Abstract
Background
It has recently become most general to use the small bore catheter to perform closed thoracostomy in treating iatrogenic pneumothorax. This study was performed for analysis of the efficacy of treatment methods by using small bore catheter such as 7 F (French) central venous catheter, 10 F trocar catheter, 12 F pigtail catheter and for analysis of the appropriateness of each procedure.
Materials and Methods
From March 2007 to February 2010, Retrospective review of 105 patients with iatrogenic pneumothorax, who underwent closed thoracostomy by using small bore catheter, was performed. We analyzed the total success rate for all procedures as well as the individual success rate for each procedure, and analyzed the cause of failure, additional treatment method for failure, influential factors of treatment outcome, and complications.
Results
The most common causes of iatrogenic pneumothorax were presented as percutaneous needle aspiration(PCNA) in 48 cases (45.7%), and central venous catheterization in 26 cases (24.8%). The mean interval to thoracostomy after the procedure was measured as 5.2 hours (1~34 hours). Total success rate of thoracostomy was 78.1%. The success rate was not significantly difference by tube type, with 7 F central venous catheter as 80%, 10 F trocar catheter as 81.6%, and 12 F pigtail catheter as 71%. Twenty one out of 23 patients that had failed with small bore catheter treatment added large bore conventional thoracostomy, and another 2 patients received surgery. The causes for treatment failure were presented as continuous air leakage in 12 cases (52.2%) and tube malfunction in 7 cases (30%). The causes for failure did not present significant differences by tube type. Statistically significant factors affecting treatment performance were not discovered.
Conclusion
Closed thoracostomy with small bore catheter proved to be effective for iatrogenic pneumothorax. The success rate was not difference for each type. However, it is important to select the appropriate catheter by considering the patient status, pneumothorax aspect, and medical personnel in the cardiothoracic surgery department of the relevant hospital.
Keywords: Pneumothorax; Iatrogenic disease; Thoracostomy; Catheter, indwelling
INTRODUCTION
Iatrogenic pneumothorax refers to the pneumothorax generated after diagnostic or treatment procedure and is a complication commonly observed at various clinical fields. Recently, the incidence of iatrogenic pneumothorax is increased with the development of invasive procedures for various diagnostic or treatment purposes [1]. Although conventional thoracostomy with large bore chest tube had been used for treating iatrogenic pneumothorax in the past, minimally invasive thoracostomy using various small bore catheters have become more common recently [2-6].
This study was performed for analysis of the treatment efficacy and outcomes of closed thoracostomy by using small bore catheter, such as 7 F central venous catheter, 10 F trocar catheter, fluoroscope guided 14 F pigtail catheter (PCD) for the patients with iatrogenic pneumothorax to evaluate the appropriateness of each procedure.
MATERIALS AND METHODS
A total of 168 patients were diagnosed and treated for iatrogenic pneumothorax from March 2007 to December 2010. In these cases, 105 patients were enrolled in this retrospective study that received closed thoracostomy procedure using small bore catheter. Patients that received conservative treatment, such as oxygen inhalation, and patients generated by barotraumas of mechanical ventilator were excluded from the research.
Pneumothorax with more than 20% of thoracic cavity and symptoms such as dyspnea, chest discomfort, subcutaneous emphysema were presented at thoracostomy indication for iatrogenic pneumothorax, and chest tube type was selected by the attending physician. 7-french central venous catheter was inserted by the physician by using the Seldinger method at bed side, while the 10-french trocar catheter was inserted in conventional thoracostomy method by the cardiothoracic surgeon. 14-french pig-tail catheter (PCD) was inserted by the diagnostic radiologist under fluoroscope guid after transferring the patient to the fluoroscope room. All tubes were drained by the underwater seal method and were maintained with low negative pressure suction of approximately -10~15 cmH2O.
The total success rate for all procedures and the individual success rate for each procedure were measured. Cases that succeeded in chest tube removal in the first procedure were regarded successful. Tube removal was performed only in situations without air-leak and after full expansion of lungs had been achieved in the chest X-ray. Also, the reason for failure of treatment, treatment method after failure, influential factors of treatment outcomes and complications were analyzed.
