Abstract
There are serious problems concerning the inadequate prescription of antibiotics and overuse of injections in primary care. However, the determinants of prescription patterns in Korea are not well-documented. To examine the area characteristics affecting the prescription of antibiotics and injections in primary care practices in the treatment of respiratory tract infections (RTIs), a nationwide cross-sectional study was performed in all 250 administrative districts of Korea. The outcome was modeled as a binary variable: over-prescription or not compared with the nation-wide average. Over-prescription of antibiotics was associated with the ratio of specialists to general physicians and over-prescription in previous years in the area (adjusted odds ratio [aOR], 4.8; 95% confidence interval [CI] 1.5-14.8; and aOR, 12.0; 95% CI 5.5-25.9, respectively). Over-use of injections was associated with younger population, urban living and the number of hospital beds in the area (aOR, 0.2; 95% CI 0.1-0.4; aOR, 0.3; 95% CI 0.1-0.8; and aOR, 0.4, 95% CI 0.2-0.9; respectively). There were differences in the prescribing patterns in different districts; prescription patterns were affected more by supply factors than by demand factors. Highly competitive medical environment associated with supply factors is a significant determinant of prescription patterns in Korea.
Keywords: Primary Care, Antibiotics, Injections, Prescription Pattern
INTRODUCTION
Appropriate use of antibiotics and injections has contributed to the control of infectious diseases and the reduction of mortality (1, 2). However, there are serious problems concerning the inadequate use of antibiotics and the overuse of injections in ambulatory practice (3, 4). Overuse of antibiotics, particularly broad-spectrum antibiotics, in primary care is a major contributing factor to reduced drug efficacy, increased prevalence of resistant pathogens in the community, and the appearance of new co-infections (5). The overuse of injected medications is also a serious problem. Prescribing injection-delivered medications can produce side effects, which include local problems related to the injection site such as bleeding, inflammation, atrophy, and nerve injury, and systemic problems related to hypersensitivity reactions such as anaphylactic shock. Injection-drug users likely acquire human immunodeficiency virus infection or hepatitis C virus infection by sharing drug equipment (6, 7).
Decision model of prescribing antibiotics and injections is complex, and multiple factors other than clinical considerations can influence the decision to prescribe (8). These include patient characteristics, physician characteristics, and medical environments such as competition. Patient characteristics such as age, lower socio-economic status, and higher co-morbidity have significant effects on the antibiotic prescription rate (8-10). Physician characteristics, including gender, age, time since graduation, and volume of practice, significantly influence antibiotic prescription (8, 11, 12). An urban location of a medical practice and patient income level also influence antibiotic prescription rates (8, 13). Other significant predictors are the physician expertise (i.e., specialist or generalist) (8, 14). Medical environment variables such as the number of primary care clinics and number of hospital beds affect the rate of antibiotic prescription (15).
Previous studies concerning prescribing patterns tended to address the characteristics of individual patients and doctors, related with prescription episodes. Such results are not easily extrapolated to a regional or national scale. Several studies have described regional patterns of medical care utilization and health care delivery with the application of small area variation. These outcome variables were classified and measured by the unit of area (16). Factors affecting health care episodes are classified as demand and supply factors. Demand factors include age, gender, education, income, and insurance types of population, and supply factors include the number of hospital beds per population and the number of doctors (17).
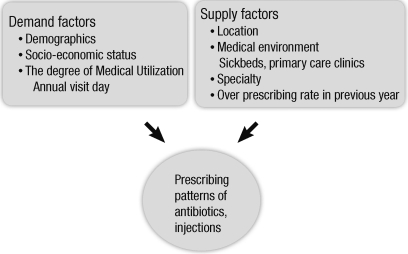
Using area as a unit of analysis, this study examined the prescription patterns of antibiotics and injections in primary care in Korea. The hypothesis of this study was that the demand and supply characteristics of areas, defined as administrative districts in Korea, affect the prescription patterns of antibiotics and the use of injections (Fig. 1). Some variables, such as co-morbidity of patients and demographic characteristics of physicians, were not included due to data unavailability.
Fig. 1.
Theoretical model regarding prescribing pattern of antibiotics and injected medications.
MATERIALS AND METHODS
Data and variables
This was a cross-sectional study that used population census data, the evaluation of medical institutions, and the assessment of prescribing rate of individual primary care clinics concerning upper respiratory tract infections (URIs).
