Abstract
Galectin-1 is a lectin recognized by galactoside-containing glycoproteins, and is involved in cancer progression and metastasis. The role of galectin-1 in radiosensitivity has not previously been investigated. Therefore, this study tests whether galectin-1 is involved in the radiosensitivity mediated by the H-Ras signaling pathway using cervical carcinoma cell lines. A knockdown of galectin-1 expression in HeLa cells decreased clonogenic survival following irradiation. The clonogenic survival increased in both HeLa and C33A cells with galectin-1 overexpression. The overexpression or knockdown of galectin-1 did not alter radiosensitivity, whereas H-Ras was silenced in both cell lines. Whereas K-Ras was knocked down, galectin-1 restored the radiosensitivity in HeLa cells and C33A cells. The knockdown of galectin-1 increased the high-dose radiation-induced cell death of HeLa cells transfected by constitutively active H-Ras. The knockdown of galectin-1 inhibited the radiation-induced phosphorylation of Raf-1 and ERK in HeLa cells. Overexpression of galectin-1 enhanced the phosphorylation of Raf-1 and ERK in C33A cells following irradiation. Galectin-1 decreased the DNA damage detected using comet assay and γ-H2AX in both cells following irradiation. These findings suggest that galectin-1 mediates radioresistance through the H-Ras-dependent pathway involved in DNA damage repair.
Keywords: galectin-1, cervical cancer, radiosensitivity, radioresistance, H-Ras
Cancer of the uterine cervix is prevalent in developing countries. Radiotherapy has a significant role in definitive and adjuvant therapy. Local recurrence in patients following radiotherapy presents a challenge because salvaging previously radioresistant tumors using either radiotherapy or surgery with concern for normal tissue complications is difficult. The analysis of our prior study reveals that the overall incidence of local recurrence is 13% following definitive radiotherapy.1 Clinical trials targeting EGFR2, 3, 4 or COX-25, 6, 7 failed to improve the treatment outcome; severe side effects were even noted. Hence, the reconsideration of other molecular targets involving radioresistance will be a future goal.
Galectins are proteins with galactoside-binding glycoproteins. Clinical evidence of galectin involvement in cancer progression is increasing.8 Galectin-1 is associated with a poor prognosis in head and neck cancer9, 10, 11, 12 and prostate cancer.13 Because radiotherapy is among the major therapies of head and neck, prostate, and cervical cancer, investigating the role of galectin-1 in radiation response is valuable.
Based on clinical evidence, two major mechanisms of radioresistance exist, and galectin-1 may involve both. The first factor is DNA repair. Parliament and Murray14 reviewed the clinical evidence of numerous DNA repair genes involving radioresistance. H-Ras involves DNA repair15, 16, 17, 18 and radioresistance.15, 19, 20, 21 In addition, galectin-1 can interact with H-Ras to promote downstream signals.22, 23 The second factor is tumor hypoxia. Hypoxia is a radioresistance-influencing factor for patients with cervical cancer.24, 25 Coincidentally, hypoxia is associated with galectin-1 expression.9, 10, 26 Furthermore, galectin-1 is associated with the progression of cervical cancer.27 Overall, this study explored the association between galectin-1 and radioresistance in cervical cancer cells. The results show that galectin-1 mediates resistance to radiation-induced cell death through H-Ras, but not K-Ras.
Results
Varying expressions of galectin-1 in different cervical cancer cell lines
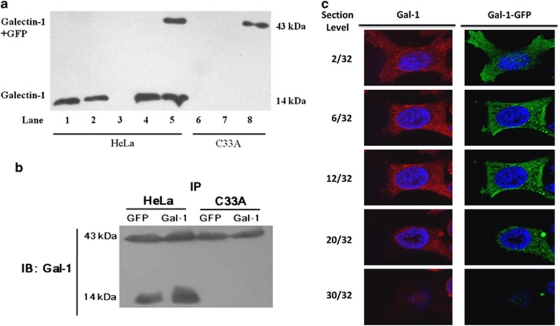
To evaluate the role of galectin-1 in the radiation response of cervical cancer cells, this study first assessed the galectin-1 expression in different cervical cells. We noted a high expression of galectin-1 in HeLa cells and an extremely weak expression of galectin-1 in C33A cells (Figure 1a). Therefore, this study transfected the siRNA of galectin-1 in HeLa cells for knockdown and transfected the cDNA in C33A cells/HeLa cells for galectin-1 overexpression. Transfection of cDNA with green fluorescent protein (GFP) and galectin-1 increased the expression of galectin-1 in HeLa and C33A cells (Figure 1a). The siRNA of galecin-1 inhibited galectin-1 expression in RNA and protein levels (Supplementary Figure S1). In both cells transfected with GFP and galectin-1, immunoprecipitation (IP) for GFP and then immunoblotting for galectin-1 revealed positive galectin-1 (14 kDa) in HeLa cells, but not C33A cells (Figure 1b). The result demonstrated the interaction between endogenous galectin-1 and fusion protein in HeLa cells. In HeLa cells, similar cellular distributions of GFP–galectin-1 fusion protein (green) compared with those of galectin-1 (red) were observed using confocal microscopy (Figure 1c).
Figure 1.
Expression of galectin-1 in HeLa and C33A cells. (a) Cells transfected with GFP only, GFP plus galectin-1, or shRNA were compared with cells without a vector. Lane 1: wild type; lane 2: empty vector; lane 3: shRNA; lane 4: GFP; lane 5: GFP+galectin-1; lane 6: wild type; lane 7: GFP; and lane 8: GFP+galectin-1. (b) Interaction between endogenous galectin-1 and GFP-galectin-1 fusion protein in C33A and HeLa cells. IP was performed for GFP or galectin-1, and then immunoblotting was performed for galectin-1 in both cells transfected with fusion protein. A band (43 kDa) on each lane indicates fusion protein expression formation. A band (14 kDa) on Lane 1 indicates heterodimer formation of endogenous galectin-1 and fusion protein. (c) Distribution of galectin-1 (red color) and GFP-galectin-1 fusion protein (green color) in HeLa cells transfected with GFP-galectin-1 fusion protein
Galectin-1 involves the radioresistance of HeLa and C33A cells
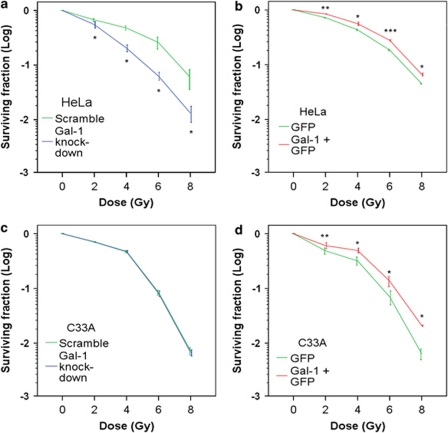
The next step to examine the role of galectin-1 in the radiation response of cervical cancer cells is to perform a clonogenic assay using galectin-1 knockdown in HeLa cells or galectin-1 overexpression in HeLa and C33A cells. HeLa and C33A cells were transfected with scrambled RNA or galectin-1 siRNA 48 h before 0, 2, 4, 6, or 8 Gy of irradiation. HeLa or C33A cells were transfected with GFP vector or galectin-1 cDNA and then irradiated. Significantly lower surviving fractions were noted in HeLa cells (Figure 2a) with galectin-1 knockdown compared with that of scrambled RNA. The clonogenic survival of HeLa (Figure 2b) cells was enhanced by galectin-1 overexpression. Galectin-1 knockdown did not alter clonogenic survival in C33A cells (Figure 2c). However, galectin-1 overexpresssion inhibited radiation-induced cell death in C33A cells (Figure 2d).