All analyses were carried out using statistical software (SPSS version 14.0 for Windows; SPSS, Chicago, IL, USA). Univariate analysis for comparing the continuous variables between groups was performed using independent T-tests, and comparing the categorical variables was performed with χ2 tests. Differences were considered statistically significant for p values less than 0.05.
RESULTS
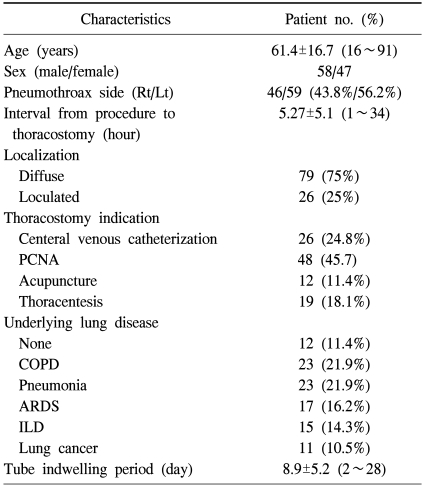
The mean age of the patients was measured as 61.4years (16~91 years), with 58 men and 47 women. Thoracostomy indication was generated after percutaneous needle aspiration (PCNA) in 48 cases (45.7%), central venous catheterization in 26 cases (24.8%), thoracentesis in 19 cases (18.1%), and acupuncture in 12 cases (11.4%). Pre-procedure underlying lung disease was presented in 93 cases (88.6%), with chronic obstructive pulmonary disease in 23 cases (21.9%) and pneumonia in 23 cases (21.9%). No differences were shown between left and right side. The mean interval to thoracostomy after the invasive procedures was 5.2 hours (1~34 hours) (Table 1).
Table 1.
Characteristics in 105 episode of iatrogenic pneumothorax
PCNA=Percutaneous needle aspiration; COPD=Chronic obstructive pulmonary disease; ARDS=Acute respiratory distress syndrome; ILD=Interstitial lung disease.
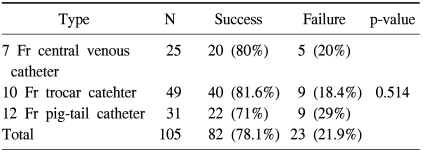
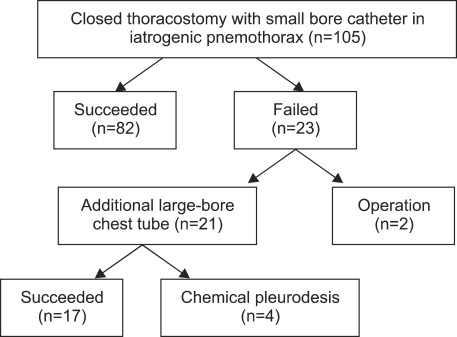
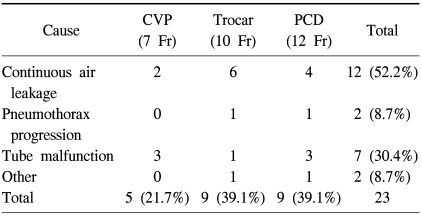
As 82 of 105 patients were treated by using small bore catheter at the first procedure, the total success rate was measured as 78.1%, and the success rate did not present significant differences for tube type (Table 2). Large bore conventional thoracostomy was added to 21 of 23 patients that did not achieve successful air reduction, and the surgery was executed to another 2 patients. 17 out of 21 patients that received additional thoracostomy with conventional large bore chest tube achieved treatment without additional procedure, while 4 patients received chemical pleurodesis due to continued air-leakage. 1 of the 2 patients that received the surgery was a patient with pneumothorax after PCNA and had received surgery for lung cancer diagnosed during drainage. The other patient received emergency surgery for hemopneumothorax (Fig. 1). All of the surgery was performed by VATS. None of the patients had received surgery for continued air-leakage in iatrogenic pneumothorax. The causes of treatment failure were presented as continuous air leakage in 12 cases (52.2%) and tube malfunction in 7 cases (30%). Causes for treatment failure did not present differences for each tube type (Table 3).
Table 2.
Comprasion of success rate according to tube type
Fig. 1.
Flow chart represent the treatment outcomes in 105 episode of iatrogenic pneumothorax.
Table 3.
Cause of treatment failure
CVP=Central venous pressure; PCD=Percutaneous drainage (pig-tail catheter).