We analyzed data from the 2005 Population Census of Korea, the 2008 Community Health Survey, and the 2006 and 2007 data of the Health Insurance Review and Assessment Services (HIRA). All dependent and independent variables were measured in terms of administrative districts, which are the unit of analysis in the databases. The dependent variables from the 2006 and 2007 HIRA data were binary variables depending on whether the over-prescription rate of antibiotics and injections in a given administrative district was greater than the national average of over-prescription rate. We calculated the mean prescribing rate in the administrative districts using data from the entire primary care clinics located in the administrative districts. The mean antibiotic prescription rate of all primary care clinics was 62.4% in the first-quarter of 2006 and 54.2% in the first-quarter of 2007. The mean injection prescription rate of all primary care clinics was 27.9% in the first-quarter of 2006 and 25.8% in the first quarter of 2007. Furthermore, the over-prescription rate of a given administrative district was calculated by the proportion of over-prescribing clinics in all evaluated primary care clinics. Then, the binary dependent variable was constructed by comparing the overprescribing rate of a given administrative district with the mean over-prescribing rate of all administrative districts. Using this design, the mean over-prescribing rate of antibiotics and injection rate in 2007 were 41.8% and 36.8%, respectively.
The independent variables from the 2005 Population Census of the Korean National Statistical Office and the 2008 Community Health Survey represent demand and supply factors. Demand factors in the area included demographic factors (sex ratio, total population, and elderly population in each area) and socioeconomic factors (educational level, unemployment rate, and local tax). The sex ratio was the ratio of male to female population. The percentage of people over age 65 yr and under age 15 yr to total population was defined as elderly population and younger population, respectively. The proportion of those completing education beyond high school was used to measure the educational level. Unemployment rate was defined as the proportion of unemployed people to all economically active people aged 16-64 yr. Local tax data were extracted from the 2006 Regional National Tax Yearbook. The model included annual outpatient days of the area to control for the effect of medical use on prescription rate, and classified the population into urban and rural dwellers to account for any influence due to residence or medical environment. Other supply factors in the area included total number of hospital beds per 10,000 people, total number of primary care clinics per 10,000 people, ratio of specialists to general physicians, number of primary care physicians per 10,000 persons, and prescription patterns in the previous year. Internal medicine physicians, pediatricians, family physicians and general practice providing primary care services were categorized as primary care physicians. The ratio of specialists to general physicians was limited to primary care clinics. All independent variables were binary variables based on whether the value of a given area was greater than the national average.
Statistical analyses
We evaluated the effect of demand and supply factors in the area on the prescription patterns of antibiotics and injections. First, we evaluated the odds ratio (OR) of antibiotic and injective over-prescription using univariate logistic regression. Next, the association of the above area indices with over-prescription or not over-prescription were also examined using multivariate logistic regression. All analyses were conducted using Stata software (Stata Corp, College Station, TX, USA), and statistical significance was tested with the criterion of P value of 0.05. We showed the regional distribution of over-prescription or not over-prescription to visualize prescribing patterns using the Statistical Map program of the National Statistical Office.
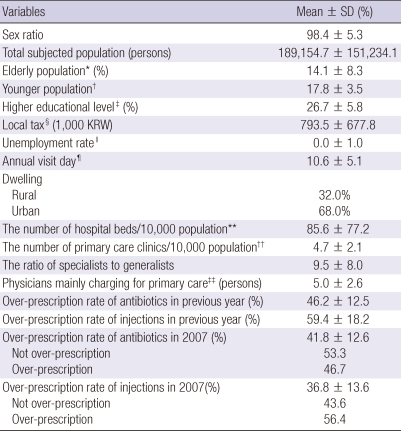
RESULTS
All administrative districts of Korea (n = 250) were included in the analysis of antibiotic and injections prescriptions in 2006 and 2007. The over-prescription rates of antibiotics were 46.2% in 2006 and 41.8% in 2007. The over-prescription rates of injections were 59.4% in 2006 and 36.8% in 2007. Descriptive statistics of demand and supply factors are shown in Table 1.
Table 1.
