INTRODUCTION
Spinal cord injury (SCI) is a devastating condition associated with significant functional and sensory deficits, emotional, social, and financial burdens, and an increased risk of cardiovascular complications, deep vein thrombosis, osteoporosis, pressure ulcers, autonomic dysreflexia, and neuropathic pain.
The estimated annual global incidence of SCI is 15–40 cases per million. In the USA, approximately 1.275 million individuals are affected, with over 12,000 new cases each year.1–5 The most common causes of traumatic SCI are road traffic accidents, falls, occupational and sports-related injuries that result in contusion and compression of the spinal cord.1 Approximately 55% of SCIs occur at the cervical level (C1 to C7-T1) with a mortality of 10% in the first year following injury and an expected lifespan of only 10–15 years post-injury, and thoracic (T1–T11), thoracolumbar (T11–T12 to L1–L2) and lumbosacral (L2–S5) injuries each account for approximately 15% of SCI.1–4 Depending on the age of the patient, severity, and levels of SCI, the lifetime cost of health care and other injury-related expenses can reach $25 million.1–5
Despite advances in pre-hospital care, medical and surgical management and rehabilitation approaches, many SCI sufferers still experience substantial neurological disability. Intensive efforts are underway to develop effective neuroprotective and regenerative strategies.
PATHOPHYSIOLOGY
SCI involves a primary (the physical injury) and a secondary injury (the subsequent cascade of molecular and cellular events which amplify the original injury).6 The primary injury damages both upper and lower motor neurons and disrupts motor, sensory and autonomic functions. Pathophysiological processes occurring in the secondary injury phase are rapidly instigated in response to the primary injury in an attempt to homeostatically control and minimize the damage. Paradoxically, this response is largely responsible for exacerbating the initial damage and creating an inhibitory milieu that prevents endogenous efforts of repair, regeneration and remyelination. These secondary processes include inflammation, ischemia, lipid peroxidation, production of free radicals, disruption of ion channels, axonal demyelination, glial scarring (astrogliosis), necrosis and programmed cell death. Nevertheless, endogenous repair and regenerative mechanisms during the secondary phase of injury minimize the extent of the lesion (through astrogliosis), reorganize blood supply through angiogenesis, clear cellular debris, and reunite and remodel damaged neural circuits. The spatial and temporal dynamics of these secondary mediators7 are fundamental to SCI pathophysiology and as such offer exploitable targets for therapeutic intervention.
CELL THERAPY
A multitude of characteristics of cells tested pre-clinically and clinically make them attractive to potentially address the multifactorial nature of the pathophysiology of secondary SCI – they are anti-inflammatory, immunomodulatory,8–12 anti-gliotic,13 pro-oligodendrogliogenic,14 pro-neuronogenic,15 and secrete various anti-apoptotic and pro-angiogenic neurotrophic factors. Given the pathophysiological targets of SCI,7 transplanted cells should: 1) enable regenerating axons to cross barriers; 2) functionally replace lost cells; and/or 3) create an environment supportive of neural repair.16 However, given the multifactorial nature of SCI and its dynamic pathophysiological consequences, the success of future clinical trials of cell therapy will likely depend on the informed co-administration of multiple strategies, including pharmacological and rehabilitation therapies.7
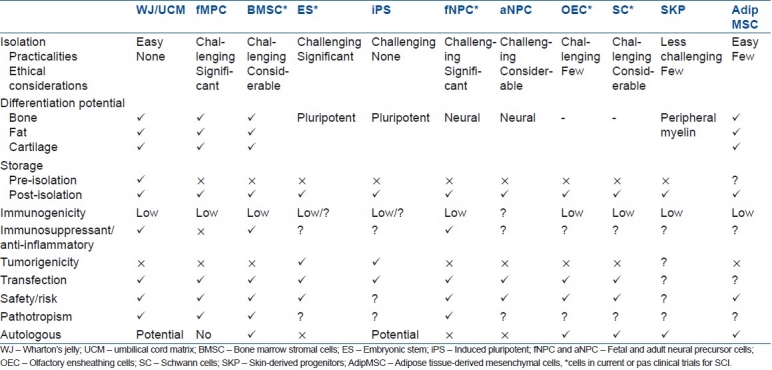
Different sources and types of cells have been and/or are being tested in clinical trials for SCI, including embryonic stem cells (ESCs), neural progenitor cells (NPCs), bone marrow mesenchymal cells (BMSCs) and non-stem cells such as olfactory ensheathing cells and Schwann cells.17 Other cell types are being developed for the clinic, including other sources of mesenchymal cells (fetal blood,18 adipose tissue, umbilical cord19–36), adult21,37 and immortalized neural progenitors (PISCES, NCT01151124), skin-derived progenitors,38–47 induced pluripotent stem cells48–52 and endogenous spinal cord progenitors53–58 [Table 1]. The advantages and disadvantages of each cell source and type being considered or already in clinical trials for SCI have been extensively described and compared elsewhere,17,59–63 and reflect their potential in the clinic [Table 1]. There are currently more than a dozen cell therapy clinical trials for SCI listed on clinicaltrials.gov.64 Most are Phase I or I/II clinical safety and feasibility studies, indicating that cellular treatments for SCI developed in the laboratory are still in the very early stages of clinical translation.
Table 1.
A comparison of the different cell types and sources currently in (*) or under consideration for clinical trials for SCI
This editorial will focus specifically on the most widely studied progenitor cells currently in clinical trials for SCI: BMSCs and NPCs.