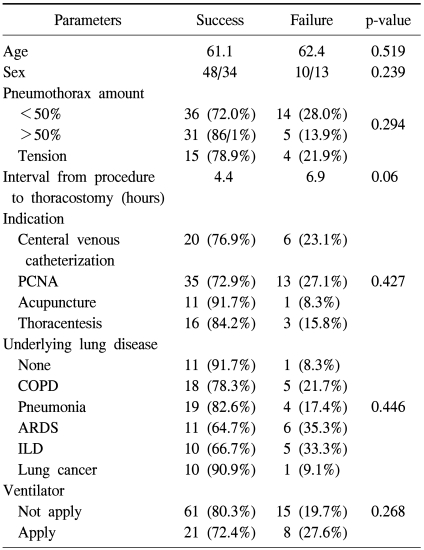
According to analysis on influential factors of treatment outcomes, it was presented that success rate was not affected by age, sex, pneumothorax amount, thoracostomy indication, underlying lung disease, or ventilator apply. Although success rate tended to be decreased with longer interval from procedure to thoracostomy, it did not show statistical significance (Table 4).
Table 4.
Comparasion of successful and failed thoracostomy in 105 episode of iatrogenic pneumothorax
PCNA=Percutaneous needle aspiration; COPD=Chronic obstructive pulmonary disease; ARDS=Acute respiratory distress syndrome; ILD=Interstitial lung disease.
The mean tube indwelling period was measured as 8.9 days (2~28 days). Complications were generated in 3 cases (2.9%), which were chest tube site infection in all.
DISCUSSION
The use of small bore catheter for pneumothorax treatment was first reported by Sargent and Turner in 1970 regarding the use of 9-french Teflon catheter based on Trocar technique in 20 iatrogenic pneumothorax patients after percutaneous needle aspiration [3]. Afterward, 5.5~16 French catheter was used in iatrogenic pneumothorax to present 80~95% success rate [7-9]. The initial treatment of pneumothorax based on use of small bore catheter is reported as the most recent trend. Small bore chest tubes of various types and are used not only in iatrogenic pneumothorax but also in spontaneous pneumothorax to report results comparable to the treatment based on the use of conventional large bore chest tube, such as more than 20-french. Ryu et al. [6] presented 77% treatment success rate for primary spontaneous pneumothorax using 7-french catheter commonly used in central venous catheterization, while Park et al. [10] reported that the use of 8-french catheter (Pleuracan®, B. Braun, Melsungen, Germany) in primary spontaneous pneumothorax patients do not present differences in clinical efficacy when compared with large bore chest tube thoracostomy and is rather more comfortable for patients as the use of intravenous analgesics is reduced. Liu et al. [11] reported that the insertion of fluoroscope-guided pigtail tube in spontaneous pneumothorax treatment did not present differences in tube indwelling period, air-reduction rate, hospital stay when compared with conventional conventional thoracostomy and also decreased restrictions in activity and presented less complications when compared with large bore tube. The mean success rate of this study was analyzed as 78.1% and did not show differences with most other reports. Differences were not presented in success rate between use of 7-french, 10-french, 12-french small bore catheters.
The advantages of using small bore catheter include convenient procedure, lower possibility of complications which can be generated by invasive procedure, less pain and fear experienced by patients from procedure, and less scar after procedure. Each small bore catheter had individual advantages and disadvantages. The procedure can be easy to perform in use of 7-french catheter as insertion is achieved by using the seldinger technique. On the other hand, line kinking may be generated to cause tube malfunction in the use of 7-french catheter [5,6]. The 10-french thoracic catheter insertion using trocar technique is a procedure that can overcome such disadvantage of 7-french catheter. This method facilitates bed side procedure and presents little tube malfunction. However, lung damage may be exerted on patients with severe adhesion and thus require careful manipulation [10]. We experienced this complication on one patient during the research period. As a solution, large bore thoracostomy was added and chemical pleurodesis was conducted on this patient. As the fluoroscope-guided pigtail catheter insertion achieves treatment in the accurate space, it is advantageous in that it can be easily applied in pneumothorax loculated in locations that are difficult to access or in areas with adhesion. On the other hand, a skilled diagnostic radiology doctor is required and patients experience greater anxiety as they must be transferred to the fluoroscope room due to difficulties in achieving bed side treatment.