Descriptive statistics of the administrative districts
*The proportion of population > 65-yr-of-age; †The proportion of population < 15-yr-of-age; ‡The proportion of population with more than high school education; §Amount of local tax per person in districts of year (1,000 KRW); ∥Standardized Z-score by subtracting the mean of all areas from each area and dividing by the standard deviation for variables. The actual mean value was -0.01; ¶Annual outpatient days in primary care clinics; **The number of hospital beds per 10,000 people; ††The number of primary care clinics per 10,000 people; ‡‡The number of physicians charging primary care per 10,000 people: Family medicine; Internal medicine; Pediatrics; General practice.
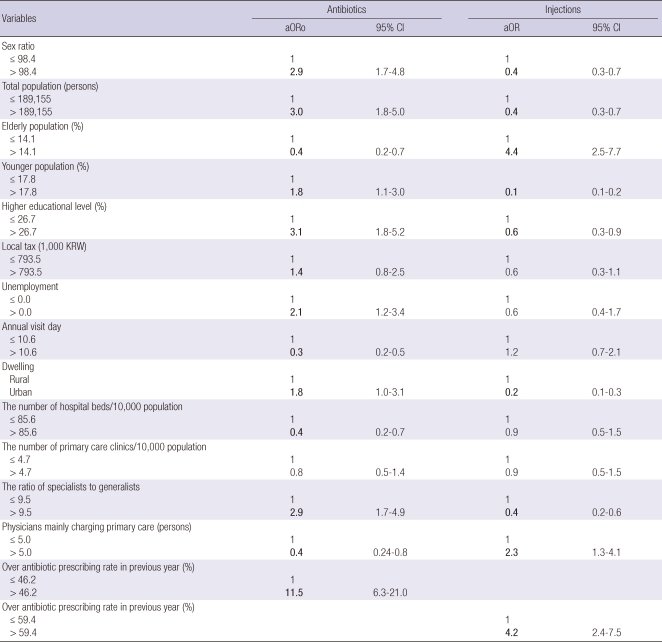
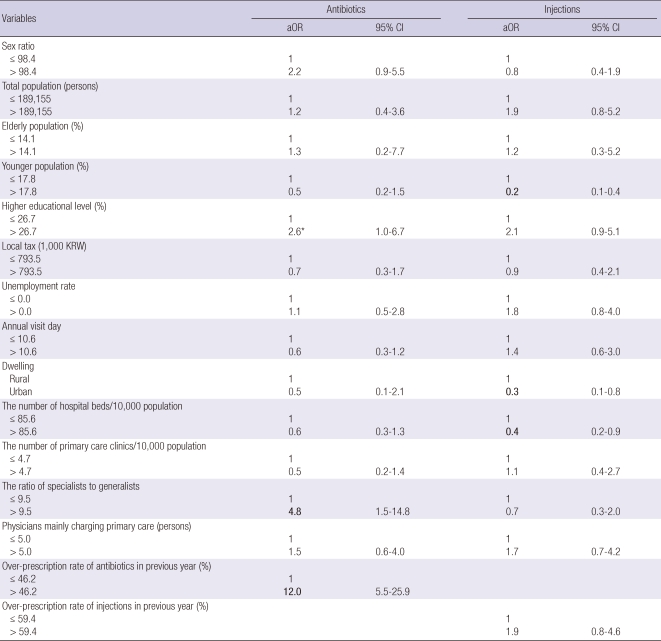
Relationships between area characteristics and prescribing patterns of antibiotics
There were differences between over-prescription and not over-prescription according to demand and supply factors of the area. The areas with greater sex ratio, total population, education level, unemployment, ratio of specialists to general physicians, and over-prescribing rate of antibiotics in the previous year were associated with higher adjusted OR (aOR) to over-prescription of antibiotics. The areas with greater aged population, annual visit days, number of hospital beds, number of physicians mainly charging for primary care, and district population were less likely to be over-prescribed (Table 2). The results of multivariate logistic regression indicated that areas with higher ratio of specialists to general physicians and over-prescription in the previous year had a higher OR of antibiotic over-prescription (aOR, 4.8; 95% CI 1.5-14.8 and aOR, 12.0; 95% CI 5.5-25.9, respectively). Higher educational level had a marginally significant relationship with over-prescriptio (aOR, 2.6; 95% CI 1.0-6.7) (Table 3).
Table 2.
Univariate association between study variables and over-prescription in primary care clinics
The bold characters are statistically significant.
Table 3.
