Abstract
Background:
The optimal approach to provide satisfactory decompression and minimize complications for ossification of the posterior longitudinal ligament (OPLL) involving multiple levels (3 levels or more) remains controversial. The purpose of this study was to compare the results of two surgical approaches for cervical OPLL involving multiple levels; anterior direct decompression and fixation, and posterior indirect decompression and fixation. We present a retrospective review of 56 cases followed at a single Institution.
Materials and Methods:
We compared patients of multiple levels cervical OPLL that were treated at a single institution either with anterior direct decompression and fixation or with posterior indirect decompression and fixation. The clinical records of the patients with a minimum duration of follow-up of 2 years were reviewed. The associated complications were recorded.
Results:
Fifty-six patients constitute the clinical material. 26 cases were treated by anterior corpectomy and fixation and 30 cases received posterior laminectomy and fixation. The two populations were similar. It was found that both anterior and posterior decompression and fixation can achieve satisfactory outcomes, and posterior surgery was accomplished in a shorter period of time with lesser blood loss. Although patients had comparable preoperative Japanese Orthopaedics Association (JOA) scores, those with a canal occupancy by OPLL more than 50% and managed anteriorly had better outcomes. However, for those with more severe stenosis, anterior approach was more difficult and associated with higher risks and complications. Despite its limitations in patients with high occupancy OPLLs, through the multiple level laminectomy, posterior fixation can achieve effective decompression, maintaining or restoring stability of the cervical spine, and thereby improving neural outcome and preventing the progression of OPLL.
Conclusions:
The posterior indirect decompression and fixation has now been adopted as the primary treatment for cervical OPLL involving multiple levels with the canal occupancy by OPLL <50% at our institution because this approach leads to significantly less implant failures. Those patients with the occupancy ≥50% managed with anterior approach surgeries had better outcomes, but approach was more difficult and associated with higher risk and complications.
Keywords: Anterior decompression, cervical OPLL, internal fixation, posterior decompression
INTRODUCTION
Cervical ossification of the posterior longitudinal ligament (OPLL) may compress the spinal cord and nerve roots, leading to sensory and motor dysfunction. Although the majority of patients with the condition are asymptomatic, when OPLL manifests as cervical myelopathy, non-surgical intervention is often ineffective to arrest the progression of neural deficit. It is well recognized that surgery should be performed before irreversible damage to the nervous system occurs, to avoid further deterioration of spinal cord function. However, the optimal surgical approach remains controversial.1 When planning for surgery, surgeons must take into consideration the region and extent of the OPLL, as well as the degree of canal stenosis. The surgery should achieve sufficient decompression and prevent further progression of symptoms.2
Both anterior and posterior approaches have their advantages as well as disadvantages. The anterior approach can directly relieve compression, but the procedure is more complicated and prone to an increased risk of spinal cord injury. Moreover, the anterior decompression and fusion is associated with complications including pseudoarthrosis, implant failure or movement, and symptomatic adjacent segment spondylosis, which have drawn attention in recent years.3–10 Posterior approach can also provide canal decompression, but the degree of decompression is sometimes insufficient since the ventral compression persists. Instability following laminectomy has also raised concerns.11–14 The present study was designed to compare anterior corpectomy, decompression and fixation and posterior laminectomy, decompression and fixation for treatment of cervical OPLL involving multiple levels (three levels or more), and to evaluate the factors that influence the outcome of the two approaches.