BONE MARROW STROMAL CELLS
BMSCs are isolated from the stromal compartment of bone marrow, and fractioned from hematopoietic stem cells by virtue of their adherence to tissue culture plastic and/or their expression of distinct cell surface antigenic markers. They are non-teratogenic, have anti-inflammatory and immunomodulatory effects65,66 and secrete neurotrophic factors, making them attractive candidates in CNS cell rescue and as autologous transplanted cellular sources of trophic support for endogenous and co-implanted cells. Despite recurring claims of their neurogenic differentiation potential in vitro or in vivo, there is no conclusive evidence to support this.67
Most studies of BMSCs have found beneficial effects of BMSC administration after thoracic SCI, largely as a result of neurotrophic factor secretion68,69 and possibly also anti-inflammatory cytokine secretion. Intraspinal as well as intrathecal and systemic (intravenous) routes of delivery have been successful.70–72 Porcine and non-human primate studies have been carried out to further support their clinical use,73,74 and as in rodent studies, it has been found that BMSCs promote a certain degree of axonal regrowth and sprouting, at least in transection models,75 especially when treated with growth factors prior to being implanted.68
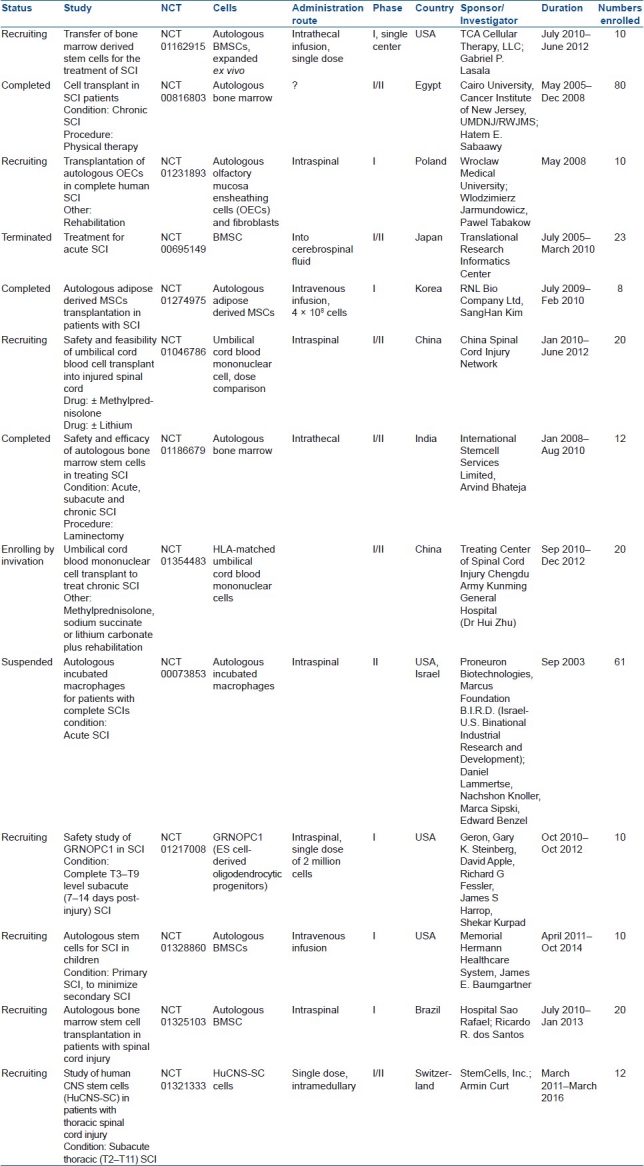
The inflammatory component of SCI and subsequent demyelination of surviving axons are serious limiting factors in the efficacy of early cell therapy for SCI, as implanted cells are more likely to be eliminated by the host.76 The immunomodulatory effect of bone marrow-derived cells has been demonstrated in the Canadian Bone Marrow Transplant (BMT) clinical trials for multiple sclerosis led by Freedman.65,66 It is therefore worth considering interventions to modify the inflammatory milieu in order to enhance donor cell survival and efficacy, as in the newly initiated clinical trial of autologous BMSCs in children suffering from SCI [Table 2] (NCT01328860).
Table 2.
Clinical trials of cell therapy for SCI listed on www.clinicaltrials.gov.
Ongoing clinical studies and those carried out to date have enrolled small patient numbers and have used autologous marrow-derived cells rather than purified stromal cells.77–80 A recently published dose-escalation trial examined autologous BMSCs in patients with chronic SCI.66 Although BMSCs were safe, they were not found to be beneficial in this cohort of patients. Having clearly established the safety and feasibility of the clinical use of BM-derived cells specifically for SCI in these trials, the continued testing of BMSCs in the context of SCI appears justified although the use of this intervention in complete thoracic cases may not be optimal. Based on the mechanism of action of BMSCs, which appear to provide trophic support to the penumbra zone of the acutely and subacutely injured cord, trials in patients with subacute severe, but incomplete spinal cord lesions are a consideration.
The use of BMSCs in SCI does, however, present certain issues. BMSC migration beyond the injection site (for intraspinally delivered cells) is limited, and inter-donor variability in efficacy and immunomodulatory potency might confer variable clinical outcome,81 making evaluation of efficacy difficult. Studies of BMSCs in cervical contusion-compression models have yet to be carried out. BMSCs have, in all but two studies by the same group, been used in subacute and acute models.82–85 Based on the limited number of pre-clinical studies in chronic models, it is not yet possible to evaluate their efficacy. It is also not known whether BMSCs provide functional preservation of axons or de novo axonal regrowth across the lesion site in contusion–compression models, which are more appropriate models to distinguish these processes than transection models.86–89
NEURAL PROGENITOR CELLS
NPCs can be generated from ESCs, which are derived from the blastocyst-stage embryo. These cells have indefinite self-renewal capacity and are pluripotent, with the potential to generate all cell types of the body, making them a potentially limitless source of cells for therapy. However, they are not without problems [Table 1], including the moral issues and practical constraints of their embryonic derivation, their karyotypic instability with repeated freeze–thaw cycles,90,91 and their teratogenic potential in the host.
Pre-clinical studies have shown that animals transplanted with human ESC-derived oligodendrocytic progenitors cells (OPCs) show improvement in functional recovery following SCI.12,92–96 With this background, extensive pre-clinical studies were conducted by Geron to characterize the safety and efficacy of hESC-OPCs exclusively in rodent models prior to the conduct (not without considerable objection and controversy) of a clinical trial of human ESC-derived OPCs implanted within 2 weeks into patients with thoracic SCI.97–99 This Geron-sponsored clinical trial is further supported by behavioral and histological data from studies implanting glial restricted progenitors (GRPs)100 and OPCs101,102 isolated from embryonic and post-natal rodents in SCI models, albeit indirectly. Whilst these show predominantly astroglial differentiation of GRP implanted within the blunt contusion-induced thoracic lesion site, there is a shift toward oligodendrocytic specification beyond the injury site correlated with the degree of functional improvement,103–105 both of which can be enhanced by transduction of factors such as D15A, brain-derived neurotrophic factor (BDNF) and neurotrophin-3 (NT-3).106 GRP implantation was also shown to be neuroprotective and inhibited neuropathic pain.