Figure 2.
Galectin-1 inhibits radiation-induced cell death. Clonogenic survival curves were compared between (a) galectin-1 knockdown and scrambled RNA in HeLa cells 48 h after transfection (b) galectin-1 cDNA and GFP vectors in HeLa cells (c) galectin-1 knockdown and scrambled RNA in C33A cells 48 h after transfection (d) galectin-1 cDNA and GFP vectors in C33A cells. Cells were irradiated and clonogenic assay performed 12 to 14 days following irradiation. Clonogenic assays were performed during three independent experiments at each paired condition (with and without galectin-1 modulation). The error bar represents the standard error of mean: *P<0.05, **P<0.01, and ***P<0.001
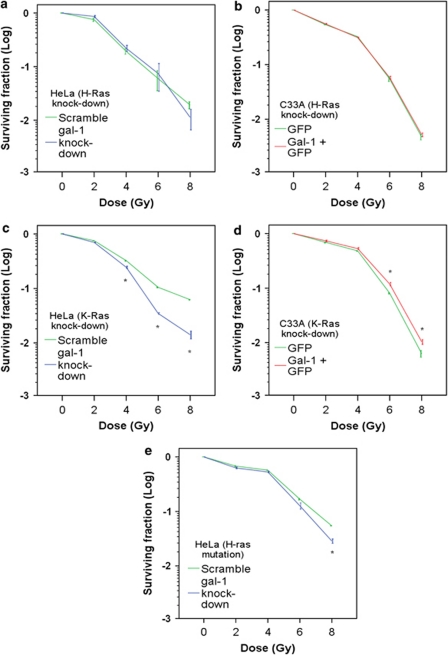
H-Ras, not K-Ras, has a significant role in galectin-1-mediated radioresistance
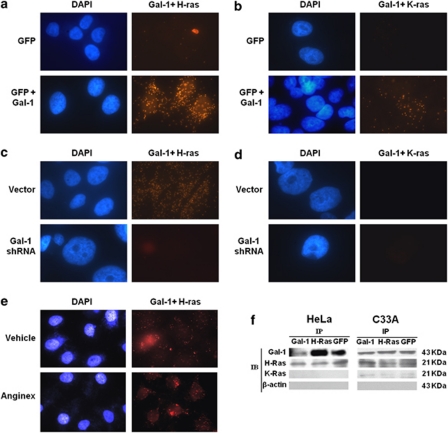
To assess whether the radioresistant effect of galectin-1 was dependent on H-Ras, this study knocked down H-Ras (Supplementary Figure S2a) to compare the survival curve in cancer cells with and without galectin-1 modulation. The galectin-1 knockdown did not further decrease clonogenic survival of HeLa cells with H-Ras knockdown (Figure 3a). Galectin-1 overexpression did not increase clonogenic survival of C33A cells with H-Ras knockdown (Figure 3b). To investigate the involvement of K-Ras in galectin-1-mediated radioresistance, this study performed the same experiment on HeLa cells and C33A cells with K-Ras knockdown (Supplementary Figure S2b). Galectin-1 knockdown significantly decreased clonogenic survival of HeLa cells, especially at high doses (Figure 3c). Galectin-1 overexpression significantly increased clonogenic survival, especially at high doses (Figure 3d). To assess whether the radioresistance effect of galectin-1 depended on activated H-Ras, we transfected constitutively active H-Ras into HeLa cells. Galectin-1 knockdown significantly decreased clonogenic survival of HeLa cells transfected with constitutively active H-Ras at high doses but not low doses (Figure 3e), defending against radiation-induced cell death in HeLa cells with gal-1 knockdown. To investigate the interaction between Ras and galectin-1, we performed immunocytochemistry using dual staining with two antibodies. Positive staining is considered protein–protein interaction. To study the interaction between H-Ras and galectin-1 in C33A cells with weak galectin-1 expression, we noted weak staining in GFP-transfected C33A cells. However, moderately enhanced dual staining was noted in galectin-1-transfected cells (Figure 4a). To study the interaction of K-Ras, we observed extremely weak staining in GFP-transfected C33A cells. However, mildly enhanced dual staining was noted in galectin-1-transfected cells (Figure 4b). Hence, the intensity of H-Ras and galectin-1 interaction was stronger than K-Ras and galectin-1 interaction in galectin-1-transfected C33A cells. In HeLa cells, the intensity of both H-Ras and galectin-1 was eliminated in shRNA-transfected cells compared with that of scrambled RNA cells (Figure 4c). No interaction between K-Ras and galectin-1 was noted in HeLa cells (Figure 4d). Anginex (Phoenix Pharmaceuticals, Inc., Burlingame, CA, USA), used for anti-angiogenesis and as a galectin-1 inhibitor, did not alter the interaction between H-Ras and galectin-1 (Figure 4e). To confirm interaction between GFP-galectin-1 and H-Ras, we performed IP on the galectin-1-overexpressing HeLa and C33A cells (Figure 4f). This study observed significant interaction between galectin-1 and H-Ras and positive immunoblotting of H-Ras during IP for GFP in both cells. No interaction between K-Ras and galectin-1 was noted in HeLa cells, whereas weak interaction between K-Ras and galectin-1 was noted in C33A cells. These findings were consistent with similar profiles of radiosensitivity between wild-type and K-Ras-knockdown HeLa cells (Figures 2a and 3c) and C33A cells (Figures 2d and 3d). Therefore, the radioresistant effect of galectin-1 is H-Ras-dependent.
Figure 3.
Galectin-1-mediated radioresistance was dependent on H-Ras but not on K-Ras. The knock down of HeLa cells by the siRNA of galectin-1 and H-Ras was confirmed by reverse transcription-polymerase chain reaction analysis and western-blot analysis in cells transfected with siRNA. Control cells were treated with scrambled RNA. The clonogenic survival curves were compared among scrambled RNA, H-Ras knockdown/scrambled RNA, and H-Ras knockdown/galectin-1 knockdown. After 48 h following transfection, cells were irradiated, and a clonogenic assay was performed 12 to 14 days after irradiation. Galectin-1 (a) knockdown or (b) overexpression did not affect the radiosensitivity of cervical cancer cells with H-Ras knockdown. However, galectin-1 (c) knockdown or (d) overexpression altered the radiosensitivity of cervical cancer cells with K-Ras knockdown. (e) Galectin-1 knockdown decreased clonogenic survival in HeLa cells transfected with mutated H-Ras at high doses but not at low doses. Clonogenic assays were performed during three independent experiments at each paired condition (with and without galectin-1 modulation). The error bar represents the standard error of mean: *P<0.05
Figure 4.
