Abstract
Background:
A number of techniques have been described to reattach the torn distal biceps tendon to the bicipital tuberosity. We report a retrospective analysis of single incision technique using an endobutton fixation in sports persons.
Materials and Methods:
The present series include nine torn distal biceps tendons in eight patients, fixed anatomically to the radial tuberosity with an endobutton by using a single incision surgical technique; seven patients had suffered the injuries during contact sports. The passage of the endobutton was facilitated by using a blunt tipped pin in order to avoid injury to the posterior interosseous nerve. The patients were evaluated by Disabilities of the Arm, Shoulder and Hand (DASH) score and Mayo elbow score.
Results:
The average age of the patients was 27.35 years (range 21–42 years). Average follow-up was 41.5 months (range 24–102 months). The final average flexion extension arc was 0°–143°, while the average pronation and supination angles were 77° (range 70°–82°) and 81° (range 78°–85°), respectively at the last followup. All the patients had a Disabilities of the Arm, Shoulder and Hand (DASH) score of 0 and a Mayo elbow score of 100 each. All the seven active sports persons were able to get back to their respective game. There was no nerve injury or any other complication.
Conclusions:
The surgical procedure used by us is a simple, safe and reproducible technique giving minimal morbidity and better cosmetic results.
Keywords: Autograft, biceps tendon, elbow, tendon repair, tendon rupture
INTRODUCTION
Rupture of the distal biceps tendon is estimated to be approximately 10% of all biceps brachii ruptures.1 Sports persons involved in competitive strength training and contact sports are more susceptible to sustain distal tendon biceps injuries.2 Although nonsurgical management is an option in sedentary patients, the treatment of complete distal biceps ruptures in active persons and athletes is primarily surgical, which is crucial to improve the strength of supination and flexion.1–6
Between anatomic repair of attaching the ruptured tendon back to the original site at radial tuberosity and nonanatomic reconstruction of attaching the ruptured tendon to the brachialis, the former is recognized to be a superior option to maximize functional upper extremity potential.7,8 Both the commonly used surgical techniques of using one incision and two incisions have been reported to have high complication rate in the range of 16–31%, which include posterior interosseous nerve injury, median nerve entrapment, radioulnar synostosis, stiffness, heterotopic ossification, etc. The former technique has been mainly blamed of having an inherent risk of causing injury to posterior interosseous nerve, while the latter technique has been reported to be having the high risk of causing radioulnar synostosis.9–15 While the controversy of ideal surgical approach for fixing the distal biceps tendon is still unresolved, the use of different methods of fixation of the torn tendon to the radial tuberosity, including the suture material with the trans-osseous tunnels, bone anchors, interference screws and endobuttons, has also been a topic of debate in the literature.7,15–21
We present a retrospective case series of 8 patients (9 elbows), wherein the torn distal biceps tendon was reattached to the radial tuberosity with an endobutton through a single surgical incision using a novel blunt tipped pin for the facilitation of the passage of the endobutton through the tunnel in the radial tuberosity in order to avoid the risk of nerve injury.
MATERIALS AND METHODS
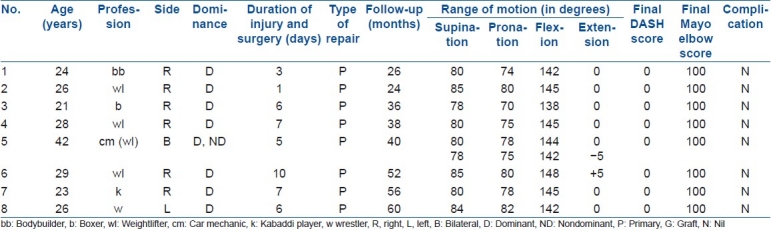
All the nine completely torn distal biceps tendons in eight patients who presented between 2000 and 2008 were included in the study [Table 1]. The data of the patients were collected from the records and all the patients were called for final assessment by the same surgeon. Two left-sided elbows (one dominant) and seven right-sided elbows (all dominant) were injured. The duration between injury and surgery was 1–10 days (average 5.6 days). All the patients were diagnosed clinically. The patients with unilateral ruptures had asymmetrical contour of the biceps muscle belly. On palpation of the biceps belly, while the patient was asked to contract the biceps, the feel of the muscle was flaccid. Hook test was positive in all the cases. Average follow-up was 41.5 months (range 24–102 months). Results were assessed by using a 30 point Disabilities of the Arm, Shoulder and Hand (DASH) score and Mayo elbow score.22,23
Table 1.
