coefficients and sign-rank tests between interviewers scoring the same interview.
KEY RESULTS
The SKILLD demonstrated fair correlation with the DKT (Pearson’s coefficient 0.54, 95% CI = 0.49 to 0.66, p < 0.001). Health literacy, education level, male gender, household income, and years with diabetes were independent predictors of SKILLD score in the regression model. Cronbach’s Alpha for inter-item relatedness was 0.54. There were some topics on the NIH website not addressed by the SKILLD. The inter-rater correlation coefficient was 0.79 (95% CI 0.56 to 0.91, p < 0.001).
CONCLUSIONS
The SKILLD is an adequate diabetes knowledge test and is appropriate for people of all literacy levels. However, it should be expanded to more completely evaluate diabetes knowledge.
KEY WORDS: diabetes knowledge, health literacy, diabetes education, validation
BACKGROUND
Diabetes mellitus is a leading cause of morbidity, diminished quality of life, and mortality in the United States.1,2 Although guidelines exist for diabetes care3, less than half of those with diabetes have good control of their glucose.4 The reasons for this lack of good control includes physician, patient, and system factors.5
Self-management support, one of the principles of the Chronic Care Model, involves a collaborative effort of clinicians helping patients acquire the necessary knowledge, skills and confidence to manage their diabetes.6 Patients with diabetes must acquire a significant degree of new knowledge after diagnosis. For example, they must learn to recognize symptoms, risks and adverse consequences of hyperglycemia and hypoglycemia, engage in proper foot care, calculate carbohydrates, and perhaps administer insulin.
Studies have shown that patients who score well on a diabetes knowledge test, with or without an educational intervention, generally have better clinical outcomes than those who score poorly.7–18 Higher diabetes-related knowledge (DRK) has been associated with improved glucose control11, lower blood pressure11, enhanced quality of life10,14,19,20, and improved self-care behaviors such as dietary adherence11,12,21–23, home glucose monitoring11,12,20,21, increased exercise11,21, and foot inspection11,21. Assessment of DRK by the validated Michigan Diabetes Knowledge Test (DKT)24 may help determine what diabetes education is required, and to monitor knowledge educational progress over time.
Unfortunately, limited health literacy may pose a barrier to delivery of diabetes care.25–28 Health literacy is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”29 Limited health literacy is prevalent30–33 and associated with poorer glycemic control.26,27,34–36
A disparity in DRK has been observed between those with low and high health literacy both following37 and unrelated to27 an educational intervention.
This disparity is addressed with interventions designed to improve diabetes-related knowledge for a range of literacy levels38–40, and with those designed exclusively for patients with low literacy.37,41–43 However, there is only one published DRK test specifically designed for individuals with low literacy: the Spoken Knowledge in Low Literacy in Diabetes scale (SKILLD).44 Since its introduction in 2005, the SKILLD has not been validated in a population of patients with diabetes and wide range of health literacy levels.
The purpose of this study is to further validate the use of the SKILLD for application in clinical and research practice. To do so, we sought to answer the following questions: Does the SKILLD relate to other validated measures of DRK (criterion validity)? Does it relate to other variables the way a satisfactory DRK test should (construct validity)? Are its test items a reasonable sample of what a diabetic patient should know (content validity)? Are the scores meaningfully reproducible between interviewers (inter-rater reliability) and populations (external validity)? We hypothesized that the SKILLD would adequately perform these tasks.
METHODS
Data Collection
This study is part of a larger research protocol designed to study the association of health literacy with DRK, patient behaviors, and health outcomes. The Ohio State University Biomedical Institutional Review Board approved this protocol.
As part of the larger study protocol, participants were invited to sit for a one-hour interview conducted by trained research assistants. After consenting to participate, subjects provided demographic information and answered a verbal questionnaire. Data were collected from their medical record. Subjects took in random order the following battery of tests: the Michigan Diabetes Knowledge Test (DKT), the Rapid Estimate of Adult Literacy in Medicine (REALM), and the SKILLD, and two other literacy tests related to the larger protocol. Participants were asked at the end of each test to rate the difficulty of that test.