MATERIALS AND METHODS
Patient recruitment
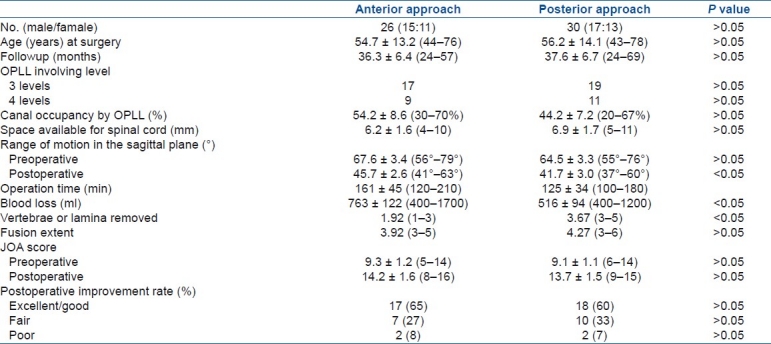
Fifty six patients who presented between January 2005 and December 2008 and met the following criteria were recruited: 1) underwent anterior or posterior surgery for cervical OPLL involving three levels or more; 2) with complete medical records and related radiographic data, including preoperative and postoperative X-rays, computed tomography (CT) and magnetic resonance imaging (MRI); 3) underwent canal decompression, fusion and internal fixation; 4) with 24 months or more of followup. Patients with spinal injuries due to trauma were excluded [Table 1]. Informed written consent was taken from all the patients.
Table 1.
Clinical details of two groups
Operative procedure
Anterior approach: The patients were placed in the supine position with the head slightly extended. The cervical spine was exposed through a standard left sided Robinson-Smith anterior approach. The anterior longitudinal ligament was exposed. A rectangular area of the ligament was resected. After the ventral annulus fibrosus was removed, a curette and a laminectomy rongeur were used to excise the vertebra. A sharp scalpel was used to cut the OPLL along the slot under direct vision. The ossified ligament was carefully resected. In case of severe adhesion of the OPLL to the dura or ossified dura, the ossified tissue was disconnected all around and “floated.” Then, a titanium mesh cage and plate combined with a bone graft was used for the fixation.
Posterior approach
The patients were placed in the prone position and a midline incision was made. Subsequently, paraspinous muscles were peeled to expose the bilateral laminae of the affected vertebrae. Margel's method was used to place pedicle screws on the levels to be decompressed. The starting point for the pedicle screw was just medial to the hillock of the lateral mass in the coronal plane and midway between the surfaces of the superior and inferior articular process. A 2-mm burr was used to start the hole. Next, a hand drill was inserted into the starting hole, angling laterally about 20° and parallel to the facet joint in the sagittal plane. This could be judged best by placing a thin, flat instrument into the joint to be fused. Drilling proceeded carefully just to, but not through, the second cortex, as bicortical fixation has not been demonstrated to be of biomechanical superior. A depth gauge was then inserted to determine screw length, and then a pedicle screw system was used for fixation. The laminae were resected, and small wedges of bone were placed adjacent to bilateral joints to facilitate fusion.
Postoperative care
After surgeries, the patients were ordered to wear neck braces for 3 months for protection. X-rays, CTs and MRI were taken 1 week, 3 months, 6 months, 12 months, and 24 months after surgery, and at the last follow-up.
The Japanese Orthopaedic Association (JOA) scoring system was used to assess the improvement of neurological status after the operation. The improvement rate (IR) was calculated as follows:4 IR = (postoperative JOA score – preoperative JOA score) / (17 – preoperative JOA score) × 100%. Surgical outcome was defined as excellent (IR ≥ 75%), good (75% > IR ≥ 50%), fair (50% > IR ≥ 25%), or poor (IR < 25%).
Statistical analysis
Statistical analyses were performed using SPSS statistical software (version 13.0, SPSS, Chicago, IL, USA). Paired t-test and group t-test were used for comparison of quantitative data. Fisher's exact test was applied for qualitative data. The results were considered significant when P-value was less than 0.05.
RESULTS
Of the 56 patients included in our study, 26 were treated with anterior approach and the rest 30 treated with posterior approach. There were no significant differences in the baseline characteristics of the two groups, including the preoperative canal occupancy rate, canal sagittal diameter, cervical curvature, type of OPLL, the mean preoperative cervical range of motion (ROM) in the sagittal plane and the JOA score [Table 1].