Data of eight patients with biceps rupture
Operative procedure
The patients were operated in a supine position under general anesthesia. A high tourniquet was used in all the patients. A 4–5 cm long transverse incision, 2 cm distal to the elbow crease, was used [Figure 1A (a)]. In all the cases, the retracted biceps tendon was able to be retrieved into the incision by milking maneuver over the belly of the biceps tendon from proximal to distal direction except in one patient in whom arthroscopy was used through the surgical incision to visualize and grasp the tendon that was then pulled into the incision.
Figure 1A.
(a) Transverse small surgical incision placed 2 cm distal to the elbow crease (b) Number 5 Ethibond suture passed over 5 cm length of the torn tendon and attachment of endobutton (c) Site of attachment of the torn tendon on radial tuberosity after preparation (black arrows showing leading and trailing sutures of endobutton)
Preparation of the tendon end
The free end of the torn tendon was prepared by passing number 5 synthetic polyester sutures (Ethibond, Johnson and Johnson, India) over a length of distal 5 cm. [Figure 1A (b)]. The first bite of the suture was taken at the proximal most end of the proposed suture length of the tendon. Suturing was then continued from proximal to distal direction on one side of the tendon length by using baseball sutures. At the end of the tendon, the needle was passed through the two central holes of the endobutton (4 mm × 12 mm endobutton, Smith and Nephew, India) and then suturing was continued on the other side of the tendon using the same baseball sutures from distal to proximal direction and finally tying the knot on the proximal part of the tendon near the first bite; it was ensured that there was 6 mm distance between the free end of the tendon and the endobutton to facilitate toggling of the endobutton subsequently.
Preparation of the radial tuberosity
Avoiding injury to the lateral antebrachial cutaneous nerve, the plain between the muscles of brachialis and brachioradialis was developed, which harbored the fluid-filled bicipito-radial bursa in its depth. In the recent cases of injury, a fibrous sheath in continuity of the torn tendon was sometimes identifiable along with the bursa that acted as a guide to reach the bicipital tuberosity. With careful dissection of the bursa and the fibrous sheath, the radial tuberosity was approached. Two fine Hohman spike retractors were carefully used on both the sides of the proximal radius for gentle retraction. It was ensured that the retractors were gently held by the assistant to avoid too much pressure on the retracted structures which included radial nerve, median nerve and brachial artery; the assistant was intermittently instructed to release the pressure. With the second assistant holding the forearm in as much supination as possible, thus bringing into view the site of attachment of the avulsed biceps tendon on the radial tuberosity, a 2.5 mm K wire was drilled into the middle of the proximal radius at the site of the avulsed tendon, ensuring the angle of insertion of the K wire into the proximal radius stayed at right angle in both the coronal and sagittal planes to avoid injury to the posterior interosseous nerve. A 4.5 canulated drill bit was used to drill a hole over the K wire in both the cortices of the proximal radius. A 2-mm burr was used to enlarge the near cortex of the hole in the radius to create a trough for the torn biceps tendon in the near cortex [Figure 1A (c)]. A thorough irrigation of the wound was done by using normal saline and suction to clear the wound of any bone dust.
A specially designed blunt tipped needle of 2.5 mm diameter and 20 cm length [Figure 1B (a)] was loaded with different colored leading and trailing sutures passed through the two peripheral holes of the endobutton respectively. With elbow in 90° flexion and forearm in full supination, the needle was gently passed from anterior to posterior side through the hole in the proximal radius, ensuring to stay at right angles in both the coronal as well as the sagittal Planes [Figure 1B (b)]. If a slightest resistance of soft tissue was felt to the tip of the needle between the bone and the skin, a gentle rocking movement of the needle was made to bypass the obstructing soft tissue before it was pushed just underneath the skin. As the tip of the needle tented the skin on the posterior side, a stab nick [Figure 1B(d)] was made to facilitate the passage of needle through the skin; the nick was made only in the skin at the tenting tip of the needle and was not a formal incision described for the standard two incision technique. The leading sutures of the endobutton were pulled so that the endobutton passed through the hole; acute flexion of the elbow facilitated the movement of the endobutton through the tunnel in the radius. The trailing sutures were now pulled to toggle the endobutton so that it lay on the posterior cortex of the radius. The elbow was moved through full range of motion of extension, flexion, pronation and supination to ensure the stable seating of the endobutton on the posterior radial cortex. The position of the endobutton was confirmed by using intraoperative fluoroscopy [Figure 1B (c)]. The wound was closed by using subcuticular sutures after thorough irrigation.
