Abstract
Background: Asthma is a sometimes severe respiratory illness with an increased prevalence, especially in low-income, minority, and inner-city populations, over the past 2 decades. Prior reports have suggested a link between depression and asthma deaths. However, no studies have examined the relationship between objective measures of asthma severity and clinician-rated depressive symptom severity.
Method: In this pilot study, 46 children receiving treatment at an inner-city asthma clinic were assessed with the Children's Depression Rating Scale, Revised (CDRS-R). The current percentage of forced expiratory volume in 1 second (FEV1%) predicted and the inhaled steroid dose were recorded, as were oral steroid use, emergency room visits, and hospitalizations in the preceding year.
Results: Depressive symptoms were common in this sample, with 30% (N = 14) of the participants having CDRS-R scores consistent with likely, very likely, or almost certain major depressive disorder. When mean CDRS-R scores were compared between the sample divided by these asthma severity measures, only hospitalizations in the past year was associated with higher depressive symptom scores (p = .03).
Conclusion: These findings suggest that in the patient sample studied, depressive symptoms appear to be common. However, depressive symptom severity is related only to hospitalization, not other measures of asthma severity. Larger studies are needed to confirm these findings and determine if other variables such as family history of depression or subjective assessment of asthma severity explain the high prevalence of depressive symptoms in these patients.
Asthma is a common and sometimes severe and chronic medical condition. Asthma prevalence, mortality, and hospitalizations have increased dramatically in the past 2 decades, particularly in children in low-income, inner-city, and minority communities.1–5
Depressive symptoms may be associated with poor asthma medication compliance,6 increased asthma severity,7 and asthma-related morbidity and mortality.8,9 Strunk et al.7 found that 78% of children who later died of asthma had depressive symptoms versus 56% of controls with less severe asthma (p = .05). Mascia et al.9 examined the psychological characteristics of children with severe asthma (N = 140) over a 10-year period and found depressive symptoms in 77% of fatalities. Together, these studies suggest that depressive symptoms in children may be associated with greater asthma severity.
Moreover, depressive symptoms may be common in children with asthma. Seigel and Golden10 found adolescents with asthma (N = 40) had significantly higher Beck Depression Inventory scores than normal controls (p < .001) and scores similar to those of patients with sickle cell disease and diabetes. As the subjects were relatively asymptomatic outpatients, the investigators suggested that the increase in depressive symptoms was not related to asthma symptoms. Padur et al.11 found significantly higher scores on the Child Depression Inventory in children with asthma (N = 25) than in children with diabetes (N = 25) or cancer (N = 25) or healthy controls (N = 25). Meijer12 examined dependency and emotional disturbance in children with asthma (N = 31) and found that “low-dependency” boys with asthma had significantly more depressive symptoms (p = .05), as determined by the Mother-Child Questionnaire, than non-asthmatic low-dependency boys. Low-dependency girls with asthma also showed more depression than their high-dependency counterparts, but the difference was not significant. Weil et al.13 found that self-reported caregiver assessment of mental health, but not the child's mental health, correlated with frequency of hospitalization.
However, in a large study (N = 1041), Bender et al.14 found no increase in scores for self-reported depression, anxiety, and other psychological symptoms in children with mild-to-moderate asthma. Only 1 measure of asthma symptom severity, postbronchodilator percentage of forced expiratory volume in 1 second (FEV1%) predicted, showed even a modest (r = −0.071, p < .05) correlation with depressive symptoms scores. Vila et al.15 found that none of 93 children in France with asthma had major depressive disorder and only 5/93 (5%) had dysthymic disorder, findings similar to depressive symptoms scores on a self-report questionnaire of a control group (N = 93) with diabetes.
Most depression studies in children with asthma have relied on self-report measures of psychiatric symptoms. These instruments offer the advantage of ease of administration and thus allow large numbers of subjects to be screened. However, as self-report measures rely solely on the patient's subjective assessment of depressive symptoms, using such measures may result in overreporting. Kessler et al.16 pointed out in a recent review that self-report depression instruments have found that “20% and 50% of children and adolescents exceed conventionally established adult cut points for clinically significant depression,”(p1004) while studies using diagnostic interviews have reported a point prevalence of 1% to 6%. Similar findings were recently reported in a meta-analysis of 42 studies in adult patients with diabetes, in which Anderson et al.17 found a 31% prevalence of depression in studies using self-report instruments but a prevalence of only 11% in studies relying on diagnostic interviews. To our knowledge, no studies published to date have used clinician-administered instruments to examine the prevalence of depressive symptoms and their relationship to asthma severity in a primarily minority, inner-city children's asthma clinic setting despite the fact that this population appears to be at great risk for asthma-related morbidity and mortality. In this pilot study, we examined clinician-rated depressive symptoms in inner-city children with asthma.
