Abstract
Background:
There are a few studies reporting the long term outcome of conservatively treated acetabular fractures. The present study aims to evaluate the quality of reduction, and radiological and functional outcome in displaced acetabular fractures treated conservatively.
Materials and Methods:
Sixty-nine patients (55 men and 14 women) with 71 displaced acetabular fractures (mean age 38.6 years) managed conservatively were retrospectively evaluated. There were 11 posterior wall, 5 posterior column, 6 anterior column, 13 transverse, 2 posterior column with posterior wall, 9 transverse with posterior wall, 6 T-shaped, 1 anterior column with posterior hemi-transverse, and 18 both-column fractures. The follow-up radiographs were graded according to the criteria developed by Matta J. Functional outcome was assessed using Harris hip score and Merle d’Aubigne and Postel score at final followup. Average follow-up was 4.34 years (range 2–11 years).
Results:
Patients with congruent reduction (n=45) had good or excellent functional outcome. Radiologic outcome in incongruent reduction (n=26) was good or excellent in 6 and fair or poor in 20 hips. The functional outcome in patients with incongruent reduction was good or excellent in 16 and satisfactory or poor in 10 hips. Good to excellent radiologic and functional outcome was achieved in all patients with posterior wall fractures including four having more than 50% of broken wall. Good to excellent functional outcome was observed in 88.8% of both-column fractures with secondary congruence despite medial subluxation.
Conclusions:
Nonoperative treatment of acetabular fractures can give good radiological and functional outcome in congruent reduction. Posterior wall fractures with a congruous joint without subluxation on computed tomography axial section, posterior column, anterior column, infratectal transverse or T-shaped, and both-column fractures may be managed conservatively. Small osteochondral fragments in the cotyloid fossa or non–weight-bearing part of the hip with a congruous joint do not seem to adversely affect the functional outcome. Displaced transverse fractures with “V” sign may require operative treatment.
Keywords: Acetabulum fracture, anterior column fractures, posterior column fractures, conservative treatment
INTRODUCTION
The operative treatment of acetabular fractures is technically challenging. The surgical approaches and reduction techniques must be thoroughly understood to properly manage this three-dimensional problem.1 The complicated anatomy of the acetabular region, frequent severe associated injuries, and long-term complications, all contribute to management difficulties.1 Displaced fractures of the acetabulum are best treated with anatomical reduction and rigid internal fixation.2–6 Good to excellent functional outcomes have been reported in 71–88% patients after operative management of acetabular fractures.2,3,5,7–10 The type of fracture and the quality of reduction influences on the functional outcome.5,10–12 However Ochs et al reported that despite changes in the chosen approaches and an increased surgical frequency, the operative treatment of the last 15 years did not lead to an increased reduction quality.13
Conservative treatment continues to be the mainstay of treatment in most centers in the developing countries. Lack of infrastructure, non-availability of skilled services, delayed referrals from peripheral units because of associated injuries, economic constraints, patient's unwillingness to undergo surgery often make the conservative treatment inevitable.14 Patients may even not be able to undergo the complete supervised conservative treatment at times because of reasons beyond surgeon's control. There are several studies on the outcome of operative management of acetabular fractures.2,3,7–12 However, only a few studies have reported the long-term outcome of acetabular fractures managed conservatively.14–18 Hence, we conducted a retrospective study to evaluate the radiologic and functional outcome of patients with displaced acetabular fractures, who were treated conservatively on traction.