Neural progenitor cells can also be derived from several regions of the fetal, post-natal and adult CNS, including the sub-ventricular zone of the brain, the central canal of the spinal cord and the hippocampus. They can be expanded in culture as non-adherent neurospheres and have the potential to generate all three neural cell types under the appropriate conditions. The key advantage of this NPC source is the amenability to in vitro manipulation (including immortalization) prior to implantation as well as the lack of tumorigenicity. However, autologous derivation of CNS NPCs would be unfeasible for cell therapy purposes.
On the basis of promising results in clinically relevant primate107–109 and canine cervical contusion models of SCI and cell number-dependent locomotor recovery in acute, subacute and chronic thoracic rodent models,110–113 a StemCells Inc-sponsored clinical trial is underway to treat SCI sufferers with non-immortalized fetal human CNS stem cells (HuCNS-SC, NCT01321333). The lack of trials of NPCs in SCI is in spite of the bulk of pre-clinical findings to date in support of the potential of fetal and adult NPCs (particularly the former) in experimental SCI models,17 and is likely to reflect ethical concerns over their origins and practical issues hindering their isolation and directed differentiation. Another possible explanation for the absence of clinical trials of NPCs for SCI is that the mechanisms through which NPCs provide functional benefit (including immunomodulation and angiogenesis) are only now beginning to be understood. Also, aims of axonal regeneration through the injury site have been replaced pre-clinically by more realistic objectives of remyelination17 and provision of trophic support for endogenous precursors and axons. This makes NPCs much more promising candidates for cell therapy for SCI and probably heralds their increased use in clinical trials.
CONCLUSION
Cell therapy can potentially enhance the quality of life of those affected by SCI. The significant advances that have been made on the basis of pre-clinical studies carried out in rodent models of SCI have enabled clinical trials demonstrating the safety of cell therapy for SCI to proceed and have informed researchers of the knowledge gaps that remain to be addressed. However, rodent contusion/compression models of SCI are generally “incomplete” with partial sparing of motor and sensory functions, and mimic most closely patients with severe, partial lesions with an American Spinal Injury Association (ASIA) impairment scale rating of AIS B or C. Given that most trials of cell therapy have been carried out in AIS A patients (the safest to treat but also the least likely to show cell therapy-induced benefit), there is a need for future clinical trials to include patients modeled in the laboratory. There is a compelling need for preclinical researchers to develop valid models of compressive/contusive cervical SCI given that approximately 50–60% of human SCI involves the cervical region.
ACKNOWLEDGEMENTS
Thank you to Dr Madeleine O’Higgins, Communications Specialist, for help with the manuscript and submission of this Editorial.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Sekhon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26(24 Suppl):S2–12. doi: 10.1097/00007632-200112151-00002. [DOI] [PubMed] [Google Scholar]
- 2.Spinal Cord Injury Facts and Statistics, Rick Hansen Spinal Cord Injury Registry. 2006. http://rickhansenregistry.org/en/news-and-resources/sci-facts.html .
- 3.Birmingham, Alabama: 2010. Spinal cord injury facts and figures at a glance, National Spinal Cord Injury Statistical Center. https://www.nscisc.uab.edu/public_content/pdf/Facts%202011%20Feb%20Final.pdf . [PubMed] [Google Scholar]
- 4.New Jersey: Christopher and Dana Reeve Foundation; 2010. One Degree of Separation: Paralysis and Spinal Cord Injury in the United States. [Google Scholar]
- 5.Fehlings MG, Tighe A. Spinal cord injury: The promise of translational research. Neurosurg Focus. 2008;25:E1. doi: 10.3171/FOC.2008.25.11.E1. [DOI] [PubMed] [Google Scholar]
- 6.Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg. 1991;75:15–26. doi: 10.3171/jns.1991.75.1.0015. [DOI] [PubMed] [Google Scholar]
- 7.Figley SA, Austin JW, Rowland JW, Fehlings MG. Philadelphia: Lippincott, Williams and Wilkins; 2011. Pathophysiology of Spinal Cord Injury, in The Cervical Spine (in review) [Google Scholar]
- 8.Wang L, Shi J, van Ginkel FW, Lan L, Niemeyer G, Martin DR, et al. Neural stem/progenitor cells modulate immune responses by suppressing T lymphocytes with nitric oxide and prostaglandin E2. Exp Neurol. 2009;216:177–83. doi: 10.1016/j.expneurol.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Pluchino S, Gritti A, Blezer E, Amadio S, Brambilla E, Borsellino G, et al. Human neural stem cells ameliorate autoimmune encephalomyelitis in non-human primates. Ann Neurol. 2009;66:343–54. doi: 10.1002/ana.21745. [DOI] [PubMed] [Google Scholar]