Multivariate logistic regression models: Factors affecting the incidence of over-prescription of primary care clinics
*The result shows marginally significant relationship with over-prescription of antibiotics.
Relationships between area characteristics and prescribing patterns of injections
Areas with greater aged population, number of physicians mainly charging for primary care and over-prescribing rate of injections in the previous year were more likely to be over-prescribed. Areas with high sex ratio, total population, educational level, ratio of specialists to general physicians and urban dwellers were less likely to be over-prescribed (Table 2). The results of multivariate logistic regression indicated that younger population, urban living and the number of hospital beds were significantly associated with the incidence of over-prescription in the district. Younger population (aOR, 0.2; 95% CI 0.1-0.4), urban dwellers (aOR, 0.3; 95% CI 0.1-0.8), and the number of hospital beds had a low aOR for over-prescription (aOR, 0.4; 95% CI 0.2-0.9). However, over-prescription in the previous year was not associated with the incidence of over-prescription in the district (Table 3).
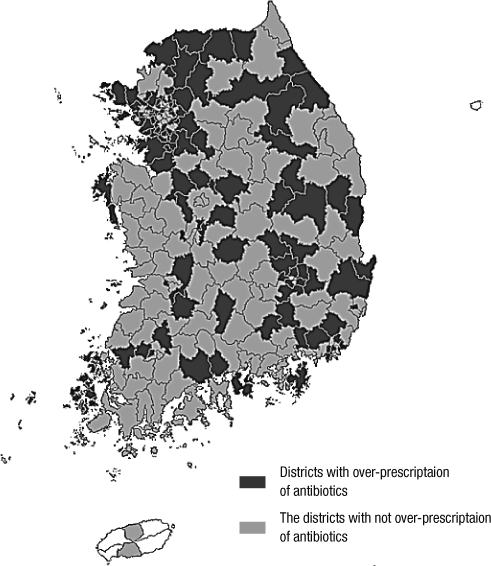
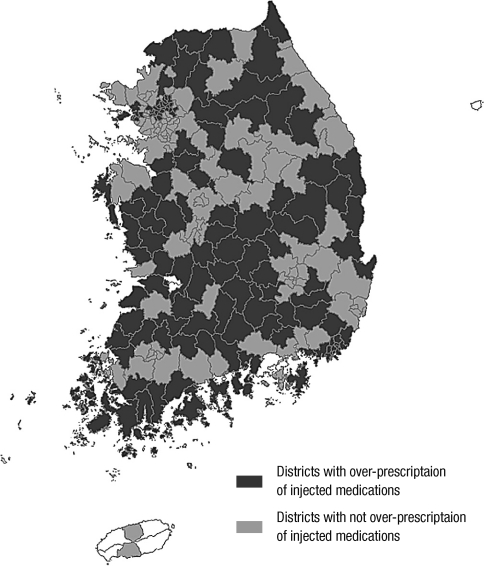
Area distribution of over-prescription of antibiotics and injections
The area distribution of antibiotic over-prescription revealed that Gyeonggi-do and Gyeongsangnam-do had many administrative districts displaying over-prescription compared with the national average (Fig. 2). Chungcheong-do and Jeolla-do had many districts displaying not over-prescription. The area distribution of over-prescription of injection medications indicated that Gangwon-do, Gyeongsangbuk-do, and Jeolla-do tended to display over-prescribing districts, whereas Gyeonggi-do had a lower number of over-prescribing areas than other provinces (Fig. 3).
Fig. 2.
Area distribution of over-prescription or not over-prescription of antibiotics.
Fig. 3.
Area distribution of over-prescription or not over-prescription of injected medications.
DISCUSSION
This study was designed to demonstrate the relationships between area characteristics and the prescription patterns of antibiotics and use of injections in primary care clinics in Korea. The data reveal that the prescribing patterns of antibiotics and injection use are related to demand and supply factors of the areas, along with other factors.