The duration of surgery for the anterior and posterior approaches were 161±45 min (range 120–210 min) and 125±34 min (range 100–180 min), respectively. The blood loss in anterior and posterior approaches was 763±122 ml (range 400–1700 ml) and 516±94 ml (range 400–1200 ml), respectively. The posterior approach required significantly lesser time and resulted in significantly lesser blood loss than the anterior approach. The number of vertebrae removed was 1.92 (range 1–3 vertebrae) on average and the mean of fusion extent was 3.92 (range 3–5) vertebrae in the anterior approach group. In the posterior approach group, the number of vertebrae lamina removed was 3.67 (range 3–5 vertebrae lamina) on average and the mean of fusion extent was 4.27 (range 3–6) vertebrae.
All patients healed by primary intention. All cases were followed up for 2 years or more. For the anterior and posterior approaches, the patients were followed up for 36.3±6.4 months (range 24–57 months) and 37.6±6.7 months (range 24–69 months), respectively. At the last follow-up, the mean ROM in the sagittal plane of the anterior approach group decreased from preoperative 67.6°±3.4° to postoperative 45.7°±2.6°. In the posterior group, the preoperative value of 64.5°±3.3° dropped to 41.7°±3.0°. The mean preoperative ROM and the ROM at the last follow-up were not significantly different between the two groups.
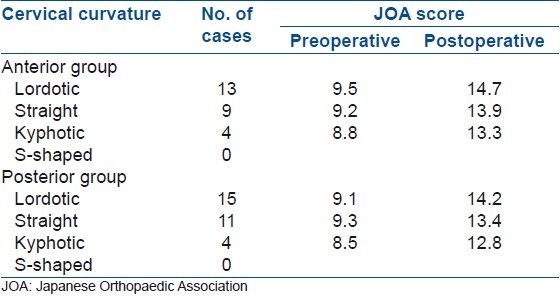
The mean postoperative JOA score of the anterior approach group increased to 14.2±1.6 points from the preoperative 9.3±1.2 points, with a mean improvement rate of 58.6%±10.4% and 65% of the patients had excellent or good outcomes. In the posterior approach group, the mean postoperative JOA score improved from 9.1±1.1 to 13.7±1.5 points postoperatively; the average improvement rate was 54.8%±9.7% and 60% of patients had excellent or good outcomes. The preoperative and the last follow-up JOA scores were not significantly different between the two groups. There were significant differences in the JOA score at the last follow-up between the two groups with canal occupancy ratios ≥50%, and the anterior approach group had better outcomes. However, no noticeable association was found between cervical curvature or type of OPLL and outcome in the two groups [Tables 1–4 and Figure 1].
Table 4.
Surgical outcomes in the anterior or posterior groups with different types of OPLL
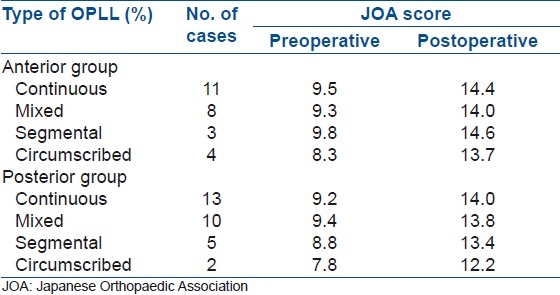
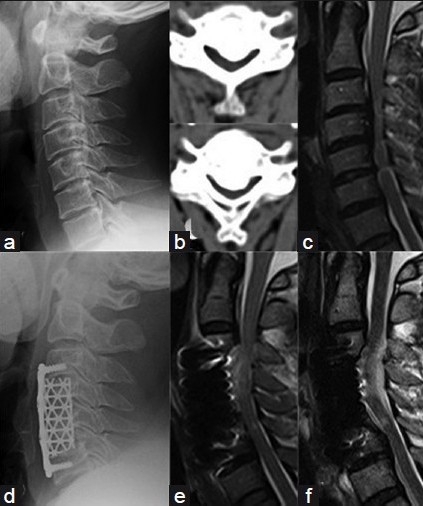
Figure 1A.

