Abstract
Youth onset type 2 diabetes (T2DM) continues to increase worldwide, concomitant with the rising obesity epidemic. There is evidence to suggest that youth with T2DM are affected by the same comorbidities and complications as adults diagnosed with T2DM. This review highlights specifically the kidney disease associated with youth onset T2DM, which is highly prevalent and associated with a high risk of end-stage kidney disease in early adulthood. A general understanding of this complex disease by primary care providers is critical, so that at-risk individuals are identified and managed early in the course of their disease, such that progression can be modified in this high-risk group of children and adolescents. A review of the pediatric literature will include a focus on the epidemiology, risk factors, pathology, screening, and treatment of kidney disease in youth onset T2DM.
1. Epidemiology of Youth Onset Type 2 Diabetes
Type 2 diabetes (T2DM) has been described in children and adolescents since the 1980s [1], and coincident with the rising obesity epidemic, the incidence and prevalence have continued to rise over the last thirty years [2, 3]. Youth onset T2DM has now been described around the world, including Canada, Japan, India, Australia, the United States (US), and the United Kingdom (UK) [4–9]. The highest rates have been reported in the Pima Indian population in the US, with a prevalence of 1.4% in boys and 2.88% in girls between 10 and 14 years [10]. In Canadian First Nation children 4–19 years of age, the prevalence has been reported to be as high as 1% in some communities [11]. In most other populations, although rates are increasing, the disease remains comparably rare. In the US, for example, the incidence in 10–14 years old is 8.1/100,000 person years, and 11.8 per 100,000 person years in children 15–19 years [12]. In Canada, a recent active surveillance initiative revealed a minimum incidence rate of T2DM in children less than 18 years of 1.54 per 100,000 per year. The highest rate was seen in the province of Manitoba, with a minimum incidence rate of 12.45 per 100,000 children [13]. The lowest rates have been reported in the UK at 0.53 per 100,000 in less than 17 year olds [14].
In addition to obesity, multiple other risk factors for the development of youth onset T2DM have been identified. Firstly, most affected children belong to minority ethnic groups including Canadian First Nation, American Indian, Hispanic, African-American, and Indo-Asian [6]. T2DM represents only 6% of non-Hispanic white children in the US with diabetes [15] but accounts for 46.1% of newly diagnosed Hispanics, 57.8% of non-Hispanic blacks, 69.7% of Asian Pacific Islanders, and 86.2% of American Indians with youth onset diabetes [12].
A strong family history is almost universal, with 45–80% of children with T2DM having at least one parent and 70–100% having a first or second-degree relative affected with the disease [16, 17]. The intrauterine environment has also been shown to be important. Children at the lowest and highest extremes of birth weight are at increased risk [18], as are those exposed to pregestational or gestational diabetes in utero [19, 20]. In contrast, breastfeeding has been shown to be protective [19, 20]. Finally, specific genetic factors may play an important role. For example, a unique hepatic nuclear factor- (HNF-)1α is a transcription factor expressed in many tissues including the liver, intestine, pancreatic β-cell, and kidney. A polymorphism of this gene (HNF-1α G319S) has been identified in the Oji-Cree language group of First Nation people in Manitoba and northwestern Ontario. It is associated with an insulin-secretory defect, which predisposes to early onset T2DM in this population [21, 22].
2. Nephropathy Associated with Type 2 Diabetes
In adults, T2DM is the leading cause of end-stage kidney disease (ESKD) accounting for 30–40% of cases in most countries. ESKD secondary to diabetic nephropathy typically manifests after 20 to 30 years of diabetes exposure [23]. In children and adolescents, diabetes accounts for only 0.1% of ESKD [24]. However, there is mounting evidence to suggest that renal complications in youth onset T2DM manifest themselves early in the course of disease, and that progression parallels that seen in adult onset T2DM [25]. As youth onset T2DM has only been described for twenty years, we are just now starting to see the impact of the renal complications associated with this devastating disease, as the first cohort of youth enter their third decade.
Microalbuminuria is the first manifestation of a renal complication of diabetes and is the most commonly reported complication of T2DM in youth [26–30]. Reported rates vary widely between 7 and 22% at presentation [27, 28, 31] and between 9.6 and 72% within 3–10 years after diagnosis [26–32]. Variation in rates depends mainly on the definition of albuminuria utilized in each study. Most studies report albuminuria in one random urine sample, which overestimates the prevalence of pathologic albuminuria, as urinary albumin excretion can be transient. Studies that have utilized more stringent criteria (2 out of 3 abnormal samples over a 3–6 month period) report more conservative rates, such as the TODAY study cohort, which reported a prevalence of albuminuria of 13% at a mean age of 14 years, and mean diabetes duration of 7.8 months [33]. This cohort had an average hemoglobin A1c (HbA1c) of 5.9% at enrollment and is therefore likely a low-risk group. In contrast, rates of microalbuminuria in a Manitoba, Canada, cohort with an average HbA1c of 8.9%, based on at least 2 abnormal samples, are much higher at 26.9%, at a mean age of 16.5 years and mean duration of diabetes of 3 years [34]. There has yet to be a study in youth that has reported rates of persistent albuminuria confirmed with a first morning urine sample or overnight urine collection, which are considered the gold standard tests. Nevertheless, these high rates in adolescence are concerning, as microalbuminuria is predictive of progressive diabetic nephropathy, declining glomerular filtration rate (GFR), and cardiovascular disease [35–38].