The result suggested that educational level had a marginally significant relationship with over-prescription of antibiotics. The ratio of specialists to general physicians and the prescription rate in the previous year were significantly associated with antibiotic prescribing patterns. Previous studies evaluating the relationship between educational level and antibiotic prescription concluded that people with a lower educational level are more likely to have antibiotics prescribed (18). These findings are not consistent with our results. Infectious diseases including upper respiratory infections (URIs) are related to the educational level of a family; higher risk of URIs among those with a lower educational status is attributed to greater exposure to infectious agents, perhaps reflecting less than adequate hygiene procedures, overcrowding, and related decrease in immunity. Belief or expectation of antibiotic effect as a demand factor has been correlated with the prescription of antibiotics (19). Our results suggest that the influence of education level may be more closely associated with the perceived efficacy of antibiotics in the treatment of URIs than the influence of the environment related to URIs. Those areas with higher ratio of specialists to general physician had a higher aOR concerning antibiotic over-prescription. Internal medicine physicians and pediatric physicians are less likely to prescribe antibiotics than general or family medicine physicians (20). This may suggest that general physicians are more likely to respond to their patients' expectations and requests for prescriptive action. However, our results are not consistent with previous studies, perhaps due to the characteristics of the primary care medical environment in Korea. The proportion of clinics with general practices in primary care clinics was only 15.2% according to 2007 data of the HIRA. Highly competitive environments may make specialists more apt to prescribe antibiotics for fast recovery from URIs and prevention of complications related to URIs such as otitis media, sinusitis, and pneumonia (21, 22). However, these patterns related to specialties should be considered in light of various factors affecting antibiotic prescription rates, which include practice volume and other physician factors such as age, gender, and time since graduation from medical school (8, 23). This study could not conclusively establish relationships between antibiotic prescription and patient demographics, other socioeconomic determinants, accessibility of primary care, supply of inpatient beds, urban/rural dwelling, and the number of physicians mainly charging for primary care. Antibiotic over-prescription was strongly affected by the incidence of over-prescription in the previous year, or the mean prescription rate of the previous year. A short interval of a single year does not accurately reflect changing prescription patterns. But, these findings suggest that antibiotic prescribing patterns of the area do not readily change with time.
According to this study, factors to influence less over-use of injections were younger population, urban dwelling and the higher number of hospital beds. Low over-prescription of injections to younger population may indicate that younger group in general tends to be prescribed oral medication than injections. On the other hand, adult group can be prescribed both oral medication and injection without considering side effects or without special restriction. And adult group more tend to want to prescribe injections for fast relief of respiratory symptoms due to their work. One study reported that people in rural area tend to more strongly ascribe to the benefits of injected medications, and consequently are more likely to be prescribed such medications (24). Rural dwellers can experience less social support when they get sick, and seek prompt relief of their symptoms, allowing them to get back to work as soon as possible. On the other hand, a physician's reputation, be it positive or negative, becomes more widely-known in rural areas than in urban areas. As a result, physicians may be more likely to prescribe injections as a way of enhancing their reputation (24). These trends did not appear in the over-prescription of antibiotics. The preference for injections by consumers may be more pronounced because the rural area consists of a high percentage of elderly population. The finding of this study that the number of hospital beds influences both the capacity of admission and accessibility to health care system indicates that patients in an environment with a greater number of hospital beds have a lower rate of overuse of injections. This result may suggest that physicians are less likely to prescribe and patients are less likely to demand injections in a health care environment where they are promptly admitted and treated. Over-prescription rate of injections in the previous year were not closely related with over-prescription. This may be because over-prescription of injections is mainly affected by demand factors such as medical accessibility or living area, on the other hand, over-prescription of antibiotics is more strongly affected by supply factors such as over-prescription rate in the previous year or competitive medical environment.
Presently, geographic differences were apparent in prescription patterns. Gyeonggi-do and Gyeongsangnam-do have high density of the total population compared with other provinces. These regions also displayed a high rate for over-prescription of antibiotics. Regions with a lower population density had a high rate for over-prescription of injected medications. These results may indicate that a provider's motivation due to competitive environments may influence antibiotic use (25). Moreover, aspects of the medical environment, such as location and accessibility to health care system, have a greater impact on injection use. Geographic differences in prescription pattern are explained by provider practice and population characteristics (26). Our results further suggest that both over-prescription of antibiotics and injected medications may be more affected by supply factors than by demand factors. The majority of the previous studies conducted at the level of the individual patient concluded that various factors of both patient's and doctor's characteristics influence the rate of prescription pattern. It is reasonable to suggest that the highly competitive medical environment created by a large number of primary care clinics in the area and the resulting pressure on physicians for a rapid improvement of symptoms can influence the prescription pattern in primary care practices (15).