- 10.Okamura RM, Lebkowski J, Au M, Priest CA, Denham J, Majumdar AS. Immunological properties of human embryonic stem cell-derived oligodendrocyte progenitor cells. J Neuroimmunol. 2007;192:134–44. doi: 10.1016/j.jneuroim.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 11.Bai L, Lennon DP, Eaton V, Maier K, Caplan AI, Miller SD, et al. Human bone marrow-derived mesenchymal stem cells induce Th2-polarized immune response and promote endogenous repair in animal models of multiple sclerosis. Glia. 2009;57:1192–203. doi: 10.1002/glia.20841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bottai D, Cigognini D, Madaschi L, Adami R, Nicora E, Menarini M, et al. Embryonic stem cells promote motor recovery and affect inflammatory cell infiltration in spinal cord injured mice. Exp Neurol. 2010;223:452–63. doi: 10.1016/j.expneurol.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Jaderstad J, Jäderstad LM, Li J, Chintawar S, Salto C, Pandolfo M, et al. Communication via gap junctions underlies early functional and beneficial interactions between grafted neural stem cells and the host. Proc Natl Acad Sci U S A. 2010;107:5184–9. doi: 10.1073/pnas.0915134107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arriola A, Kiel ME, Shi Y, McKinnon RD. Adjunctive MSCs enhance myelin formation by xenogenic oligodendrocyte precursors transplanted in the retina. Cell Res. 2010;20:728–31. doi: 10.1038/cr.2010.63. [DOI] [PubMed] [Google Scholar]
- 15.Zhang J, Wang B, Xiao Z, Zhao Y, Chen B, Han J, et al. Olfactory ensheathing cells promote proliferation and inhibit neuronal differentiation of neural progenitor cells through activation of Notch signaling. Neuroscience. 2008;153:406–13. doi: 10.1016/j.neuroscience.2008.02.067. [DOI] [PubMed] [Google Scholar]
- 16.Rowland JW, Hawryluk GW, Kwon B, Fehlings MG. Current status of acute spinal cord injury pathophysiology and emerging therapies: Promise on the horizon. Neurosurg Focus. 2008;25:E2. doi: 10.3171/FOC.2008.25.11.E2. [DOI] [PubMed] [Google Scholar]
- 17.Tetzlaff W, Okon EB, Karimi-Abdolrezaee S, Hill CE, Sparling JS, Plemel JR, et al. A systematic review of cellular transplantation therapies for spinal cord injury. J Neurotrauma. 2011;28:1611–82. doi: 10.1089/neu.2009.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campagnoli C, Roberts IA, Kumar S, Bennett PR, Bellantuono I, Fisk NM. Identification of mesenchymal stem/progenitor cells in human first-trimester fetal blood, liver, and bone marrow. Blood. 2001;98:2396–402. doi: 10.1182/blood.v98.8.2396. [DOI] [PubMed] [Google Scholar]
- 19.Ikegami T, Nakamura M, Yamane J, Katoh H, Okada S, Iwanami A, et al. Chondroitinase ABC combined with neural stem/progenitor cell transplantation enhances graft cell migration and outgrowth of growth-associated protein-43-positive fibers after rat spinal cord injury. Eur J Neurosci. 2005;22:3036–46. doi: 10.1111/j.1460-9568.2005.04492.x. [DOI] [PubMed] [Google Scholar]
- 20.Karimi-Abdolrezaee S, Eftekharpour E, Wang J, Schut D, Fehlings MG. Synergistic effects of transplanted adult neural stem/progenitor cells, chondroitinase, and growth factors promote functional repair and plasticity of the chronically injured spinal cord. J Neurosci. 2010;30:1657–76. doi: 10.1523/JNEUROSCI.3111-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bottai D, Madaschi L, Di Giulio AM, Gorio A. Viability-dependent promoting action of adult neural precursors in spinal cord injury. Mol Med. 2008;14:634–44. doi: 10.2119/2008-00077.Bottai. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hofstetter CP, Holmström NA, Lilja JA, Schweinhardt P, Hao J, Spenger C, et al. Allodynia limits the usefulness of intraspinal neural stem cell grafts; directed differentiation improves outcome. Nat Neurosci. 2005;8:346–53. doi: 10.1038/nn1405. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell KE, Weiss ML, Mitchell BM, Martin P, Davis D, Morales L, et al. Matrix cells from Wharton's jelly form neurons and glia. Stem Cells. 2003;21:50–60. doi: 10.1634/stemcells.21-1-50. [DOI] [PubMed] [Google Scholar]
- 24.Wang HS, Hung SC, Peng ST, Huang CC, Wei HM, Guo YJ, et al. Mesenchymal stem cells in the Wharton's jelly of the human umbilical cord. Stem Cells. 2004;22:1330–7. doi: 10.1634/stemcells.2004-0013. [DOI] [PubMed] [Google Scholar]
- 25.Weiss ML, Medicetty S, Bledsoe AR, Rachakatla RS, Choi M, Merchav S, et al. Human umbilical cord matrix stem cells: preliminary characterization and effect of transplantation in a rodent model of Parkinson's disease. Stem Cells. 2006;24:781–92. doi: 10.1634/stemcells.2005-0330. [DOI] [PubMed] [Google Scholar]
- 26.La Rocca G, Anzalone R, Corrao S, Magno F, Loria T, Lo Iacono M, et al. Isolation and characterization of Oct-4+/HLA-G+ mesenchymal stem cells from human umbilical cord matrix: Differentiation potential and detection of new markers. Histochem Cell Biol. 2009;131:267–82. doi: 10.1007/s00418-008-0519-3. [DOI] [PubMed] [Google Scholar]
- 27.Vawda R, Kennea NK, Mehmet H. Stem Cells in Neurodegeneration and Injury, in Tissue stem cells. In: Potten CS, Clarke RB, Wilson J, Renehan AG, editors. London: Taylor and Francis Pubs; 2006. pp. 271–93. [Google Scholar]
- 28.Vawda R, Woodbury J, Covey M, Levison SW, Mehmet H. Stem cell therapies for perinatal brain injuries. Semin Fetal Neonatal Med. 2007;12:259–72. doi: 10.1016/j.siny.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Troyer DL, Weiss ML. Wharton's jelly-derived cells are a primitive stromal cell population. Stem Cells. 2008;26:591–9. doi: 10.1634/stemcells.2007-0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss ML, Anderson C, Medicetty S, Seshareddy KB, Weiss RJ, VanderWerff I, et al. Immune properties of human umbilical cord Wharton's jelly-derived cells. Stem Cells. 2008;26:2865–74. doi: 10.1634/stemcells.2007-1028. [DOI] [PubMed] [Google Scholar]
- 31.Weiss ML, Mitchell KE, Hix JE, Medicetty S, El-Zarkouny SZ, Grieger D, et al. Transplantation of porcine umbilical cord matrix cells into the rat brain. Exp Neurol. 2003;182:288–99. doi: 10.1016/s0014-4886(03)00128-6. [DOI] [PubMed] [Google Scholar]
- 32.Lund RD, Wang S, Lu B, Girman S, Holmes T, Sauvé Y, et al. Cells isolated from umbilical cord tissue rescue photoreceptors and visual functions in a rodent model of retinal disease. Stem Cells. 2007;25:602–11. doi: 10.1634/stemcells.2006-0308. [DOI] [PubMed] [Google Scholar]