In the Pima Indian population of the US, there is a 5-fold increased risk of age-specific ESKD in those diagnosed with diabetes before the age of 20 compared to those with diabetes onset between 25 and 54 years of age [39]. However, after controlling for confounders, age at onset was no longer associated with an increased incidence of ESKD, suggesting that the longer duration of diabetes accounted for the increased risk in middle age. These results are in keeping with a previous study by Krakoff et al. which directly compared youth with T2DM <20 years at diagnosis versus young adults 20–39 years versus older adults >40 years at diagnosis which did not show a difference in risk of nephropathy over 25 years between groups [25]. What remains especially concerning, however, is the young age at which youth with T2DM will reach ESKD, requiring dialysis or kidney transplant to sustain life. In Manitoba, ESKD has previously been reported to occur prior to the age of 30 years in young adults diagnosed with T2DM prior 18 years [40]. The same cohort has also recently been shown to have a 4-fold increased risk of ESKD compared to youth with type 1 diabetes (T1DM). In addition, the renal survival fifteen years after diagnosis is 92%, and only 55% in those individuals with 20 years of followup [34]. A higher incidence of nephropathy in young adults with T2DM compared to those with T1DM has also been reported in the Japanese population [41]. A subgroup of this population with proliferative retinopathy prior to age 35 was associated with diabetic nephropathy in 60% and renal failure in 23%, with a requirement for renal replacement therapy at 35 years of age [42].
3. Risk Factors for Progression
Kim et al. followed youth with T2DM longitudinally for a median of 3 years, and microalbuminuria identified on one initial urine assessment remained persistent in >93% of youth less than 20 years of age [45]. This study also demonstrated that microalbuminuria in adolescents with T2DM is a predictor of progression to macroalbuminuria over a median followup of 8.1 years [45]. Albuminuria detected in adolescence has also been associated with a 4-fold increased risk of renal failure in early adulthood [34]. Microalbuminuria can therefore be considered a harbinger of renal injury in youth with T2DM, consistent with adult onset T2DM.
The adult literature has identified clinical risk factors associated with the development of diabetic nephropathy. There may also be a genetic predisposition, as has been shown in the Pima Indians in the US [46] as well as in Caucasians [47]. A study of 191 normoalbuminuric adults with T2DM followed prospectively for 5 years described a risk of microalbuminuria of 5% per year and identified male sex, older age, baseline albuminuria, HbA1c, cholesterol, and presence of retinopathy as risk factors [48]. In addition, glomerular hyperfiltration (i.e., increased GFR) has been well described in adults with T2DM, hypothesized to be secondary to concomitant obesity and hyperglycemia. The GFR has been shown to progressively increase and reach a plateau once microalbuminuria develops. Once progression to macroalbuminuria occurs, the GFR begins to decline [49]. It is, however, not consistent in the literature that hyperfiltration is pathogenic, as some studies have shown no association between hyperfiltration and decreased GFR [49].
The Diabetes Control and Complications Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS) have shown that the intensity of glycemic control significantly impacts the development of diabetic nephropathy in T1DM and adult onset T2DM [50–52]. The pediatric literature is scant but available data suggests that glycemic control is also an important risk factor in youth with T2DM [30, 53]. However, the ideal target for HbA1c to minimize the risk of nephropathy in youth with T2DM has not yet been determined. The clinical practice guidelines currently extrapolate from adult data to target an HbA1c ≤7% [54]. Unfortunately, this target HbA1c is difficult to achieve in youth, due in part to adolescent behavior and nonadherence to treatment recommendations.
Youth with type 2 diabetes have a high prevalence of co-morbidities such as obesity, hypertension, and dyslipidemia [55, 56]. The role of these potentially modifiable clinical risk factors in the development of diabetic nephropathy has not yet been clearly defined in youth onset T2DM. Obesity is associated with glomerular hyperfiltration and the development of glomerulosclerosis and kidney failure [57, 58]. Renal hyperfiltration and hypertrophy may develop in the setting of T2DM in response to disproportionate weight gain and declining insulin sensitivity [59]. According to this hypothesis, adolescents with T2DM may be particularly at risk for premature renal injury relative to adults who experience more gradual weight gain and insulin resistance in adulthood.
Hypertension is highly prevalent in youth with T2DM, with a reported prevalence between 10 and 73% at diagnosis [28, 55, 60–64]. In contrast to the T1DM and adult onset T2DM literature [65], which consistently demonstrates hypertension to be an important modifiable risk factor for the development and progression of diabetic nephropathy, the association between blood pressure control and microalbuminuria in adolescents with T2DM is inconsistent [32, 45, 53]. A small case-control study (n = 23) revealed that daytime systolic blood pressure was ~8 mmHg higher among youth with T2DM, relative to normoalbuminuric controls [32]. In contrast, multivariate regression analyses from a larger cross-sectional study and a prospective cohort study demonstrated that systolic blood pressure is not associated with microalbuminuria in adolescents and young adults with T2DM [30, 31, 53]. These different findings may be explained by differences in measurement techniques (casual clinic-based measures versus 24 hr blood pressure monitoring), underpowered studies, or a lack of prospective studies with adequate followup.
Dyslipidemia is a frequent finding in youth with T2DM [27, 28, 31, 55, 62, 64, 66–68]. Two small studies have shown increased LDL cholesterol and triglyceride levels in youth with T2DM and microalbuminuria compared with those with normal albumin excretion [30, 32], suggesting that modification of dyslipidemia may affect risk of nephropathy.
Smoking is reported in 7–48% of youth with diabetes [69, 70]. In T1DM, smoking has been shown to increase the risk of microalbuminuria [71]. In addition, smoking is also associated with a reduced GFR in adults with T1DM and T2DM even after controlling for multiple confounders, including microalbuminuria [72]. Strategies to help with smoking cessation are therefore very important for these high-risk youth.