A 66-year-old man, with a continuous cervical OPLL involving multiple levels. (a–c) Preoperative lateral X-ray, cervical plain CT and MRI demonstrated significant compression of the spinal cord. The patient underwent C3–C6 laminectomy, decompression and pedicle screw fixation. (d) Postoperative lateral X-ray showing satisfactory fixation with a pedicle screw system. (e, f) Plain MRI on the day after surgery and 24 months postoperative demonstrated good morphology of the spinal cord
Table 2.
Surgical outcomes in the anterior or posterior groups with different canal occupancy ratio
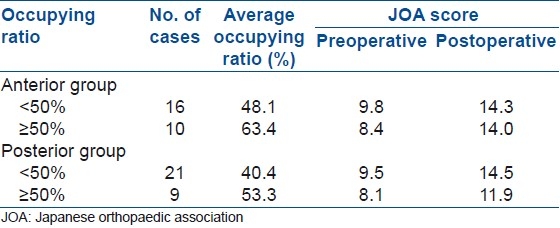
Table 3.
Surgical outcomes in the anterior or posterior groups with different cervical curvature
Complications
The cerebrospinal fluid leaks were seen in two cases in the present study in anterior approach surgeries. Both of them were managed successfully by keeping the patients in supine positions for 5 and 7 days. One patient had quadriplegia after surgery and was presumably due to a gradually resected bony structure causing a slow decompression that led to repeated bulging of the spinal cord, eventually severing the spinal cord [Figure 2]. Twelve months postoperatively, a patient demonstrated asymptomatic implant subsidence, and no specific measure was taken. These two patients were considered as having poor outcome.
Figure 1B.
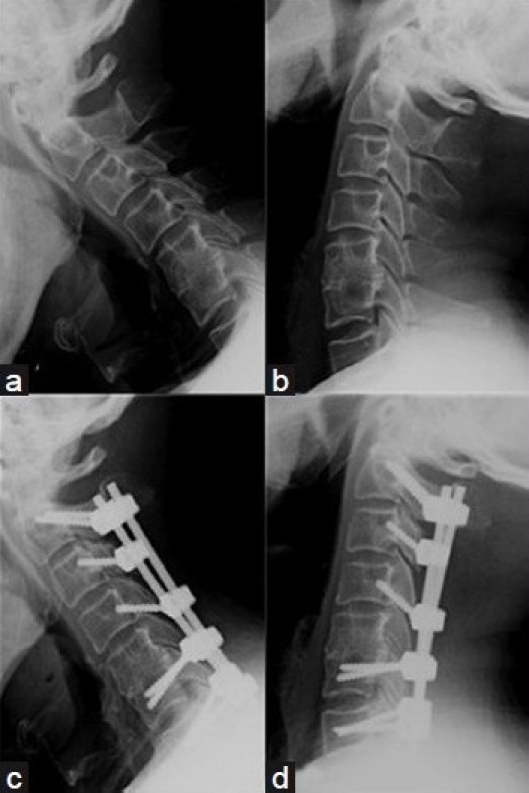
Followup of same patient. His preoperative JOA score was 8, the postoperative JOA score was 15, and his IR was 78%. (a-d) His cervical ROM in the sagittal plane decreased from 50° preoperative to 40° postoperative. At the last follow-up, no progression of the OPLL or related complications was observed. The outcome was satisfactory
Figure 2A.
A 45-year-old man, who also suffered from continuous cervical OPLL of multiple levels. (a–c) Preoperative lateral X-ray, cervical plain CT and MRI demonstrated significant compression of the spinal cord. The patient underwent subtotal C4–C6 corpectomy and decompression, and a titanium mesh cage and plate combined with bone graft was used for the fixation. (d) Postoperative lateral X-ray showing satisfactory reduction with a titanium mesh cage and plate, (e, f) but the degeneration of the spinal cord can be observed at the day after surgery and 24 months postoperative, respectively
Figure 2B.