MATERIALS AND METHODS
This retrospective study involves 318 patients of acetabular fractures treated between 1997 and 2007. Of these patients, 232 were treated nonoperatively and 86 operatively. Records were scrutinized for all those patients admitted with the diagnosis of acetabular fractures who were managed conservatively at author's institute. The radiographs and computed tomography (CT) scan of the patients (if available) were studied as per the classification of Judet et al. The patients involving sacro-iliac joint dislocation or associated pelvic injury were excluded from the study. The inclusion criteria of the study were displaced acetabular fracture with a minimum follow-up of 2 years. A fracture was considered displaced if any of the radiographs including Judet views showed more than 3 mm intra-articular displacement (either a step or widening of fracture). From the 232 patients treated conservatively, 102 had displaced acetabular fractures. Out of 102 patients, 7 were found to have died and 26 could not be traced. Therefore, 69 patients with 71 displaced acetabular fractures fulfilled the inclusion criteria of the study. 2 patients had bilateral acetabular fractures. The patients were treated conservatively for reasons beyond surgeons control despite fractures being displaced, i.e. severe comminution, osteoporosis, associated abdominal, head and chest injury, local soft tissue problem, medical contraindications, patient's unwillingness for surgery and occasional non-availability of skilled surgeons. The treatment protocol of nonoperative treatment for the acetabular fractures at the institute involved initial closed reduction maneuvers under sedation/anesthesia followed by skeletal (longitudinal and/or lateral) traction. Most commonly used closed reduction maneuvers included reduction of posterior dislocation by Stimson/Bigelow's methods and lateral traction in patients with central dislocation under anesthesia. Longitudinal traction was given through upper tibial or distal femoral Steinmann pin. Lateral traction was applied with Schanz pin through upper femur just below greater trochanter. Skeletal traction was given for 6–8 weeks with weights equivalent to 10–20% of body weight of the patient. This was followed by touch toe non-weight bearing for 3–4 weeks and full weight bearing after 12–16 weeks. There were 55 men and 14 women with an average age of 38.6 years (range 20–65 years). The patients presented to the author's institute at 6.9 days (range 1–16 days) after injury. The right hip was involved in 36 patients and the left hip in 35 patients. Fifty-one patients (74%) suffered injuries in road traffic accidents and 18 (26%) patients had fall from height. Four patients had associated head injury, 3 had visceral, 3 had chest injury and 16 patients had associated injuries to the upper and lower extremities. The mode of injury, the type and duration of traction, were inquired and confirmed from the patients and noted. The complications, if any, of non-operative treatment, e.g. bed sore, lateral popliteal nerve palsy, joint stiffness, pin site infection, deep vein thrombosis, were also noted. All clinical data retrieved from old records were further confirmed from the patients directly at final follow-up.
Follow-up radiographs of the affected hip including the anteroposterior, iliac, and obturator views were assessed. Patients were subjected to CT scan examination where possible at the time of final assessment. There were 11 posterior wall, 5 posterior column, 6 anterior column, 13 transverse, 2 posterior column with posterior wall, 9 transverse with posterior wall, 6 T-shaped, 1 anterior column with posterior hemi-transverse, and 18 both-column fractures. One patient had sciatic nerve palsy. Six patients had intra-articular bony fragments. Sixty-one patients were treated with skeletal traction through upper tibial pin. Five patients (of both-column fractures with medial subluxation of femoral head) received additional lateral traction through trochanteric pin. Six patients were treated with skin traction alone Two patients did not receive any type of treatment. The average period of traction was 5.9 weeks (range 4–10 weeks). Average period of follow-up was 4.34 years (range 2–11 years). Forty-one patients (59%) had follow-up of 5 years or more.
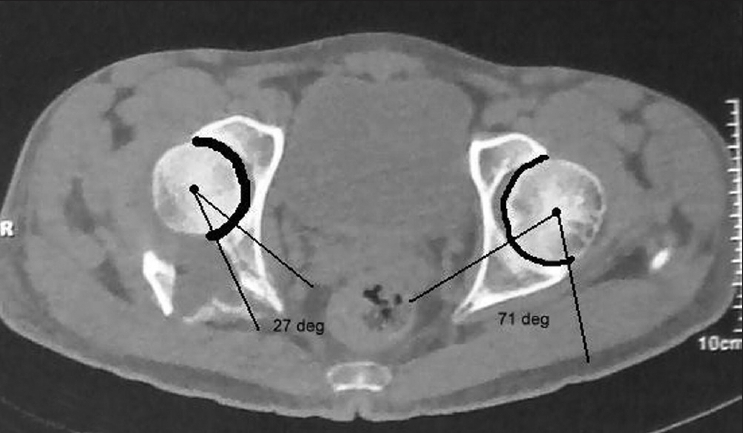
Roof arc angle measurements were done as described by Matta et al.19 to quantify the intact acetabular weight-bearing dome (WBD). The roof arc angles were not measured in posterior wall fractures and both-column fractures. Measurements of the percentage of remaining posterior acetabulum on CT scan in posterior wall fractures of acetabulum were evaluated according to the criteria of Calkins et al.20 Congruent reduction was defined as presence of parallelism between joint surfaces.
The final follow-up radiographs were graded according to the criteria developed by Matta.2 Excellent denotes a normal-appearing hip joint, good as mild changes with minimal sclerosis and joint narrowing, fair indicates intermediate changes with moderate sclerosis and joint narrowing (<50%), and poor signifies advanced changes.2 Functional outcome was assessed using Harris hip score and Merle d’Aubigne and Postel score.21
The study was conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2000.