4. Pathology
Classic diabetic nephropathy is characterized by glomerular hypertrophy, basement membrane (GBM) thickening, and mesangial matrix expansion [73]. There is very little biopsy data available on youth with T2DM. In a cohort of ten Canadian First Nation youth with T2DM and macroalbuminuria who underwent renal biopsy, nine of ten biopsies exhibited immune complex disease or glomerulosclerosis, and none had classic diabetic nephropathy [74]. This may in part be due to the high burden of nondiabetic primary renal disease in Canadian First Nation populations [75–77]. Adults with T2DM have also been shown to have nondiabetic glomerular disease, either superimposed on diabetic nephropathy (17%) or more commonly without underlying diabetic disease (28%) [78]. Concomitant obesity is also associated with focal glomerulosclerosis and renal failure [57, 58]. Therefore, there may be early changes seen in youth with T2DM related to nondiabetic kidney disease, and obesity. The additive effects of diabetes and its associated comorbidities may alter progression of renal dysfunction over time.
5. Screening
Canadian, American, and International guidelines [15, 54, 79] all recommend screening for diabetic nephropathy at first presentation of diabetes. There are no validated definitions for albuminuria in youth, therefore, the adult values are currently utilized to stage patients (Table 1).
Table 1.
Definitions for albuminuria* [43].
| Albumin : Creatinine ratio (mg/mmol) [43]¶ | 24 hour collection for albumin excretion (mg/day) | |
|---|---|---|
| Normal | <2.0 (boys) | <30 |
| <2.8 (girls) | ||
|
| ||
| Microalbuminuria | 2.0–20.0 (boys) | 30–300 |
| 2.8–28.0 (girls) | ||
|
| ||
| Macroalbuminuria | >20.0 (boys) | >300 |
| >28.0 (girls) | ||
¶Must be confirmed with either first morning urine sample or overnight urine collection.
*Persistent albuminuria defined as 2/3 positive samples over a 3–6 month period, samples must be at least 1 month apart.
Albumin excretion rates in adolescents are influenced by several factors including orthostatic changes, fever, infection, and physical activity. Therefore, it is necessary to have at least 2 positive samples over 3 to 6 months, separated by at least 1 month to confirm the diagnosis [43]. In addition, the diagnosis in youth should be confirmed with a first-morning urine sample or overnight urine collection, to rule or orthostatic proteinuria [80]. An algorithm for screening and treatment has been proposed (Figure 1).
Figure 1.
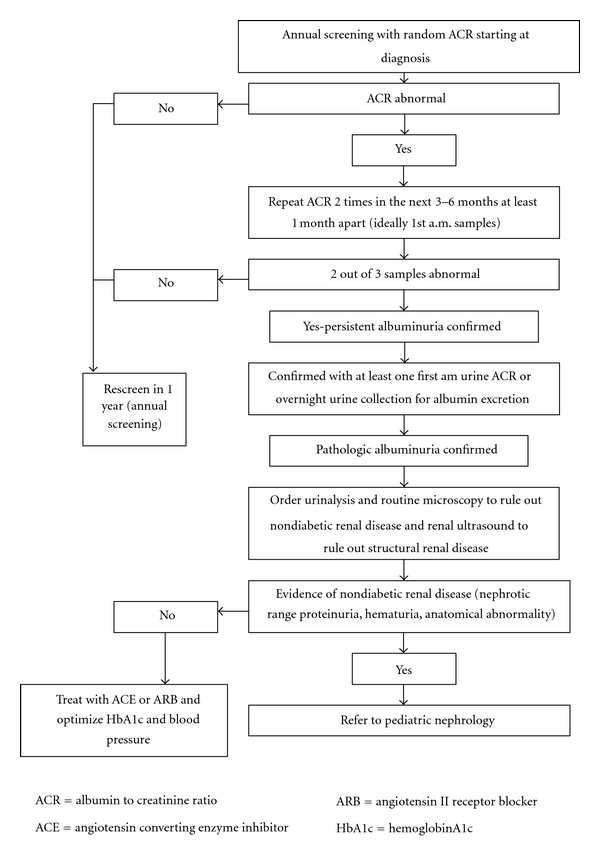
Screening algorithm for albuminuria in youth with type 2 diabetes (modified from CDA guidelines) [43].
In addition to screening for albuminuria, screening for concomitant comorbidities (dyslipidemia, hypertension, and smoking) is also recommended [54, 79, 81]. An assessment of renal function should also be considered in the form of an estimated glomerular filtration rate [43, 82]. A urinalysis and a renal ultrasound should be performed. The presence of hematuria or red blood cell casts raises the possibility that a nondiabetic kidney disease could be present. In those cases, a glomerulonephritis workup should be initiated, and a renal biopsy considered. In the event of macroalbuminuria, evidence of nondiabetic kidney disease, or an atypical course, a referral to a pediatric nephrologist is recommended.
6. Treatment of Nephropathy and Associated Comorbidities (Table 2)
Table 2.
Recommended treatment targets that may reduce risk of nephropathy in youth with type 2 diabetes.
| Clinical parameter | Intervention | Treatment target |
|---|---|---|
| Glycemic control | Lifestyle/Insulin/Metformin | HbA1c ≤ 7% |
| Prehypertension [44] (bp > 90th–95th) | Lifestyle | Bp < 90th percentile |
| Hypertension [44] (bp > 95th percentile) | Lifestyle ± Ace inhibitor or Angiotensin II Receptor Blocker | Bp < 90th percentile |
| Dyslipidemia LDL ≥2.6 mmol/L | Lifestyle | LDL < 2.6 mmol/L |
| Dyslipidemia LDL >4.1 mmol/L | Lifestyle + Statin | LDL < 2.6 mmol/L |
| Overweight and Obesity | Lifestyle | BMI < 85th percentile |
| Smoking | Cessation strategies | Nonsmoker |
First line in the prevention and treatment of nephropathy associated with T2DM is lifestyle modification and behavior change, including weight reduction, low-sodium diet, and exercise [17] in order to optimize glycemic control and reduce comorbidities such as obesity, hypertension, and hypercholesterolemia. Smoking cessation strategies should be implemented. Unfortunately, this type of therapy requires significant buy in from patients, families, and health care providers. This patient population is particularly challenging to treat due to their adolescent age, as well as the very high rates of lower socioeconomic status (SES). In the TODAY study, 41.5% of participants had a household income <$25,000 [33], and in Manitoba 59.1% of youth with T2DM are in the lowest SES quintile [34]. If lifestyle modification is not sufficient to reduce and maintain HbA1c to <9% (target HbA1c is ≤7%), then pharmacologic management is indicated, in the form of insulin and/or metformin [17, 54, 81], which is the only oral hypoglycemic agent that has been approved (in 2000) by the US Food and Drug Administration [83, 84].