The DKT is a multiple-choice exam meant to test a patient’s knowledge about topics relevant to diabetes self-care.24 The first 16 questions are relevant to any patient with diabetes, whereas the last seven apply only to those who are using insulin. This test was administered orally, which has been shown to correlate extremely well with the written DKT and is recommended for persons with unknown health literacy or poor visual acuity (Miser WF, Jeppesen KM, Coyle J, unpublished data, 2009).
The REALM, perhaps the most widely used test of health literacy that can be administered in one to two minutes, consists of three lists of 22 words each, to be read aloud by the test taker.45 A score is given based on how many words the subject pronounces correctly. Although this test is meant primarily as a screening tool, its results correlate well to other previously developed literacy tests.
The SKILLD was developed in 2005 by Rothman et al. to screen patients with diabetes and low literacy for deficits in self-care knowledge.44 Administered orally, it is a 10-item, open-answer test. Questions ask about behaviors patients should have to best manage their diabetes. As the questions are open-ended, alternative wording is provided for each of the 10 questions. Question #3 of the SKILLD asks how to treat low blood sugar and requires an answer regarding some form of oral glucose plus rechecking blood sugar. Although this is correct according to the medical standards established by the American Diabetes Association3, there is some concern that checking the glucose may not be considered by some to be “treatment.” As such, we separately recorded whether the subjects mentioned to check their blood sugar. A subsample of SKILLD tests was audio recorded and graded by three different graders to determine inter-rater reliability.
Participants
The population consisted of all patients diagnosed with diabetes mellitus (ICD code 250.xx) seen at least twice at the Ohio State University Rardin Family Practice Center in Columbus, Ohio from August 25, 2006 to December 5, 2007. Patients were contacted either in person at the office, via telephone shortly prior to an appointment, or randomly if no appointment was scheduled. Potential participants were excluded if they were under 18 years of age, pregnant, did not speak English, or had a known cognitive defect that would interfere with their ability to complete the interview.
Data Analyses
Time to complete the test, difficulty ratings, and relationships of SKILLD with demographic variables were summarized and face validity was assessed. Formal analyses were designed to test criterion validity, construct validity, content validity and reliability of the SKILLD. All analyses were performed with STATA SE version 9.2 (StataCorp. 2005. College Station, TX). P-values were considered significant at alpha < 0.05 unless otherwise mentioned.
To assess criterion validity, the extent to which a test relates to another previously validated metric, we compared SKILLD scores to oral DKT scores using Pearson’s correlation coefficient, with an acceptable value being > 0.6. We calculated confidence intervals using Fisher’s Z transformation. To establish construct validity, the extent to which a test behaves as we would expect it to given our understanding of the concept to be measured, we hypothesized that DRK would be independently related to both education level attained and health literacy level. We created a regression model predicting SKILLD using the REALM and highest education level attained as independent variables. The model also controlled for age, gender, race, household income, use of insulin, and years with diabetes. We considered the construct valid if both education level and health literacy were independent, significant predictors of SKILLD score in this model, after adjusting for covariates.
We tested content validity, the extent to which a test’s material matches the material we wish to test, using two methods. First, we calculated Cronbach’s Alpha for inter-item relatedness, considering 0.6 < alpha <0.9 an ideal range. Second, we compared the concepts tested in the SKILLD to the domain of topics found in seven educational pamphlets, a video, and an informational web page produced by the National Institute of Health’s National Diabetes Education Program (NDEP).46 To assess inter-rater reliability, agreement between various test administrators, we calculated the Fleiss Kappa statistic for each item using scores obtained from the three different graders previously described. We tested overall reliability and accuracy by calculating Spearman correlation coefficients and sign-rank test p-values, comparing the original grader to the other two graders.
RESULTS
We contacted 384 patients with diabetes to participate in this study; 40 were excluded (6 were blind, 25 spoke little or no English, nine had a cognitive deficit). Of the 344 remaining, 243 consented to participate (71% response rate). During test administration, one subject was excluded due to newly discovered dementia, one subject refused to finish the battery of tests, and results from one subject’s SKILLD test was incomplete, leaving complete data available for analysis for 240 subjects. Subjects who participated were not significantly different from non-participating patients with respect to age, gender, race, and years with diabetes. Table 1.
Table 1.