- 33.Ganta C, Chiyo D, Ayuzawa R, Rachakatla R, Pyle M, Andrews G, et al. Rat umbilical cord stem cells completely abolish rat mammary carcinomas with no evidence of metastasis or recurrence 100 days post-tumor cell inoculation. Cancer Res. 2009;69:1815–20. doi: 10.1158/0008-5472.CAN-08-2750. [DOI] [PubMed] [Google Scholar]
- 34.Ayuzawa R, Doi C, Rachakatla RS, Pyle MM, Maurya DK, Troyer D, et al. Naive human umbilical cord matrix derived stem cells significantly attenuate growth of human breast cancer cells in vitro and in vivo. Cancer Lett. 2009;280:31–7. doi: 10.1016/j.canlet.2009.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang CC, Shih YH, Ko MH, Hsu SY, Cheng H, Fu YS. Transplantation of human umbilical mesenchymal stem cells from Wharton's jelly after complete transection of the rat spinal cord. PLoS ONE. 2008;3:e3336. doi: 10.1371/journal.pone.0003336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang L, Zhang HT, Hong SQ, Ma X, Jiang XD, Xu RX. Cografted Wharton's Jelly Cells-derived neurospheres and BDNF promote functional recovery after rat spinal cord transection. Neurochem Res. 2009 doi: 10.1007/s11064-009-9992-x. [DOI] [PubMed] [Google Scholar]
- 37.Hernandeza J, Torres-Espina A, Navarro X. Adult stem cell transplants for spinal cord injury repair: Current state in preclinical research. Curr Stem Cell Res Ther. 2011;6:273–87. doi: 10.2174/157488811796575323. [DOI] [PubMed] [Google Scholar]
- 38.Biernaskie JA, McKenzie IA, Toma JG, Miller FD. Isolation of skin-derived precursors (SKPs) and differentiation and enrichment of their Schwann cell progeny. Nat Protoc. 2006;1:2803–12. doi: 10.1038/nprot.2006.422. [DOI] [PubMed] [Google Scholar]
- 39.Biernaskie J, Miller FD. White matter repair: Skin-derived precursors as a source of myelinating cells. Can J Neurol Sci. 2010;37(Suppl 2):S34–41. doi: 10.1017/s0317167100022411. [DOI] [PubMed] [Google Scholar]
- 40.Biernaskie J, Sparling JS, Liu J, Shannon CP, Plemel JR, Xie Y, et al. Skin-derived precursors generate myelinating Schwann cells that promote remyelination and functional recovery after contusion spinal cord injury. J Neurosci. 2007;27:9545–59. doi: 10.1523/JNEUROSCI.1930-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fernandes KJ, McKenzie IA, Mill P, Smith KM, Akhavan M, Barnabé-Heider F, et al. A dermal niche for multipotent adult skin-derived precursor cells. Nat Cell Biol. 2004;6:1082–93. doi: 10.1038/ncb1181. [DOI] [PubMed] [Google Scholar]
- 42.Fernandes KJ, Toma JG, Miller FD. Multipotent skin-derived precursors: Adult neural crest-related precursors with therapeutic potential. Philos Trans R Soc Lond B Biol Sci. 2008;363:185–98. doi: 10.1098/rstb.2006.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKenzie IA, Biernaskie J, Toma JG, Midha R, Miller FD. Skin-derived precursors generate myelinating Schwann cells for the injured and dysmyelinated nervous system. J Neurosci. 2006;26:6651–60. doi: 10.1523/JNEUROSCI.1007-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Toma JG, Akhavan M, Fernandes KJ, Barnabé-Heider F, Sadikot A, Kaplan DR, et al. Isolation of multipotent adult stem cells from the dermis of mammalian skin. Nat Cell Biol. 2001;3:78–84. doi: 10.1038/ncb0901-778. [DOI] [PubMed] [Google Scholar]
- 45.Toma JG, McKenzie IA, Bagli D, Miller FD. Isolation and characterization of multipotent skin-derived precursors from human skin. Stem Cells. 2005;23:727–37. doi: 10.1634/stemcells.2004-0134. [DOI] [PubMed] [Google Scholar]
- 46.Fernandes KJ, Kobayashi NR, Gallagher CJ, Barnabé-Heider F, Aumont A, Kaplan DR, et al. Analysis of the neurogenic potential of multipotent skin-derived precursors. Exp Neurol. 2006;201:32–48. doi: 10.1016/j.expneurol.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 47.Fernandes KJ, Miller FD. Isolation, expansion, and differentiation of mouse skin-derived precursors. Methods Mol Biol. 2009;482:159–70. doi: 10.1007/978-1-59745-060-7_10. [DOI] [PubMed] [Google Scholar]
- 48.Zhang F, Citra F, Wang DA. Prospects of induced pluripotent stem cell technology in regenerative medicine. Tissue Eng Part B Rev. 2011;17:115–24. doi: 10.1089/ten.TEB.2010.0549. [DOI] [PubMed] [Google Scholar]
- 49.Salewski RP, Eftekharpour E, Fehlings MG. Are induced pluripotent stem cells the future of cell-based regenerative therapies for spinal cord injury? J Cell Physiol. 2010;222:515–21. doi: 10.1002/jcp.21995. [DOI] [PubMed] [Google Scholar]
- 50.Parsons XH, Teng YD, Snyder EY. Important precautions when deriving patient-specific neural elements from pluripotent cells. Cytotherapy. 2009:1–11. doi: 10.3109/14653240903180092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsuji O, Miura K, Okada Y, Fujiyoshi K, Mukaino M, Nagoshi N, et al. Therapeutic potential of appropriately evaluated safe-induced pluripotent stem cells for spinal cord injury. Proc Natl Acad Sci U S A. 2010;107:12704–9. doi: 10.1073/pnas.0910106107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao T, Zhang ZN, Rong Z, Xu Y. Immunogenicity of induced pluripotent stem cells. Nature. 2011;474:212–5. doi: 10.1038/nature10135. [DOI] [PubMed] [Google Scholar]