The Fisher's exact test (two-tailed) for categorical data and Student's t-test (unpaired two-tailed) for continuous data were used for statistical analysis. Statistical significance was set at a P-value of <0.05. For the purpose of statistical analysis, the clinical outcome scores (Merle d’Aubigne and Postel score) and radiologic outcomes were defined as excellent or good, and fair or poor.
RESULTS
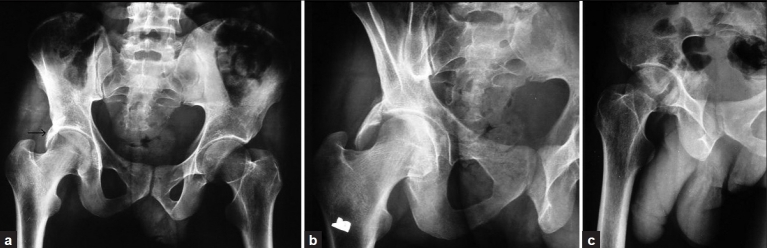
There were 11 cases of posterior wall fractures, all associated with posterior dislocation of hip which were reduced within 24 hours of injury. Reduction was congruent in all patients. The followup CT scan was available in 6 of 11 patients. Four patients demonstrated osteochondral fragments in the region of the cotyloid fossa, three of these had lateral subluxation of the head of the femur [Figure 1]. However, none of these patients had posterior subluxation. In four patients, the posterior wall fragment was displaced postero-superiorly, presenting as “cap sign” with a congruent joint [Figure 2A–D]. All the four patients had more than 50% of the posterior wall broken as assessed on CT measurements20 (range 56–68.5%) [Figure 2].
Figure 1.
Axial CT section shows posterior wall fracture and intra-articular osteochondral fragment in cotyloid fossa. The patient had good functional outcome according to the Merle d’Aubigne and Postel score
Figure 2A.
(a) Anteroposterior radiograph shows broken posterior wall fragment of right acetabulum seated over the head of femur like a “cap” (black arrow). The joint is congruous. (b) Obturator and (c) oblique iliac radiographs also show congruous reduction between the head of femur and weight-bearing dome of acetabulum
Figure 2D.
(a) Anteroposterior and (b) obturator radiographs of the same patient at 3 years followup shows good radiological outcome
Figure 2B.
Axial CT section shows more than 50% of broken posterior wall
Figure 2C.

3-D CT reconstruction shows displaced comminuted posterior wall fragments covering the femoral head posteriorly and superiorly in a patient with more than 50% of broken posterior wall
In all the patients, the displaced posterior wall fragments covered the femoral head posteriorly on coronal sections as well as 3-D reconstruction [Figure 2]. The fracture gap showed new bone formation and fibrous tissue on axial CT examination [Figure 2]. At final follow-up, the radiologic was graded as excellent in eight and good in three patients. Functional outcome was assessed as excellent using Harris hip score; and good to excellent using Merle d’Aubigne and Postel score in all patients.
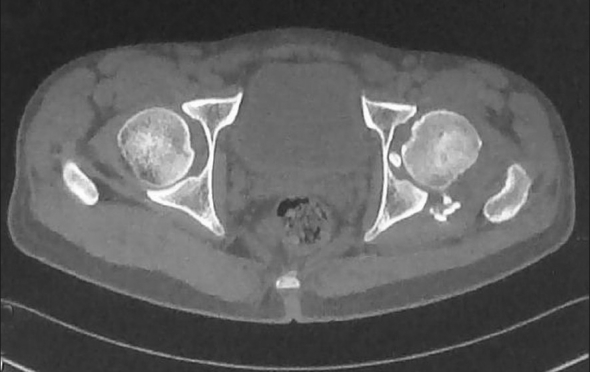
There were 13 cases of transverse fracture. Six patients were classified as transtectal fractures, two as juxtatectal and five as infratectal fractures. An average medial roof arc of 15.6°, anterior roof arc of 11.6° and posterior roof arc of 10.4° were noted in transtectal transverse fractures, indicating inadequate WBD in these patients. One patient of transtectal transverse fractures had congruent reduction with good radiologic outcome and excellent functional outcome. Five patients with transtectal transverse fractures had incongruent reduction. The WBD and head of femur formed a “V” with its apex medially in these five transtectal fractures with incongruent reduction constituting an area of stress concentration at the apex of the V [Figure 3a–c]. The radiologic outcome in these five transtectal transverse fractures was graded as good in one, fair in one and poor in three patients. Functional outcome was assessed as good in one patient and satisfactory or poor in four patients using Merle d’Aubigne and Postel score. Out of two patients, one with juxtatectal transverse fracture had congruent reduction. An average medial roof arc of 25°, anterior roof arc of 18.3° and posterior roof arc of 18.3° were observed in juxtatectal fractures, indicating inadequate WBD in these two patients. The radiologic outcome was graded as good in one and fair in another patient. Functional outcome was assessed as good in both patients using both scores. Four of the five patients with infratectal transverse fractures had congruent reduction. An average medial roof arc of 67.3°, anterior roof arc of 72.6° and posterior roof arc of 76.6° were noted in infratectal transverse fracture. The radiologic outcome was graded as excellent in two patients, good in two patients and fair in one patient. Functional outcome was assessed as excellent using Harris hip score, and good to excellent using Merle d’Aubigne and Postel score in these patients.