Characteristics of 240 Subjects with Diabetes who Took the Spoken Knowledge in Low Literacy in Diabetes Scale (SKILLD)
| Characteristic | Number | % | Mean or Median |
|---|---|---|---|
| Gender (male) | 74 | 30.8 | |
| Age (years) | Mean = 54.0; S.D. ± 1.8 | ||
| Race | |||
| White | 105 | 43.8 | |
| Black | 110 | 45.8 | |
| Other | 25 | 10.4 | |
| Annual household income (U.S. dollars) | Median = $25,000 IQR = $12,000 : $50,000 |
||
| Years with diabetes | Median = 7; IQR = 3 : 13 | ||
| Insulin use (yes) | 68 | 28.3 | |
| Highest education level completed | |||
| 6th grade | 4 | 1.7 | |
| 11th grade | 37 | 15.4 | |
| 12th grade or GED equivalent | 71 | 29.6 | |
| Some college | 58 | 24.1 | |
| Associates degree | 22 | 9.1 | |
| Bachelor’s degree | 27 | 11.3 | |
| Master’s degree or higher | 21 | 8.8 | |
| REALM category † | |||
| 0–18 (≤3rd grade) | 7 | 2.9 | |
| 19–44 (4th to 6th grade) | 14 | 5.8 | |
| 45–60 (7th to 8th grade) | 59 | 24.6 | |
| 61–66 (high school) | 150 | 62.5 | |
| SKILLD score (number correct, 0–10) ‡ | Mean = 6.8; S.D. ± 1.8 | ||
| Time to administer SKILLD (seconds) | Median = 225; IQR = 182:273 |
||
| Difficulty rating of SKILLD | |||
| Very easy | 37 | 15.4 | |
| Easy | 127 | 52.9 | |
| Okay | 61 | 25.4 | |
| Hard | 14 | 5.8 | |
| Very hard | 1 | 0.4 | |
†Analysis excluded 10 patients who did not take the REALM because of poor vision
‡ For item 3, failing to mention “and check your blood sugar” was not graded as incorrect
S.D. = standard deviation. IQR = interquartile range. Ref = referent group
The SKILLD took a median of 225 (inter-quartile range = 182, 273) seconds to complete. Its median difficulty rating was “easy,” compared to “okay” for the oral DKT. Crude associations with SKILLD score are given in Table 2 (“Unadjusted” columns). A higher SKILLD score was obtained more frequently in subjects with non-black race, higher income, use of insulin, higher education level, higher REALM score, shorter test time, and easier difficulty rating.
Table 2.
Regression Model Predicting Spoken Knowledge in Low Literacy in Diabetes Scale (SKILLD) Score
| Unadjusted | Adjusted for Other Variables | |||
|---|---|---|---|---|
| Variable | Coefficient* (95% CI) | P-Value | Coefficient* (95% CI) | P-Value |
| Male gender | −0.42 (−0.92, 0.09) | 0.10 | −0.61 (−1.07, -0.15) | 0.01 |
| Age | −0.02 (−0.04, 0.000) | 0.05 | −0.02 (−0.035, 0.001) | 0.07 |
| Black race‡ | −0.70 (−1.2, -0.21) | 0.01 | −0.09 (−0.57, 0.38) | 0.69 |
| Other race‡ | −0.40 (−1.2, 0.39) | 0.32 | −0.20 (−0.93, 0.53) | 0.59 |
| Household income† | 5.1 (2.3, 7.7) | <0.001 | 2.92 (0.09, 5.75) | 0.04 |
| Years with diabetes | 0.026 (−0.003, 0.06) | 0.08 | 0.04 (0.01, 0.07) | 0.02 |
| Insulin use | 0.76 (0.25, 1.3) | 0.004 | 0.48 (−0.03, 1.00) | 0.07 |
| Highest education level§ | 0.40 (0.26, 0.55) | <0.001 | 0.19 (0.02, 0.35) | 0.03 |
| REALM category¶ | 0.87 (0.58, 1.2) | <0.001 | 0.62 (0.30, 0.94) | <0.001 |
| (constant term) | – | – | 4.7 (3.9, 5.4) | <0.001 |
*Unless otherwise stated, coefficients represent unit increase in predicted SKILLD score per unit increase in variable as given in Table 1
†White race was the reference group
‡To improve linearity between income and SKILLD score, the variable used in this regression model was (square root of annual income)/1000
§For the regressions, “6th grade” was coded as 0, “11th grade” as 1, and so on.
