Despite the importance of sleep for recovery, hospital noise may put patients at risk for sleep loss and its associated negative effects. Objectively measured hospital noise can range as high as 67 dB in the intensive care unit to 42 dB in surgical wards, far from the World Health Organization (WHO) international recommendations of 30 dB for patient rooms.1 Although almost half of Medicare patients report that their hospital rooms were not quiet at night, data to objectively characterize noise levels and sleep in hospitalized adults in medical wards are limited.2 One study that objectively measured sleep and noise among hospitalized adults older than 70 years found no association.3 This study aimed to objectively measure noise and sleep duration in adult medical ward patients.
Methods
Eligible patients were community-dwelling ambulatory adults older than 50 years who were not transferred from the intensive care unit and enrolled in an ongoing study of general medicine inpatients at the University of Chicago Medical Center.4 Patients with a known sleep disorder (ie, obstructive sleep apnea), with cognitive impairment (score of <17 on a telephone version of the Mini-Mental State Examination), under respiratory isolation, or admitted for more than 72 hours were excluded. The study was approved by the University of Chicago institutional review board.
On the first enrollment day, trained research assistants administered the Pittsburgh Sleep Quality Index (PSQI) to assess baseline sleep quality and hygiene and the Epworth Sleepiness Scale to characterize sleepiness in routine situations.5,6 Patients rated any potential sleep disruptions from 1 (not at all disruptive) to 5 (most disruptive) using items from prior studies.7,8 Based on the skewed distribution of responses, a patient “report of noise disruption” was defined as a response of 2 or higher. Objective sleep data (sleep duration and sleep efficiency) were obtained with validated wrist activity monitors (Actiwatch 2; Respironics Inc).9 Noise levels were recorded with bedside Larson Davis 820 Sound Level Monitors (Larson Davis Inc), which recorded average (Leq), minimum (Lmin), and maximum (Lmax) sound level.
Descriptive statistics were used to summarize objective sleep and noise levels. Multivariate random effects linear regression models, controlling for study day, race, age, sex, and PSQI and Epworth scores and clustered by subject, characterized the association of nighttime noise and sleep duration and efficiency. All statistical tests were performed using Stata 10.0 (StataCorp), with statistical significance defined as P < .05.
Results
From April 2010 to May 2011, of the 145 (55%) eligible patients screened, 106 (73%) consented to the sleep study. Patients in the study were predominantly African American (63%) and female (51%), with a mean (SD) age of 66 (12) years and a median (interquartile range) length of stay of 4 (3–5) days. Subjects had relatively few comorbidities: 20% had chronic obstructive pulmonary disease; 16%, congestive heart failure; 23%, diabetes; and 36%, hypertension. One-third of subjects reported excessive daytime sleepiness on the Epworth Sleepiness Scale. Forty-eight percent of subjects were classified as “good sleepers” with a global PSQI score of 5 or lower.
For 92 patients with sound data, patient room noise levels over 155 hospital days universally exceeded the WHO recommendations for average noise level (Leq, 48.0 dB [95% CI, 47.2–49.5 dB] vs WHO, 30 dB; P < .001) and peak noise level approached that of a chain saw (Lmax, 80.3 dB [95% CI, 78.5–82.2] vs WHO, 40 dB; P < .001]). While all noise measures were lower between 11 PM to 7 AM, all nights exceeded recommendations for maximum noise level (mean Lmax, 69.7 dB [95% CI, 68.1–71.3 dB]) and 94% of the nights exceeded recommendations for average noise level (mean Leq, 38.2dB [95% CI, 36.9–39.4 dB]). More than 42% of patients (n=39 [42.5%]) reported noise disruptions of sleep, which was also associated with higher maximum noise levels (Lmax, 82.6 vs 78.6 dB; P =.04).
For 85 patients with sleep data, actigraphy data demonstrated that patients slept significantly less in the hospital than their self-reported baseline sleep (314 minutes vs 382 minutes; P=.002). Mean sleep efficiency when hospitalized was also low (73.3% [95% CI, 70.3%–76.4%]), with 52% of actigraphically recorded nights below the normal lower boundary of 80% efficiency for adults.