In the absence of concrete blood pressure data in children with diabetes, the current guidelines recommend targeting normal blood pressures in children with T2DM (<90th percentile for age and height, or a maximum of <130/80), [17, 44] not only to potentially reduce the risk of renal injury, but to decrease the risk of cardiovascular disease [17, 54, 81]. Angiotensin II receptor blockers (ARBs) have been used most often in studies of adult onset T2DM and have been shown to consistently reduce the rate of progression from microalbuminuria to macroalbuminura [85–87]. Angiotensin-converting enzyme (ACE) inhibitors have also been evaluated and been shown to decrease the risk of microalbuminuria in normoalbuminuric patients with T2DM [88]. No studies have evaluated these drugs in youth with T2DM. There is a small number of nonrandomized studies in youth with T1DM, all of which have shown reductions in albuminuria with ACE inhibitors [89–91]. Treatment with an ACE or ARB is therefore considered first-line therapy for both hypertension and microalbuminuria in youth with T2DM [17, 81]. If treatment targets are not achieved with one medication, then it is recommended that a second agent be added [17]. Female patients must be advised that congenital malformations, even in the first trimester, have been reported with ACE and ARB use [92]. Contraception counseling is thus very important when these drugs are being used.
Treatment of hyperlipidemia is more controversial. Lifestyle modification is considered first-line therapy, and improvement in glycemic control often results in improved lipid levels. If lifestyle fails, then pharmacologic management with HMG CoA reductase inhibitors is recommended. The Canadian Diabetes Association currently recommends targets used for familial hyperlipidemia for initiation of pharmacologic agents, as studies done in this particular group have not yet been done. A low-density lipoprotein (LDL) threshold value >4.1 mmol/L is utilized to initiate pharmacologic management if there is a family history of early cardiovascular events or ≥4.9 mmol/L in the absence of cardiovascular events [54, 93]. In contrast, the International Society for Pediatric and Adolescent Diabetes recommends a stricter target of <2.6 mmol/L, based on adult data [94].
7. Conclusions
The prevalence of type 2 diabetes in youth continues to increase and is associated with microalbuminuria early in the course of disease. The rate of progression to ESKD is in keeping with adult onset disease. Poor metabolic control and co-morbidities such as hypertension, dyslipidemia, and smoking are highly prevalent and likely hasten the progression of diabetic nephropathy and chronic kidney disease. Multifactorial-based prevention and treatment approaches focusing on lifestyle modification and incorporating pharmacologic management of hyperglycemia, hypertension, and albuminuria have been proven in adult studies. Similar strategies are also likely important to delay progression to ESKD in youth with T2DM, however, more research is required to better define the natural history of diabetic nephropathy and optimal treatment targets and therapies in this high-risk population.
References
- 1.Dean H, Moffatt ME. Prevalence of diabetes mellitus among Indian children in Manitoba. Arctic Medical Research. 1988;47:532–534. [PubMed] [Google Scholar]
- 2.Harron KL, Feltbower RG, McKinney PA, Bodansky HJ, Campbell FM, Parslow RC. Rising rates of all types of diabetes in south Asian and non-south Asian children and young people aged 0–29 years in West Yorkshire, U.K., 1991–2006. Diabetes Care. 2011;34(3):652–654. doi: 10.2337/dc10-1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tulloch-Reid MK, Boyne MS, Smikle MF, et al. Clinical and laboratory features of youth onset type 2 diabetes in Jamaica. The West Indian Medical Journal. 2010;59(2):131–138. [PubMed] [Google Scholar]
- 4.Dean H. Type 2 diabetes in youth: a new epidemic. Advances in Experimental Medicine and Biology. 2001;498:1–5. doi: 10.1007/978-1-4615-1321-6_1. [DOI] [PubMed] [Google Scholar]
- 5.Kitagawa T, Owada M, Urakami T, Yamauchi K. Increased incidence of non-insulin dependent diabetes mellitus among Japanese schoolchildren correlates with an increased intake of animal protein and fat. Clinical Pediatrics. 1998;37(2):111–115. doi: 10.1177/000992289803700208. [DOI] [PubMed] [Google Scholar]
- 6.Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. Journal of Pediatrics. 2000;136(5):664–672. doi: 10.1067/mpd.2000.105141. [DOI] [PubMed] [Google Scholar]
- 7.Drake AJ, Smith A, Betts PR, Crowne EC, Shield JPH. Type 2 diabetes in obese white children. Archives of Disease in Childhood. 2002;86(3):207–208. doi: 10.1136/adc.86.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Type 2 diabetes in Asian-Indian urban children. Diabetes Care. 2003;26(4):1022–1025. doi: 10.2337/diacare.26.4.1022. [DOI] [PubMed] [Google Scholar]