¶REALM = Rapid Estimate of Adult Literacy in Medicine. For the regressions, score of 0–18 was coded as 0, 19–44 as 1, and so on.
CI = confidence interval
The research assistants indicated that the SKILLD was able to discriminate a person’s understanding of diabetes. However, they observed that for question #1 and #2, regarding hyper- and hypoglycemia, subjects often stated, “I know how it feels” to have high or low blood sugar, but were unable to indicate specific symptoms. Questions were clearly written, with the exception of #3. “Check blood sugar” is a required part of the answer, but the question appears to focus more on treatment than monitoring. Only 4% of subjects mentioned checking blood sugar in their response.
The open-ended style of the questions, though helpful in an oral test, may lead to ambiguities in grading. The following illustrate responses that may rightly be graded as correct or incorrect. Question #6 asks about frequency of eye checks. “Every six months” is more frequent than the expected answer of “at least yearly”, but may be what a subject’s ophthalmologist has recommended. Question #7 is regarding normal blood sugar values. “90-100” is not the given answer range, but it falls within the accepted range of “70 (or 80) to 120”. Question #9 asks about frequency and duration of exercise. “Every day for 30 minutes” or “three times a week for an hour” could be acceptable exercise regimens but fall outside of the limits of a correct response (“3-5 times per week for a total of 30–45 minutes each”).
The correlation coefficient between the SKILLD and the oral DKT was 0.58 (95% CI 0.49 to 0.66, p < 0.001). The regression model assessing construct validity is found in Table 2 (“Adjusted” columns). Both REALM score and education level were independently associated with SKILLD score after correcting for confounders. Male gender, household income, and years with diabetes were also significantly related to SKILLD in this model. The inter-item Cronbach’s Alpha for the SKILLD scale was 0.54.
Educational materials from the NDEP provide enough information to answer all questions on the SKILLD, but the program also includes information not addressed by the SKILLD, such as frequency of HbA1c testing, blood pressure, triglyceride and cholesterol goals, nutrition, mental health implications, smoking cessation, oral care, and causes of high or low blood glucose.
We recorded 23 interviews for inter-reliability testing. Kappas for individual items are given in the appendix. All calculated Kappa p-values were <0.001. Grading of SKILLD scores were significantly correlated between graders: Spearman’s rho was 0.79 (95% CI 0.56 to 0.91, p < 0.001).
DISCUSSION
Rothman et al. developed and validated the SKILLD in 217 low income, poorly educated, low literacy patients with poorly controlled diabetes (average A1c was 10.8%).44 They found that the SKILLD had good reliability and validity in measuring diabetes knowledge in those with type 2 diabetes and low literacy. They also demonstrated that individuals with low literacy or lower economic status had poorer knowledge of diabetes, and that the results of the SKILLD was associated with metabolic control (that is, the higher the score of the SKILLD, the better the A1c).
Our construct validity analysis leads us to believe that health literacy and education level correlate well with SKILLD score independent of one another. Rothman et al. reported similar findings. This is indicative of a good knowledge test. Other portions of our analysis raise some noteworthy questions.
We analyzed the criterion validity using Pearson’s coefficient in which we evaluated how well the SKILLD predicted knowledge compared to the oral DKT. Previously two of the authors (WFM and KMJ) observed that the oral DKT evaluates knowledge as well as the written DKT (unpublished, 2009). The results of the current analysis demonstrate an only moderate correlation between the knowledge evaluated by the SKILLD and that evaluated by the oral DKT. This shows that, while they are similar, the SKILLD and the oral DKT are not the same test. It does not, however, indicate that one test is superior to the other, a point brought up in the original paper, which had no criterion validity measure. The SKILLD may be preferred because of its lower perceived difficulty, the practical nature of the questions, and its coverage of general concepts about diabetes management.
Our content validity analysis revealed a separate shortcoming that should be addressed. The domain of knowledge provided by the NDEP website was not sufficiently tested in the SKILLD, which likely led to test items that had little to do with one another resulting in a lower inter-item relatedness (Cronbach’s Alpha = 0.54). Rothman et al. attempted to create a valid short version of the SKILLD due to time constraints of administering a knowledge test in a busy clinical practice.44 Our analysis suggests that the SKILLD may require more questions to fully evaluate the full set of knowledge available on the NDEP website. Attempting to shorten the test may miss useful information. Rothman et al. make the same point, noting that the SKILLD is more skill-related and lacks questions related to nutrition or medication.