Figure 3.

(a) Anteroposterior radiograph of the pelvis of a 45-year-old female shows “V” sign on right acetabulum. The apex is formed medially between the weight-bearing dome and head of femur constituting an area of stress concentration. (b) Skeletal traction failed to reduce the transtectal fracture with V sign as seen in anteroposterior X-rays. (c) Follow-up anteroposterior radiograph shows poor radiological outcome and the patient had fair functional outcome
There were nine cases of transverse with posterior wall fracture. Three patients were associated with posterior hip dislocation which was reduced within 6 hours. Reduction was congruent in seven patients. The radiologic outcome was graded as good in six and fair in one patient; and functional outcome was graded as good to excellent in these seven patients using both scores. Two patients had incongruent reduction and one patient exhibited V sign on anteroposterior radiograph. Both the patients had transtectal transverse with posterior wall fracture and persistent subluxation of head of femur. The radiologic outcome was graded as poor and functional assessment was graded as fair in both patients using Harris hip score and satisfactory in both patients using Merle d’Aubigne and Postel score. Two patients had osteochondral intra-articular fragments in the region of cotyloid fossa; however, joint was congruent in WBD and functional outcome was assessed as excellent. In two patients, the posterior wall fragment was displaced postero-superiorly presenting as “cap sign” but with a congruent joint.
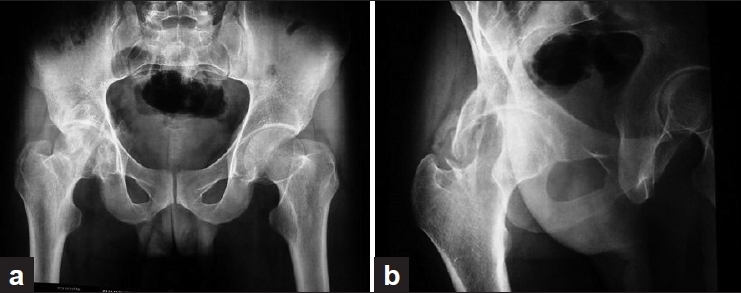
There were 18 cases of both-column fractures. Joint was congruent in seven patients; radiologic outcome was graded as excellent in one, good in five and fair in one patient. Functional outcome was assessed as good to excellent in all seven patients using both scores. Eleven patients had incongruent reduction. Radiologic outcome was excellent in one, good in four and fair in six patients. Functional assessment was good in nine and satisfactory in two patients using Merle d’Aubigne and Postel score. Function was good to excellent in six patients who had persistent medial subluxation of head of femur with fracture lines extending into the WBD. Patients with medial subluxation of head of femur had incongruent reduction; however, these patients developed secondary congruence later on follow-up. Three patients showed heterotopic ossification [Figure 4a–c].
Figure 4.

(a) Anteroposterior, (b) obturator and (c) oblique iliac radiographs of both-column fracture shows medial subluxation of head of femur with secondary congruence. The patient had good functional outcome in spite of heterotopic bone formation
All patients with posterior column (n=5) fractures had congruent reduction and good to excellent radiologic and functional outcome. There were six patients with anterior column fracture. Four patients had congruent reduction and had good to excellent radiologic and functional outcome. Two patients had incongruent reduction and had fair radiologic and good to excellent functional outcome.
