PEARLS
Type A aortic dissection (originating proximally to the aortic arch) is a rare cause of acute stroke because dissection itself is rare, but nearly 30% of dissections present with neurologic symptoms.
Aortic dissection should be considered in all patients with acute stroke who have chest or back pain, present with syncope, or have asymmetric peripheral pulses.
Even when dissection is not clinically suspected, all imaging studies (including noninvasive neck angiography) should be thoroughly reviewed as they may contain valuable information about the aortic arch and the possibility of a life-threatening aortic dissection.
OYSTER
Painless aortic dissection presenting with neurologic symptoms may be easily missed if the history, physical examination, and review of imaging studies are not conducted with dissection in the differential.
CASE REPORT
An 82-year-old woman presented to the emergency room 14 hours following the onset of headache and gait unsteadiness. Twelve hours after the symptoms began, she developed left facial droop and dysarthria. The facial droop and dysarthria had resolved prior to her evaluation in the emergency room, but the gait unsteadiness and headache persisted. She had no pain aside from the mild frontal headache. Hyperlipidemia was her only identified stroke risk factor. Vital signs on admission included a blood pressure of 124/47 mm Hg and heart rate of 70 beats per minute. No murmurs were appreciated on cardiac auscultation, and pulses were symmetric. Complete neurologic examination revealed only mild truncal ataxia. She had symmetric facial strength and no dysarthria. She had no pronator drift. She had no finger-to-nose or heel-to-shin ataxia. Muscle stretch reflexes were symmetric and plantar responses were equivocal bilaterally. Chest x-ray demonstrated borderline cardiomegaly, and head CT showed chronic bilateral subcortical infarcts.
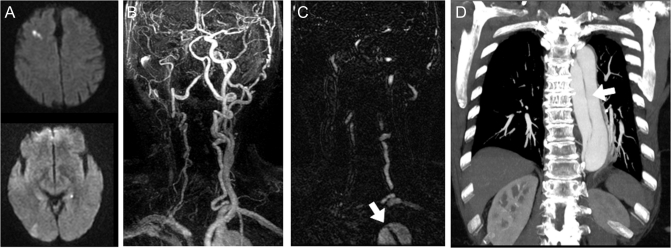
The patient was admitted for stroke evaluation and risk factor management. MRI of the head performed 8 hours into her admission (28 hours after initial symptoms) showed small right frontal and occipital areas of restricted diffusion consistent with acute cerebral infarctions (figure, A). Her head and neck contrast-enhanced magnetic resonance angiography (MRA) was performed using a neurovascular coil, and the results were notable for severe stenosis vs occlusion of her right common and internal carotid arteries (figure, B). However, further review of the axial phase of the contrasted images revealed an abnormality in the aortic arch concerning for dissection (figure, C). An urgent chest CT revealed a type A aortic dissection (figure, D).
Figure. An 82-year-old woman with acute stroke and painless aortic dissection.
MRI head with (A) diffusion-weighted images showing multiple areas of increased signal intensity (right frontal > right occipital). Contrast-enhanced magnetic resonance angiography of head and neck where (B) right common and internal carotid are not visualized, and (C) a thin black line is identified within the aortic arch on the axial phase of contrasted images thought to represent an intimal flap. (D) Contrast-enhanced chest CT illustrating Stanford type A dissection extending down the abdominal aorta.
She was taken for emergent surgical repair of her aorta, including replacement of the ascending aorta and arch with a patch of the innominate and carotid arteries. She spent 6 weeks in the hospital and an acute rehabilitation facility and at 3 months was ambulating without assistive devices and without residual neurologic deficit.
DISCUSSION
Type A aortic dissection carries a rapidly escalating mortality rate (25% during the first 24 hours of initial presentation and up to 80% in the first 2 weeks) but remains a challenging diagnosis given its variable presentation and low incidence of 5 to 30 cases per million per year.1 It remains an important diagnostic consideration for neurologists, as shown by a study of 102 consecutive patients with identified type A aortic dissection where approximately 30% of the patients had neurologic symptoms at the time of initial presentation.2 Over half (53%) of the cases with neurologic symptoms presented with cerebral ischemia, although ischemic neuropathy (37%), syncope (20%), somnolence (13%), seizures (10%), and other neurologic symptoms also occurred.2 The majority of strokes were hemispheric and predominantly right-sided in spite of frequent bilateral carotid artery extension.3
Painless dissection occurs in less than 10% of patients with aortic dissection, but a higher percentage of those cases present with stroke symptoms.4 Review of the literature on stroke and aortic dissection reveals that painless dissection is diagnosed in a variety of ways. Multiple case reports detail clinical features including altered consciousness or pulse asymmetry which led to confirmatory tests such as echocardiography or chest CT.5,6 However, the clinical examination findings recommended in aiding a diagnosis of dissection such as pulse asymmetry and cardiac murmur are seen in less than 20% and 50% of cases, respectively.7 These relatively low diagnostic yields do not minimize the importance of looking for clinical symptoms and signs of dissection but suggest that review of imaging results may increase diagnostic potential.