Our conclusion about the deficits observed in criterion and content validity is that 1) the format and style of questions in the SKILLD are more practical than those in the DKT and may be an excellent way to test for DRK, but 2) the SKILLD does not have enough questions to adequately assess all domains of DRK. Consideration should be given to expanding the SKILLD into these other domains. Modifying question # 3 could be done as part of this process, since patients may omit “checking blood sugar” as they may not realize this to be a “treatment”.
Our regression analysis indicates that certain variables appear to predict DRK as measured by the SKILLD score. The results support previous findings that patients with a higher education level, health literacy, and income, and use insulin are more likely to have a higher SKILLD score.44 Previous findings found that duration of disease, younger age, and lower HbA1c were also related to higher SKILLD scores.44 We did not investigate a relationship between the SKILLD score and clinical outcomes as our aim was to determine if the SKILLD is a good knowledge test, independent of whether it is associated with metabolic control. Of note, our crude analysis identified a relationship between “non-black race” and DRK, but our regression analysis did not identify race as a predictor of DRK. We, therefore, conclude that race may have an association with another variable that independently correlates with DRK.
Most previous studies have shown a relationship between diabetes education and improved metabolic control.8–16 Our current investigation used schooling level as a measure of education, as did Rothman et al.44 A relationship between education in a disease management program and highest level of education attained may exist, but our literature search yielded no studies that drew direct comparisons. While further investigation is necessary to elucidate such a relationship, our analysis suggests that individuals with a higher education level have more DRK than those with a lower education level. Disease management programs may be used as a tool to increase DRK among those with lower health literacy. However, it is important to note that educational interventions increase knowledge of disease for all participants, and those with lower health literacy are unlikely to experience increases in disease knowledge sufficient to “catch up” to those with higher levels of health literacy enrolled in the same program.37
Current literature suggests that a higher level of health literacy27,37 and education7–16 are related to improved knowledge of disease as well as better disease outcomes.26,27,34,35 There is also an association between higher levels of DRK and many measurements of disease outcomes and self-care behaviors,4,6–8,16–20,36 however this association does not appear to be as strong,11,14,19,20,23,47 suggesting that the relationship between DRK and behaviors that lead to better self-care is not always predictable. “While adequate diabetes knowledge is a prerequisite to good self-care…proper knowledge does not always correlate with patient behaviors”.44
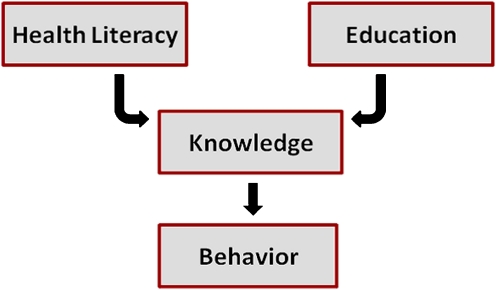
Our analysis demonstrated that higher levels of health literacy and education level independently correlate with higher levels of DRK. We did not attempt to demonstrate the link between DRK (i.e. SKILLD score) and HbA1c (a disease outcome) but we feel confident that the majority of the current literature (as well as our analysis) indicates that the model proposed in Figure 1 is accurate (with the understanding that the relationship between DRK and behaviors may be affected by other variables as well).36
Figure 1.
Construct of Diabetes Knowledge as it relates to Health Literacy, Education, and Behavior.
Limitations
Our patient population was different than that of Rothman et al. who first introduced the SKILLD.40 Our population appears to have a higher level of income, education, and health literacy. While cross verifying a study in a different population is helpful in establishing test validity, neither of these populations was sampled to be nationally representative. Different conclusions may be drawn relating to the use of the SKILLD in private or rural practice, for example. Secondly, although our sample size was adequate to draw our conclusions, we recognize that a more powered study may have led to different conclusions, particularly regarding criterion validity of the SKILLD or other variables that may have predicted SKILLD score.
CONCLUSION
In summary, we consider the SKILLD an adequate diabetes knowledge test with a very useful question format, but should be refined to more fully evaluate DRK. We maintain that any modality to improve the quality of care for patients, enhance the delivery of care by providers, and decrease the cost of treating expensive chronic diseases should be evaluated.