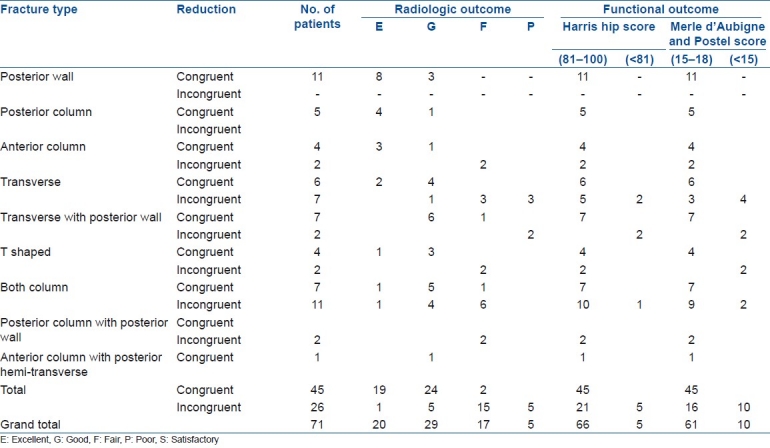
There were six patients with T-shaped fractures. Four patients had congruent reduction and good to excellent radiologic and functional outcome. Two patients had incongruent reduction and had fair radiologic and poor functional outcome using Merle d’Aubigne and Postel score. Two patients of posterior column with posterior wall fractures had incongruent reduction and fair radiologic and good functional outcome. One patient of anterior column with posterior hemi-transverse fracture had congruent reduction with good radiologic and functional outcome [Table 1].
Table 1.
Quality of reduction, radiologic and functional outcome in fractures of acetabulum
Two patients had bilateral fractures occurring as separate event. One patient initially sustained fracture posterior column with posterior wall on right side and two years later sustained T-shaped fracture on left side. Both hips had incongruent reduction with fair radiologic outcome. Functional outcome was graded as good on right side and fair on left side. Another patient had bilateral transverse fracture. One hip in this patient had congruent reduction with good radiologic and functional outcome. The contralateral hip had incongruent reduction with poor radiologic and fair functional outcome.
Good or excellent radiological outcome was achieved in 43 of 45 hips with congruent reduction in comparison to 6 of 26 hips with incongruent reduction in our study (statistically significant, P < 0.0001, Fisher's exact test). Good or excellent functional outcome was achieved in all hips (n = 45) with congruent reduction in comparison to 16 of 26 hips with incongruent reduction in our study using Merle d’Aubigne and Postel score (statistically significant, P < 0.0001, Fisher's exact test). Mean Merle d’Aubigne and Postel score was 16.64 (range 15–18; SD 1.17) in patients with congruent reduction in comparison to 14.88 (range 11–18; SD 1.63) in patients with incongruent reduction (statistically significant, P < 0.0001, Student's t-test). These results emphasize the importance of congruent reduction for achieving good functional outcome.
WBD was adequate in 26 hips of whom radiologic outcome was good or excellent in 21 (had congruent reduction) and fair in 5 hips (had incongruent reduction), and functional outcome was good or excellent in 24 and fair in 2 hips. WBD was inadequate in 16 hips of whom radiologic outcome was good in 6, fair in 5 and poor in 5 hips, and functional outcome was good or excellent in 10 and fair or poor in 6 hips [Table 2].
Table 2.
The functional outcome (according to Merle d’Aubigne and Postel score) in relation to congruency and involvement of weight-bearing dome

Good or excellent functional outcome was achieved in 24 of 26 hips with adequate WBD in comparison to 10 of 16 hips with inadequate WBD in our study using Merle d’Aubigne and Postel score (statistically significant, P = 0.037, Fisher's exact test). Mean Merle d’Aubigne and Postel score was 16.35 (range 12–18; SD 1.62) in patients with adequate WBD in comparison to 15 (range 11–18; SD 1.71) in patients with inadequate WBD (statistically significant, P = 0.014, Student's t-test). These results indicate that involvement of WBD decreases the functional outcome scores.
Overall, the radiologic outcome was graded as excellent in 20 (28.1%), good in 29 (40.8%), fair in 17 (23.9%) and poor in 5 (7%) hips. The functional outcome according to Merle d’Aubigne and Postel criteria was assessed as good (15–17 points) or excellent (18 points) in 61 patients (85.9%) and satisfactory (12–14 points) or poor (<12 points) in 10 hips (14.1%). Satisfactory or poor functions included four displaced transverse fractures, two both-column, two T-shaped and two transverse with posterior wall fractures [Table 3].
Table 3.