- 53.Hamilton LK, Truong MK, Bednarczyk MR, Aumont A, Fernandes KJ. Cellular organization of the central canal ependymal zone, a niche of latent neural stem cells in the adult mammalian spinal cord. Neuroscience. 2009;164:1044–56. doi: 10.1016/j.neuroscience.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 54.Meletis K, Barnabé-Heider F, Carlén M, Evergren E, Tomilin N, Shupliakov O, et al. Spinal cord injury reveals multilineage differentiation of ependymal cells. PLoS Biol. 2008;6:e182. doi: 10.1371/journal.pbio.0060182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hawryluk GW, Fehlings MG. The center of the spinal cord may be central to its repair. Cell Stem Cell. 2008;3:230–2. doi: 10.1016/j.stem.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 56.Yamamoto S, Yamamoto N, Kitamura T, Nakamura K, Nakafuku M. Proliferation of parenchymal neural progenitors in response to injury in the adult rat spinal cord. Exp Neurol. 2001;172:115–27. doi: 10.1006/exnr.2001.7798. [DOI] [PubMed] [Google Scholar]
- 57.Martens DJ, Seaberg RM, van der Kooy D. In vivo infusions of exogenous growth factors into the fourth ventricle of the adult mouse brain increase the proliferation of neural progenitors around the fourth ventricle and the central canal of the spinal cord. Eur J Neurosci. 2002;16:1045–57. doi: 10.1046/j.1460-9568.2002.02181.x. [DOI] [PubMed] [Google Scholar]
- 58.Martens DJ, Tropepe V, van Der Kooy D. Separate proliferation kinetics of fibroblast growth factor-responsive and epidermal growth factor-responsive neural stem cells within the embryonic forebrain germinal zone. J Neurosci. 2000;20:1085–95. doi: 10.1523/JNEUROSCI.20-03-01085.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ruff CA, Fehlings MG. Neural stem cells in regenerative medicine: bridging the gap. Panminerva Med. 2010;52:125–47. [PubMed] [Google Scholar]
- 60.Zhang HT, Cheng HY, Cai YQ, Ma X, Liu WP, Yan ZJ, et al. Comparison of adult neurospheres derived from different origins for treatment of rat spinal cord injury. Neurosci Lett. 2009;458:16–21. doi: 10.1016/j.neulet.2009.04.045. [DOI] [PubMed] [Google Scholar]
- 61.Mackay-Sim A, St John JA. Olfactory ensheathing cells from the nose: Clinical application in human spinal cord injuries. Exp Neurol. 2011;229:174–80. doi: 10.1016/j.expneurol.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 62.Kwon BK, Hillyer J, Tetzlaff W. Translational research in spinal cord injury: a survey of opinion from the SCI community. J Neurotrauma. 2010;27:21–33. doi: 10.1089/neu.2009.1048. [DOI] [PubMed] [Google Scholar]
- 63.Kwon BK, Sekhon LH, Fehlings Mg. Emerging repair, regeneration, and translational research advances for spinal cord injury. Spine (Phila Pa 1976) 2010;35(21 Suppl):S263–70. doi: 10.1097/BRS.0b013e3181f3286d. [DOI] [PubMed] [Google Scholar]
- 64.Gensel JC, Donnelly DJ, Popovich PG. Spinal cord injury therapies in humans: An overview of current clinical trials and their potential effects on intrinsic CNS macrophages. Expert Opin Ther Targets. 2011;15:505–18. doi: 10.1517/14728222.2011.553605. [DOI] [PubMed] [Google Scholar]
- 65.Atkins H, Freedman M. Immune ablation followed by autologous hematopoietic stem cell transplantation for the treatment of poor prognosis multiple sclerosis. Methods Mol Biol. 2009;549:231–46. doi: 10.1007/978-1-60327-931-4_16. [DOI] [PubMed] [Google Scholar]
- 66.Freedman MS, Bar-Or A, Atkins HL, Karussis D, Frassoni F, Lazarus H, et al. The therapeutic potential of mesenchymal stem cell transplantation as a treatment for multiple sclerosis: Consensus report of the International MSCT Study Group. Mult Scler. 2010;16:503–10. doi: 10.1177/1352458509359727. [DOI] [PubMed] [Google Scholar]
- 67.Lu P, Blesch A, Tuszynski MH. Induction of bone marrow stromal cells to neurons: differentiation, transdifferentiation, or artifact? J Neurosci Res. 2004;77:174–91. doi: 10.1002/jnr.20148. [DOI] [PubMed] [Google Scholar]
- 68.Novikova LN, Brohlin M, Kingham PJ, Novikov LN, Wiberg M. Neuroprotective and growth-promoting effects of bone marrow stromal cells after cervical spinal cord injury in adult rats. Cytotherapy. 2011;13:873–87. doi: 10.3109/14653249.2011.574116. [DOI] [PubMed] [Google Scholar]
- 69.Lu P, Jones LL, Tuszynski MH. Axon regeneration through scars and into sites of chronic spinal cord injury. Exp Neurol. 2007;203:8–21. doi: 10.1016/j.expneurol.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 70.Urdzikova L, Jendelová P, Glogarová K, Burian M, Hájek M, Syková E. Transplantation of bone marrow stem cells as well as mobilization by granulocyte-colony stimulating factor promotes recovery after spinal cord injury in rats. J Neurotrauma. 2006;23:1379–91. doi: 10.1089/neu.2006.23.1379. [DOI] [PubMed] [Google Scholar]
- 71.Ohta M, Suzuki Y, Noda T, Ejiri Y, Dezawa M, Kataoka K, et al. Bone marrow stromal cells infused into the cerebrospinal fluid promote functional recovery of the injured rat spinal cord with reduced cavity formation. Exp Neurol. 2004;187:266–78. doi: 10.1016/j.expneurol.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 72.Fan L, DU F, Cheng BC, Peng H, Liu SQ. Migration and distribution of bone marrow stromal cells in injured spinal cord with different transplantation techniques. Chin J Traumatol. 2008;11:94–7. doi: 10.1016/s1008-1275(08)60020-6. [DOI] [PubMed] [Google Scholar]
- 73.Zurita M, Vaquero J. Functional recovery in chronic paraplegia after bone marrow stromal cells transplantation. Neuroreport. 2004;15:1105–8. doi: 10.1097/00001756-200405190-00004. [DOI] [PubMed] [Google Scholar]
- 74.Deng YB, Liu XG, Liu ZG, Liu XL, Liu Y, Zhou GQ. Implantation of BM mesenchymal stem cells into injured spinal cord elicits de novo neurogenesis and functional recovery: evidence from a study in rhesus monkeys. Cytotherapy. 2006;8:210–4. doi: 10.1080/14653240600760808. [DOI] [PubMed] [Google Scholar]