The interaction between H-Ras and galectin-1 is more intense than that between K-Ras and galectin-1 in C33A and HeLa cells. An in situ proximity ligation assay (PLA) and IP were performed for the interaction between galectin-1 and Ras. (a) PLA for galectin-1 and H-Ras in C33A cells with or without galectin-1 overexpression. (b) PLA for galectin-1 and K-Ras in C33A cells with or without galectin-1 overexpression. (c) PLA for galectin-1 and H-Ras in HeLa cells with or without galectin-1 knockdown. (d) PLA for galectin-1 and K-Ras in HeLa cells with or without galectin-1 knockdown. (e) PLA for galectin-1 and H-Ras in HeLa cells with or without the galectin-1 inhibitor anginex (10 μM), which was administered for 24 h before cell fixation. (f) IP for galectin-1 and Ras in C33A and HeLa cells transfected with GFP plus galectin-1. IP was performed for GFP, H-Ras, and galectin-1 before immunoblotting for galectin-1, H-Ras, and K-Ras in both cells
Galectin-1 enhanced H-Ras activation in cervical cancer cells following irradiation
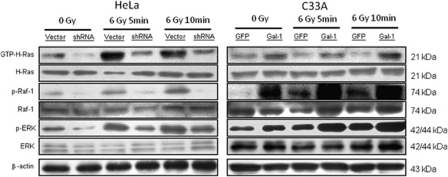
Irradiation can activate Ras and its downstream signals, such as Raf-1 and ERK. To investigate whether the phosphorylation of Raf-1 and ERK is inhibited following irradiation by the galectin-1 knockdown, we used galectin-1 shRNA compared with scrambled RNA. An increased phosphorylation of both Raf-1 and ERK was observed in HeLa cells following irradiation. The effects of phosphorylated Raf-1 and ERK induction were inhibited by the galectin-1 knockdown (Figure 5). In C33A cells, the effects of phosphorylated Raf-1 and ERK induction were enhanced by the galectin-1 overexpression (Figure 5). Thus, the effects of galectin-1 on Ras activation are through H-Ras.
Figure 5.
Effects of galectin-1 on the Ras-transmitted downstream signals. Scrambled RNA or galectin-1 shRNA were transfected in HeLa cells. GFP or galectin-1 cDNA were transfected in C33A cells. The cells were irradiated with 6 Gy and harvested 5 or 10 min later. Expressions of activated H-Ras, p-Raf-1, and p-ERK using western blots in HeLa and C33A cells were compared with or without galectin-1 modulation
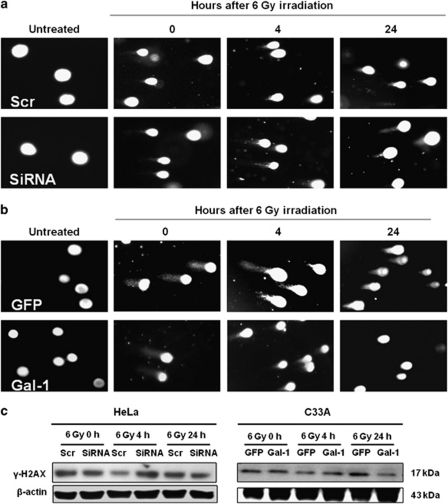
Galectin-1 enhanced DNA repair following irradiation
Because DNA repair is a significant factor of radioresistance, this study measured DNA damage in HeLa and C33A cells at various times following irradiation. Immediately following irradiation, DNA damage did not differ between the scrambled RNA and galectin-1 siRNA of HeLa cells. Similarly, no difference existed between the GFP and galectin-1 with GFP of C33A cells. However, DNA damage was severer in the galectin-1-knockdown HeLa cells than in the control 4 and 24 h following irradiation (Figure 6a). DNA damage was attenuated in the galectin-1-overexpression C33A cells than in the control 4 and 24 h following irradiation (Figure 6b). γ-H2AX is a marker of DNA damage. The expression of γ-H2AX did not differ between cancer cells with and without galectin-1 modulation, immediately following irradiation. However, after 4 h of irradiation, enhanced expressions of γ-H2AX were observed in the galectin-1-silenced HeLa cells compared with the scrambled RNA-transfected cells (Figure 6c). The expression of γ-H2AX was attenuated in the galectin-1-overexpressing C33A cells compared with the GFP-transfected cells (Figure 6c).
Figure 6.
Galectin-1 enhanced the repair of DNA damage. GFP or galectin-1 plus GFP were transfected into C33A cells. Stable clones of scrambled RNA or galectin-1 shRNA were transfected into HeLa cells. Cells were harvested immediately, 4 or 24 h following 6-Gy irradiation. Comet assay was performed. (a) A longer tail was noted in galectin-1 shRNA compared with scrambled RNA HeLa cells 24 h following irradiation. (b) A shorter tail was noted in galectin-1-overexpressed cells compared with GFP-transfected C33A cells 24 h following irradiation. (c) Western blots were performed after harvesting the cells. Greater γ-H2AX expression was noted in galectin-1-knocked down HeLa cells and GFP-transfected C33A cells 4 h and 24 h following irradiation, respectively
Discussion
This study noted a significant difference in radiosensitivity between the scrambled RNA and galectin-1 siRNA-transfected HeLa cells. However, a small difference in radiosensitivity between GFP and galectin-1 plus GFP-transfected HeLa cells was observed. This is because HeLa is rich in galectin-1 protein. Hence, the galectin-1 knockdown significantly affects the clonogenic assay. By contrast, the overexpression of galectin-1 may have a ceiling effect on the clonogenic assay. To solve this problem, we selected galectin-1-deficient C33A cells (Figure 1a). As expected, the overexpression of galectin-1 in C33A cells significantly increased clonogenic survival. Thus, this study determined that galectin-1 is involved in the radioresistance of cervical cancer cells. To the best of our knowledge, this study is the first investigation of the role of galectin-1 in radioresistance.