METHOD
Subjects were recruited at scheduled visits to the Children's Medical Center Asthma Clinic in Dallas, Texas. This clinic is located near downtown Dallas and primarily serves children from low-income families, including many minority families. Children with relatively severe asthma and those who have had recent hospitalizations for asthma are typically referred to this clinic. At clinic appointments, a consecutive series of subjects were asked to participate after completion of their asthma evaluation. An Institutional Review Board–approved form acknowledging informed consent was signed by both the child and guardian prior to assessment. Inclusion criteria included a physician diagnosis of asthma and an age of 6 to 17 years. Exclusion criteria were kept to a minimum to obtain a representative sample of the clinic population. However, subjects were excluded if they or their parents were non–English-speaking or cognitively impaired or if their parents were potentially vulnerable persons including prisoners and pregnant or nursing women.
Demographic and medical information was obtained from the patient and guardian, treating physician, and medical record including age, gender, current medications, number of hospitalizations, emergency room visits, oral steroid courses in the past year, and current FEV1% predicted that was obtained from routine spirometry on the day of clinic visit using a SensorMedics spirometer (SensorMedics Corporation, Yorba Linda, Calif.). The Children's Depression Rating Scale, Revised (CDRS-R)18 was then administered by one of the investigators (K.M.M. or A.G.) trained in the use of the instrument with established interrater reliability. The CDRS-R is a validated 17-item, clinician-administered instrument for the assessment of depressive symptoms in children aged 6 years through adolescence19 that can be reliably administered by staff members with minimal training.20 Questions on the CDRS-R assess a variety of depressive symptoms including impaired schoolwork, difficulty having fun, social withdrawal, appetite disturbance, sleep disturbance, excessive fatigue, physical complaints, irritability, excessive guilt, low self-esteem, depressed feelings, morbid ideation, suicidal ideation, excessive weeping, depressed facial affect, listless speech, and hypoactivity. Scores are primarily used to rate severity of depressive symptomatology, not to diagnose depressive disorders. However, normative data are available that rate/categorize patients' likelihood of meeting diagnostic criteria for a depressive disorder, based on normative t-scores, as extremely rare (≤ 39), unlikely (40–54), possible (55–64), likely (65–74), very likely (75–84), and almost certain (≥ 85).18 These normative data (t-scores) rather than raw scores are used in this report.
The subjects were then separated by FEV1% predicted (> 80 vs. ≤ 80, best of 3 attempts), inhaled steroid dose (high dose vs. medium/low/none [based on National Heart, Lung, and Blood Institute guidelines]),21 and oral steroid use, hospitalizations, and emergency room visits (yes vs. no) in the past 12 months. Unpaired, 2-sided t tests were used to compare mean CDRS-R scores between groups categorized as above using an a priori alpha of .05.
RESULTS
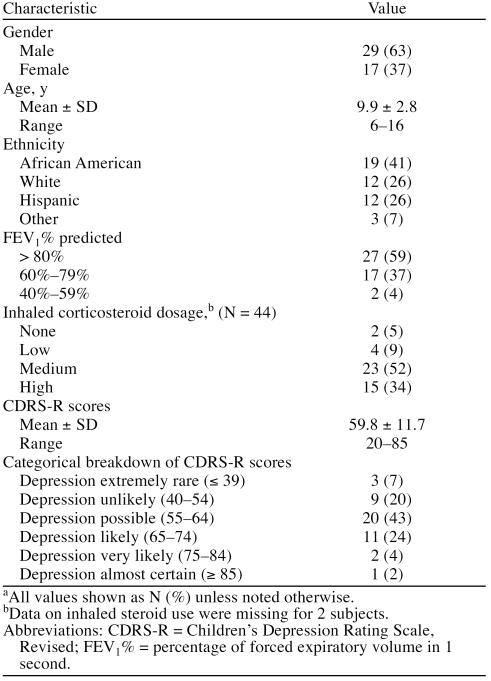
A total of 49 subjects and guardians were asked to participate; 2 declined to participate, and 1 who did not speak English was excluded. The demographic information and CDRS-R scores of the 46 participants are given in Table 1. Eighty-six percent of children (38/44) were taking medium or high doses of inhaled corticosteroids (data on inhaled steroid use were missing for 2 subjects, thus N = 44 for this outcome measure). Forty-one percent of children (N = 19) had evidence of mild-moderate airway obstruction, despite taking inhaled corticosteroids. Of all subjects, 14/46 (30%) had CDRS-R scores with the range of likely, very likely, or almost certain depression. The mean CDRS-R score was in the range of possible depression.
Table 1.