- 9.Braun B, Zimmermann MB, Kretchmer N, Spargo RM, Smith RM, Gracey M. Risk factors for diabetes and cardiovascular disease in young Australian aborigines: a 5-year follow-up study. Diabetes Care. 1996;19(5):472–479. doi: 10.2337/diacare.19.5.472. [DOI] [PubMed] [Google Scholar]
- 10.Knowler WC, Pettitt DJ, Savage PJ, Bennett PH. Diabetes incidence in Pima Indians: contributions of obesity and parental diabetes. American Journal of Epidemiology. 1981;113(2):144–156. doi: 10.1093/oxfordjournals.aje.a113079. [DOI] [PubMed] [Google Scholar]
- 11.Dean HJ, Young TK, Flett B, Wood-Steiman P. Screening for type-2 diabetes in aboriginal children in northern Canada. The Lancet. 1998;352(9139):1523–1524. doi: 10.1016/S0140-6736(05)60329-7. [DOI] [PubMed] [Google Scholar]
- 12.Dabelea D, Bell RA, D'Agostino RB, Jr., et al. Incidence of diabetes in youth in the United States. Journal of the American Medical Association. 2007;297(24):2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 13.Amed S, Dean HJ, Panagiotopoulos C, et al. Type 2 diabetes, medication-induced diabetes, and monogenic diabetes in Canadian children: a prospective national surveillance study. Diabetes Care. 2010;33(4):786–791. doi: 10.2337/dc09-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haines L, Wan KC, Lynn R, Barrett TG, Shield JPH. Rising incidence of type 2 diabetes in children in the U.K. Diabetes Care. 2007;30(5):1097–1101. doi: 10.2337/dc06-1813. [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2008;31(supplement 1):S12–S54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 16.Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. The New England Journal of Medicine. 2002;346(11):802–810. doi: 10.1056/NEJMoa012578. [DOI] [PubMed] [Google Scholar]
- 17.Type 2 diabetes in children and adolescents. American Diabetes Association. Diabetes Care. 2000;23(3):381–389. doi: 10.2337/diacare.23.3.381. [DOI] [PubMed] [Google Scholar]
- 18.Wei JN, Sung FC, Li CY, et al. Low birth weight and high birth weight infants are both at an increased risk to have type 2 diabetes among schoolchildren in Taiwan. Diabetes Care. 2003;26(2):343–348. doi: 10.2337/diacare.26.2.343. [DOI] [PubMed] [Google Scholar]
- 19.Dabelea D, Knowler WC, Pettitt DJ. Effect of diabetes in pregnancy on offspring: follow-up research in the Pima Indians. Journal of Maternal-Fetal and Neonatal Medicine. 2000;9(1):83–88. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<83::AID-MFM17>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 20.Young TK, Martens PJ, Taback SP, et al. Type 2 diabetes mellitus in children: prenatal and early infancy risk factors among Native Canadians. Archives of Pediatrics and Adolescent Medicine. 2002;156(7):651–655. doi: 10.1001/archpedi.156.7.651. [DOI] [PubMed] [Google Scholar]
- 21.Hegele RA, Zinman B, Hanley AJG, Harris SB, Barrett PH, Cao H. Genes, environment and Oji-Cree type 2 diabetes. Clinical Biochemistry. 2003;36(3):163–170. doi: 10.1016/s0009-9120(03)00004-3. [DOI] [PubMed] [Google Scholar]
- 22.Sellers EA, Triggs-Raine B, Rockman-Greenberg C, Dean HJ. The prevalence of the HNF-1α G319S mutation in Canadian aboriginal youth with type 2 diabetes. Diabetes Care. 2002;25(12):2202–2206. doi: 10.2337/diacare.25.12.2202. [DOI] [PubMed] [Google Scholar]
- 23.Remuzzi G, Schieppati A, Ruggenenti P. Nephropathy in patients with type 2 diabetes. The New England Journal of Medicine. 2002;346(15):1145–1151. doi: 10.1056/NEJMcp011773. [DOI] [PubMed] [Google Scholar]
- 24.NAPRTCS 2008 annual report. Renal transplantation dialysis chronic renal insufficiency. 2008.
- 25.Krakoff J, Lindsay RS, Looker HC, Nelson RG, Hanson RL, Knowler WC. Incidence of retinopathy and nephropathy in youth-onset compared with adult-onset type 2 diabetes. Diabetes Care. 2003;26(1):76–81. doi: 10.2337/diacare.26.1.76. [DOI] [PubMed] [Google Scholar]
- 26.Scott AR, Toomath R, Bouchier D, et al. First national audit of the outcomes of care in young people with diabetes in New Zealand: high prevalence of nephropathy in Māori and Pacific Islanders. The New Zealand Medical Journal. 2006;119(1235) Article ID U2015. [PubMed] [Google Scholar]
- 27.McGrath NM, Parker GN, Dawson P. Early presentation of type 2 diabetes mellitus in young New Zealand Maori. Diabetes Research and Clinical Practice. 1999;43(3):205–209. doi: 10.1016/s0168-8227(99)00003-0. [DOI] [PubMed] [Google Scholar]
- 28.Fagot-Campagna A, Knowler WC, Pettitt DJ. Type 2 diabetes in Pima Indian children: cardiovascular risk factors at diagnosis and 10 years later. Diabetes. 1998;47(supplement 1):p. A155. [Google Scholar]
- 29.Yoo EG, Choi IK, Kim DH. Prevalence of microalbuminuria in young patients with type 1 and type 2 diabetes mellitus. Journal of Pediatric Endocrinology and Metabolism. 2004;17(10):1423–1427. doi: 10.1515/jpem.2004.17.10.1423. [DOI] [PubMed] [Google Scholar]
- 30.Yokoyama H, Okudaira M, Otani T, et al. High incidence of diabetic nephropathy in early-onset Japanese NIDDM patients risk analysis. Diabetes Care. 1998;21(7):1080–1085. doi: 10.2337/diacare.21.7.1080. [DOI] [PubMed] [Google Scholar]