While the imaging studies for workup of cerebral ischemia typically do not overlap with diagnostic studies for aortic dissection, the stroke workup may still provide useful clues. Chest x-ray is currently recommended as an immediate diagnostic test in acute stroke patients with suspected acute cardiac or pulmonary disease,8 and it shows classic mediastinal widening in up to 50% of patients with dissection.1 Additionally, our case highlights the potential for aortic dissection to be visualized through noninvasive neck angiography. Both neck CT angiography and MRA may contain valuable imaging detail of the aortic arch, including the possibility of a painless dissection. We have identified one other case report detailing a diagnosis of painless aortic dissection from a linear intraluminal signal in the aortic arch on neck MRA.9 However, it should be noted that neck MRA cannot reliably exclude aortic dissection since the arch is not always well visualized, particularly in larger patients where the neurovascular coil may not extend far enough caudally.
The “incidental” diagnosis of dissection in our patient emphasizes the importance of keeping dissection in the differential for any patient presenting with stroke-like symptoms. It is difficult to justify the routine use of noninvasive chest imaging to rule out an aortic dissection given the rarity of dissection and possible treatment delay in the acute stroke setting. However, it should be strongly considered if there are any symptoms to suggest dissection. Chest x-rays ordered should be carefully reviewed for mediastinal widening and calcification of the aorta or great vessels. Additionally, even when the diagnosis is not suspected, all neck angiography studies should be reviewed thoroughly for dissection if the aortic arch is visualized. In our case, neck MRA, with rapid and careful radiologic review of all sequences, improved the speed of diagnosis. This allowed for acute surgical repair, which has been proven both safe and successful in the acute stroke setting.10
ACKNOWLEDGMENT
The authors thank John Bisognano for review of the manuscript.
DISCLOSURE
Dr. Hyland reports no disclosures. Dr. Holloway serves as Chair of DSMB for NINDS-sponsored ALS clinical trial; serves as an Associate Editor for Neurology Today; serves as a consultant for Milliman Inc.; and receives research support from the US Veterans Administration and the NIH/NCRR.
REFERENCES
- 1. Khan IA, Nair C. Clinical, diagnostic, and management perspectives of aortic dissection. Chest 2002;122:311–328 [DOI] [PubMed] [Google Scholar]
- 2. Gaul C, Dietrich W, Friedrich I, et al. Neurological symptoms in type A aortic dissections. Stroke 2007;38:292–297 [DOI] [PubMed] [Google Scholar]
- 3. Gaul C, Dietrich W, Erbguth F. Neurological symptoms in aortic dissection: a challenge for neurologists. Cerebrovasc Dis 2008;26:1–8 [DOI] [PubMed] [Google Scholar]
- 4. Park SW, Hutchison S, Mehta RH, et al. Association of painless acute aortic dissection with increased mortality. Mayo Clinic Proc 2004;79:1252–1257 [DOI] [PubMed] [Google Scholar]
- 5. Wright V, Horvath R, Baird AE. Aortic dissection presenting as acute ischemic stroke. Neurology 2003;61: 581 [DOI] [PubMed] [Google Scholar]
- 6. Grupper M, Eran A, Shifrin A. Ischemic stroke, aortic dissection, and thrombolytic therapy: the importance of basic clinical skills. J Gen Intern Med 2007;22:1370–1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000;283:897–903 [DOI] [PubMed] [Google Scholar]
- 8. Adams HP, Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Stroke 2007;38:1655–1711 [DOI] [PubMed] [Google Scholar]
- 9. Green SM, Macha M. Acute aortic dissection presenting as hemifacial weakness. Resident Staff Physician 2008;54 [Google Scholar]
- 10. Estrera AL, Garami Z, Miller CC, et al. Acute type A dissection complicated by stroke: can immediate repair be performed safely? J Thorac Cardiovasc Surg 2006;132:1404–1408 [DOI] [PubMed] [Google Scholar]