- 75.Kim MS, Kang KN, Lee JY, Kim da Y, Lee BN, Ahn HH, et al. Regeneration of completely transected spinal cord using scaffold of poly (D,L-lactide-co-glycolide)/small intestinal submucosa seeded with rat bone marrow stem cells. Tissue Eng Part A. 2011;17:2143–52. doi: 10.1089/ten.TEA.2011.0122. [DOI] [PubMed] [Google Scholar]
- 76.Okada S, Ishii K, Yamane J, Iwanami A, Ikegami T, Katoh H, et al. In vivo imaging of engrafted neural stem cells: Its application in evaluating the optimal timing of transplantation for spinal cord injury. Faseb J. 2005;19:1839–41. doi: 10.1096/fj.05-4082fje. [DOI] [PubMed] [Google Scholar]
- 77.Callera F, do Nascimento RX. Delivery of autologous bone marrow precursor cells into the spinal cord via lumbar puncture technique in patients with spinal cord injury: A preliminary safety study. Exp Hematol. 2006;34:130–1. doi: 10.1016/j.exphem.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 78.Chernykh ER, Stupak VV, Muradov GM, Sizikov MY, Shevela EY, Leplina OY, et al. Application of autologous bone marrow stem cells in the therapy of spinal cord injury patients. Bull Exp Biol Med. 2007;143:543–7. doi: 10.1007/s10517-007-0175-y. [DOI] [PubMed] [Google Scholar]
- 79.Yoon SH, Shim YS, Park YH, Chung JK, Nam JH, Kim MO, et al. Complete spinal cord injury treatment using autologous bone marrow cell transplantation and bone marrow stimulation with granulocyte macrophage-colony stimulating factor: Phase I/II clinical trial. Stem Cells. 2007;25:2066–73. doi: 10.1634/stemcells.2006-0807. [DOI] [PubMed] [Google Scholar]
- 80.Saito F, Nakatani T, Iwase M, Maeda Y, Hirakawa A, Murao Y, et al. Spinal cord injury treatment with intrathecal autologous bone marrow stromal cell transplantation: The first clinical trial case report. J Trauma. 2008;64:53–9. doi: 10.1097/TA.0b013e31815b847d. [DOI] [PubMed] [Google Scholar]
- 81.Neuhuber B, Timothy Himes B, Shumsky JS, Gallo G, Fischer I. Axon growth and recovery of function supported by human bone marrow stromal cells in the injured spinal cord exhibit donor variations. Brain Res. 2005;1035:73–85. doi: 10.1016/j.brainres.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 82.Vaquero J, Zurita M, Oya S, Santos M. Cell therapy using bone marrow stromal cells in chronic paraplegic rats: systemic or local administration? Neurosci Lett. 2006;398:129–34. doi: 10.1016/j.neulet.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 83.Zurita M, Vaquero J. Bone marrow stromal cells can achieve cure of chronic paraplegic rats: functional and morphological outcome one year after transplantation. Neurosci Lett. 2006;402:51–6. doi: 10.1016/j.neulet.2006.03.069. [DOI] [PubMed] [Google Scholar]
- 84.Zurita M, Vaquero J, Bonilla C, Santos M, De Haro J, Oya S, et al. Functional recovery of chronic paraplegic pigs after autologous transplantation of bone marrow stromal cells. Transplantation. 2008;86:845–53. doi: 10.1097/TP.0b013e318186198f. [DOI] [PubMed] [Google Scholar]
- 85.de Haro J, Zurita M, Ayllón L, Vaquero J. Detection of 111In-oxine-labeled bone marrow stromal cells after intravenous or intralesional administration in chronic paraplegic rats. Neurosci Lett. 2005;377:7–11. doi: 10.1016/j.neulet.2004.11.060. [DOI] [PubMed] [Google Scholar]
- 86.Kamada T, Koda M, Dezawa M, Anahara R, Toyama Y, Yoshinaga K, et al. Transplantation of human bone marrow stromal cell-derived Schwann cells reduces cystic cavity and promotes functional recovery after contusion injury of adult rat spinal cord. Neuropathology. 2011;31:48–58. doi: 10.1111/j.1440-1789.2010.01130.x. [DOI] [PubMed] [Google Scholar]
- 87.Kamada T, Koda M, Dezawa M, Yoshinaga K, Hashimoto M, Koshizuka S, et al. Transplantation of bone marrow stromal cell-derived Schwann cells promotes axonal regeneration and functional recovery after complete transection of adult rat spinal cord. J Neuropathol Exp Neurol. 2005;64:37–45. doi: 10.1093/jnen/64.1.37. [DOI] [PubMed] [Google Scholar]
- 88.Koda M, Kamada T, Hashimoto M, Murakami M, Shirasawa H, Sakao S, et al. Adenovirus vector-mediated ex vivo gene transfer of brain-derived neurotrophic factor to bone marrow stromal cells promotes axonal regeneration after transplantation in completely transected adult rat spinal cord. Eur Spine J. 2007;16:2206–14. doi: 10.1007/s00586-007-0499-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Koda M, Nishio Y, Kamada T, Someya Y, Okawa A, Mori C, et al. Granulocyte colony-stimulating factor (G-CSF) mobilizes bone marrow-derived cells into injured spinal cord and promotes functional recovery after compression-induced spinal cord injury in mice. Brain Res. 2007;1149:223–31. doi: 10.1016/j.brainres.2007.02.058. [DOI] [PubMed] [Google Scholar]
- 90.Draper JS, Moore HD, Ruban LN, Gokhale PJ, Andrews PW. Culture and characterization of human embryonic stem cells. Stem Cells Dev. 2004;13:325–36. doi: 10.1089/scd.2004.13.325. [DOI] [PubMed] [Google Scholar]
- 91.Draper JS, Smith K, Gokhale P, Moore HD, Maltby E, Johnson J, et al. Recurrent gain of chromosomes 17q and 12 in cultured human embryonic stem cells. Nat Biotechnol. 2004;22:53–4. doi: 10.1038/nbt922. [DOI] [PubMed] [Google Scholar]
- 92.Cloutier F, Siegenthaler MM, Nistor G, Keirstead HS. Transplantation of human embryonic stem cell-derived oligodendrocyte progenitors into rat spinal cord injuries does not cause harm. Regen Med. 2006;1:469–79. doi: 10.2217/17460751.1.4.469. [DOI] [PubMed] [Google Scholar]