This study focused on various area characteristics affecting the prescription patterns of antibiotics and injections, taking into account demand and supply factors. Few studies have examined the association between area characteristics and prescribing patterns of antibiotics and injections, especially in Korea where high prescribing rate of antibiotics and injections is a serious problem. This study has several limitations. First, aggregate data was used, which could not reveal physician beliefs about the efficacy of antibiotics and injections (14). Second, this study could not include physician factors such as age, practice volume, and the number of years since the establishment of clinic, which can be influential to prescribing patterns of antibiotics and injections. Third, this study did not consider the clinical diagnosis for which an injection is prescribed, and the clinical appropriateness of injection prescriptions was not considered. Lastly, this study is a kind of ecological study. So the results of this epidemiological study in which the unit of analysis is a population or region have limitations to be applied to an individual level or other situations.
This study shows an association of a few demand and supply factors in the area with the prescribing patterns of antibiotics and injections. Moreover, there were geographical differences of prescribing patterns. Some supply factors were related to over-prescription of antibiotics, and some medical-environmental factors were highlighted to over-prescription of injections. These findings can suggest the importance of supply factors for intervention strategies. The multiple interventions aimed at reducing antibiotic prescription rates in primary care revealed that general practitioners reduce prescription rates of antibiotics for URIs and maintain high satisfaction among patients (27). Monitoring and feedback mechanisms to physician's prescribing patterns can contribute to changing the prescription landscape. Efforts should be focused not only on knowledge but also on communication in the patient-doctor encounter to achieve an improvement that is reasonable and effective (28).
References
- 1.Choi JH. Recent evidences of sepsis treatment. Infect Chemother. 2008;40:67–75. [Google Scholar]
- 2.Yum HY. Antibiotics for bacterial pneumonia in children. Korean J Pediatr. 2009;52:283–288. [Google Scholar]
- 3.Del Mar C. Prescribing antibiotics in primary care. BMJ. 2007;335:407–408. doi: 10.1136/bmj.39307.642963.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan T, Little P, Stokes T Guideline Development Group. Antibiotic prescribing for self limiting respiratory tract infections in primary care: summary of NICE guidance. BMJ. 2008;337:a437. doi: 10.1136/bmj.a437. [DOI] [PubMed] [Google Scholar]
- 5.Pradier C, Rotily M, Cavailler P, Haas H, Pesce A, Dellamonica P, Obadia Y. Factors related to the prescription of antibiotics for young children with viral pharyngitis by general practitioners and paediatricians in southeastern France. Eur J Clin Microbiol Infect Dis. 1999;18:510–514. doi: 10.1007/s100960050334. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) HIV infection among injection-drug users - 34 states, 2004-2007. MMWR Morb Mortal Wkly Rep. 2009;58:1291–1295. [PubMed] [Google Scholar]
- 7.Lee SW, Kim SY, Kim JK. Seropositivity of anti-HCV in intravenous drug abusers. J Korean Acad Fam Med. 1997;18:1508–1518. [Google Scholar]
- 8.Huang N, Chou YJ, Chang HJ, Ho M, Morlock L. Antibiotic prescribing by ambulatory care physicians for adults with nasopharyngitis, URIs, and acute bronchitis in Taiwan: a multi-level modeling approach. Fam Pract. 2005;22:160–167. doi: 10.1093/fampra/cmh734. [DOI] [PubMed] [Google Scholar]
- 9.Akkerman AE, van der Wouden JC, Kuyvenhoven MM, Dieleman JP, Verheij TJ. Antibiotic prescribing for respiratory tract infections in Dutch primary care in relation to patient age and clinical entities. J Antimicrob Chemother. 2004;54:1116–1121. doi: 10.1093/jac/dkh480. [DOI] [PubMed] [Google Scholar]
- 10.Majeed A, Moser K. Age- and sex-specific antibiotic prescribing patterns in general practice in England and Wales in 1996. Br J Gen Pract. 1999;49:735–736. [PMC free article] [PubMed] [Google Scholar]