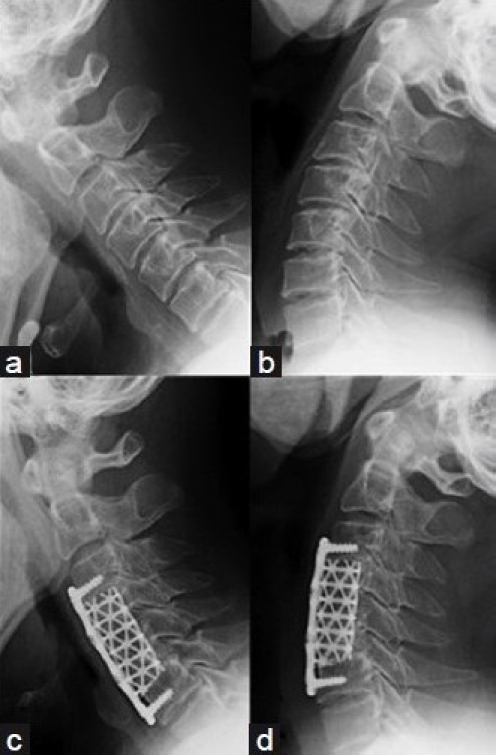
Followup of same patient. He was paralyzed postoperatively, presumably because the gradually resected bony structure caused a gradual decompression which led to repeated bulging of the spinal cord and induced a partial severing of the spinal cord. The preoperative JOA score was 9 and the JOA score 24 months postoperative was 9, with no improvement. (a-d) The ROM in the sagittal plane decreased from 60° preoperative to 50° postoperative. The outcome was poor
One case of cerebrospinal fluid leakage in posterior approach was treated by local pressure and by confining the patient in the supine position for 5 days. Two cases suffered from C5 nerve root injury (one was bilateral and the other was unilateral). They had hypoesthesia and pain of the lateral arm and weakness of the biceps and deltoid muscles. The time of initial onset of C5 palsy symptoms were all within 8 hours postoperative. The patients were treated conservatively by oral neurotrophic drugs, hyperbaric oxygen therapy and exercise. Three months later, one patient's symptoms disappeared. Symptoms of the other patient were relieved, and the patient was considered as having poor outcome. One patient experienced progression of the OPLL and had deterioration of nervous function after 45 months, which was successfully managed by anterior decompression and fixation, and was also considered as having poor outcome. No case of implant failure was observed.
DISCUSSION
OPLL begins with a pathological extracellular hyperplasia and hypertrophy of the posterior longitudinal ligament, leading to ectopic ossification at the spine. Cervical OPLL causes canal stenosis and compression of the spinal cord and nerve roots, and subsequently clinical symptoms and signs of myelopathy.15 Factors that influence the onset and progression of cervical OPLL include the compression of the ossified ligament, a congenitally narrow spinal canal, segmental instability and trauma. Conservative treatment cannot alter the natural history of cervical OPLL. Most surgeons believe that surgical intervention should be applied before irreversible myelopathy occurs, so that the progression can be arrested and deterioration of spinal function is prevented. However, the choice of anterior versus posterior approach as surgical strategy remains controversial.1
Direct removal of the OPLL by anterior surgery offers better decompression, and hence is theoretically the optimal option. Nevertheless, reviewing literature shows that anterior corpectomy and fusion is better suited for OPLL involving one or two levels.4,16–18 For OPLL of three levels or more, can a similar effect be obtained by anterior surgery? We conclude from our study that the anterior approach for multiple levels can achieve satisfactory outcomes, and the patients with an canal occupancy ratio of OPLL ≥50% managed by anterior surgery had better outcomes. However, for those with more severe stenosis, anterior approaches are more difficult and associated with higher risks and complications; also, it is a technically demanding procedure and should be performed by an experienced surgical team. OPLL of multiple levels leading to severe canal stenosis, the available space required for removal of the ossified ligaments is limited. The gradually decompressed bony structure causes repeated bulging of the spinal cord. This leads to repeated trauma to the spinal cord, which might cause spinal damage or even paraplegia. One case in the anterior group was paralyzed after surgery. Moreover, internal fixation of multiple levels is susceptible to loosening and the mobility of the cervical spine may be impaired.3,4 Even combined with anterior placement of titanium plates, the nonunion rate was reported to be as high as 6–18%.5,6 Among the anterior approach group, one case had an implant subsidence, and although the case was asymptomatic, a close follow-up was warranted. Therefore, we suggest that the patients should be ordered to wear neck braces for protection until the X-ray shows incorporation of the intervertebral bone graft.