- 31.Eppens MC, Craig ME, Cusumano J, et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care. 2006;29(6):1300–1306. doi: 10.2337/dc05-2470. [DOI] [PubMed] [Google Scholar]
- 32.Ettinger LM, Freeman K, DiMartino-Nardi JR, Flynn JT. Microalbuminuria and abnormal ambulatory blood pressure in adolescents with type 2 diabetes mellitus. Journal of Pediatrics. 2005;147(1):67–73. doi: 10.1016/j.jpeds.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Copeland KC, Zeitler P, Geffner M, et al. Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. Journal of Clinical Endocrinology and Metabolism. 2011;96(1):159–167. doi: 10.1210/jc.2010-1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dart AB, Sellers EA, Martens PJ, Rigatto C, Brownell MD, Dean HJ. High burden of kidney disease in youth onset type 2 diabetes. Diabetes Care. In Press. [DOI] [PMC free article] [PubMed]
- 35.Rudberg S, Dahlquist G. Determinants of progression of microalbuminuria in adolescents with IDDM. Diabetes Care. 1996;19(4):369–371. doi: 10.2337/diacare.19.4.369. [DOI] [PubMed] [Google Scholar]
- 36.Steinke JM, Mauer M, Aebi C, et al. Lessons learned from studies of the natural history of diabetic nephropathy in young type 1 diabetic patients. Pediatric Endocrinology Reviews. 2008;5(supplement 4):958–963. [PubMed] [Google Scholar]
- 37.Soedamah-Muthu SS, Visseren FLJ, Algra A, Van Der Graaf Y. The impact of Type 2 diabetes and microalbuminuria on future cardiovascular events in patients with clinically manifest vascular disease from the Second Manifestations of ARTerial disease (SMART) study. Diabetic Medicine. 2008;25(1):51–57. doi: 10.1111/j.1464-5491.2007.02345.x. [DOI] [PubMed] [Google Scholar]
- 38.Schultz CJ, Konopelska-Bahu T, Dalton RN, et al. Microalbuminuria prevalence varies with age, sex, and puberty in children with type 1 diabetes followed from diagnosis in a longitudinal study. Diabetes Care. 1999;22(3):495–502. doi: 10.2337/diacare.22.3.495. [DOI] [PubMed] [Google Scholar]
- 39.Pavkov ME, Bennett PH, Knowler WC, Krakoff J, Sievers ML, Nelson RG. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. Journal of the American Medical Association. 2006;296(4):421–426. doi: 10.1001/jama.296.4.421. [DOI] [PubMed] [Google Scholar]
- 40.Dean H, Flett B. Natural history of type 2 diabetes mellitus diagnosed in childhood; long term follow-up in young adults. Diabetes. 2002;51(supplement 2, 99-OR):p. A24. [Google Scholar]
- 41.Yokoyama H, Okudaira M, Otani T, et al. Higher incidence of diabetic nephropathy in type 2 than in type 1 diabetes in early-onset diabetes in Japan. Kidney International. 2000;58(1):302–311. doi: 10.1046/j.1523-1755.2000.00166.x. [DOI] [PubMed] [Google Scholar]
- 42.Yokoyama H, Okudaira M, Otani T, et al. Existence of early-onset NIDDM Japanese demonstrating severe diabetic complications. Diabetes Care. 1997;20(5):844–847. doi: 10.2337/diacare.20.5.844. [DOI] [PubMed] [Google Scholar]
- 43.Canadian Diabetes Association Clinical Practice. Guidelines Expert Committee. Chronic kidney disease in diabetes. Canadian Journal of Diabetes. 2008;32(Supplement 1):S126–S133. [Google Scholar]
- 44.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2, supplement 4th report):555–576. [PubMed] [Google Scholar]
- 45.Kim NH, Pavkov ME, Knowler WC, et al. Predictive value of albuminuria in American Indian youth with or without type 2 diabetes. Pediatrics. 2010;125(4):e844–e851. doi: 10.1542/peds.2009-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pettitt DJ, Saad MF, Bennett PH, Nelson RG, Knowler WC. Familial predisposition to renal disease in two generations of Pima Indians with Type 2(non-insulin-dependent) diabetes mellitus. Diabetologia. 1990;33(7):438–443. doi: 10.1007/BF00404096. [DOI] [PubMed] [Google Scholar]
- 47.Faronato PP, Maioli M, Tonolo G, Brocco E, Noventa F, Piarulli F, et al. Clustering of albumin excretion rate abnormalities in Caucasian patients with NIDDM. The Italian NIDDM Nephropathy Study Group. Diabetologia. 1997;40(7):816–823. doi: 10.1007/s001250050754. [DOI] [PubMed] [Google Scholar]
- 48.Gall MA, Hougaard P, Borch-Johnsen K, Parving HH. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: prospective, observational study. The British Medical Journal. 1997;314(7083):783–788. doi: 10.1136/bmj.314.7083.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nelson RG, Bennett PH, Beck GJ, et al. Development and progression of renal disease in Pima Indians with non- insulin-dependent diabetes mellitus. The New England Journal of Medicine. 1996;335(22):1636–1642. doi: 10.1056/NEJM199611283352203. [DOI] [PubMed] [Google Scholar]
- 50.Shamoon H, Duffy H, Fleischer N, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England Journal of Medicine. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 51.Diabetic Nephropathy. American Diabetes Association. 2002;25(Supplement 1):S85–S86–S89. [Google Scholar]
- 52.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. The Lancet. 1998 ;352(9131):837–853. [PubMed] [Google Scholar]