Acknowledgements
The authors would like to thank Mark Stevens, Charlie Pizanis, Stephen Wilkes, Scott Gspandl, Laura Holzer, Patrick Ellsworth, Joan Allen, and the very helpful staff at The Ohio State University Rardin Family Practice Center.
This research was funded by The Ohio State University Crisafi -Monte Primary Care Cardiopulmonary Endowment, and by grant T32RR023260 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH).
Conflict of Interest KMJ, BPH, and MR report no conflicts of interest. WFM has received research funding from Abbott Laboratories, Centocor Ortho Biotech, Inc., Bristol-Myers Squibb, Daiichi Sankyo Co., LTD, Eli Lilly and Company, Forest Research Institute, GlaxoSmithKline, Merck & Co., Inc., Novartis, Novo Nordisk, Pfizer Inc., Sanofi Pasteur, and Wyeth-Ayerst.
Appendix
Table 3 shows Fliess Kappa statistics for each item and the total score.
Table 3.
Fleiss Kappa Statistics for Each Item and Total Score
| Question number and topic | Kappa |
|---|---|
| 1. Symptoms of hyperglycemia | 0.69 |
| 2. Symptoms of hypoglycemia | 0.58 |
| 3. Treatment of hypoglycemia | -* |
| 4. Frequency of foot exams | 1.00 |
| 5. Reason for foot exams | 0.57 |
| 6. Ophthalmology follow-up interval and reason | 0.43 |
| 7. Normal blood sugar value | 0.80 |
| 8. Normal hemoglobin A1C value | 0.87 |
| 9. Exercise recommendations | 0.67 |
| 10. Complications of diabetes | 0.92 |
P < 0.001 for all calculated Kappas in this table. *Question 3 was near-completely graded as correct, so no Kappa is available. Please refer to the original article for exact wording and answers44
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: General information and national estimates of diabetes in the United States, 2005. Bethesda, MD: U.S. Department of Health and Human Services, National Institute of Health; 2005.
- 2.McKinlay J, Marceau L. US public health and the 21st century: diabetes mellitus. Lancet. 2000;356:757–61. doi: 10.1016/S0140-6736(00)02641-6. [DOI] [PubMed] [Google Scholar]
- 3.Standards of medical care in diabetes--2009. Diabetes Care 2009;32 Suppl 1:S13-61. [DOI] [PMC free article] [PubMed]
- 4.Saaddine J, Cadwell B, Gregg E, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med. 2006;144(7):465–74. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 5.Moffet HH, Parker MM, Sarkar U, et al. Adherence to laboratory test requests by patients with diabetes: the diabetes study of northern California (DISTANCE) Am J Manag Care. 2011;17(5):339–344. [PMC free article] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 7.Brown SA. Effects of educational interventions in diabetes care: a meta-analysis of findings. Nurs Res. 1988;37:223–30. [PubMed] [Google Scholar]
- 8.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care. 2002;25:259–68. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scain SF, Friedman R, Gross JL. A structured educational program improves metabolic control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Educ. 2009;35:603–11. doi: 10.1177/0145721709336299. [DOI] [PubMed] [Google Scholar]
- 10.Samuel-Hodge CD, Keyserling TC, Park S, Johnston LF, Gizlice Z, Bangdiwala SI. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ. 2009;35:439–54. doi: 10.1177/0145721709333270. [DOI] [PubMed] [Google Scholar]
- 11.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2005:CD003417. [DOI] [PubMed]
- 12.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–87. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 13.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 2008:CD006424. [DOI] [PubMed]
- 14.Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med. 2006;23:944–54. doi: 10.1111/j.1464-5491.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- 15.Herenda S, Tahirovic H, Poljakovic D. Impact of education on disease knowledge and glycaemic control among type 2 diabetic patients in family practice. Bosn J Basic Med Sci. 2007;7:261–5. doi: 10.17305/bjbms.2007.3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iqbal N, Morgan C, Maksoud H, Idris I. Improving patients’ knowledge on the relationship between HbA1c and mean plasma glucose improves glycaemic control among persons with poorly controlled diabetes. Ann Clin Biochem. 2008;45:504–7. doi: 10.1258/acb.2008.008034. [DOI] [PubMed] [Google Scholar]
- 17.Colleran KM, Starr B, Burge MR. Putting diabetes to the test: Analyzing glycemic control based on patients’ diabetes knowledge. Diabetes Care. 2003;26:2220–1. doi: 10.2337/diacare.26.7.2220. [DOI] [PubMed] [Google Scholar]