Clinical details of 71 fractures of acetabulum

Six patients had avascular necrosis of head of femur. Five patients developed pin site infection which was treated with curettage and antiseptic dressing, two had knee joint stiffness, one patient developed bed sore and another one had permanent lateral popliteal nerve palsy which was treated with tendon transfers after 1 year.
DISCUSSION
Displaced fractures of the acetabulum are best treated with anatomical reduction and rigid internal fixation.2–6 In spite of advances made in the operative management, conservative treatment is being followed in most of the centers in developing countries. The present study is aimed to evaluate quality of reduction, and radiologic and functional outcome in patients of displaced acetabular fractures managed conservatively.
All the patients with posterior wall fractures (n=11) had congruent reduction and good to excellent radiologic and functional outcome. Four patients had more than 50% of broken posterior wall with congruous joint. Epstein advocated conservative treatment for patients who have a fracture dislocation of the hip with a so-called insignificant acetabular fragment, but he did not specify what constituted an insignificant fragment.22 Posterior wall fractures involving more than 50% of wall are considered unstable,23,24 and therefore require osteosynthesis. However, we are of the opinion that if the joint is congruent, femoral head is well contained in the socket of the hip and not subluxating on CT examination, and head of femur is well covered with displaced posterior wall fragment on 3D reconstruction, conservative treatment may be considered even if more than 50% of the posterior wall is broken.
Congruent reduction was achieved in 20 of 22 (90.9%) patients with single column or single wall fracture, with good to excellent results in all patients in the present series. Similar findings have been reported in various studies on conservative treatment.14,16,25 The fracture line is hardly ever located on the weight-bearing surface of the acetabulum and the post-traumatic arthrosis is seldom found.14,16,25 Lovric et al. prefer operative treatment in anterior column fractures.26
Good functional outcome was observed in patients with intra-articular osteochondral fragments located in the cotyloid fossa or in the inferior portion of the hip in six patients. The bony or cartilaginous fragments in the joint are considered indications for surgery.27,28 Rosenthal and Coker concluded in their study that the presence of intra-articular bone fragments does not necessarily indicate open reduction unless the fragments are trapped in the weight-bearing area.29 The present study highlights that small osteochondral fragments in the cotyloid fossa or non–weight-bearing part in a congruous joint do not adversely affect the functional outcome.
We had good to excellent functional outcome in 88.8% of both-column fractures even though medial subluxation was seen in six cases. Tipton et al. reported good to excellent functional outcome in 58.4% patients.18 We believe that secondary congruence is achieved even though femoral head remains subluxated medially. Sen and Veerappa observed good functional outcomes in patients with central fracture dislocations where fracture reduction could be achieved.14 Displaced both-column fractures with secondary congruence gave better results than other displaced fractures.4,30
The V sign is formed due to (i) intimate contact of the head of the femur with the impacted WBD and (ii) tilting of the part of WBD to form an area of stress concentration on the head of the femur. The average medial, anterior and posterior roof arc measurements were 15.6°, 11.6° and 10.4°, respectively, in these patients. The study reveals that traction failed to reduce such a transtectal fracture showing the V sign [Figure 3b and c]. The identification of V sign on anteroposterior radiograph of pelvis is quite simple and does not require exact measurements of roof arc. V sign was observed in 6 of 10 transtectal (transverse, T-shaped; and transverse with posterior wall) fractures and 5 of these had poor or fair functional outcome. We, therefore, believe that the presence of V sign is an indication for operative management to achieve a congruous joint. Matta et al. depicted marked reduction in contact area between the femoral head and acetabulum in a diagram.30 Operative management is advised in all acetabular fractures involving WBD or with insufficient roof arc.4,17,19,27 Weise et al. observed that the larger the intact roof arc, the better the prognosis.31 Good to excellent functional outcomes were achieved in 62.5% fractures despite involvement of WBD in the present series. Heeg et al. observed good to functional outcome in 47.3% fractures involving WBD.15 Good clinicoradiologic results are expected in fractures involving WBD, but with adequate or congruent fracture reduction.14,15 Lovric et al. preferred conservative treatment in transverse fractures.26 However, operative treatment has been recommended in high or displaced transverse fractures.15,25,30
Congruent reduction was achieved in 63.3% of fractures, which is comparable to findings (56.2–80.7%) reported in the literature.14,15 Good or excellent radiologic outcome was achieved in 95.5% of patients having congruent reduction in comparison to 23% of patients with incongruent reduction in our study (statistically significant). Similarly, good or excellent radiologic outcome was reported in 77.8–100% of patients with congruent reduction in other studies.14,15 Good or excellent functional outcome was achieved in all patients with congruent reduction in comparison to 61.5% patients with incongruent reduction in our study using Merle d’Aubigne and Postel score (statistically significant). Similarly, good or excellent functional outcome was reported in 83.3–100% of the conservatively treated patients with congruent reduction in other studies.1,14,15 These results emphasize that good functional outcome can be achieved in displaced acetabular fractures managed conservatively if congruent reduction could be achieved. The functional outcome was fair or poor in 38.4% patients with incongruent reduction using Merle d’Aubigne and Postel score as compared to 78.5–81.8% reported in other studies.14,15 The functional outcome in patients with incongruent reduction seems better because the number of both-column fractures achieving secondary congruence was more in our series.