Figure 1B.
(a) Specially designed blunt-tipped pin (b) Passage of blunt-tipped needle loaded with sutures of endobutton through the tunnel (c) Intraoperative X-ray showing confirmation of position of endobutton (d) Final minimal surgical scar in a bodybuilder (e) Small posterior surgical nick to adjust the position of the endobutton
Postoperative regimen
The elbow was put in a posterior splint with 90° flexion at elbow in midprone position of the forearm for 2 weeks, mainly to allow soft tissue healing and reduce the inflammation and swelling. The splint was intermittently removed during the day for 3–4 times to perform a range of motion exercises as tolerated by the patient. After 2 weeks, the slab was discarded, allowing activities of daily living with prohibition of lifting of heavy weight for 6 weeks. At 6 weeks, the muscle strengthening exercises were started which were gradually increased over the period of next 2 months. At 3–4 months, sports specific exercises were started and all the patients were allowed to return to sports by the end of 5 months.
RESULTS
The mean age was 27.35 years (range 21–42 years). All the patients were males. Seven patients ruptured their tendons during contact sports: three weightlifters, one boxer, one kabaddi player (a high-impact contact sport popular in the country side), one bodybuilder and one wrestler. The eighth patient was a car mechanic but an erstwhile weightlifter had bilateral ruptures, while trying to lift out the rear wheel of his small car that was stuck in an open manhole with both the hands, and while being helped by other two co-workers who suddenly dropped the entire weight of the car on to both the hands of the patient; the patient did not have history of addiction to tobacco/alcohol/steroids.
The final average flexion extension arc was 0°–143°, while the average pronation and supination angles were 77° (range 70°–82°) and 81° (range 78°–85°), respectively. All the patients had a DASH score of 0 each and a Mayo elbow score of 100 each [Table 1]. No complication was seen in any of the patients. All the patients went back to sports. The patient with bilateral rupture, who was not into active sports anymore even preoperatively, went back to his original job of car mechanic.
DISCUSSION
Though rupture of the distal biceps tendon was earlier reported to be around 3% of all biceps tendon ruptures, it has been recently estimated to be closer to 10%.24,25 Prior to 1995, there were 53 published articles concerning the distal biceps, in contrast to more than 70 new publications on this topic over the past 3 years, reflecting an incidence trend or a possible increase in detection.1
The patients are usually able to perform unhampered activities of daily living with some weakness and fatigability of the supination movement (e.g. using a screw driver) on a long followup when treated non-surgically.1 This is the probable reason that the patients with sedentary occupations do not usually visit the specialized centers and the incidence of the injuries is under reported. The professional sportspersons do not neglect injuries, hence a higher rates of detection of the injuries. Seven of the eight patients included in our series were referred to us specifically for the surgical treatment by the sports physicians who initially provided first aid to the patients.
The asymmetrical contours of the biceps muscle bellies on the two sides and on palpation of a relatively proximally situated muscle belly of the ruptured biceps led us to diagnose it. Hook test was positive in all the cases. The sensitivity and specificity of clinical examination has earlier been reported to be 100% in comparison to 92% sensitivity and 85% specificity of magnetic resonance imaging (MRI).5,26 Furthermore, the musculoskeletal radiologist performing MRI examination on such patients ought to be aware of the fact that proper visualization of the distal biceps tendon with MRI requires a special flexed abducted supinated (FABS) position of the upper limb, which includes 90° of elbow flexion, 180° of shoulder abduction and forearm supination.27 A thorough and complete clinical examination is of utmost importance to make an early diagnosis especially in sportspersons because a delay in the diagnosis and treatment can result in loss of their sports career.28
We intended to use minimal invasive technique to the best of our ability. In one case we faced difficulty in retrieving the retracted biceps tendon through the small distal incision, we used arthroscopy through the distal incision to retrieve the tendon. Since the majority of the patients were competitive sports persons in our series, who belonged to bodybuilding, wrestling, weightlifting, etc., minimal invasive technique was supposed to give them the advantage of early functional recovery as well as cosmetic esthesis. In a comparative prospective study of the single versus double surgical incision techniques, El Hawary et al. have reported the results of the single-incision surgical technique to be superior at 1-year follow-up, but with a higher rate of complications.29 In a systematic review of distal biceps tendon repairs, Chavan et al. have reported a significantly higher rate of unsatisfactory surgical outcomes of the two incision technique in comparison to the single-incision technique, while the endobutton fixation was reported to give the best biomechanical performance in terms of stiffness and load failure.15 However, the authors reported a high rate of complication to the tune of 18% in one incision technique, with the most common complication being nerve injury that was reported in 13% of the patients.15 Taking the advantage of the higher success rate of the single incision technique and the best biomechanical strength of the endobutton, we were able to altogether avoid the complication of nerve injury in our series with the present surgical technique using a blunt tipped needle. The nick used by us on the tented skin posteriorly to facilitate the passage of the blunt tipped needle was placed only in the skin and was not a formal second incision used in the standard two incision technique for the surgical exposure of the proximal radius from the posterior side10.