We are interested in the mechanism of galectin-1 involved in radioresistance. H-Ras is among the molecules associated with radioresistance20, 21 and interacts with galectin-1.22, 23 The common signaling pathways downstream of Ras are phosphoinositide 3-kinase (PI3K) and Raf-1. Elad-Sfadia et al.28 found that galectin-1 involves Ras activation and diverts Ras signals to Raf-1 at the expense of PI3K.23 Galectin-1 stabilizes GTP-bound H-Ras and enhances the activation of Raf-1 and ERK. Our results also demonstrated that galectin-1 was involved in radiation-induced H-Ras and Raf-1 and ERK activation. This study noted a weaker interaction between K-Ras and galectin-1 than between H-Ras and galectin-1, especially in HeLa cells. In addition, galectin-1-mediated radioresistance did not exist in H-Ras-silenced cells and was partially observed in K-Ras-silenced cells. The transfection of constitutively active H-Ras could rescue the radiation-induced cell death of HeLa cells with galectin-1 knockdown (Figure 3e versus Figure 2a). Additionally, radiation-induced wild-type H-Ras activation was dependent on galectin-1 (Figure 5). The radioresistant effect of galectin-1 was also wild-type H-Ras dependent. Once H-Ras is constitutively activated, the downstream signals of radioresistance may be independent from galectin-1 following low irradiation doses (Figure 3e) because the level of GTP-form H-Ras may be sufficient to alleviate radiation damage. However, at high doses, endogenous H-Ras and galectin-1 may co-operate H-Ras mutant against radiation. Therefore, galectin-1 knockdown partially affects radiosensitivity at high doses, and wild-type H-Ras may have a significant role in galectin-1-mediated radioresistance. Though Paz et al.22 was the first to discover an interaction between galectin-1 and H-Ras, we reviewed literature regarding this interaction and noted that all the studies used transformed cells instead of cancer cells. In cell lines without transformations, the expression of GTP-H-Ras is low. However, the expression of GTP-H-Ras is high in cancer cells (Figure 5). Based on the study by Paz et al.,22 galectin-1 interacts with activated H-Ras. Our study using cancer cell lines reveals that galectin-1 interacts with H-Ras more than with K-Ras (Figure 4), and also correlates to the expression of GTP-form H-Ras (Figure 5). Furthermore, this phenomenon can be observed through clonogenic assays. The radiosensitive effect of a galectin-1 knockdown (Figure 2a) is similar to that of a H-Ras knockdown in HeLa cells (Figure 3a). The survival of C33A cells (Figure 2c) that are galectin-1 deficient is inferior compared with HeLa cells (Figure 2a) that are galectin-1 rich. Both cells possess abundant H-Ras expression. The knockdown of H-Ras (Figure 3a versus Figure 2a) alters the radiosensitivity of HeLa cells, whereas the knock down of K-Ras (Figure 3c versus Figure 2a) does not. However, the knock down of both H-Ras (Figure 3b versus Figure 2d) and K-Ras (Figure 3d versus Figure 2d) does not alter the radiosensitivity of C33A cells. These data prove that H-Ras, instead of K-Ras, has a significant role in radioresistance in the presence of galectin-1. Increased GTP-H-Ras can defend against radiation-induced cell death through either constitutive active H-Ras or galectin-1 and wild-type H-Ras cooperation.
Concerns exist regarding the function of GFP and galectin-1 fusion protein. This study noted a heterodimer formation based on the IP results (Figure 1b). Because almost no endogenous galectin-1 was expressed in C33A cells (Figure 1a), we propose that a monomer of fusion protein possesses the biological function of radioresistance (Figure 2d). Overexpression of the fusion protein enhanced radioresistance (Figure 2b) regardless of the abundant endogenous galectin-1 expression in HeLa cells (Figure 1a). In addition, both the fusion protein of C33A cells (Figure 4a) and the endogenous galectin-1 of HeLa cells (Figure 4c) interacted with H-Ras. Positive immunoblotting of H-Ras (Figure 4f) was noted in both cells transfected with GFP plus galectin-1 and immunoprecipitated with GFP. Thus, fusion protein possesses a similar biological function as endogenous galectin-1. However, differing amounts of endogenous galectin-1 expression was noted between C33A and HeLa cells. Satelli et al.29 noted that galectin-1 is silenced by promoter hypermethylation in human colorectal cancer cells. None of the cancer cell lines with endogenous galectin-1 expression possessed p53 mutation, whereas 66.7% of the cancer cell lines without endogenous galectin-1 expression exhibited p53 mutation. Because p53 mutation is noted in C33A cells but not in HeLa cells, the association between p53 mutation and galectin-1 promotor hypermethylation is worth investigating.
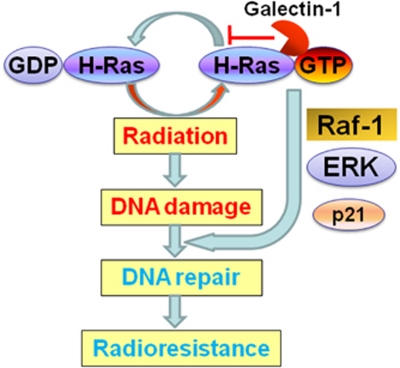
Raf-1 and ERK present an interesting issue regarding radioresistance because the shift of H-Ras transmits downstream signals to Raf-1 and ERK through galectin-1. Grana et al.30 demonstrated that the mechanism of radioresistance is related to PI3K and Raf-1, but not to ERK. In addition, a number of studies support the involvement of Raf-1 in radioresistance.31, 32 Hence, this study reasonably proposes that Raf-1 is associated with galectin-1-mediated radioresistance. Golding et al.33 noted that Raf-1 enhanced radiation-induced DNA damage repair. Ras–Raf–MAPK signals enhance cell proliferation. However, the high-intensity Raf signal induces cell cycle arrest through p21.34 The cell cycle is associated with radioresistance. A greater amount of cells in the G1 phase are expected to possess high radioresistance than cells with a lower G1 fraction.35 Hence, we expected the involvement of galectin-1 in cell cycle regulation and distribution before and after irradiation based on a number of investigations. Fischer et al.36 demonstrated that galectin-1 increased the G1 fraction of the cell cycle through the induction of p21 transcription. The comet assay and γ-H2AX expression revealed that galectin-1 enhanced the repair of DNA damage in both HeLa and C33A cells. Considered together, this study proposes (Figure 7) that galectin-1 enhances the activation of H-Ras/Raf-1. Raf-1 is involved in DNA damage repair and cell cycle arrest through p21. Radiation-induced cell death is inhibited following galectin-1-mediated H-Ras activation and the subsequent enhancement of DNA damage repair. Further studies are suggested to verify the mechanisms of H-Ras downstream signaling regarding radioresistance.
Figure 7.
A proposed model of cooperation between H-Ras and galectin-1 for radioresistance. Galectin-1 enhances activation (GTP form) of H-Ras following irradiation. Galectin-1 potentiates downstream signals of H-Ras, such as Raf-1 and ERK, that may mediate DNA damage repair33 and radioresistance.31, 32 Galectin-1 may regulate p21 expression36 through Raf-1.34 Hence, Raf-1 may have a significant role in galectin-1-mediated radioresistance
This is the first study demonstrating galectin-1 to be a radioresistant marker of cervical cancer. Whether galectin-1 is also a radioresistant marker of other cancers still requires confirmation. Tumor-bearing mice with or without modulations of galectin-1 should be investigated in further study of radiosensitivity. Dings et al.37 first noted that anginex induced radiosensitization in a murine mammary carcinoma model. However, during a clonogenic assay, anginex radiosensitized endothelial cells (ECs) but not cancer cells. In 2006, Thijssen et al.38 discovered that anginex could inhibit various effects of galectin-1, such as angiogenesis, migration, and tumor progression. They also found that anginex could be detected at the membrane of intracellular vesicles in ECs. Pilch et al.39 noted that anginex damaged the membrane of ECs but not red blood cells. This study demonstrates that anginex does not inhibit the interaction of H-Ras and galectin-1 (Figure 4e). Considered together, anginex may not translocate into cancer cells. The cell type-specific cytotoxicity of anginex may explain its anti-angiogenesis effect. Thus, different rationales of animal models for radiosensitivity using exist between the anti-angiogenesis of anginex and gene modulation of galectin-1. The mechanism of radioresistance based on the close interaction between galectin-1 and H-Ras is worth investigating. In conclusion, galectin-1 mediates the radioresistance of cervical cancer cells through H-Ras-dependent pathways. Targeting galectin-1 may be considered a radiosensitizing therapy for cancer.