Functional outcome after operative treatment in fractures of more than 3 weeks duration was reported as fair or poor in 38.4–40.6% patients.32,33 Despite changes in the chosen approaches and an increased surgical frequency, the operative treatment of the last 15 years did not lead to an increased reduction quality.13 Conservative treatment also avoids complications related to operative treatment, such as iatrogenic nerve palsies, wound infections, deep vein thrombosis/pulmonary embolism. Arthrosis, necrosis of the femoral head and heterotopic ossification tend to decline the outcome of acetabular fractures despite good fracture reduction achieved after surgery.7,34 Overall, good to excellent functional result was achieved in 85.9% patients in the present series. Therefore, the outcome of conservatively managed fractures is not bleak and operative treatment should be considered when absolute indications are there.
In conclusion a reasonable outcome can still be achieved in fractures with congruent reduction treated conservatively. Posterior wall fractures with a congruous joint without subluxation on CT axial section, posterior column, anterior column, infratectal transverse or T-shaped, and both-column fractures may be managed conservatively and good or excellent functional outcome can be expected in most of the patients. Small osteochondral fragments in the cotyloid fossa or non–weight-bearing part of the hip with a congruous joint do not seem to adversely affect the functional outcome. The transtectal transverse or T-shaped fractures presenting with “V” sign should be managed operatively.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Hofmann AA, Dahl CP, Wyatt RWB. Experience with acetabular fractures. J Trauma. 1984;24:750–2. doi: 10.1097/00005373-198408000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–45. [PubMed] [Google Scholar]
- 3.Moed BR, Carr SE, Watson JT. Open reduction and internal fixation of posterior wall fractures of the acetabulum. Clin Orthop Relat Res. 2000;377:57–67. doi: 10.1097/00003086-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Tornetta P., 3rd Displaced acetabular fractures: Indications for operative and nonoperative management. J Am Acad Orthop Surg. 2001;9:18–28. doi: 10.5435/00124635-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 6.Moed BR, Willson Carr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84:752–8. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Roetman B, Seybold D, Keil D, Muhr G, Mollenhoff G. Long-term results after acetabular fractures with respect to heterotopic ossifications. Zentrabl Chir. 2006;131:188–93. doi: 10.1055/s-2006-933457. [DOI] [PubMed] [Google Scholar]
- 8.Petsatodis G, Antonarakos P, Chalidis B, Papadopoulos P, Christoforidis J, Pournaras J. Surgically treated acetabular fractures via a single posterior approach with a follow-up of 2-10 years. Injury. 2007;38:334–43. doi: 10.1016/j.injury.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Ma B, Zhang Y, Zhang X. Operative management of acetabular fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2006;20:640–2. [PubMed] [Google Scholar]
- 10.Elmali N, Ertem K, Inan M, Ayan I, Denizhan Y. Clinical and radiologic results of surgically-treated acetabular fractures. Acta Orthop Traumatol Turc. 2003;37:97–101. [PubMed] [Google Scholar]
- 11.Chen HW, Zhao GS. Surgical treatment of acetabular posterior wall fractures. Zhongguo Gu Shang. 2008;21:674–5. [PubMed] [Google Scholar]
- 12.Chiu FY, Lo WH, Chen TH, Chen CM, Huang CK, Ma HL. Fractures of posterior wall of acetabulum. Arch Orthop Trauma Surg. 1996;115:273–5. doi: 10.1007/BF00439052. [DOI] [PubMed] [Google Scholar]