Posterior laminectomy, decompression and fixation is a well-established technique and is relatively simple and safe. We found that for OPLL of three levels or more, it is an effective strategy. In most of the cases, effective and safe decompression of the spinal cord was accomplished. It can also improve the cervical curvature through pedicle screw system and provide immediate and long-term stability of the cervical spine, and avoid development of kyphosis. Theoretically, it can reduce the progression of cervical OPLL.19,20 Lack of immediate stability after laminoplasty or laminectomy without fixation might lead to development of postoperative kyphosis and progression of OPLL, eventually causing the relapse of myelopathy.12 In our study, at the last follow-up, no kyphosis was observed. Only one patient had progression of the OPLL. Nevertheless, even when OPLL progresses after posterior cervical decompression, because of the available space from resected lamina, a secondary anterior decompression can excise intervertebral discs or floated OPLL and a simultaneous bone graft combined with fusion and fixation can be done. This can effectively solve the progression of OPLL and minimize complications due to posterior decompression surgery.
Compared with the anterior approach, posterior surgery is safer, less technically demanding, and is associated with less blood loss and better long-term outcomes.21 Posterior surgery also has its disadvantages. First, since the compression is located anteriorly, decompression in posterior surgery is indirect, without removal of the OPLL. Our study showed that when the canal occupancy ratio of OPLL was more than 50%, the outcomes were less favourable. Moreover, cervical OPLL is often accompanied by various levels of cervical degeneration, spinal disc herniation and nerve root compression, and posterior surgery is ineffective for decompression of nerve roots, causing postoperative symptoms. Furthermore, it has been reported that segmental root palsy occurred in 3.2–28.6% of patients.11 The mechanisms have not been elucidated so far, although most surgeons believe that the main reason might be that a floated spinal cord after posterior decompression causes traction on the nerve roots, leading to nerve root edema. We believe that sustaining a physiological cervical curvature during surgery and reliable internal fixation and fusion could reduce prominently the incidence of this complication.
CONCLUSION
The critical step of treatment for cervical OPLL involving multiple levels, is effective decompression and immediate cervical spine stability. Both anterior and posterior decompression and fixation can achieve this therapeutic aim. In patients with the canal occupancy ratio of OPLL ≥50%, treatment by the anterior approach can have better outcomes, though it is more difficult and associated with higher risks and complications. Despite its limitations in patients with high occupancy ratio OPLLs, through the multiple-level laminectomy, posterior fixation can achieve effective decompression, maintaining or restoring stability of the cervical spine, and thereby improving neural outcome and preventing the progression of OPLL. We believe that the posterior indirect decompression and fixation may be adopted as the primary treatment for cervical OPLL involving multiple levels with the canal occupancy ratios of OPLL <50%.