Demographic Information for Study Participants (N = 46)a
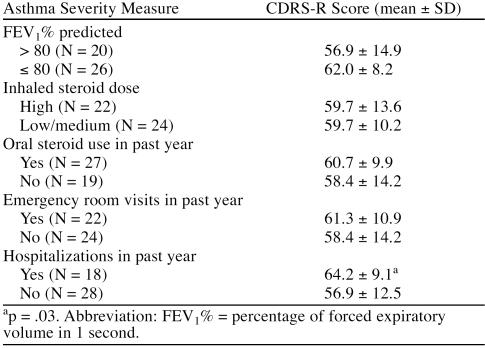
Subjects were divided by demographic variables and measures of asthma severity including FEV1% and inhaled steroid dose and oral steroid use, emergency room visits, and hospitalizations in the past year. Differences between these groups in mean CDRS-R scores are given in Table 2. No statistically significant between-group differences were found except for higher CDRS-R scores in patients who had been hospitalized in the past year.
Table 2.
Relationship of Children's Depression Rating Scale, Revised (CDRS-R) Scores to Asthma Severity in 46 Subjects
DISCUSSION
The results suggest that depressive symptoms are common in this sample of inner-city minority youths with asthma. The 30% current prevalence of likely depression is much higher than the 1% to 6% reported in epidemiologic studies in children.16 However, without more extensive diagnostic interviews, one cannot determine if all of the participants with likely depression actually met full diagnostic criteria for major depressive disorder.
This study, in general, did not support a relationship between asthma severity and depression scores. Only 1 of the measures of asthma severity, hospitalization in the past year, was associated with higher depression scores. However, the relationship between hospitalization and depressive symptom severity is intriguing in light of the earlier reports by Strunk et al.7 and Mascia et al.9 suggesting a relationship between depression and asthma-related death in children. Perhaps severe asthma exacerbations resulting in hospitalization or even death may be associated with depression. Larger studies examining the impact of depression on asthma-related hospitalizations, intubations, and mortality are needed.
In adult populations, other investigations that, like ours in children, relied primarily on objective rather than subjective measures of asthma severity have reported similar findings. We recently reported similar findings, suggesting depression is not associated with more severe asthma, in a group of inner-city adults with asthma.22 Janson et al.23 found a correlation between depression and self-reported asthma-related symptoms, but no correlation between a diagnosis of asthma and depression or objective asthma-related measurements (e.g., spirometry) and depression. Janson-Bjerklie et al.24 found that elevated scores on the Center for Epidemiologic Studies-Depression Scale (CES-D) were related to subjectively perceived asthma severity and danger, but not to objective asthma severity (i.e., medication, intubation history, and hospitalization frequency). Our findings in children are consistent with a recent report by Brinke et al.25 in adults that found no differences in objective measures of asthma severity between those with or without psychiatric symptoms, but that did find more frequent asthma-related physician, emergency room, and hospital visits in the group with psychiatric symptoms.
There are several methodological limitations in our study. First, the single FEV1% predicted used may not reflect the severity of a chronic illness. Second, the majority of patients seen in this clinic had moderate-to-severe, persistent asthma and were taking medium or high doses of inhaled corticosteroids, making it difficult to show a difference between various inhaled corticosteroid dosages and depression scores. In fact, only 14% of subjects were taking low or no inhaled corticosteroid. Nevertheless, this patient population is representative of high-risk patients with asthma in the inner city. Third, given the relatively small sample size, a type I error may be a possible explanation for our findings. Several measures of asthma severity including lower FEV1% predicted, emergency room visits, and oral steroid use in the past year were associated with numerically higher depression scores than the comparison group, although these findings did not reach significance. However, these between-group differences were small and not likely of clinical significance. The depression instrument used may exaggerate the prevalence of depressive symptoms in a medically ill population due to inflation of scores from asthma symptoms. However, the CDRS-R emphasizes cognitive (e.g., excessive guilt, morbid ideation) rather than neurovegetative factors (e.g., sleep disturbance, physical complaints), which may minimize this potential problem (see Method for a full listing of CDRS-R questions). In addition, one might expect a depression scale heavily weighted toward physical symptoms to show an exaggerated association between depression and asthma severity rather than the similar between-group depression scores observed in this study. Finally, given the study design, we cannot determine if depression is the direct cause of increased hospitalizations or if the relationship is indirect and mediated through living conditions, family dysfunction, poor access to health care, or other factors. For example, a recent study found that adolescent depression was associated with many problems in early adulthood, including early parenthood, substance abuse, and failure to attend college.26 However, these outcomes appeared to be secondary to confounding social and environmental factors, and not directly related to depression.
An important finding in this study is that the inner-city children with asthma in our sample had higher depression scores than expected in the general population. Physicians should be aware of the risk for depression in asthma patients and, when necessary, treat with antidepressants or make referrals to mental health professionals for further evaluation.
Footnotes
The authors report no financial affiliation or other relationship relevant to the subject matter of this article.