- 11.Cadieux G, Tamblyn R, Dauphinee D, Libman M. Predictors of inappropriate antibiotic prescribing among primary care physicians. CMAJ. 2007;177:877–883. doi: 10.1503/cmaj.070151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kozyrskyj AL, Dahl ME, Chateau DG, Mazowita GB, Klassen TP, Law BJ. Evidence-based prescribing of antibiotics for children: role of socioeconomic status and physician characteristics. CMAJ. 2004;171:139–145. doi: 10.1503/cmaj.1031629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuyvenhoven M, de Melker R, van der Velden K. Prescription of antibiotics and prescribers' characteristics. A study into prescription of antibiotics in upper respiratory tract infections in general practice. Fam Pract. 1993;10:366–370. doi: 10.1093/fampra/10.4.366. [DOI] [PubMed] [Google Scholar]
- 14.Hwang JH, Kim DS, Lee SI, Hwang JI. Relationship between physician characteristics and their injection use in Korea. Int J Qual Health Care. 2007;19:309–316. doi: 10.1093/intqhc/mzm030. [DOI] [PubMed] [Google Scholar]
- 15.Jo CI, Lim JY, Soo YL. The effect of the degree of competition of the hospital market regions on clinic's rate of antibiotics prescription. KDI J Econ Policy. 2008;30:132–155. [Google Scholar]
- 16.Parchman ML. Small area variation analysis: a tool for primary care research. Fam Med. 1995;27:272–276. [PubMed] [Google Scholar]
- 17.Cho WH, Lee SH, Park EC, Sohn MS, Kim SR. An analysis of small area variations of hospital services utilization in Korea. Korean J Prev Med. 1994;27:609–626. [Google Scholar]
- 18.Thrane N, Olesen C, Schønheyder HC, Sørensen HT. Socioeconomic factors and prescription of antibiotics in 0- to 2-year-old Danish children. J Antimicrob Chemother. 2003;51:683–689. doi: 10.1093/jac/dkg118. [DOI] [PubMed] [Google Scholar]
- 19.Britten N, Ukoumunne O. The influence of patients' hopes of receiving a prescription on doctors' perceptions and the decision to prescribe: a questionnaire survey. BMJ. 1997;315:1506–1510. doi: 10.1136/bmj.315.7121.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutschmann OT, Domino ME. Antibiotics for upper respiratory tract infections in ambulatory practice in the United States, 1997-1999: does physician specialty matter? J Am Board Fam Pract. 2004;17:196–200. doi: 10.3122/jabfm.17.3.196. [DOI] [PubMed] [Google Scholar]
- 21.Chonmaitree T, Revai K, Grady JJ, Clos A, Patel JA, Nair S, Fan J, Henrickson KJ. Viral upper respiratory tract infection and otitis media complication in young children. Clin Infect Dis. 2008;46:815–823. doi: 10.1086/528685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kristo A, Uhari M. Timing of rhinosinusitis complications in children. Pediatr Infect Dis J. 2009;28:769–771. doi: 10.1097/INF.0b013e3181a3aa7f. [DOI] [PubMed] [Google Scholar]
- 23.Mainous AG, 3rd, Hueston WJ, Love MM. Antibiotics for colds in children: who are the high prescribers? Arch Pediatr Adolesc Med. 1998;152:349–352. [PubMed] [Google Scholar]
- 24.Janjua NZ, Hutin YJ, Akhtar S, Ahmad K. Population beliefs about the efficacy of injections in Pakistan's Sindh province. Public Health. 2006;120:824–833. doi: 10.1016/j.puhe.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Kim NS, Jang SN, Jang SM. Factors influencing antibiotics prescribing of primary health physicians in acute upper respiratory infections. J Prev Med Public Health. 2005;38:1–8. [PubMed] [Google Scholar]
- 26.Wang KY, Seed P, Schofield P, Ibrahim S, Ashworth M. Which practices are high antibiotic prescribers? A cross-sectional analysis. Br J Gen Pract. 2009;59:e315–e320. doi: 10.3399/bjgp09X472593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welschen I, Kuyvenhoven MM, Hoes AW, Verheij TJ. Effectiveness of a multiple intervention to reduce antibiotic prescribing for respiratory tract symptoms in primary care: randomised controlled trial. BMJ. 2004;329:431. doi: 10.1136/bmj.38182.591238.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Altiner A, Brockmann S, Sielk M, Wilm S, Wegscheider K, Abholz HH. Reducing antibiotic prescriptions for acute cough by motivating GPs to change their attitudes to communication and empowering patients: a cluster-randomized intervention study. J Antimicrob Chemother. 2007;60:638–644. doi: 10.1093/jac/dkm254. [DOI] [PubMed] [Google Scholar]