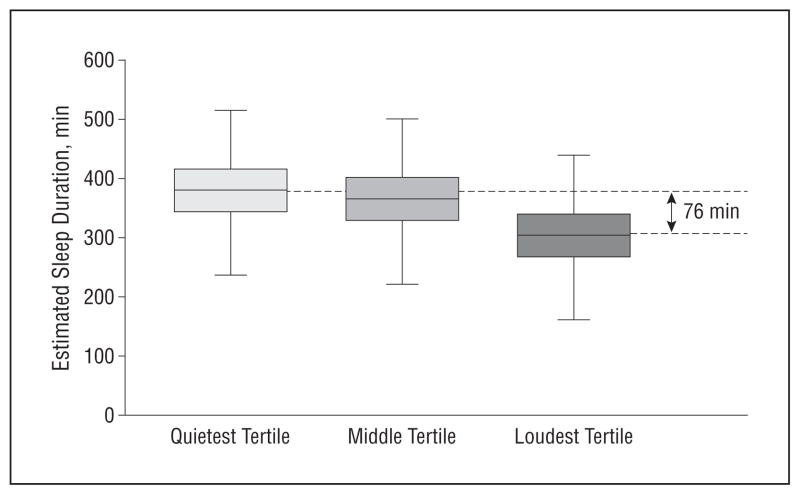
In multivariate analyses, patients exposed to the loudest tertile of average nighttime noise levels (mean Leq, 50 dB [95% CI, 47.8–52.0 dB]) slept significantly less (−76 minutes [95% CI, −134 to −18 minutes]; P=.01) than patients exposed to the quietest tertile of average nighttime noise (mean Leq, 43.3 dB [95% CI, 41.1–44.8 dB]) (Figure). The most common sources of noise disruption reported by patients were staff conversation (65%), roommates (54%), alarms (42%), intercoms (39%), and pagers (38%).
Figure.
Predicted values of sleep duration across tertiles of average nighttime noise level from a multivariate linear regression model (85 patients; 117 nights) shows a difference of 76 minutes in sleep duration between quietest and loudest tertile (P=.01). Boxes represent interquartile range and bars represent overall range.
Comment
Hospital noise levels in patient rooms are markedly higher than recommended levels and associated with clinically significant sleep loss among hospitalized patients. Much of this noise is attributable to preventable sources such as staff conversation. Hospitals should implement interventions to reduce nighttime noise levels in an effort to improve patient sleep, which may also improve patient satisfaction and health outcomes.
Acknowledgments
Funding/Support: We acknowledge funding by the National Institute on Aging through a Short-Term Aging-Related Research Program (1T35AG028785-01A1), National Institute on Aging career development award (1K23AG033763-01A1), a midcareer career development award (1 K24 AG031326-01), a Program Project (PO1 AG-11412), and the Agency for Healthcare Research and Quality Centers for Education and Research on Therapeutics (1U18HS016967-01).
Role of the Sponsors: The sponsors had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Arora had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Yoder, Staisiunas, Meltzer, Knutson, and Arora.
Acquisition of data: Yoder, Staisiunas, Meltzer, Knutson, and Arora.
Analysis and interpretation of data: Yoder, Meltzer, Knutson, and Arora.
Drafting of the manuscript: Yoder, Staisiunas, Knutson, and Arora.
Critical revision of the manuscript for important intellectual content: Yoder, Staisiunas, Meltzer, Knutson, and Arora.
Statistical analysis: Yoder, Meltzer, and Arora.
Obtained funding: Staisiunas, Meltzer, and Arora.
Administrative, technical, and material support: Yoder, Staisiunas, Meltzer, Knutson, and Arora.
Study supervision: Staisiunas, Meltzer, and Arora.
Financial Disclosure: None reported.
Previous Presentation: The data were previously presented at the 2011 Society of Hospital Medicine Annual Meeting; May 11, 2011; Dallas, Texas.
Additional Contributions: We thank Eve Van Cauter, PhD, of the Sleep, Metabolism, and Health Center at the University of Chicago for her support on this project.
References
- 1.Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. World Health Organization Web site; 1999. [Accessed July 22, 2011]. http://www.who.int/docstore/peh/noise/guidelines2.html. [Google Scholar]
- 2.Young JS, Bourgeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482. doi: 10.1002/jhm.372. [DOI] [PubMed] [Google Scholar]
- 3.Missildine K, Bergstrom N, Meininger J, Richards K, Foreman MD. Sleep in hospitalized elders: a pilot study. Geriatr Nurs. 2010;31(4):263–271. doi: 10.1016/j.gerinurse.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 5.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 6.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 7.Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–715. doi: 10.1164/rccm.2201090. [DOI] [PubMed] [Google Scholar]
- 8.Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J Appl Psychol. 1985;70(1):22–28. [PubMed] [Google Scholar]
- 9.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26(3):342–392. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]