REFERENCES
- The Centers for Disease Control. Leads from the Morbidity and Mortality Weekly Report: Asthma—United States, 1980–1990. JAMA. 1992;268:1995, 1998. [Google Scholar]
- Weitzman M, Gortmaker SL, Sobol AM, et al. Recent trends in the prevalence and severity of childhood asthma. JAMA. 1992;268:2673–2677. [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Pertowski CA, et al. Surveillance for asthma—United States, 1960–1995. Morb Mortal Wkly Rep CDC Surveill Summ. 1998;47:1–27. [PubMed] [Google Scholar]
- Evans R, Mullally DI, Wilson RW, et al. National trends in the morbidity and mortality of asthma in the US: prevalence, hospitalization and death from asthma over two decades: 1965–1984. Chest. 1987;91:65S–74S. [PubMed] [Google Scholar]
- Weiss KB, Wagener DK. Changing patterns of asthma mortality identifying target populations at high risk. JAMA. 1990;264:1683–1687. [PubMed] [Google Scholar]
- Bosley CM, Fosbury JA, Cochrane GM. The psychological factors associated with poor compliance with treatment in asthma. Eur Respir J. 1995;8:899–904. [PubMed] [Google Scholar]
- Strunk RC, Mrazek DA, Fuhrmann GS, et al. Physiologic and psychological characteristics associated with deaths due to asthma in childhood: a case-controlled study. JAMA. 1985;254:1193–1198. [PubMed] [Google Scholar]
- Picado C, Montserrat JM, de Pablo J, et al. Predisposing factors to death after recovery from a life-threatening asthmatic attack. J Asthma. 1989;26:231–236. doi: 10.3109/02770908909073254. [DOI] [PubMed] [Google Scholar]
- Mascia A, Frank S, Berkman A, et al. Mortality versus improvement in severe chronic asthma: physiologic and psychologic factors. Ann Allergy. 1989;62:311–317. [PubMed] [Google Scholar]
- Seigel WM, Golden NH. Depression, self-esteem, and life events in adolescents with chronic diseases. J Adolesc Health. 1990;11:501–504. doi: 10.1016/0197-0070(90)90110-n. [DOI] [PubMed] [Google Scholar]
- Padur JS, Rapoff MA, Houston BK, et al. Psychosocial adjustment and the role of functional status for children with asthma. J Asthma. 1995;32:345–353. doi: 10.3109/02770909509082759. [DOI] [PubMed] [Google Scholar]
- Meijer A. Emotional disorders of asthmatic children. Child Psychiatry Hum Dev. 1979;9:161–169. doi: 10.1007/BF01433479. [DOI] [PubMed] [Google Scholar]
- Weil CM, Wade SL, Bauman LJ, et al. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–1280. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- Bender BG, Annett RD, and Ikle D. et al, for the CAMP Research Group. Relationship between disease and psychological adaptation in children in the Childhood Asthma Management Program and their families. Arch Pediatr Adolesc Med. 2000 154:706–713. [DOI] [PubMed] [Google Scholar]
- Vila G, Nollet-Clemencon C, Vera M, et al. Prevalence of DSM-IV disorders in children and adolescents with asthma versus diabetes. Can J Psychiatry. 1999;44:562–569. doi: 10.1177/070674379904400604. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Mokros HB. Children's Depression Rating Scale, Revised (CDRS-R), Administration Booklet. Los Angeles, Calif: Western Psychological Services. 1995 [Google Scholar]
- Poznanski EO, Grossman JA, Buchsbaum Y, et al. Preliminary studies of the reliability and validity of the Children's Depression Rating Scale. J Am Acad Child Psychiatry. 1984;23:191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Cook SC, Carroll BJ, et al. Use of the Children's Depression Rating Scale in an inpatient psychiatric population. J Clin Psychiatry. 1983;44:200–203. [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Practical Guide for the Diagnosis and Management of Asthma. Based on the Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Institutes of Health. 1997 NIH publication 97-4053. [Google Scholar]
- Nejtek VA, Brown ES, Khan DA, et al. Prevalence of mood disorders and relationship to asthma severity in patients at an inner-city asthma clinic. Ann Allergy Asthma Immunol. 2001;87:129–133. doi: 10.1016/s1081-1206(10)62206-5. [DOI] [PubMed] [Google Scholar]
- Janson C, Bjornsson E, Hetta J, et al. Anxiety and depression in relation to respiratory symptoms and asthma. Am J Respir Crit Care Med. 1994;149:930–934. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- Janson-Bjerklie S, Ferketich S, Benner P, et al. Clinical markers of asthma severity and risk: importance of subjective as well as objective factors. Heart Lung. 1992;21:265–272. [PubMed] [Google Scholar]
- Brinke A, Ouwerkerk ME, Bel EH, et al. Similar psychological characteristics in mild and severe asthma. J Psychosom Res. 2001;50:7–10. doi: 10.1016/s0022-3999(00)00203-8. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]