- 53.Eppens MC, Craig ME, Jones TW, Silink M, Ong S, Ping YJ. Type 2 diabetes in youth from the Western Pacific region: glycaemic control, diabetes care and complications. Current Medical Research and Opinion. 2006;22(5):1013–1020. doi: 10.1185/030079906X104795. [DOI] [PubMed] [Google Scholar]
- 54.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. 2008 clinical practice guidelines type 2 diabetes in children and adolescents. The Canadian Journal of Diabetes. 2008;32(supplement 1):S162–S167. [Google Scholar]
- 55.Sellers EAC, Yung G, Dean HJ. Dyslipidemia and other cardiovascular risk factors in a Canadian First Nation pediatric population with type 2 diabetes mellitus. Pediatric Diabetes. 2007;8(6):384–390. doi: 10.1111/j.1399-5448.2007.00284.x. [DOI] [PubMed] [Google Scholar]
- 56.Dean HJ, Sellers EAC. Comorbidities and microvascular complications of type 2 diabetes in children and adolescents. Pediatric Diabetes. 2007;8(9):35–41. doi: 10.1111/j.1399-5448.2007.00340.x. [DOI] [PubMed] [Google Scholar]
- 57.Adelman RD, Restaino IG, Alon US, Blowey DL. Proteinuria and focal segmental glomerulosclerosis in severely obese adolescents. Journal of Pediatrics. 2001;138(4):481–485. doi: 10.1067/mpd.2001.113006. [DOI] [PubMed] [Google Scholar]
- 58.Sarafidis PA. Obesity, insulin resistance and kidney disease risk: insights into the relationship. Current Opinion in Nephrology and Hypertension. 2008;17(5):450–456. doi: 10.1097/MNH.0b013e328305b994. [DOI] [PubMed] [Google Scholar]
- 59.Bagby SP. Obesity-initiated metabolic syndrome and the kidney: a recipe for chronic kidney disease? Journal of the American Society of Nephrology. 2004;15(11):2775–2791. doi: 10.1097/01.ASN.0000141965.28037.EE. [DOI] [PubMed] [Google Scholar]
- 60.Scott CR, Smith JM, Cradock MM, Pihoker C. Characteristics of youth-onset noninsulin-dependent diabetes mellitus and insulin-dependent diabetes mellitus at diagnosis. Pediatrics. 1997;100(1):84–91. doi: 10.1542/peds.100.1.84. [DOI] [PubMed] [Google Scholar]
- 61.Upchurch SL, Brosnan CA, Meininger JC, et al. Characteristics of 98 children and adolescents diagnosed with type 2 diabetes by their health care provider at initial presentation. Diabetes Care. 2003;26(7):p. 2209. doi: 10.2337/diacare.26.7.2209. [DOI] [PubMed] [Google Scholar]
- 62.Hotu S, Carter B, Watson PD, Cutfield WS, Cundy T. Increasing prevalence of type 2 diabetes in adolescents. Journal of Paediatrics and Child Health. 2004;40(4):201–204. doi: 10.1111/j.1440-1754.2004.00337.x. [DOI] [PubMed] [Google Scholar]
- 63.Zdravkovic V, Daneman D, Hamilton J. Presentation and course of Type 2 diabetes in youth in a large multi-ethnic city. Diabetic Medicine. 2004;21(10):1144–1148. doi: 10.1111/j.1464-5491.2004.01297.x. [DOI] [PubMed] [Google Scholar]
- 64.Rodriguez BL, Fujimoto WY, Mayer-Davis EJ, et al. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2006;29(8):1891–1896. doi: 10.2337/dc06-0310. [DOI] [PubMed] [Google Scholar]
- 65.Mortensen HB, Marinelli K, Norgaard K, et al. A nation-wide cross-sectional study of urinary albumin excretion rate, arterial blood pressure and blood glucose control in Danish children with type 1 diabetes mellitus. Diabetic Medicine. 1990;7(10):887–897. doi: 10.1111/j.1464-5491.1990.tb01324.x. [DOI] [PubMed] [Google Scholar]
- 66.Wei JN, Sung FC, Lin CC, Lin RS, Chiang CC, Chuang LM. National surveillance for type 2 diabetes mellitus in Taiwanese children. Journal of the American Medical Association. 2003;290(10):1345–1350. doi: 10.1001/jama.290.10.1345. [DOI] [PubMed] [Google Scholar]
- 67.Kershnar AK, Daniels SR, Imperatore G, et al. Lipid abnormalities are prevalent in youth with type 1 and type 2 diabetes: the SEARCH for diabetes in youth study. Journal of Pediatrics. 2006;149(3):314–319. doi: 10.1016/j.jpeds.2006.04.065. [DOI] [PubMed] [Google Scholar]
- 68.Newfield RS, Dewan AK, Jain S. Dyslipidemia in children with type 2 diabetes vs. obesity. Pediatric Diabetes. 2008;9(2):115–121. doi: 10.1111/j.1399-5448.2007.00345.x. [DOI] [PubMed] [Google Scholar]
- 69.Hargrave DR, McMaster C, O’Hare MMT, Carson DJ. Tobacco smoke exposure in children and adolescents with diabetes mellitus. Diabetic Medicine. 1999;16(1):31–34. doi: 10.1046/j.1464-5491.1999.00016.x. [DOI] [PubMed] [Google Scholar]
- 70.Holl RW, Grabert M, Heinze E, Debatin KM. Objective assessment of smoking habits by urinary cotinine measurement in adolescents and young adults with type 1 diabetes. Reliability of reported cigarette consumption and relationship to urinary albumin excretion. Diabetes Care. 1998;21(5):787–791. doi: 10.2337/diacare.21.5.787. [DOI] [PubMed] [Google Scholar]
- 71.Harvey JN, Allagoa B. The long-term renal and retinal outcome of childhood-onset Type 1 diabetes. Diabetic Medicine. 2004;21(1):26–31. doi: 10.1046/j.1464-5491.2003.01062.x. [DOI] [PubMed] [Google Scholar]
- 72.Orth SR, Schroeder T, Ritz E, Ferrari P. Effects of smoking on renal function in patients with type 1 and type 2 diabetes mellitus. Nephrology Dialysis Transplantation. 2005;20(11):2414–2419. doi: 10.1093/ndt/gfi022. [DOI] [PubMed] [Google Scholar]