Materials and Methods
Cell culture and antibodies
293T cells (CRL-11268), HeLa cells (CCL-2), and C33A (HTB-31) were purchased from the American Type Culture Collection (ATCC). Cells were grown in DMEM medium (Gibco Life Technologies, Grand Island, NY, USA) with 10% fetal bovine serum (FBS) (Gibco Life Technologies) and antibiotics (Gibco Life Technologies) at 37°C under an atmosphere of 10% CO2. The medium was changed every 3 days. Cells were passaged by 0.25% trypsin-EDTA (Gibco Life Technologies). Subconfluent cancer cells were cultured in a 25-T flask for further experiments. Antibody to galectin-1 (H-45) was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibodies to phospho-histone H2AX (Ser139), phospho-Raf-1, Raf-1, phospho-p42/44 ERK, and p42/44 ERK were purchased from Cell Signaling Technology (Beverly, MA, USA). Antibodies to â-actin, H-Ras, and K-Ras were purchased from Abcam Cambridge Science Park (Cambridge, UK). The secondary antibody (goat anti-rabbit IgG) of the detection system (alexa Fluor 568) was purchased from Invitrogen (Carlsbad, CA, USA).
Short interfering RNA (siRNA)
siRNAs (Invitrogen) were used to silence galectin-1, H-Ras, or K-Ras according to the protocol provided by the manufacturer. siRNA (7.5 μl) and Opti-MEM (250 μl) were mixed. Lipofectamine 2000 (7.5 μl) was added to the other Opti-MEM (250 μl) mixture and mixed for 5 min. The diluted siRNA and Lipofectamine were mixed for 20 min. The reagents were added into six-well plates, into which HeLa and C33A cells had been seeded (5 × 105 cells/well) for 4 h. Control cells were treated with Stealth RNAi Negative Control Duplex (Invitrogen).
Stable knockdown of galectin-1
All recombinant lentiviruses were produced by the transient transfection of 293T cells according to the manufacturer's instructions. Briefly, subconfluent 293T cells were cotransfected with 1 μg of a hairpin-pLKO.1 vector shLGALS1 (Clone ID TRCN0000057423, National RNAi Core Facility, Taipei, Taiwan), 900 ng of psPAX2, and 100 ng of pMD2.G by Lipofetamine 2000 Transfection Reagent (Invitrogen). After 16 h, the medium was changed, and the recombinant lentivirus vectors were harvested 48 h later and then filtered through 0.45 μm filters. The virus titers were calculated 72 h following virus infection by counting the number of GFP-expressing foci divided by the dilution factor. For virus infection, culture cells were incubated with the medium-diluted culture virus supernatant supplemented with polybrene (8 μg/ml) for 6 h. To achieve >95% infection efficiency, virus titers of 20 to 40 transduction unit/cells were used.
Stable transfected cell line
p or p was transfected by TrueORF destination vectors (OriGene, Rockville, MD, USA) with the Lipofetamine 2000 Transfection Reagent (Invitrogen). The C-terminal sequence encoding human Gal-1 was cloned into pCMV6-AC-GFP. To transfect HeLa or C33A cells with the plasmid vector, cells were plated into 24-well plates (2 × 105 cells per well) and allowed to adhere for 4 to 6 h. Lipofectamine 2000 (Invitrogen) was used for the transfection. After pCMV6-AC-GAL-1-GFP or pCMV6-AC-GFP transfection, the cells were cultured for 24 h. Then the medium was replaced with fresh medium supplemented with 10% FBS. G418 was used for selection; at the lowest drug concentration, G418 resulted in massive cell death after 3 days and killed all the cells within 2 weeks. Cells were diluted at a ratio of 1 : 10 into fresh growth medium 24 h after transduction; then, a selective medium with 600 to 1000 μg/ml of G418 was added to stable cell lines the next day. The transducted cells were trypsinized, collected, and resuspended for flow cytometry to determine the percentage of green fluorescent cells at 48 h following transfection.
Measurement of GFP expression using flow cytometry
We placed approximately 105 cells into a 12 × 15 mm test tube and washed them once with PBS by centrifugation for 5 min at 300 × g and 2 to 8°C. Supernatant was removed through aspiration or rapid decanting, and 500 μl of cold PBS was added to the cell pellet. Then, 500 μl of cold, buffered 2% formaldehyde solution was added. The mixture was incubated at 2 to 8°C for 1 h. The cells were spun down by centrifugation for 5 min at 300 × g and 2 to 8°C. Supernatant was removed by rapid decanting and the cells were washed once with cold PBS; then, 1 ml of 70% ethanol was added at −20°C to the cell pellet with the tube sitting on a vortex. The cell suspension was incubated overnight at 2 to 8°C; then, cells were spun down by centrifugation for 5 min at 300 × g and 2 to 8°C. Supernatant was removed by aspiration or rapid decanting, and 1 ml of a solution containing 40 μg/ml of propidium iodide (PI) and 100 μg/ml of ribonuclease A was added. The cell suspension was incubated at 37°C in dark conditions for 30 min. The samples were filtered through a nylon mesh to remove clumps before acquisition on a flow cytometer.
Stable transfection of constitutively active H-Ras in HeLa cells
Retroviral packaging 293T cells (1 × 106) were seeded in a 10-cm dish, incubated for 24 h, and then transfected by Fugene 6 (Roche, Roche Applied Science, Indianapolis, IN, USA) with 1 μg retroviral plasmids. The retroviral plasmids pBabe puro H-Ras G12 V T35S and pBABE-puro control were obtained from Addgene (Cambridge, MA, USA). After 60 h, the retrovirus-containing medium was filtered (0.45-μm filter; Acrodisc Syringe, Pall Corporation, Port Washington, NY, USA), concentrated 50-fold (from 25 ml to 500 μl), and titrated. The HeLa cells were plated at 70 to 80% confluence in a 10-cm dish at night before infection. Each infection used 100 μl of the concentrated virus (MOI 0.5) supplemented with 8 μg/ml of polybrene (Sigma-Aldrich, St. Louis, MO, USA). The infected HeLa cells were selected in media containing 2 μg/ml of puromycin for stable cell lines.
Reverse transcription-polymerase chain reaction (RT-PCR)
Total RNA was extracted from the cells using the Trizol reagent (Invitrogen) according to the manufacturer's instructions. The total RNA (1 μg) was then reverse transcribed using SuperScript III Reverse Transcriptase (Invitrogen). The RNA content was measured using 260/280 UV spectrophotometry. The following primers were used: Gal-1: forward 5′-GCATGCATGGCTTGTGGTCTGGTCGC-3′ and reverse 5′-AAGCTTTCAGTCAAAGGCCACACATTTGA-3′. H-Ras: forward 5′-ATGACGGAATATAAGCTGGTGG-3′ and reverse 5′-TCAGGAGAGCACACACTTGCAGC-3′. K-Ras: forward 5′-ACTGAATATAAACCTTGTGGTAG-3′ and reverse 5′-TCAAAGAATGGTCCTGGACC-3′. The internal control was β-actin.