- 18.Panja S, Starr B, Colleran KM. Patient knowledge improves glycemic control: is it time to go back to the classroom? J Investig Med. 2005;53:264–6. doi: 10.2310/6650.2005.53509. [DOI] [PubMed] [Google Scholar]
- 19.Corser W, Holmes-Rovner M, Lein C, Gossain V. A shared decision-making primary care intervention for type 2 diabetes. Diabetes Educ. 2007;33:700–8. doi: 10.1177/0145721707304086. [DOI] [PubMed] [Google Scholar]
- 20.Bendik CF, Keller U, Moriconi N, et al. Training in flexible intensive insulin therapy improves quality of life, decreases the risk of hypoglycaemia and ameliorates poor metabolic control in patients with type 1 diabetes. Diabetes Res Clin Pract. 2009;83:327–33. doi: 10.1016/j.diabres.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 21.Arend IJ, Stolk RP, Rutten GE, Schrijvers GJ. Education integrated into structured general practice care for Type 2 diabetic patients results in sustained improvement of disease knowledge and self-care. Diabet Med. 2000;17:190–7. doi: 10.1046/j.1464-5491.2000.00232.x. [DOI] [PubMed] [Google Scholar]
- 22.Miller CK, Gutschall M. A randomized trial about glycemic index and glycemic load improves outcomes among adults with type 2 diabetes. Health Educ Behav. 2009;36:615–26. doi: 10.1177/1090198108317598. [DOI] [PubMed] [Google Scholar]
- 23.Duke SA, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2009:CD005268. [DOI] [PMC free article] [PubMed]
- 24.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21:706–10. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 25.Jeppesen KM, Coyle JD, Miser WF. Screening questions to predict limited health literacy: a cross-sectional study of patients with diabetes mellitus. Ann Fam Med. 2009;7:24–31. doi: 10.1370/afm.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 27.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33:144–51. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 28.Aikens JE, Piette JD. Diabetic patients’ medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care. 2009;32:19–24. doi: 10.2337/dc08-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berkman N, DeWalt D, Pignone M, et al. Literacy and Health Outcomes. Summary, Evidence Report/Technology Assessment No. 87 (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). AHRQ Publication No. 04-E007-1. Rockville, MD: Agency for Healthcare Research and Quality. January 2004.
- 30.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 31.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 32.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 33.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009;32:1614–9. doi: 10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs. 2008;62:74–83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- 36.Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13(3):335–341. doi: 10.1089/dia.2010.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kandula NR, Nsiah-Kumi PA, Makoul G, et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ Couns. 2009;75:321–7. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 38.Wallace AS, Seligman HK, Davis TC, et al. Literacy-appropriate educational materials and brief counseling improve diabetes self-management. Patient Educ Couns. 2009;75:328–33. doi: 10.1016/j.pec.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997;20:254–7. doi: 10.2337/diacare.20.3.254. [DOI] [PubMed] [Google Scholar]
- 40.Rothman R, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004;30:263–73. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 41.Hill-Briggs F, Renosky R, Lazo M, et al. Development and pilot evaluation of literacy-adapted diabetes and CVD education in urban, diabetic African Americans. J Gen Intern Med. 2008;23:1491–4. doi: 10.1007/s11606-008-0679-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wolff K, Cavanaugh K, Malone R, et al. The Diabetes Literacy and Numeracy Education Toolkit (DLNET): materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educ 2009;35:233–6, 38–41, 44–5. [DOI] [PMC free article] [PubMed]
- 43.Kleinbeck C. Reaching positive diabetes outcomes for patients with low literacy. Home Healthc Nurse. 2005;23:16–22. [PubMed] [Google Scholar]
- 44.Rothman RL, Malone R, Bryant B, et al. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005;31:215–24. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 45.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 46.National Diabetes Education Program. Available at: http://www.ndep.nih.gov/. Accessed September 13, 2011.
- 47.Herenda S, Tahirovic H, Zildzic M. Impact of education on metabolic control in type 2 diabetic patients in family practice. Med Arh. 2007;61:236–9. [PubMed] [Google Scholar]