- 73.Ruggenenti P, Remuzzi G. Nephropathy of type-2 diabetes mellitus. Journal of the American Society of Nephrology. 1998;9(11):2157–2169. doi: 10.1681/ASN.V9112157. [DOI] [PubMed] [Google Scholar]
- 74.Sellers EA, Blydt-Hansen TD, Dean HJ, Gibson IW, Birk PE, Ogborn M. Macroalbuminuria and renal pathology in first nation youth with type 2 diabetes. Diabetes Care. 2009;32(5):786–790. doi: 10.2337/dc08-1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bulloch B, Postl BD, Ogborn MR. Excess prevalence of non diabetic renal disease in native American children in Manitoba. Pediatric Nephrology. 1996;10(6):702–704. doi: 10.1007/s004670050193. [DOI] [PubMed] [Google Scholar]
- 76.Dyck RF, Tan L. Rates and outcomes of diabetic end-stage renal disease among registered native people in Saskatchewan. CMAJ. 1994;150(2):203–208. [PMC free article] [PubMed] [Google Scholar]
- 77.Dyck RF, Tan L. Non-diabetic end-stage renal disease among Saskatchewan aboriginal people. Clinical and Investigative Medicine. 1998;21(1):33–38. [PubMed] [Google Scholar]
- 78.Mazzucco G, Bertani T, Fortunato M, et al. Different patterns of renal damage in type 2 diabetes mellitus: a multicentric study on 393 biopsies. The American Journal of Kidney Diseases. 2002;39(4):713–720. doi: 10.1053/ajkd.2002.31988. [DOI] [PubMed] [Google Scholar]
- 79.Donaghue KC, Chiarelli F, Trotta D, Allgrove J, Dahl-Jorgensen K. International Society for Pediatric and Adolescent Diabetes. ISPAD clinical practice consensus guidelines 2006-2007, microvascular and macrovascular complications. Pediatr Diabetes. 2007;8(3):163–170. doi: 10.1111/j.1399-5448.2007.00250.x. [DOI] [PubMed] [Google Scholar]
- 80.Gatling W, Knight C, Hill RD. Screening for early diabetic nephropathy: which sample to detect microalbuminuria? Diabetic Medicine. 1985;2(6):451–455. doi: 10.1111/j.1464-5491.1985.tb00681.x. [DOI] [PubMed] [Google Scholar]
- 81.Rosenbloom AL, Silverstein JH, Amemiya S, Zeitler P, Klingensmith GJ. Type 2 diabetes in children and adolescents. Pediatric Diabetes. 2009;10(12):17–32. doi: 10.1111/j.1399-5448.2009.00584.x. [DOI] [PubMed] [Google Scholar]
- 82.Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clinical Journal of the American Society of Nephrology. 2009;4(11):1832–1843. doi: 10.2215/CJN.01640309. [DOI] [PubMed] [Google Scholar]
- 83.Pinhas-Hamiel O, Zeitler P. Clinical presentation and treatment of type 2 diabetes in children. Pediatric Diabetes. 2007;8(supplement 9):16–27. doi: 10.1111/j.1399-5448.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 84.Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. Journal of Pediatrics. 1996;128(5 I):608–615. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 85.Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. The New England Journal of Medicine. 2001;345(12):851–860. doi: 10.1056/NEJMoa011303. [DOI] [PubMed] [Google Scholar]
- 86.Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. The New England Journal of Medicine. 2001;345(12):870–878. doi: 10.1056/NEJMoa011489. [DOI] [PubMed] [Google Scholar]
- 87.Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. The New England Journal of Medicine. 2001;345(12):861–869. doi: 10.1056/NEJMoa011161. [DOI] [PubMed] [Google Scholar]
- 88.Remuzzi G, Macia M, Ruggenenti P. Prevention and treatment of diabetic renal disease in type 2 diabetes: the BENEDICT study. Journal of the American Society of Nephrology. 2006;17(2, supplement):S90–S97. doi: 10.1681/ASN.2005121324. [DOI] [PubMed] [Google Scholar]
- 89.Yuksel H, Darcan S, Kabasakal C, Cura A, Mir S, Mavi E. Effect of enalapril on proteinuria, phosphaturia, and calciuria in insulin-dependent diabetes. Pediatric Nephrology. 1998;12(8):648–650. doi: 10.1007/s004670050520. [DOI] [PubMed] [Google Scholar]
- 90.Rudberg S, Aperia A, Freyschuss U, Persson B. Enalapril reduces microalbuminuria in young normotensive Type 1 (insulin-dependent) diabetic patients irrespective of its hypotensive effect. Diabetologia. 1990;33(8):470–476. doi: 10.1007/BF00405108. [DOI] [PubMed] [Google Scholar]
- 91.Cook J, Daneman D, Spino M, Sochett E, Perlman K, Balfe JW. Angiotensin converting enzyme inhibitor therapy to decrease microalbuminuria in normotensive children with insulin-dependent diabetes mellitus. Journal of Pediatrics. 1990;117(1, par 1):39–45. doi: 10.1016/s0022-3476(05)82441-2. [DOI] [PubMed] [Google Scholar]
- 92.Cooper WO, Hernandez-Diaz S, Arbogast PG, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. The New England Journal of Medicine. 2006;354(23):2443–2451. doi: 10.1056/NEJMoa055202. [DOI] [PubMed] [Google Scholar]
- 93.Lauer RM, Barness LA, Clark R, et al. National Cholesterol Education Program (NCEP): highlights of the report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics. 1992;89(3):495–501. [PubMed] [Google Scholar]
- 94.Donaghue KC, Chiarelli F, Trotta D, Allgrove J, Dahl-Jorgensen K. Microvascular and macrovascular complications associated with diabetes in children and adolescents. Pediatric Diabetes. 2009;10(12):195–203. doi: 10.1111/j.1399-5448.2009.00576.x. [DOI] [PubMed] [Google Scholar]