Peters et al. have reported a malposition of the endobutton in three of the nine patients, but without a significant difference in the functional outcome; although ultimately they had to remove one malpositioned endobutton.30 We routinely see the position of the endobutton fluoroscopically by rotating the forearm in full supination and pronation at the end of the procedure. In one patient, we had to use an additional posterior surgical nick to adjust the position of the endobutton that was found to be lying subcutaneously on fluoroscopic examination.
We did not observe the complication of heterotopic ossification or radioulnar synostosis in any of the patients in our series. We mainly attribute this to copious irrigation of the wound with saline to wash out any bone dust generated as a result of drilling and burring of the proximal radius. Moreover, we did not dissect in the radioulnar interval at all that would predispose the formation of a radioulnar synostosis. We did not use any additional agent postoperatively to prevent the incidence of heterotopic ossification.
Both DASH scores and Mayo elbow performance score have been individually used in the literature to assess the outcome after the surgical repair of torn biceps tendon.30,31 We used both the tools in the present series and they correlated well with each other and also with the final function of the patient.
In conclusion, we feel that the single incision surgical technique used by us with a blunt tipped pin to facilitate the passage of endobutton to repair torn distal biceps tendon is a simple, safe and effective technique with excellent results.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Sutton KM, Dodds SD, Ahmad CS, Sethi PM. Surgical treatment of distal biceps rupture. J Am Acad Orthop Surg. 2010;18:139–48. doi: 10.5435/00124635-201003000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kokkalis ZT, Sotereanos DG. Biceps tendon injuries in athletes. Hand Clin. 2009;25:347–57. doi: 10.1016/j.hcl.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 3.D’Alessandro DF, Shields CL, Jr, Tibone JE, Chandler RW. Repair of distal biceps tendon ruptures in athletes. Am J Sports Med. 1993;21:114–9. doi: 10.1177/036354659302100119. [DOI] [PubMed] [Google Scholar]
- 4.Chillemi C, Marinelli M, De Cupis V. Rupture of the distal biceps brachii tendon: conservative treatment versus anatomic reinsertion-clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg. 2007;127:705–8. doi: 10.1007/s00402-007-0326-7. [DOI] [PubMed] [Google Scholar]
- 5.Miyamoto RG, Elser F, Millett PJ. Distal biceps tendon injuries. J Bone Joint Surg Am. 2010;92:2128–38. doi: 10.2106/JBJS.I.01213. [DOI] [PubMed] [Google Scholar]
- 6.Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii.Operative versus non-operative treatment. J Bone Joint Surg Am. 1985;67:414–7. [PubMed] [Google Scholar]
- 7.Greenberg JA. Endobutton repair of distal biceps tendon ruptures. J Hand Surg Am. 2009;34:1541–8. doi: 10.1016/j.jhsa.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Rantanen J, Orava S. Rupture of the distal biceps tendon.A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med. 1999;27:128–32. doi: 10.1177/03635465990270020201. [DOI] [PubMed] [Google Scholar]
- 9.Meherin JM, Kilgore ES. The treatment of ruptures of the distal biceps brachii tendon. Am J Surg. 1960;99:636–40. [Google Scholar]
- 10.Boyd HB, Anderson LD. A method for reinsertion of the distal biceps brachii tendon. J Bone Joint Surg Am. 1961;43:1041–3. [Google Scholar]
- 11.Failla JM, Amadio PC, Morrey BF, Beckenbaugh RD. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two-incision technique. Report of four cases. Clin Orthop Relat Res. 1990;253:133–6. [PubMed] [Google Scholar]