Irradiation and clonogenic assay
Cells of different conditions (scrambled RNA, siRNA, overexpression, or GFP) were irradiated in 25 T flasks. For the clonogenic assay, 0, 2, 4, 6, and 8 Gy were delivered using a linear accelerator. Cells (100–10 000/well, according to the radiation dose) were plated in six-well plates immediately following irradiation. In the 1 to 2 weeks following irradiation, glutaraldehyde (6.0% v/v) and crystal violet (0.5% w/v) were added to fix and stain colonies, respectively. Cells were counted using a stereomicroscope. A colony was considered to be surviving when 50 or more cells were counted. Normalization to 0 Gy in each condition was according to the plating efficiency (PE) (Table 1). The surviving fraction equaled the number of colonies/(number of cells plated × PE). The survival curve was drawn according to the survival rate (log) and dose.
Table 1. Plating efficiency (%) of clonogenic assay.
| Cells and condition | Ras WT | H-Ras KD | K-Ras KD | H-Ras mutant |
|---|---|---|---|---|
| HeLa Scr | 75.2±2.1 | 33.7±3.2 | 29.2±1.2 | 72.4±0.8 |
| HeLa gal-1 KD | 29.1±0.8** | 22.5±7.6 | 23.5±0.8* | 59.3±3.7* |
| HeLa GFP | 71.2±0.7 | |||
| HeLa gal-1+GFP | 42.1±13.0 | |||
| C33A Scr | 73.1±1.6 | |||
| C33A gal-1 KD | 68.6±0.9* | |||
| C33A GFP | 73.1±1.6 | 34.2±1.9 | 32.3±0.2 | |
| C33A gal-1+GFP | 68.6±0.9** | 37.7±2.9 ** | 32.1±0.8 |
Abbreviations: gal-1, galectin-1; GFP, green fluorescent protein; KD, knockdown; Scr, scrambled RNA; WT, wild type.
*P<0.05; **P<0.01 versus control group
IP and western blotting
Cells (1 × 107) were lysed in RIPA buffer (150 mM NaCl, 50 mM Tris-HCl (pH 7.4), 1% NP40, 1 mM PMSF, 1 × Roche complete mini protease-inhibitor cocktail, and 1 × Pierce phosphatase-inhibitor cocktail). Co-IP was performed using the Catch and Release v2.0 Reversible Immunoprecipitation System (Millipore) according to the manufacturer's instructions. The immunoprecipitates or protein extracts (50 μg) of cells were heated at 94°C for 3 min, resolved by 10% SDS-PAGE, and electrotransferred to PVDF membranes using semi-dry transfer. The membranes were blocked for 1 h at room temperature with PBS containing 5% milk powder, then incubated with the primary antibody (diluted concentrations of galectin-1 1 : 1000, Raf-1 1 : 500, pRaf-1 1 : 1000, ERK 1 : 2000, pERK 1 : 2000, and actin 1 : 10 000), and subsequently incubated with the horseradish peroxidase-conjugated secondary antibody (diluted concentration 1 : 3000; room temperature for 45 min). Following application of the peroxidase-conjugated secondary antibodies (Santa Cruz), the blots were developed using a chemiluminescent HRP substrate (Immobilon Western, Millipore, Billerica, MA, USA) for 1 min and then transferred onto a film (Amersham Hyperfilm MP, GE healthcare, Little Chalfont, UK).
H-Ras activation assays
HeLa or C33A cells were lysed in a RIPA buffer containing 10 mM of Tris-HCl (pH 7.6), 150 mM of NaCl, 10 mM of MgCl2, 1% of Nonidet P-40, 1 mM of phenylmethylsulfonyl fluoride (PMSF), 10 μg/ml of leupeptin, and 10 U/ml of aprotinin. Lysates were centrifuged at 14 000 g for 30 min at 4°C. The resulting supernatants were incubated for 1 h at 4°C with 20 μg of Raf-1 RBD Agrose immobilized onto glutathione Sepharose beads (Cell Biolabs, San Diego, CA, USA). After incubation, the beads were collected by centrifugation for 10 s at 14 000 g and washed with 1 × Assay buffer three times. The bound proteins were then analyzed by immunoblotting using the anti-H-Ras antibody.
Comet assay
The comet assay was performed using the CometAssay kit (Trevigen Inc., Gaithersburg, MD, USA), following the manufacturer's instructions. Briefly, an aliquot of 50 μl of cells (1 × 105 cells/ml) was added to 500 μl of molten LM agarose (0.5% low-melting agarose) stored at 37°C. Upon mixing the sample, a 75-μl aliquot was pipetted onto an area of the comet slide. The slide was incubated at 4°C for 10 min to accelerate the gelling of the agarose disc and then transferred to a pre-chilled lysis solution for 10 min at 4°C. A denaturation step was performed in an alkaline solution (0.3 M NaOH, 1 mM EDTA) at room temperature (RT) and shielded from light for 5 min. The slide was then transferred to 1 × TBE (10 mM Tris (pH 7.5), 1 mM EDTA) for 5 min to neutralize before undergoing electrophoresis in a horizontal chamber in fresh 1 × TBE at 1 V/cm for 10 min. The slide was fixed in ice-cold, 70% methanol for 5 min and air dried. For observation, the samples were stained with SYBR Green (Molecular Probes, Eugene, OR, USA), diluted to 1 : 10 000 in 10 mM of Tris-HCl, pH 7.5, 1 mM EDTA, and observed using a fluorescence microscope with a 490-nm filter.
In situ proximity ligation assay (PLA)
To investigate the protein–protein interaction, this study used the Duolink reagent kit (Olink Biosciences, Uppsala, Sweden). We seeded 1 × 103 cells in 200 μl of medium into the chamber slide for culture. Cells were fixed in 1% paraformaldehyde for 15 min and washed by Wash Buffer A for 5 min twice. Cells were incubated with a blocking solution at 37°C for 30 min, and then washed with Wash Buffer A for 5 min twice. The procedures for administrating the primary antibodies (galectin-1 versus H-Ras or galectin-1 versus K-Ras), PLA probes, hybridization, ligation, amplification, detection, and mounting followed the manufacturer's recommended protocol. The cells were observed using a fluorescence microscope (Axio Observer Z1, Carl Zeiss MicroImaging, Inc., Welwyn Garden City, UK), and photographed using an integrated camera with the appropriate filter for detection.