ACKNOWLEDGEMENT
We acknowledge the patients who featured in this manuscript for their written consent for publication.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Edwards CC, 2nd, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF. Cervical myelopathy. Current diagnostic and treatment strategies. Spine J. 2003;3:68–81. doi: 10.1016/s1529-9430(02)00566-1. [DOI] [PubMed] [Google Scholar]
- 2.Morio Y, Teshima R, Nagashima H, Nawata K, Yamasaki D, Nanjo Y. Correlation between operative outcomes of cervical compression myelopathy and mri0 of the spinal cord. Spine (Phila Pa 1976) 2001;26:1238–45. doi: 10.1097/00007632-200106010-00012. [DOI] [PubMed] [Google Scholar]
- 3.Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976) 2007;32:654–60. doi: 10.1097/01.brs.0000257566.91177.cb. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y, Chen D, Wang X, Lu X, Guo Y, He Z, et al. Anterior corpectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. Int Orthop. 2009;33:477–82. doi: 10.1007/s00264-008-0542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2001;26:643–6. doi: 10.1097/00007632-200103150-00015. [DOI] [PubMed] [Google Scholar]
- 6.Mayr MT, Subach BR, Comey CH, Rodts GE, Haid RW., Jr Cervical spinal stenosis: Outcome after anterior corpectomy, allograft reconstruction, and instrumentation. J Neurosurg. 2002;96(1 Suppl):10–6. doi: 10.3171/spi.2002.96.1.0010. [DOI] [PubMed] [Google Scholar]
- 7.Wang JC, McDonough PW, Endow KK, Delamarter RB. A comparison of fusion rates between single-level cervical corpectomy and tow-level discectomy and fusion. J Spinal Disord. 2001;14:222–5. doi: 10.1097/00002517-200106000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS. Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine (Phila Pa 1976) 2003;28:2352–8. doi: 10.1097/01.BRS.0000085344.22471.23. [DOI] [PubMed] [Google Scholar]
- 9.Hale JJ, Gruson KI, Spivak JM. Laminoplasty: A review of its role in compressive cervical myelopathy. Spine J. 2006;6(6 Suppl):289S–98S. doi: 10.1016/j.spinee.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 10.Choi S, Lee SH, Lee JY, Choi WC, Choi G, Jung B, et al. Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech. 2005;18:309–14. doi: 10.1097/01.bsd.0000161236.94894.fc. [DOI] [PubMed] [Google Scholar]
- 11.Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy: Review of the literature. Spine (Phial Pa 1976) 2003;28:2447–51. doi: 10.1097/01.BRS.0000090833.96168.3F. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, et al. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;1:168–74. doi: 10.3171/spi.2004.1.2.0168. [DOI] [PubMed] [Google Scholar]
- 13.Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976. 2007;32:647–53. doi: 10.1097/01.brs.0000257560.91147.86. [DOI] [PubMed] [Google Scholar]
- 14.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg. 2002;96(2 Suppl):180–9. [PubMed] [Google Scholar]
- 15.Matsunaga S, Sakou T. The Cervical Spine. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. Ossification of the posterior longitudinal ligaments: prevalence, presentation, and natural history; pp. 1091–8. [Google Scholar]
- 16.Mizuno J, Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6(6 Suppl):282S–8S. doi: 10.1016/j.spinee.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Goto S, Kita T. Long-term follow-up evaluation of surgery for ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 1995;20:2247–56. doi: 10.1097/00007632-199510001-00012. [DOI] [PubMed] [Google Scholar]
- 18.Onari K, Akiyama N, Kondo S, Toguchi A, Mihara H, Tsuchiya T. Long-term follow-up results of anterior interbody fusion applied for cervical myelopathy due to ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2001;26:488–93. doi: 10.1097/00007632-200103010-00011. [DOI] [PubMed] [Google Scholar]
- 19.Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic mylopathy and ossification of the posterior longitudinal ligament: Effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery. 2003;52:1081–7. [PubMed] [Google Scholar]
- 20.Tokuhashi Y, Ajiro Y, Umezawa N. A patient with two re-surgeries for delayed myelopathy due to progression of ossification of the posterior longitudinal ligaments after cervical laminoplasty. Spine (Phila Pa 1976) 2009;34:E101–5. doi: 10.1097/BRS.0b013e31818a3135. [DOI] [PubMed] [Google Scholar]
- 21.Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine (Phila Pa 1976) 2006;31:2998–3005. doi: 10.1097/01.brs.0000250307.78987.6b. [DOI] [PubMed] [Google Scholar]