- 12.Katzman BM, Caligiuri DA, Klein DM, Gorup JM. Delayed onset of posterior interosseous nerve palsy after distal biceps tendon repair. J Shoulder Elbow Surg. 1997;6:393–5. doi: 10.1016/s1058-2746(97)90008-2. [DOI] [PubMed] [Google Scholar]
- 13.Lin KH, Leslie BM. Surgical repair of distal biceps tendon rupture complicated by median nerve entrapment.A case report. J Bone Joint Surg Am. 2001;83:741–3. doi: 10.2106/00004623-200105000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Kelly EW, Morrey BF, O’Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82:1575–81. doi: 10.2106/00004623-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: a systematic review. Am J Sports Med. 2008;36:1618–24. doi: 10.1177/0363546508321482. [DOI] [PubMed] [Google Scholar]
- 16.Berlet GC, Johnson JA, Milne AD, Patterson SD, King GJ. Distal biceps brachii tendon repair. An in vitro biomechanical study of tendon reattachment. Am J Sports Med. 1998;26:428–32. doi: 10.1177/03635465980260031501. [DOI] [PubMed] [Google Scholar]
- 17.Pereira DS, Kvitne RS, Liang M, Giacobetti FB, Ebramzadeh E. Surgical repair of distal biceps tendon ruptures: a biomechanical comparison of two techniques. Am J Sports Med. 2002;30:432–6. doi: 10.1177/03635465020300032101. 50. [DOI] [PubMed] [Google Scholar]
- 18.Lemos SE, Ebramzedeh E, Kvitne RS. A new technique: in vitro suture anchor fixation has superior yield strength to bone tunnel fixation for distal biceps tendon repair. Am J Sports Med. 2004;32:406–10. doi: 10.1177/0363546503261720. [DOI] [PubMed] [Google Scholar]
- 19.Idler CS, Montgomery WH, 3rd, Lindsey DP, Badua PA, Wynne GF, Yerby SA. Distal biceps tendon repair: a biomechanical comparison of intact tendon and 2 repair techniques. Am J Sports Med. 2006;34:968–74. doi: 10.1177/0363546505284185. [DOI] [PubMed] [Google Scholar]
- 20.Kettler M, Lunger J, Kuhn V, Mutschler W, Tingart MJ. Failure strengths in distal biceps tendon repair. Am J Sports Med. 2007;35:1544–8. doi: 10.1177/0363546507300690. [DOI] [PubMed] [Google Scholar]
- 21.Mazzocca AD, Burton KJ, Romeo AA, Santangelo S, Adams DA, Arciero RA. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35:252–8. doi: 10.1177/0363546506294854. [DOI] [PubMed] [Google Scholar]
- 22.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected].The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 23.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–74. [PubMed] [Google Scholar]
- 24.Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii: A biomechanical study. J Bone Joint Surg Am. 1985;67:418–21. [PubMed] [Google Scholar]
- 25.Safran MR, Graham SM. Distal biceps tendon ruptures: Incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–83. [PubMed] [Google Scholar]
- 26.O’Driscoll SW, Goncalves LB, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35:1865–9. doi: 10.1177/0363546507305016. [DOI] [PubMed] [Google Scholar]
- 27.Giuffr’e BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol. 2004;182:944–6. doi: 10.2214/ajr.182.4.1820944. [DOI] [PubMed] [Google Scholar]
- 28.Gupta RK, Singh D, Kansay R, Singh H. Cricket ball injury: a cause of symptomatic muscle hernia of leg. Br J Sports Med. 2008;42:1002–3. doi: 10.1136/bjsm.2007.041541. [DOI] [PubMed] [Google Scholar]
- 29.El-Hawary R, Macdermid JC, Faber KJ, Patterson SD, King GJ. Distal biceps tendon repair: comparison of surgical techniques. J Hand Surg Am. 2003;28:496–502. doi: 10.1053/jhsu.2003.50081. [DOI] [PubMed] [Google Scholar]
- 30.Peeters T, Ching-Soon NG, Jansen N, Sneyers C, Declercq G, Verstreken F. Functional outcome after repair of distal biceps tendon ruptures using the endobutton technique. J Shoulder Elbow Surg. 2009;18:283–7. doi: 10.1016/j.jse.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Karunakar MA, Cha P, Stern PJ. Distal biceps ruptures. A followup of Boyd and Anderson repair. Clin Orthop Relat Res. 1999;363:100–7. [PubMed] [Google Scholar]