Before March 2007, treatment protocol for iatrogenic pneumothorax of our hospital was achieved by conducting conventional thoracoscomy by using 20~28 french chest tube. Afterward, thoracostomy using small bore catheter was performed for initial treatment. Currently, 10-french thoracic catheter insertion is preferentially considered for the initial treatment protocol of iatrogenic pneumothorax. If immediate treatment is required for patients with serious symptoms or if the cardiothoracic surgeon is absent in place, the attending doctor is responsible for performing 7-french central venous catheter insertion. 12-french pigtail catheter is executed by the diagnostic department for loculated pneumothorax.
To increase the success rate of treatment, chest X-rays must be used to check the existence of pneumothorax after performing procedures that present possible occurrence of iatrogenic pneumothorax. If the patient presents dyspnea, chest discomfort, or subcutaneous emphysema after procedure, chest X-rays must be immediately inspected. In this study, the success rate tended to be decreased with longer interval from procedure to thoracostomy, but it did not show statistical significance.
CONCLUSION
Thoracostomy with small bore catheter proved to be effective for iatrogenic pneumothorax. Difference in success rate was not presented by type. However, appropriate catheter must be selected by considering patient condition, pneumothorax aspect, and availability of medical personnel of cardiothoracic surgery department in the relevant hospital.
References
- 1.Khan MF, Straub R, Moghaddam SR, et al. Variables affecting the risk of pneumothorax and intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur Radiol. 2008;18:1356–1363. doi: 10.1007/s00330-008-0893-1. [DOI] [PubMed] [Google Scholar]
- 2.Henry M, Arnold T, Harvey J Pleural Diseases Group; Standards of Care Committee; British Thoracic Society. BTS guidelines for the management of spontaneous pneumothorax. Thorax. 2003;58(Suppl 2):ii39–ii52. doi: 10.1136/thorax.58.suppl_2.ii39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sargent EN, Turner AF. Emergency treatment of pneumothorax. A simple catheter technique for use in the radiology department. Am J Roentgenol Radium Ther Nucl Med. 1970;109:531–535. [PubMed] [Google Scholar]
- 4.Lin YC, Tu CY, Liang SJ, et al. Pigtail catheter for the management of pneumothorax in mechanically ventilated patients. Am J Emerg Med. 2010;28:466–471. doi: 10.1016/j.ajem.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 5.Cho S, Lee EB. Management of primary and secondary pneumothorax using a small-bore thoracic catheter. Interact Cardiovasc Thorac Surg. 2010;11:146–149. doi: 10.1510/icvts.2009.226589. [DOI] [PubMed] [Google Scholar]
- 6.Ryu KM, Jung ES, Cho SK, Sung SW, Jheon S. Clinical efficacy of 7-French catheter for initial treatment of primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg. 2006;39:394–398. [Google Scholar]
- 7.Crouch JD, Keagy BA, Delany DJ. "Pigtail" catheter drainage in thoracic surgery. Am Rev Respir Dis. 1987;136:174–175. doi: 10.1164/ajrccm/136.1.174. [DOI] [PubMed] [Google Scholar]
- 8.Conces DJ, Jr, Tarver RD, Gray WC, Pearcy EA. Treatment of pneumothoraces utilizing small caliber chest tubes. Chest. 1988;94:55–57. doi: 10.1378/chest.94.1.55. [DOI] [PubMed] [Google Scholar]
- 9.Light RW. Management of spontaneous pneumothorax. Am Rev Respir Dis. 1993;148:245–248. doi: 10.1164/ajrccm/148.1.245. [DOI] [PubMed] [Google Scholar]
- 10.Park JS, Lee JI, Hwang YJ, et al. Treatment of primary spontaneous pneumothorax using a commercialized 8-French catheter (Pleuracan(R)) Korean J Thorac Cardiovasc Surg. 2007;40:292–296. [Google Scholar]
- 11.Liu CM, Hang LW, Chen WK, Hsia TC, Hsu WH. Pigtail tube drainage in the treatment of spontaneous pneumothorax. Am J Emerg Med. 2003;21:241–244. doi: 10.1016/s0735-6757(02)42247-4. [DOI] [PubMed] [Google Scholar]