- 13.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, et al. Changes in the treatment of acetabular fractures over 15 years: Analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41:839–51. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Sen RK, Veerappa LA. Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma. 2009;67:155–9. doi: 10.1097/TA.0b013e31819db092. [DOI] [PubMed] [Google Scholar]
- 15.Heeg M, Oostvogel HJ, Klasen HJ. Conservative treatment of acetabular fractures: The role of the weight bearing dome and anatomic reduction in the ultimate results. J Trauma. 1987;27:555–9. [PubMed] [Google Scholar]
- 16.Heeg H, Otter N, Klasen HJ. Anterior column fractures of the column. J Bone Joint Surg Br. 1992;74:554–7. doi: 10.1302/0301-620X.74B4.1624515. [DOI] [PubMed] [Google Scholar]
- 17.Hesp WL, Goris RJ. Conservative treatment of fractures of the acetabulum.Results after longtime follow-up. Acta Chir Belg. 1988;88:27–32. [PubMed] [Google Scholar]
- 18.Tipton WW, D’ Ambrosia RD, Ryle GP. Non-operative management of central fracture-dislocations of the hip. J Bone Joint Surg Am. 1975;57:888–93. [PubMed] [Google Scholar]
- 19.Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum: a retrospective analysis. Clin Orthop Relat Res. 1986;205:230–40. [PubMed] [Google Scholar]
- 20.Calkins MS, Zych G, Latta L, Borja FJ, Mnaymneh W. Computed tomography evaluation of stability in posterior fracture dislocation of the hip. Clin Orthop Relat Res. 1988;227:152–63. [PubMed] [Google Scholar]
- 21.d’Aubigné RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–75. [PubMed] [Google Scholar]
- 22.Epstein HC. Posterior fracture-dislocations of the hip.Long-term follow-up. J Bone Joint Surg Am. 1974;56:1103–27. [PubMed] [Google Scholar]
- 23.Keith JE, Jr, Brashear HR, Jr, Guilford WB. Stability of posterior fracture-dislocations of the hip.Quantitative assessment using computed tomography. J Bone Joint Surg Am. 1988;70:711–4. [PubMed] [Google Scholar]
- 24.Vailas JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture-dislocations: Fragment size, joint capsule, and stability. J Trauma. 1989;29:1494–6. [PubMed] [Google Scholar]
- 25.Ylinen P, Sentavirta S, Slatis P. Outcome of acetabular fractures: A 7-year follow-up. J Trauma. 1989;29:19–24. doi: 10.1097/00005373-198901000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Lovric I, Jovanovic S, Leksan I, Biuk E, Kristek J, Radic R. Functional status of hip joint after surgical and conservative treatment of acetabular fracture. Coll Antropol. 2007;31:285–9. [PubMed] [Google Scholar]
- 27.de Ridder VA, de Lange S, Kingma L, Hogervorst M. Results of 75 consecutive patients with an acetabular fracture. Clin Orthop Relat Res. 1994;305:53–7. [PubMed] [Google Scholar]
- 28.Pascarella R, Maresca A, Reggiani LM, Boriani S. Intra-articular fragments in acetabular fracture-dislocation. Orthopedics. 2009;32:402. doi: 10.3928/01477447-20090511-15. [DOI] [PubMed] [Google Scholar]
- 29.Rosenthal RE, Coker WL. Posterior fracture-dislocations of the hip: An epidemiologic review. J Trauma. 1979;19:572–81. doi: 10.1097/00005373-197908000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. 1988;230:83–97. [PubMed] [Google Scholar]
- 31.Weise K, Maurer F, Schrade J. Hip dislocations and hip fractures--acetabular fractures.Indication, technique and results of conservative treatment. Orthopade. 1997;26:336–47. doi: 10.1007/PL00003389. [DOI] [PubMed] [Google Scholar]
- 32.Jing LY, Liu GY, Hu Y, Zhang F, Ruan YP, Xu RM. Operative treatment of old acetabular fractures. Zhongguo Gu Shang. 2010;23:386–8. [PubMed] [Google Scholar]
- 33.Wang MY, Wu XB, Zhu SW, Cao QY, Wu HH, Rong GW. Operative treatment of delayed acetabular fractures. Zhonghua Wai Ke Za Zhi. 2003;41:130–3. [PubMed] [Google Scholar]
- 34.Wright R, Barrett K, Christie MJ, Johnson KD. Acetabular fractures: Long-term follow-up of open reduction and internal fixation. J Orthop Trauma. 1994;8:397–403. doi: 10.1097/00005131-199410000-00005. [DOI] [PubMed] [Google Scholar]