Confocal microscopy for the distribution of GFP-galectin-1 fusion protein
To compare the distribution of transfected GFP-galectin-1 fusion protein, we used a confocal microscope to observe galectin-1 staining and GFP expression. HeLa cells with GFP-galectin-1 fusion protein transfection were fixed in 1% paraformaldehyde for 15 min and washed using PBS for 5 min twice. The cells were incubated with a galectin-1 antibody at 37°C for 30 min, and then washed using PBS for 5 min twice. The cells were also incubated with a secondary antibody at 37°C for 30 min, and then washed using PBS for 5 min twice. Finally, the cells were incubated with a DAPI for 10 min and washed using PBS for 5 min twice. After mounting, the cells were observed using a confocal microscope (VivaTome, Carl Zeiss MicroImaging, Inc.,). The procedure was performed according to the manufacturer's instructions. Red and green filters were used to observe galectin-1 and GFP, respectively.
Statistics
A comparison of the clonogenic assay of each pair was performed using a paired t-test. A P-value <0.05 was considered statistically significant. Statistical analyses were performed using Statistical Package for Social Sciences version 17.0 (SPSS, Chicago, IL, USA).
Acknowledgments
This study was partially supported by the grant for the Chang-Gung Medical Research Project (CMRPG880631-2).
Glossary
- GFP
green fluorescent protein
- IP
immunoprecipitation
- ECs
endothelial cells
- FBS
fetal bovine serum
- PI
propidium iodide
- RT-PCR
reverse transcriptase-polymerase chain reaction
- PE
plating efficiency
- PLA
in situ proximity ligation assay
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on Cell Death and Disease website (http://www.nature.com/cddis)
Edited by P Salomoni
Supplementary Material
References
- Huang EY, Wang CJ, Chen HC, Fang FM, Huang YJ, Wang CY, et al. Multivariate analysis of para-aortic lymph node recurrence after definitive radiotherapy for stage IB-IVA squamous cell carcinoma of uterine cervix. Int J Radiat Oncol Biol Phys. 2008;72:834–842. doi: 10.1016/j.ijrobp.2008.01.035. [DOI] [PubMed] [Google Scholar]
- Hertlein L, Lenhard M, Kirschenhofer A, Kahlert S, Mayr D, Burges A, et al. Cetuximab monotherapy in advanced cervical cancer: a retrospective study with five patients. Arch Gynecol Obstet. 2011;283:109–113. doi: 10.1007/s00404-010-1389-1. [DOI] [PubMed] [Google Scholar]
- Kurtz JE, Hardy-Bessard AC, Deslandres M, Lavau-Denes S, Largillier R, Roemer-Becuwe C, et al. Cetuximab, topotecan and cisplatin for the treatment of advanced cervical cancer: a phase II GINECO trial. Gynecol Oncol. 2009;113:16–20. doi: 10.1016/j.ygyno.2008.12.040. [DOI] [PubMed] [Google Scholar]
- Goncalves A, Fabbro M, Lhommé C, Gladieff L, Extra JM, Floquet A, et al. A phase II trial to evaluate gefitinib as second- or third-line treatment in patients with recurring locoregionally advanced or metastatic cervical cancer. Gynecol Oncol. 2008;108:42–46. doi: 10.1016/j.ygyno.2007.07.057. [DOI] [PubMed] [Google Scholar]
- Gaffney DK, Winter K, Dicker AP, Miller B, Eifel PJ, Ryu J, et al. A Phase II study of acute toxicity for Celebrex (celecoxib) and chemoradiation in patients with locally advanced cervical cancer: primary endpoint analysis of RTOG 0128. Int J Radiat Oncol Biol Phys. 2007;67:104–109. doi: 10.1016/j.ijrobp.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Gaffney DK, Winter K, Dicker AP, Miller B, Eifel PJ, Ryu J, et al. Efficacy and patterns of failure for locally advanced cancer of the cervix treated with celebrex (celecoxib) and chemoradiotherapy in RTOG 0128. Int J Radiat Oncol Biol Phys. 2007;69:111–117. doi: 10.1016/j.ijrobp.2007.02.050. [DOI] [PubMed] [Google Scholar]
- Herrera FG, Chan P, Doll C, Milosevic M, Oza A, Syed A, et al. A prospective phase I-II trial of the cyclooxygenase-2 inhibitor celecoxib in patients with carcinoma of the cervix with biomarker assessment of the tumor microenvironment. Int J Radiat Oncol Biol Phys. 2007;67:97–103. doi: 10.1016/j.ijrobp.2006.08.024. [DOI] [PubMed] [Google Scholar]
- van Kooyk Y, Rabinovich GA. Protein-glycan interactions in the control of innate and adaptive immune responses. Nat Immunol. 2008;9:593–601. doi: 10.1038/ni.f.203. [DOI] [PubMed] [Google Scholar]
- Le QT, Shi G, Cao H, Nelson DW, Wang Y, Chen EY, et al. Galectin-1: a link between tumor hypoxia and tumor immune privilege. J Clin Oncol. 2005;23:8932–8941. doi: 10.1200/JCO.2005.02.0206. [DOI] [PubMed] [Google Scholar]
- Le QT, Kong C, Lavori PW, O'byrne K, Erler JT, Huang X, et al. Expression and prognostic significance of a panel of tissue hypoxia markers in head-and-neck squamous cell carcinomas. Int J Radiat Oncol Biol Phys. 2007;69:167–175. doi: 10.1016/j.ijrobp.2007.01.071. [DOI] [PubMed] [Google Scholar]
- Chiang WF, Liu SY, Fang LY, Lin CN, Wu MH, Chen YC, et al. Overexpression of galectin-1 at the tumor invasion front is associated with poor prognosis in early-stage oral squamous cell carcinoma. Oral Oncol. 2008;44:325–334. doi: 10.1016/j.oraloncology.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Saussez S, Decaestecker C, Lorfevre F, Cucu DR, Mortuaire G, Chevalier D, et al. High level of galectin-1 expression is a negative prognostic predictor of recurrence in laryngeal squamous cell carcinomas. Int J Oncol. 2007;30:1109–1117. [PubMed] [Google Scholar]
- van den Brûle FA, Waltregny D, Castronovo V. Increased expression of galectin-1 in carcinoma-associated stroma predicts poor outcome in prostate carcinoma patients. J Pathol. 2001;193:80–87. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH730>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Parliament MB, Murray D. Single nucleotide polymorphisms of DNA repair genes as predictors of radioresponse. Semin Radiat Oncol. 2010;20:232–240. doi: 10.1016/j.semradonc.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Iliakis G, Metzger L, Muschel RJ, McKenna WG. Induction and repair of DNA double strand breaks in radiation-resistant cells obtained by transformation of primary rat embryo cells with the oncogenes H-ras and v-myc. Cancer Res. 1990;50:6575–6579. [PubMed] [Google Scholar]