- 93.Keirstead HS, Nistor G, Bernal G, Totoiu M, Cloutier F, Sharp K, et al. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants remyelinate and restore locomotion after spinal cord injury. J Neurosci. 2005;25:4694–705. doi: 10.1523/JNEUROSCI.0311-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Faulkner J, Keirstead HS. Human embryonic stem cell-derived oligodendrocyte progenitors for the treatment of spinal cord injury. Transpl Immunol. 2005;15:131–42. doi: 10.1016/j.trim.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 95.Nistor GI, Totoiu MO, Haque N, Carpenter MK, Keirstead HS. Human embryonic stem cells differentiate into oligodendrocytes in high purity and myelinate after spinal cord transplantation. Glia. 2005;49:385–96. doi: 10.1002/glia.20127. [DOI] [PubMed] [Google Scholar]
- 96.Sharp J, Frame J, Siegenthaler M, Nistor G, Keirstead HS. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants improve recovery after cervical spinal cord injury. Stem Cells. 2010;28:152–63. doi: 10.1002/stem.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bretzner F, Gilbert F, Baylis F, Brownstone RM. Target populations for first-in-human embryonic stem cell research in spinal cord injury. Cell Stem Cell. 2011;8:468–75. doi: 10.1016/j.stem.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 98.Solbakk JH, Zoloth L. The tragedy of translation: The case of “first use” in human embryonic stem cell research. Cell Stem Cell. 2011;8:479–81. doi: 10.1016/j.stem.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 99.Wirth E, 3rd, Lebkowski JS, Lebacqz K. Response to Frederic Bretzner et al. “Target populations for first-in-human embryonic stem cell research in spinal cord injury”. Cell Stem Cell. 2011;8:476–8. doi: 10.1016/j.stem.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 100.Mitsui T, Shumsky JS, Lepore AC, Murray M, Fischer I. Transplantation of neuronal and glial restricted precursors into contused spinal cord improves bladder and motor functions, decreases thermal hypersensitivity, and modifies intraspinal circuitry. J Neurosci. 2005;25:9624–36. doi: 10.1523/JNEUROSCI.2175-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bambakidis NC, Miller RH. Transplantation of oligodendrocyte precursors and sonic hedgehog results in improved function and white matter sparing in the spinal cords of adult rats after contusion. Spine J. 2004;4:16–26. doi: 10.1016/j.spinee.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 102.Lee KH, Yoon DH, Park YG, Lee BH. Effects of glial transplantation on functional recovery following acute spinal cord injury. J Neurotrauma. 2005;22:575–89. doi: 10.1089/neu.2005.22.575. [DOI] [PubMed] [Google Scholar]
- 103.Enzmann GU, Benton RL, Woock JP, Howard RM, Tsoulfas P, Whittemore SR. Consequences of noggin expression by neural stem, glial, and neuronal precursor cells engrafted into the injured spinal cord. Exp Neurol. 2005;195:293–304. doi: 10.1016/j.expneurol.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 104.Han SS, Liu Y, Tyler-Polsz C, Rao MS, Fischer I. Transplantation of glial-restricted precursor cells into the adult spinal cord: survival, glial-specific differentiation, and preferential migration in white matter. Glia. 2004;45:1–16. doi: 10.1002/glia.10282. [DOI] [PubMed] [Google Scholar]
- 105.Hill CE, Proschel C, Noble M, Mayer-Proschel M, Gensel JC, Beattie MS, et al. Acute transplantation of glial-restricted precursor cells into spinal cord contusion injuries: survival, differentiation, and effects on lesion environment and axonal regeneration. Exp Neurol. 2004;190:289–310. doi: 10.1016/j.expneurol.2004.05.043. [DOI] [PubMed] [Google Scholar]
- 106.Cao Q, Xu XM, Devries WH, Enzmann GU, Ping P, Tsoulfas P, et al. Functional recovery in traumatic spinal cord injury after transplantation of multineurotrophin-expressing glial-restricted precursor cells. J Neurosci. 2005;25:6947–57. doi: 10.1523/JNEUROSCI.1065-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Iwanami A, Kaneko S, Nakamura M, Kanemura Y, Mori H, Kobayashi S, et al. Transplantation of human neural stem cells for spinal cord injury in primates. J Neurosci Res. 2005;80:182–90. doi: 10.1002/jnr.20436. [DOI] [PubMed] [Google Scholar]
- 108.Iwanami A, Yamane J, Katoh H, Nakamura M, Momoshima S, Ishii H, et al. Establishment of graded spinal cord injury model in a nonhuman primate: The common marmoset. J Neurosci Res. 2005;80:172–81. doi: 10.1002/jnr.20435. [DOI] [PubMed] [Google Scholar]
- 109.Yamane J, Nakamura M, Iwanami A, Sakaguchi M, Katoh H, Yamada M, et al. Transplantation of galectin-1-expressing human neural stem cells into the injured spinal cord of adult common marmosets. J Neurosci Res. 2010;88:1394–405. doi: 10.1002/jnr.22322. [DOI] [PubMed] [Google Scholar]
- 110.Cummings BJ, Uchida N, Tamaki SJ, Salazar DL, Hooshmand M, Summers R, et al. Human neural stem cells differentiate and promote locomotor recovery in spinal cord-injured mice. Proc Natl Acad Sci U S A. 2005;102:14069–74. doi: 10.1073/pnas.0507063102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Salazar DL, Uchida N, Hamers FP, Cummings BJ, Anderson AJ. Human neural stem cells differentiate and promote locomotor recovery in an early chronic spinal cord injury NOD-scid mouse model. PLoS One. 2010;5:e12272. doi: 10.1371/journal.pone.0012272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hooshmand MJ, Sontag CJ, Uchida N, Tamaki S, Anderson AJ, Cummings BJ. Analysis of host-mediated repair mechanisms after human CNS-stem cell transplantation for spinal cord injury: Correlation of engraftment with recovery. PLoS One. 2009;4:e5871. doi: 10.1371/journal.pone.0005871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cummings BJ, Uchida N, Tamaki SJ, Anderson AJ. Human neural stem cell differentiation following transplantation into spinal cord injured mice: Association with recovery of locomotor function. Neurol Res. 2006;28:474–81. doi: 10.1179/016164106X115116. [DOI] [PubMed] [Google Scholar]