- Cho HJ, Jeong HG, Lee JS, Woo ER, Hyun JW, Chung MH, et al. Oncogenic H-Ras enhances DNA repair through the Ras/phosphatidylinositol 3-kinase/Rac1 pathway in NIH3T3 cells. Evidence for association with reactive oxygen species. J Biol Chem. 2002;277:19358–19666. doi: 10.1074/jbc.M200933200. [DOI] [PubMed] [Google Scholar]
- Chang IY, Youn CK, Kim HB, Kim MH, Cho HJ, Yoon Y, et al. Oncogenic H-Ras up-regulates expression of Ku80 to protect cells from gamma-ray irradiation in NIH3T3 cells. Cancer Res. 2005;65:6811–6819. doi: 10.1158/0008-5472.CAN-04-4065. [DOI] [PubMed] [Google Scholar]
- Youn CK, Kim MH, Cho HJ, Kim HB, Chang IY, Chung MH, et al. Oncogenic H-Ras up-regulates expression of ERCC1 to protect cells from platinum-based anticancer agents. Cancer Res. 2004;64:4849–4857. doi: 10.1158/0008-5472.CAN-04-0348. [DOI] [PubMed] [Google Scholar]
- Sklar MD. The ras oncogenes increase the intrinsic resistance of NIH 3T3 cells to ionizing radiation. Science. 1988;239:645–647. doi: 10.1126/science.3277276. [DOI] [PubMed] [Google Scholar]
- Hermens AF, Bentvelzen PA. Influence of the H-ras oncogene on radiation responses of a rat rhabdomyosarcoma cell line. Cancer Res. 1992;52:3073–3082. [PubMed] [Google Scholar]
- Cengel KA, Voong KR, Chandrasekaran S, Maggiorella L, Brunner TB, Stanbridge E, et al. Oncogenic K-Ras signals through epidermal growth factor receptor and wild-type H-Ras to promote radiation survival in pancreatic and colorectal carcinoma cells. Neoplasia. 2007;9:341–348. doi: 10.1593/neo.06823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz A, Haklai R, Elad-Sfadia G, Ballan E, Kloog Y. Galectin-1 binds oncogenic H-Ras to mediate Ras membrane anchorage and cell transformation. Oncogene. 2001;20:7486–7493. doi: 10.1038/sj.onc.1204950. [DOI] [PubMed] [Google Scholar]
- Elad-Sfadia G, Haklai R, Ballan E, Gabius HJ, Kloog Y. Galectin-1 augments Ras activation and diverts Ras signals to Raf-1 at the expense of phosphoinositide 3-kinase. J Biol Chem. 2002;277:37169–37175. doi: 10.1074/jbc.M205698200. [DOI] [PubMed] [Google Scholar]
- Hockel M, Schlenger K, Aral B, Mitze M, Schaffer U, Vaupel P. Association between tumor hypoxia and malignant progression in advanced cancer of the uterine cervix. Cancer Res. 1996;56:4509–4515. [PubMed] [Google Scholar]
- Rofstad EK, Sundfør K, Lyng H, Tropé CG. Hypoxia-induced treatment failure in advanced squamous cell carcinoma of the uterine cervix is primarily due to hypoxia-induced radiation resistance rather than hypoxia-induced metastasis. Br J Cancer. 2000;83:354–359. doi: 10.1054/bjoc.2000.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao XY, Chen TT, Xia L, Guo M, Xu Y, Yue F, et al. Hypoxia inducible factor-1 mediates expression of galectin-1: the potential role in migration/invasion of colorectal cancer cells. Carcinogenesis. 2010;31:1367–1375. doi: 10.1093/carcin/bgq116. [DOI] [PubMed] [Google Scholar]
- Kohrenhagen N, Volker HU, Kapp M, Dietl J, Kammerer U. Increased expression of galectin-1 during the progression of cervical neoplasia. Int J Gynecol Cancer. 2006;16:2018–2022. doi: 10.1111/j.1525-1438.2006.00741.x. [DOI] [PubMed] [Google Scholar]
- Rotblat B, Belanis L, Liang H, Haklai R, Elad-Zefadia G, Hancock JF, et al. H-Ras nanocluster stability regulates the magnitude of MAPK signal output. PLoS One. 2010;5:e11991. doi: 10.1371/journal.pone.0011991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satelli A, Rao US. Galectin-1 is silenced by promoter hypermethylation and its re-expression induces apoptosis in human colorectal cancer cells. Cancer Lett. 2011;301:38–46. doi: 10.1016/j.canlet.2010.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana TM, Rusyn EV, Zhou H, Sartor CI, Cox AD. Ras mediates radioresistance through both phosphatidylinositol 3-kinase-dependent and Raf-dependent but mitogen-activated protein kinase/extracellular signal-regulated kinase kinase-independent signaling pathways. Cancer Res. 2002;62:4142–4150. [PubMed] [Google Scholar]
- Kasid U, Pfeifer A, Brennan T, Beckett M, Weichselbaum RR, Dritschilo A, et al. Effect of antisense c-raf-1 on tumorigenicity and radiation sensitivity of a human squamous carcinoma. Science. 1989;243:1354–1356. doi: 10.1126/science.2466340. [DOI] [PubMed] [Google Scholar]
- McKenna WG, Muschel RJ, Gupta AK, Hahn SM, Bernhard EJ. The RAS signal transduction pathway and its role in radiation sensitivity. Oncogene. 2003;22:5866–5875. doi: 10.1038/sj.onc.1206699. [DOI] [PubMed] [Google Scholar]
- Golding SE, Rosenberg E, Neill S, Dent P, Povirk LF, Valerie K. Extracellular signal-related kinase positively regulates ataxia telangiectasia mutated, homologous recombination repair, and the DNA damage response. Cancer Res. 2007;67:1046–1053. doi: 10.1158/0008-5472.CAN-06-2371. [DOI] [PubMed] [Google Scholar]
- Sewing A, Wiseman B, Lloyd AC, Land H. High-intensity Raf signal causes cell cycle arrest mediated by p21Cip1. Mol Cell Biol. 1997;17:5588–5597. doi: 10.1128/mcb.17.9.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodson H, Wheatley SP, Morrison CG. Involvement of centrosome amplification in radiation-induced mitotic catastrophe. Cell Cycle. 2007;6:364–370. doi: 10.4161/cc.6.3.3834. [DOI] [PubMed] [Google Scholar]
- Fischer C, Sanchez-Ruderisch H, Welzel M, Wiedenmann B, Sakai T, André S, et al. Galectin-1 interacts with the {alpha}5{beta}1 fibronectin receptor to restrict carcinoma cell growth via induction of p21 and p27. J Biol Chem. 2005;280:37266–37277. doi: 10.1074/jbc.M411580200. [DOI] [PubMed] [Google Scholar]
- Dings RP, Williams BW, Song CW, Griffioen AW, Mayo KH, Griffin RJ. Anginex synergizes with radiation therapy to inhibit tumor growth by radiosensitizing endothelial cells. Int J Cancer. 2005;115:312–319. doi: 10.1002/ijc.20850. [DOI] [PubMed] [Google Scholar]
- Thijssen VL, Postel R, Brandwijk RJ, Dings RP, Nesmelova I, Satijn S, et al. Galectin-1 is essential in tumor angiogenesis and is a target for antiangiogenesis therapy. Proc Natl Acad Sci USA. 2006;103:15975–15980. doi: 10.1073/pnas.0603883103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilch J, Franzin CM, Knowles LM, Ferrer FJ, Marassi FM, Ruoslahti E. The anti-angiogenic peptide anginex disrupts the cell membrane. J Mol Biol. 2006;356:876–885. doi: 10.1016/j.jmb.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.